Ethics and Total Worker Health®: Constructs for Ethical Decision-Making and Competencies for Professional Practice
Abstract
1. Introduction
2. Ethics
3. Ethical Principles
- Conducting team walk-throughs to identify potential hazards and make recommendations for hazard abatement;
- Targeting potential causes of stress be they work (e.g., work overload) or non-work-related (e.g., lactation support) for risk reduction;
- Providing health screenings, such as preplacement and periodic examinations, that may identify early disease or disease interactive agents (e.g., noise exposure and presbycusis);
- Providing protective immunizations (e.g., influenza vaccine; Sars-CoV-2 vaccine);
- Placement of engineering controls or development of a back-injury prevention program for workers with previous back injury;
- Assuring a worker with a disability that they will receive the best possible disability health care, through providing qualified health care providers;
- Providing adequate and continuous training so workers know how to do the job and are aware of potential hazards and their rights and responsibilities.
- The TWH approach seeks to both protect workers (nonmaleficence) and promote their well-being (beneficence).
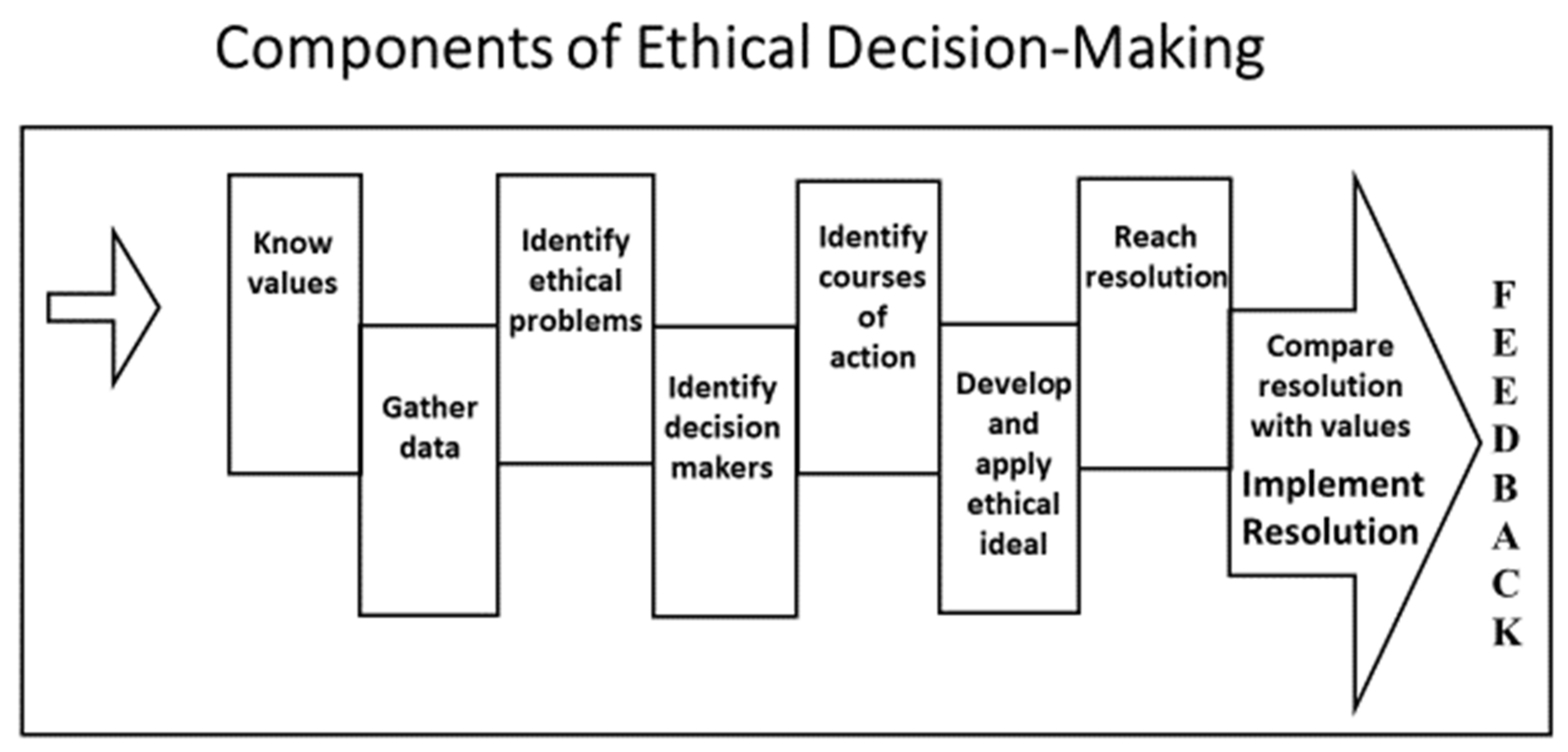
4. Ethical Decision-Making
5. Case Study
- Know values
- Gather data
- Identify ethical problems
- Identify decision-makers
- Identify courses of action
- Develop and apply the ethical ideal
- Reach a resolution
- Compare the resolution with values
- Implement the resolution
- Feedback
6. Case Presentation
7. Ethical Analysis
7.1. Know Values
- Corporate executives value a TWH program, specifically to improve worker satisfaction and retention.
- The VP values healthier workers but focuses on the attainment of a healthy weight.
- The corporation values workers by offering health care insurance but believes premiums could be lower if workers were healthier. Lower health insurance premiums would improve the financial health of the corporation and could save money for the workers themselves.
- The TWH practitioner believes a comprehensive approach is needed to address worker health issues, including weight, stress, fatigue, and lifting injuries.
- The TWH practitioner has been offered monetary and prestige incentives to implement the mandatory weight loss program.
- A TWH program is of value to some workers.
- Informed consent for workers and confidentiality of health information is valued by the OSH/TWH professional and workers but their value to corporate executives is uncertain given the directive for a mandatory program.
7.2. Gather Data
- Activities undertaken to date for TWH program implementation including the workers’ input who have been involved in program development.
- Demographic data of workforce.
- Aggregated statistics related to the prevalence of workers who are overweight and obese, and the associated insurance costs as compared with workers whose weight is in the normal range.
- Aggregated statistics on workers’ compensation for worker injuries related to unsafe resident handling procedures.
- Potential burden of health insurance penalties for those who do not achieve the desired weight loss.
- Staffing to resident ratios; current and recent trends.
- Use of mandatory overtime, including double shifts and perceived stress levels among the workers.
- Issues and formal complaints regarding compromised quality of care for residents.
- Costs associated with mechanical lift devices including equipment and training.
- Types of meals offered at the facilities.
- How the confidentiality of health data is managed.
7.3. Identify Ethical Problems
- Autonomy—Coercion and paternalism by management for mandatory worker participation in a weight loss program; lack of worker informed consent; pressure from management for OSH/TWH professional to conduct a mandatory weight loss program, with a potential conflict of interest for bonus pay/incentives, which could be in conflict with the professional code of ethics and also considered professionally offensive.
- Nonmaleficence—Staff shortages resulting in mandatory overtime, including double shifts for workers creating stress, fatigue, and potential practice errors; exposure to continued unsafe lifting practices of residents create a further risk of harm; failure to achieve weight loss creating worker poor self-image and concern for continued employment.
- Beneficence—Purchase of mechanical device equipment rejected by management because of cost; company meals provided are mostly fatty or fried food.
- Justice—Health insurance penalties for those who do not or who are unable to lose the required amount of weight in the defined period discriminate against this worker group; a monetary penalty may impact worker salary.
7.4. Identify Decision-Makers
7.5. Identify Courses of Action
- Ask a representative from each department of the local residential facilities to offer one or two suggestions for making the work environment safer and healthier and improving the health of staff members.
- Offer voluntary weight management program with incentives for weight loss, including new uniforms to celebrate weight loss achievements; eliminate health insurance penalties for workers who are unable to achieve the desired biometrics in the defined time.
- Develop a plan for using dietary staff and kitchens in residential facilities to provide healthier meal options for staff during their work shifts.
- Identify funding options (budget, grant, gift) for purchase/rental of mechanical lift devices for residents with limited mobility. Eliminate the need for staff bonuses.
- Focus efforts on becoming a community employer of choice to help eliminate staffing shortages (long-term).
- Refuse to implement weight loss program unless voluntary for workers, without penalty, and with informed consent and confidentiality of health information and seek higher chain of command for discussion. Indicate that this would be a violation of the professional code of ethics.
7.6. Develop and Apply Ethical Ideal
7.7. Reach Resolution
7.8. Compare Resolution with Values, Implement, and Provide Feedback
8. Professional Codes of Ethics
9. Ethical Competencies in Total Worker Health
Occupational health should aim at: the promotion and maintenance of the highest degree of physical, mental and social well-being of workers in all occupations; the prevention amongst workers of departures from health caused by their working conditions; the protection of workers in their employment from risks resulting from factors adverse to health; the placing and maintenance of the worker in an occupational environment adapted to his physiological and psychological capabilities; and, to summarize, the adaptation of work to man and of each man to his job. The main focus in occupational health is on three different objectives: (i) the maintenance and promotion of workers’ health and working capacity; (ii) the improvement of working environment and work to become conducive to safety and health; and (iii) development of work organizations and working cultures in a direction which supports health and safety at work and in doing so also promotes a positive social climate and smooth operation and may enhance productivity of the undertakings. The concept of working culture is intended in this context to mean a reflection of the essential value systems adopted by the undertaking concerned. Such a culture is reflected in practice in the managerial systems, personnel policy, principles for participation, training policies and quality management of the undertaking [33].
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tamers, S.L.; Streit, J.; Pana-Cryan, R.; Ray, T.; Syron, L.; Flynn, M.A.; Howard, J. Envisioning the future of work to safeguard the safety, health, and well-being of the workforce: A perspective from the CDC’s National Institute for Occupational Safety and Health. Am. J. Ind. Med. 2020, 63, 1065–1084. [Google Scholar] [CrossRef] [PubMed]
- Schulte, P.A.; Pandalai, S.; Wulsin, V.; Chun, H.K. Interaction of occupational and personal risk factors in workforce health and safety. Am. J. Public Health 2012, 102, 434–448. [Google Scholar] [PubMed]
- Pandalai, S.P.; Schulte, P.A.; Miller, D.B. Conceptual heuristic models of the interrelationships between obesity and the occupational environment. Scand. J. Work Environ. Heath 2013, 39, 221–232. [Google Scholar] [CrossRef][Green Version]
- National Institute for Occupational Safety and Health. What Is Total Worker Health? 2020. Available online: www.cdc.gov/niosh/twh/default.html (accessed on 12 January 2020).
- Tamers, S.L.; Chosewood, L.C.; Childress, A.; Hudson, H.; Nigam, J.; Chang, C.C. Total worker health® 2014–2018: The novel approach to worker safety, health, and well-being evolves. Int. J. Environ. Res. Public Health 2019, 16, 321. [Google Scholar] [CrossRef]
- National Institute for Occupational Safety and Health. Fundamentals of Total Worker Health Approaches: Essential Elements for Advancing Worker Safety, Health, and Well-Being; DHHS (NIOSH) Publication No. 2017-112; U. S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health: Cincinnati, OH, USA, 2016.
- Hudson, H.L.; Nigam, J.A.S.; Sauter, S.L.; Chosewood, L.C.; Schill, A.L.; Howard, J. Total Worker Health; American Psychological Association: Washington, DC, USA, 2019. [Google Scholar]
- Beauchamp, T.L.; Childress, J.F. Principles of Biomedical Ethics; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Hammer, L.B.; Perry, M.L. Reducing work-life stress. In Total Worker Health; Hudson, H.L., Nigam, J.A., Sauter, S.L., Chosewood, L.C., Schill, A.L., Howard, J., Eds.; American Psychological Association: Washington, DC, USA, 2019; pp. 263–278. [Google Scholar]
- Department of Justice. Americans with Disabilities Act of 1990 Amended. 2009. Available online: https://ada.gov/pubs/adastatute08.htm (accessed on 22 January 2020.).
- Liburd, L.C.; Hall, J.E.; Mpofu, J.J.; Marshall Williams, S.; Bouye, K.; Pennman-Aguilar, A. Addressing health equity in public health practice: Frameworks, promising strategies, and measurement considerations. Annu. Rev. Public Health 2020, 41, 417–432. [Google Scholar] [CrossRef] [PubMed]
- Allen, K. What is an ethical dilemma? New Soc. Work. 2012, 19, 2. Available online: https://www.socialworker.com/feature-articles/ethics-articles/what_is_an_ethical_dilemma%3F/ (accessed on 9 March 2020).
- Iavicoli, S.; Valenti, A.; Gagliardi, D.; Rantanen, J. Ethics and occupational health in the contemporary world of work. Int. J. Environ. Res. Public Health 2018, 15, 1713. [Google Scholar]
- Curtain, L.L. How do we get into morally questionable situations? Am. Nurse Today 2014, 9, 62. [Google Scholar]
- Milliken, A. Ethical awareness: What is it and why it matters. Online J. Issues Nurs. 2018, 23, 1. [Google Scholar] [CrossRef]
- Department of Labor. Occupational Safety and Health Act of 1970; Public Law 91-5946. 2004. Available online: www.osha.gov/laws-reg/abstract/completeoshact (accessed on 22 January 2020).
- Environmental Protection Agency. Toxic Substances Control Act of 1976. 2016. Available online: https://www.ewpa.gov/laws-regulations/summary-toxic-substances-control-act (accessed on 22 January 2020).
- Department of Labor Occupational Safety and Health Administration. Hazard Communication. 2012. Available online: www.osha/gov/dsg/hazcom (accessed on 22 January 2020).
- Landsbergis, P.A.; Dobson, M.; LaMontagne, A.D.; Choi, B.; Schnall, P.; Baker, D.B. Occupational stress. In Occupational and Environmental Health; Levy, B., Wegman, D.H., Baron, S.L., Sokas, R.K., Eds.; Oxford University Press: New York, NY, USA, 2018; pp. 325–344. [Google Scholar]
- Kirch, W. (Ed.) Precautionary Principle. Encyclopaedia of Public Health 2008; Springer Science+Business Media: New York, NY, USA, 2008. [Google Scholar]
- Pless, I.B. Expanding the precautionary principle. Inj. Prev. 2003, 9, 1–2. [Google Scholar] [PubMed]
- Science and EH Network. Precautionary Principle FAQs. 2013. Available online: https://www.sehn.org/sehn/precautionary-principle-faqs (accessed on 6 September 2021).
- Rogers, B. Occupational and Environmental Health Nursing: Concepts and Practice, 2nd ed.; Saunders: Philadelphia, PA, USA, 2003. [Google Scholar]
- Rogers, B. Chapter: Legal and ethical issues. In Fundamentals of Occupational and Environmental Health Nursin, 2nd ed.; American Association of Occupational Health Nurses, Inc.: Chicago, IL, USA, 2020. [Google Scholar]
- Miranda, H.; Gore, R.J.; Boyer, J.; Nobrega, S.; Punnett, L. Health behaviors and overweight in nursing home employees: Contribution of workplace stressors and implications for worksite health promotion. Sci. World J. 2015, 2015, 915359. [Google Scholar]
- American Association of Occupational Health Nurses. Code of Ethics and Interpretive Statements. 2016. Available online: http://aaohn.org/d/do/165 (accessed on 11 April 2020).
- American College of Occupational and Environmental Medicine. The Seven Ethical Principles of Occupational and Environmental Medicine. 2010. Available online: https://acoem.org/acoem/media/PDF-Library/About_ACOEM/Code-of-Ethics-Condensed-Version.pdf (accessed on 11 April 2020).
- American Industrial Hygiene Association. Joint Industrial Hygiene Associations Member Ethical Principles. 2007. Available online: https://aiha-assets.sfo2.digitaloceanspaces.com/AIHA/resources/About-AIHA/Member-Ethical-Principles.pdf (accessed on 11 April 2020).
- American Board of Industrial Hygiene. American Board of Industrial Hygiene Code of Ethics. 2007. Available online: http://www.abih.org/sites/default/files/downloads/ABIHCodeofEthics.pdf (accessed on 11 April 2020).
- American Society of Safety Professionals. Code of Professional Conduct. 2012. Available online: https://www.assp.org/about/society-bylaws-and-guidelines/code-of-conduct (accessed on 11 April 2020).
- Coalition for National Health Education Organizations (CNHEO). Code of Ethics for Health Education Profession®. 2020. Available online: http://cnheo.org/ethics-0f-the-profession.html (accessed on 11 April 2020).
- International Commission on Occupational Health. International Code of Ethics for Occupational Safety and Health Professionals. 2012. Available online: http://www.icohweb.org/site/multimedia/code_of_ethics/code-of-ethics-en.pdf (accessed on 30 January 2020).
- Joint International Labour Organization; World Health Organization Commission on Occupational Health. Definition of Occupational Health; Twelfth Session; International Labour Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Streit, J.M.K.; Swanson, N.G.; Chosewood, L.C.; Pana-Cryan, R.; Reeves, K. NIOSH Healthy Work Design and Well-Being Program; DHHS (NIOSH) Publication 2019–171; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health: Atlanta, GA, USA, 2019. [CrossRef]
- Rogers, B.; Randolph, S.A.; Mastroianni, K. Occupational Health Nursing Guidelines for Primary Clinical Conditions, 5th ed.; OEM Press: Beverly, MA, USA, 2018. [Google Scholar]
- Rogers, B. Occupational and environmental health nursing: Ethics and professionalism. Workplace Health Saf. 2012, 60, 177–181. [Google Scholar] [PubMed]
| 1. Provide non-discriminatory care or service, based on the principle of equity, to protect health related to work. |
| 2. Practice with professional independence, based on knowledge, scientific evidence, good practice, and the highest professional standards, when making decisions related to the protection and promotion of worker health and safety. |
| 3. Emphasize primary prevention, defined in terms of worksite assessment, policies, design, technology, and practice, to determine if workers can safely complete the required job tasks. |
| 4. Protect confidentiality of individual employee health and medical data and prevent misuse of these data to respect human dignity, protect privacy, and enhance the acceptability and effectiveness of occupational health practice for physicians and nurses. |
| 5. Use validated methods for risk assessment, monitoring, and health promotion, propose effective preventive measures, assess effectiveness of implementation, and be proactive in improving health and safety for workers based on professional codes for competency and ethics. |
| 6. Recognize danger signs for violent or suicidal employees, take appropriate action, make referral, and follow up as appropriate. |
| 7. Provide sound and honest advice to employers about legal, regulatory, and ethical responsibility in the field of occupational safety and health, and to workers for the protection and promotion of their health in relation to work. |
| 8. Balance ethical principles with need to report hazards impacting others. |
| 9. Understand the concepts of risk perception, acceptable risk, and risk communication. |
| 10. Recognize prevention efforts and programs should be provided at both individualized and population-focused levels and be implemented with non-coerced, informed worker consent, including a discussion of potentially positive and negative consequences of participation in screening and health surveillance activities. Screening tests or unproven methods, which are not reliable, or methods that overly invasive should be avoided. |
| 11. Provide guidance to workers and employers about optimal health and productivity programs and the value of health promotion programs, such as those for smoking cessation, physical activity, healthy eating, and fatigue prevention. |
| 12. Provide multidisciplinary team support to the organization in creating and sustaining a culture of health at both system and individual levels while respecting the cultural and health beliefs of workers. |
| 13. Remain knowledgeable about the work, work organization, and the work environment. Be well informed on current scientific and technical knowledge about occupational hazards from biological, chemical, enviromechanical, physical, and psychosocial agent exposures and the most efficient and effective means to eliminate or to minimize toxic agent exposure risk. |
| 14. Conduct and participate in occupational health and safety program evaluations and audits to provide for continual improvement. |
| 15. Contribute to the information for workers on occupational hazards to which they may be exposed in an objective and understandable manner, which does not conceal any fact, recognizes uncertainties of known or suspected hazards, and emphasizes preventive measures while addressing language barriers and cross-cultural differences. |
| 16. Understand that determination of fitness for job duty must be based on a good knowledge of the job demands, essential job functions, the worksite, and assessment of the health of the worker. |
| 17. Seek the participation of both employers and workers in the design and implementation of health education, health promotion, health screening, and public health programs. |
| 18. Design and carry out research activities on a sound scientific basis within the context of ethical principles relevant to health and medical research work. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogers, B.; Schill, A.L. Ethics and Total Worker Health®: Constructs for Ethical Decision-Making and Competencies for Professional Practice. Int. J. Environ. Res. Public Health 2021, 18, 10030. https://doi.org/10.3390/ijerph181910030
Rogers B, Schill AL. Ethics and Total Worker Health®: Constructs for Ethical Decision-Making and Competencies for Professional Practice. International Journal of Environmental Research and Public Health. 2021; 18(19):10030. https://doi.org/10.3390/ijerph181910030
Chicago/Turabian StyleRogers, Bonnie, and Anita L. Schill. 2021. "Ethics and Total Worker Health®: Constructs for Ethical Decision-Making and Competencies for Professional Practice" International Journal of Environmental Research and Public Health 18, no. 19: 10030. https://doi.org/10.3390/ijerph181910030
APA StyleRogers, B., & Schill, A. L. (2021). Ethics and Total Worker Health®: Constructs for Ethical Decision-Making and Competencies for Professional Practice. International Journal of Environmental Research and Public Health, 18(19), 10030. https://doi.org/10.3390/ijerph181910030




