Assessing Relative Stressors and Mental Disorders among Canadian Provincial Correctional Workers
Abstract
:1. Introduction
1.1. Correctional Worker Occupational Stressors and Exposure to PPTEs
1.2. Correctional Worker Psychological Well-Being
1.3. Current Study
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.2.1. Occupational Stressors
2.2.2. Mental Disorder Symptoms
2.2.3. Total Number of PPTE Exposures
2.2.4. Sociodemographic Covariates
2.2.5. Statistical Analyses
3. Results
| Study Variable | % | n |
|---|---|---|
| Sex | ||
| Male | 48.4 | 419 |
| Female | 51.6 | 447 |
| Age | ||
| 20 to 29 years | 18.3 | 158 |
| 30 to 39 years | 29.0 | 250 |
| 40 to 49 years | 26.7 | 230 |
| 50 to 59 years | 23.9 | 206 |
| 60 years and older | 2.1 | 18 |
| Marital status | ||
| Married/common-law | 63.9 | 548 |
| Single | 18.4 | 158 |
| Separated/divorced/widowed | 14.0 | 120 |
| Remarried | 3.6 | 31 |
| Education | ||
| High school or less | 4.9 | 41 |
| Some post-secondary (less than 4-year college/university degree) | 46.6 | 393 |
| 4-year college program/university degree | 48.5 | 409 |
| Years of Service | ||
| Less than 4 years | 29.8 | 256 |
| 4 to 9 years | 12.5 | 107 |
| 10 to 15 years | 18.6 | 160 |
| More than 15 years | 39.1 | 336 |
| Occupational Category | ||
| Wellness | 8.4 | 73 |
| Training | 3.7 | 32 |
| Governance | 9.5 | 82 |
| Correctional Officers | 58.1 | 504 |
| Probation/Parole Officers | 17.2 | 149 |
| Administration | 3.2 | 28 |
| Positive PTSD Screen | ||
| No | 70.3 | 582 |
| Yes | 29.7 | 246 |
| Positive Depression Screen | ||
| No | 62.9 | 545 |
| Yes | 37.1 | 321 |
| Positive Generalized Anxiety Screen | ||
| No | 68.8 | 593 |
| Yes | 31.2 | 269 |
| Positive Panic Disorder Screen | ||
| No | 85.7 | 685 |
| Yes | 14.3 | 114 |
| Positive Alcohol Use Disorder Screen | ||
| No | 93.3 | 788 |
| Yes | 6.8 | 57 |
| Any Positive Mental Disorder Screen | ||
| No | 43.6 | 348 |
| Yes | 56.4 | 450 |
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ricciardelli, R. Surviving Incarceration: Inside Canadian Prisons; Wilfrid Laurier University Press: Brantford, ON, Canada, 2014. [Google Scholar]
- Pratt, J. Punishment and the civilizing process. In The SAGE Handbook of Punishment and Society; Simon, J., Sparks, R., Eds.; Sage Publications: London, UK, 2013. [Google Scholar]
- Butler, D.; Tasca, M.; Zhang, Y.; Carpenter, C. A systematic and meta-analytic review of the literature on correctional officers: Identifying new avenues for research. J. Crim. Justice 2019, 60, 84–92. [Google Scholar] [CrossRef]
- Ricciardelli, R. Also Serving Time: Canada’s Provincial and Territorial Correctional Officers; University of Toronto Press: Toronto, ON, Canada, 2019. [Google Scholar]
- Ricciardelli, R. Recognizing Federal Correctional Officers as First Responders and under the Memorial Grant. A Position Paper for the Minister of Public Safety and Emergency Preparedness: The Honourable Ralph Goodale. 7 July 2019. Available online: https://ucco-sacc-csn.ca/assets/uploads/2019/08/08-2019-COs-as-First-Responders_Final.pdf (accessed on 16 September 2021).
- Regehr, C.; Carey, M.; Wagner, S.; Alden, L.; Buys, N.; Corneil, W.; Fyfe, T.; Fraess-Phillips, A.; Krutop, E.; Matthews, L.; et al. Prevalence of PTSD, depression and anxiety disorders in correctional officers: A systematic review. Correct. Policy Pract. Res. 2021, 6, 229–241. [Google Scholar] [CrossRef]
- Norman, M.; Ricciardelli, R. Operational and organisational stressors in community correctional work: Insights from probation and parole officers in Ontario, Canada. Probat. J. 2021, 0264550520984253. [Google Scholar] [CrossRef]
- Lambert, E.; Minor, K.; Wells, J.; Hogan, N. Social support’s relationship to correctional staff job stress, job involvement, job satisfaction, and organizational commitment. Soc. Sci. J. 2016, 53, 22–32. [Google Scholar] [CrossRef]
- Canadian Institute of Public Safety Research and Treatment. Glossary of Terms: Psychologically Traumatic Event. Available online: https://www.cipsrt-icrtsp.ca/en/resources/glossary-of-terms#667 (accessed on 3 September 2021).
- Carleton, R.N.; Afifi, T.O.; Taillieu, T.; Turner, S.; Krakauer, R.; Anderson, G.S.; MacPhee, R.S.; Ricciardelli, R.; Cramm, H.A.; Groll, D.; et al. Exposures to potentially traumatic events among public safety personnel in Canada. Can. J. Behav. Sci. 2019, 51, 37–52. [Google Scholar] [CrossRef]
- Denhof, M.D.; Spinaris, C.G. Prevalence of Trauma-Related Health Conditions in Correctional Officers: A Profile of Michigan Corrections Organization Members. 2016. Available online: https://www.mco-seiu.org/wp-content/uploads/2016/05/MCO-Paper_FINAL.pdf (accessed on 16 September 2021).
- James, L.; Todak, N. Prison employment and post-traumatic stress disorder: Risk and protective factors. Am. J. Ind. Med. 2018, 61, 725–732. [Google Scholar] [CrossRef]
- Carleton, R.N.; Afifi, T.O.; Turner, S.; Taillieu, T.; Duranceau, S.; LeBouthillier, D.M.; Sareen, J.; Ricciardelli, R.; MacPhee, R.S.; Groll, D.; et al. Mental disorder symptoms among public safety personnel. Can. J. Psychiatry 2018, 63, 54–64. [Google Scholar] [CrossRef] [Green Version]
- Carleton, R.N.; Ricciardelli, R.; Taillieu, T.; Mitchell, M.; Andres, E.; Afifi, T.O. Provincial correctional service workers: The prevalence of mental disorders. Int. J. Environ. Res. Public Health 2020, 17, 2203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carleton, R.N.; Afifi, T.O.; Taillieu, T.; Turner, S.; Mason, J.; Ricciardelli, R.; McCreary, D.; Vaughan, A.; Anderson, G.; Krakauer, R.; et al. Assessing the relative impact of diverse stressors among public safety personnel. Int. J. Environ. Res. Public Health 2020, 17, 1234. [Google Scholar] [CrossRef] [Green Version]
- Fusco, N.; Ricciardelli, R.; Jamshidi, L.; Carleton, R.N.; Barnim, N.; Hilton, Z.; Groll, D. When our work hits home: Trauma and mental disorders in correctional officers and other correctional workers. Front. Psychiatry 2021, 11, 493391. [Google Scholar] [CrossRef]
- Jaegers, L.A.; Matthieu, M.M.; Vaughn, M.G.; Werth, P.; Katz, I.M.; Ahmad, S.O. Posttraumatic stress disorder and job burnout among jail officers. J. Occup. Environ. Med. 2019, 61, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Ricciardelli, R.; Groll, D.; Czarnuch, S.; Carleton, R.N.; Cramm, H. Behind the frontlines: Exploring the mental health and help-seeking behaviours of public safety personnel who work to support frontline operations. Annu. Rev. Interdiscip. Justice Res. 2019, 8, 315–348. [Google Scholar]
- Oliphant, R.C. Healthy Minds, Safe Communities: Supporting Our Public Safety Officers through a National Strategy for Operational Stress Injuries; Security, Standing Committee on Public Safety and National Security, Ed.; Standing Committee on Public Safety and National Security: Ottawa, ON, Canada, 2016; Available online: http://www.parl.gc.ca/HousePublications/Publication.aspx?DocId=8457704&Language=E (accessed on 13 August 2021).
- Picard, M. (Chair). National roundtable on post-traumatic stress disorder. In Proceedings of the Standing Committee on Public Safety and National Security (SECU), Regina, SK, Canada, 29 January 2016. [Google Scholar]
- Lambert, E.; Hogan, N. Correctional staff: The issue of job stress. In The Practice of Correctional Psychology; Ternes, M., Magaletta, P., Patry, M., Eds.; Springer: Cham, Switzerland, 2018; pp. 259–281. [Google Scholar] [CrossRef]
- Lambert, E.G.; Hogan, N.L.; Griffin, M.L.; Kelley, T. The correctional staff burnout literature. Crim. Justice Stud. 2015, 28, 397–443. [Google Scholar] [CrossRef]
- Arnold, H. The psychological and emotional effects of prison on prison staff. In The Routledge International Handbook of Forensic Psychology in Secure Settings; Ireland, J., Ireland, C., Fisher, M., Gredecki, N., Eds.; Routledge: London, UK, 2017; pp. 283–299. [Google Scholar]
- Armstrong, G.; Griffin, M. Does the job matter? Comparing correlates of stress among treatment and correctional staff in prisons. J. Crim. Justice 2004, 32, 577–592. [Google Scholar] [CrossRef]
- Dowden, C.; Tellier, C. Predicting work-related stress in correctional officers: A meta- analysis. J. Crim. Justice 2004, 32, 31–47. [Google Scholar] [CrossRef]
- Lambert, E.; Cluse-Tolar, T.; Hogan, N. This job is killing me: The impact of job characteristics on correctional staff job stress. Appl. Psychol. Crim. Justice 2007, 3, 117–142. [Google Scholar]
- Armstrong, G.; Atkin-Plunk, C.; Wells, J. The relationship between work–family conflict, correctional officer job stress, and job satisfaction. Crim. Justice Behav. 2015, 42, 1066–1082. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Lambert, E.G.; Jiang, S.; Zhang, J. A research note on the association between work–family conflict and job stress among Chinese prison staff. Psychol. Crime Law 2017, 23, 633–646. [Google Scholar] [CrossRef]
- Lambert, E.; Qureshi, H.; Frank, J.; Keena, L.; Hogan, N. The relationship of work-family conflict with job stress among Indian police officers: A research note. Police Pract. Res. 2017, 18, 37–48. [Google Scholar] [CrossRef]
- Obidoa, C.; Reeves, D.; Warren, N.; Reisine, S.; Cherniack, M. Depression and work family conflict among corrections officers. J. Occup. Environ. Med. 2011, 53, 1294–1301. [Google Scholar] [CrossRef]
- Lambert, E.; Altheimer, I.; Hogan, N. An exploratory examination of a gendered model of the effects of role stressors. Women Crim. Justice 2010, 20, 193–217. [Google Scholar] [CrossRef]
- Liu, J.; Lambert, I.E.; Kelley, T.; Zhang, J.; Jiang, S. Exploring association between work-family conflict and job involvement. Int. J. Offender Ther. Comp. Criminol. 2020, 64, 791–817. [Google Scholar] [CrossRef]
- Keinan, G.; Malach-Pines, A. Stress and burnout among prison personnel: Sources, outcomes, and intervention strategies. Crim. Justice Behav. 2007, 34, 380–398. [Google Scholar] [CrossRef]
- Paoline, E.; Lambert, E. The issue of control in jail: The effects of professionalism, detainee control, and administrative support on job stress, job satisfaction, and organizational commitment among jail staff. Am. J. Crim. Justice 2012, 37, 179–199. [Google Scholar] [CrossRef]
- Paoline, E.; Lambert, E.; Hogan, N. Job stress and job satisfaction among jail staff: Exploring gendered effects. Women Crim. Justice 2015, 25, 339–359. [Google Scholar] [CrossRef]
- Savicki, V.; Cooley, E.; Gjesvold, J. Harassment as a predictor of job burnout in correctional officers. Crim. Justice Behav. 2003, 30, 602–619. [Google Scholar] [CrossRef]
- Ricciardelli, R.; Carleton, N.; Groll, D.; Cramm, H. Qualitatively unpacking Canadian public safety personnel experiences of trauma and their well-being. Can. J. Criminol. Crim. Justice 2018, 60, 566–577. [Google Scholar] [CrossRef]
- Ricciardelli, R.; Power, N. How “conditions of confinement” impact “conditions of employment”: The work-related well-being of provincial correctional officers in Atlantic Canada. Violence Vict. 2020, 35, 88–107. [Google Scholar] [CrossRef] [PubMed]
- Union of Canadian Correctional Officers. Plus Que Jamais, l’Unité c’Est la Clé! More Than Ever, Unity Is the Key. Vigilance no 4. July 2016. Available online: https://ucco-sacc-csn.ca/assets/uploads/2019/03/UCCO-SACC_Vigilance-SUmmer-2016.pdf (accessed on 16 September 2021).
- Konda, S.; Tiesman, H.; Reichard, A.; Hartley, D.U.S. correctional officers killed or injured on the job. Correct. Today 2013, 75, 122–123. [Google Scholar] [PubMed]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). Scale Available from the National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 16 September 2021).
- Spinaris, C.G.; Denhof, M.D.; Kellaway, J.A. Posttraumatic Stress Disorder in United States Corrections Professionals: Prevalence and Impact on Health and Functioning. 2012. Available online: https://www.ojp.gov/ncjrs/virtual-library/abstracts/posttraumatic-stress-disorder-united-states-corrections (accessed on 16 September 2021).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Bremner, J.D. Does Stress Damage the Brain? Understanding Trauma-Related Disorders from a Mind-Body Perspective; W.W. Norton & Co.: New York, NY, USA, 2002. [Google Scholar]
- Andersen, L.; Hogh, A.; Elklit, A.; Andersen, J.; Biering, K. Work-related threats and violence and post-traumatic symptoms in four high-risk occupations: Short- and long- term symptoms. Int. Arch. Occup. Environ. Health 2019, 92, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Bourbonnais, R.; Jauvin, N.; Dussault, J.; Vézina, M. Psychosocial work environment, interpersonal violence at work and mental health among correctional officers. Int. J. Law Psychiatry 2007, 30, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Kunst, M.; Bogaerts, S.; Winkel, F.W. Peer and inmate aggression, type D-personality and posttraumatic stress among Dutch prison workers. Stress Health 2009, 25, 387–395. [Google Scholar] [CrossRef]
- Kunst, M. Working in prisons: A critical review of stress in the occupation of correctional officers. In Handbook of Stress in the Occupations; Lnagan-Fox, J., Cooper, C., Eds.; Edward Elgar Publishing: Cheltenham, UK, 2011; pp. 241–283. [Google Scholar]
- Bezerra, C.; Assis, S.; Constantino, P. Psychological distress and work stress in correctional officers: A literature review. Ciência & Saúde Coletiva 2016, 21, 2135–2146. [Google Scholar]
- Neveu, J. Jailed resources: Conservation of resources theory as applied to burnout among prison guards. J. Organ. Behav. 2007, 28, 21–42. [Google Scholar] [CrossRef]
- Boudoukha, A.; Hautekeete, M.; Abdelaoui, S.; Groux, W.; Garay, D. Burnout et victimisations: Effets des agressions des personnes détenues envers les personnels de surveillance. L’Encéphale 2011, 37, 284–292. [Google Scholar] [CrossRef]
- Griffin, M.; Hogan, N.; Lambert, E. Doing “People Work” in the prison setting: An examination of the job characteristics model and correctional staff burnout. Crim. Justice Behav. 2012, 39, 1131–1147. [Google Scholar] [CrossRef]
- Public Safety Canada. Post-Traumatic Stress Injuries and Support for Public Safety Officers. 2018. Available online: https://www.publicsafety.gc.ca/cnt/mrgnc-mngmnt/mrgnc-prprdnss/ptsi-en.aspx (accessed on 16 September 2021).
- Silliker, A. Correctional Officers Calling for Presumptive PTSD Coverage across Canada. Canadian Occupational Safety, pp. 14–17. February/March 2018. Available online: https://www.cos-mag.com/psychological-health-safety/35965-correctional-officers-calling-for-presumptive-ptsd-coverage-across-canada/ (accessed on 16 September 2021).
- McCreary, D.R.; Thompson, M.M. Development of two reliable and valid measures of stressors in policing: The operational and organizational police stress questionnaires. Int. J. Stress Manag. 2006, 13, 494–518. [Google Scholar] [CrossRef]
- Ashbaugh, A.R.; Houle-Johnson, S.; Herbert, C.; El-Hage, W.; Brunet, A. Psychometric validation of the English and French versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PLoS ONE 2016, 11, e0161645. [Google Scholar] [CrossRef] [PubMed]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef]
- MacIntosh, H.B.; Séguin, G.; Abdul-Ramen, I.; Randy, M. Première Traduction Française PCL-5-LEC, Civilian Checklist for PTSD, DSM5; McGill: Montreal, QC, Canada, 2015. [Google Scholar]
- Beard, C.; Bjorgvinsson, T. Beyond generalized anxiety disorder: Psychometric properties of the GAD-7 in a heterogeneous psychiatric sample. J. Anxiety Disord. 2014, 28, 547–552. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Lowe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Lowe, B.; Unutzer, J.; Callahan, C.M.; Perkins, A.J.; Kroenke, K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med. Care 2004, 42, 1194–1201. [Google Scholar] [CrossRef]
- Manea, L.; Gilbody, S.; McMillan, D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen. Hosp. Psychiatry 2015, 37, 67–75. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swinson, R.P. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evid. Based Med. 2006, 11, 184. [Google Scholar] [CrossRef] [Green Version]
- Furukawa, T.A.; Katherine Shear, M.; Barlow, D.; Gorman, J.M.; Woods, S.W.; Money, R.; Etschel, E.; Engel, R.R.; Leucht, S. Evidence-based guidelines for interpretation of the Panic Disorder Severity Scale. Depress. Anxiety 2009, 26, 922–929. [Google Scholar] [CrossRef] [Green Version]
- Shear, M.K.; Brown, T.A.; Barlow, D.H.; Money, R.; Sholomskas, D.E.; Woods, S.W.; Gorman, J.M.; Papp, L.A. Multicenter collaborative Panic Disorder Severity Scale. Am. J. Psychiatry 1997, 154, 1571–1575. [Google Scholar] [CrossRef]
- Shear, M.K.; Rucci, P.; Williams, J.; Frank, E.; Grochocinski, V.; Vander Bilt, J.; Houck, P.; Wang, T. Reliability and validity of the Panic Disorder Severity Scale: Replication and extension. J. Psychiatr. Res. 2001, 35, 293–296. [Google Scholar] [CrossRef]
- Gache, P.; Michaud, P.; Landry, U.; Accietto, C.; Arfaoui, S.; Wenger, O.; Daeppen, J.B. The Alcohol Use Disorders Identification Test (AUDIT) as a screening tool for excessive drinking in primary care: Reliability and validity of a French version. Alcohol. Clin. Exp. Res. 2005, 29, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; Delafuente, J.R.; Grant, M. Development of the Alcohol-Use Disorders Identification Test (Audit)—WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol-Consumption 2. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Cullen, F.; Link, B.; Wolfe, N.; Frank, J. The social dimensions of correctional officer stress. Justice Q. 1985, 2, 505–533. [Google Scholar] [CrossRef]
- Paoline, E.; Lambert, H.; Hogan, N. A calm and happy keeper of the keys: The impact of ACA views, relations with coworkers, and policy views on the job stress and job satisfaction of correctional staff. Prison J. 2006, 86, 182–205. [Google Scholar] [CrossRef]
- Ricciardelli, R.; Czarnuch, S.; Carleton, R.N.; Gacek, J.; Shewmake, J. Canadian public safety personnel and occupational stressors: How PSP interpret stressors on duty. Int. J. Environ. Res. Public Health 2020, 17, 4736. [Google Scholar] [CrossRef] [PubMed]
- Regehr, C.; Goldberg, G.; Glancy, G.D.; Knott, T. Posttraumatic symptoms and disability in paramedics. Can. J. Psychiatry Revue Canadienne de Psychiatrie 2002, 47, 953–958. [Google Scholar] [CrossRef] [PubMed]
- Turner, R.J.; Brown, R.L. Social support and mental health. In A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems, 2nd ed.; Scheid, T.L., Brown, T.N., Eds.; Cambridge University Press: Cambridge, UK, 2009; pp. 200–212. [Google Scholar]
- Denhof, M.D.; Spinaris, C.G.; Morton, G.R. Occupational Stressors in Corrections Organizations: Types, Effects and Solutions; National Institute of Corrections: Washington, DC, USA, 2014. Available online: https://info.nicic.gov/nicrp/system/files/028299.pdf (accessed on 13 August 2021).
- Ferdik, F.; Smith, H. Correctional Officer Safety and Wellness Literature Synthesis; National Institute of Justice: Washington, DC, USA, 2017. Available online: https://www.ncjrs.gov/pdffiles1/nij/250484.pdf (accessed on 13 August 2021).
| Occupational Stressor | Total | Wellness a | Training b | Governance c | Correctional Officers d | Probation/Parole Officers e | Administration f | F-Statistic | Significant Differences between Occupational Categories |
|---|---|---|---|---|---|---|---|---|---|
| Mean (SE) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Organizational Stressors (PSP-Org) | |||||||||
| Dealing with co-workers | 4.40 (0.06) | 4.63 (0.20) | 4.34 (0.35) | 4.94 (0.17) | 4.36 (0.08) | 4.17 (0.15) | 4.39 (0.43) | 2.29 * | e < c |
| The feeling that different rules apply to different people (e.g., favouritism) | 4.61 (0.06) | 4.75 (0.24) | 4.38 (0.36) | 4.85 (0.20) | 4.68 (0.08) | 4.20 (0.16) | 4.68 (0.43) | 2.00 | No significant differences |
| Feeling like you always have to prove yourself to the organization | 4.08 (0.07) | 3.66 (0.23) | 3.88 (0.36) | 4.55 (0.23) | 4.04 (0.09) | 4.20 (0.16) | 1.04 (0.41) | 1.81 | No significant differences |
| Excessive administrative duties | 3.48 (0.07) | 3.66 (0.23) | 3.47 (0.36) | 4.45 (0.21) | 2.83 (0.08) | 5.07 (0.15) | 3.54 (0.44) | 40.82 *** | a < d a, b, d, f < e |
| Constant change in policy/legislation | 4.45 (0.07) | 3.59 (0.21) | 3.25 (0.33) | 4.78 (0.20) | 4.54 (0.08) | 4.81 (0.15) | 3.57 (0.35) | 8.69 *** | a, b < c, d, e f < e |
| Staff shortages | 4.89 (0.07) | 5.00 (0.24) | 4.13 (0.39) | 5.20 (0.20) | 4.79 (0.09) | 5.20 (0.15) | 4.61 (0.38) | 2.54 * | No significant differences |
| Bureaucratic red tape | 4.66 (0.07) | 4.14 (0.26) | 3.81 (0.40) | 5.06 (0.18) | 4.66 (0.09) | 4.99 (0.15) | 4.25 (0.38) | 3.84 ** | a < e b < c, e |
| Too much computer work | 3.00 (0.07) | 2.81 (0.21) | 3.00 (0.32) | 3.94 (0.21) | 2.28 (0.07) | 4.99 (0.16) | 3.04 (0.41) | 65.79 *** | a, b, c, d, f < e a, d < c |
| Lack of training on new equipment | 3.42 (0.07) | 2.75 (0.21) | 2.81 (0.39) | 2.56 (0.22) | 3.70 (0.09) | 2.91 (0.15) | 3.04 (0.35) | 6.89 *** | a, e < c |
| Perceived pressure to volunteer free time | 2.12 (0.06) | 1.85 (0.18) | 1.97 (0.32) | 2.52 (0.21) | 2.05 (0.07) | 2.27 (0.14) | 2.32 (0.36) | 1.99 | No significant differences |
| Dealing with supervisors | 4.06 (0.07) | 3.45 (0.23) | 3.13 (0.37) | 4.16 (0.22) | 4.29 (0.09) | 3.78 (0.15) | 3.89 (0.43) | 5.03 *** | a, b < d |
| Inconsistent leadership style | 4.76 (0.07) | 4.13 (0.26) | 4.09 (0.40) | 4.68 (0.22) | 5.14 (0.08) | 4.04 (0.16) | 4.21 (0.48) | 10.48 *** | a, e < d |
| Lack of resources | 4.52 (0.07) | 4.36 (0.25) | 4.16 (0.35) | 4.48 (0.22) | 4.64 (0.09) | 4.41 (0.17) | 3.79 (0.41) | 1.56 | No significant differences |
| Unequal sharing of work responsibilities | 4.26 (0.07) | 4.49 (0.25) | 3.81 (0.43) | 4.23 (0.21) | 4.36 (0.09) | 3.99 (0.17) | 3.93 (0.49) | 1.39 | No significant differences |
| If you are sick or injured your co-workers seem to look down on you | 3.09 (0.07) | 2.71 (0.25) | 2.13 (0.29) | 3.23 (0.24) | 3.29 (0.10) | 2.71 (0.15) | 2.93 (0.46) | 3.65 ** | b < d |
| Leaders over-emphasize the negatives (e.g., supervisor evaluations, public complaints) | 3.95 (0.07) | 3.01 (0.24) | 2.63 (0.38) | 4.16 (0.23) | 4.18 (0.10) | 3.85 (0.18) | 3.54 (0.51) | 6.67 *** | a, b < c, d |
| Internal investigations | 3.52 (0.08) | 3.14 (0.28) | 2.50 (0.34) | 3.77 (0.23) | 3.90 (0.11) | 2.74 (0.17) | 2.25 (0.34) | 9.94 *** | b, e, f < d e, f < c |
| Dealing with the court system | 2.56 (0.06) | 2.34 (0.19) | 2.09 (0.30) | 2.61 (0.18) | 2.27 (0.07) | 3.69 (0.14) | 2.64 (0.39) | 17.75 *** | a, b, c, d, f < e |
| The need to be accountable for doing your job | 3.91 (0.07) | 3.37 (0.24) | 3.03 (0.37) | 4.05 (0.20) | 3.85 (0.09) | 4.51 (0.16) | 3.71 (0.47) | 5.18 *** | a, b, d < e |
| Inadequate equipment | 3.65 (0.07) | 3.51 (0.26) | 2.97 (0.37) | 3.61 (0.24) | 3.96 (0.09) | 3.04 (0.17) | 2.50 (0.34) | 7.75 *** | e, f < d |
| Total Mean Organizational Stress Score, mean (SD) | 3.87 (0.04) | 3.59 (0.14) | 3.28 (0.23) | 4.14 (0.15) | 3.89 (0.06) | 3.99 (0.10) | 3.54 (0.31) | 3.34 ** | b < c |
| Operational Stressors (PSP-Op) | |||||||||
| Shift work | 3.36 (0.08) | 2.49 (0.26) | 1.34 (0.20) | 3.29 (0.25) | 4.42 (0.09) | 1.09 (0.05) | 1.21 (0.15) | 93.96 *** | a < d, e, f c < d b, e, f < c, d |
| Working alone at night | 2.23 (0.07) | 2.14 (0.26) | 1.00 (0.0) | 2.23 (0.22) | 2.68 (0.09) | 1.24 (0.07) | 1.00 (0.00) | 20.26 *** | b, e < a, c, d f < c, d |
| Over-time demands | 2.51 (0.06) | 2.23 (0.21) | 1.19 (0.11) | 3.44 (0.25) | 2.66 (0.08) | 2.05 (0.14) | 1.68 (0.24) | 11.30 *** | a, b, d, e, f < c b < c, d e < d |
| Risk of being injured on the job | 3.73 (0.07) | 2.64 (0.19) | 2.53 (0.33) | 3.20 (0.21) | 4.56 (0.08) | 2.40 (0.13) | 1.75 (0.26) | 54.50 | a, b, c, e, f < d c < e, f |
| Work-related activities on days off (e.g., court, community events) | 2.00 (0.05) | 1.53 (0.13) | 1.34 (0.16) | 2.09 (0.17) | 2.11 (0.07) | 2.04 (0.13) | 1.57 (0.25) | 3.67 ** | a < d |
| Traumatic events (e.g., motor vehicle accidents, domestics, death, injury) | 2.82 (0.07) | 2.21 (0.21) | 1.94 (0.24) | 2.87 (0.20) | 3.02 (0.09) | 2.72 (0.15) | 2.07 (0.34) | 4.79 *** | a, b < d |
| Managing your social life outside of work | 3.28 (0.06) | 2.58 (0.19) | 2.50 (0.31) | 3.29 (0.21) | 3.62 (0.08) | 2.77 (0.14) | 2.64 (0.34) | 9.67 *** | a, b, e < d |
| Not enough time available to spend with friends and family | 3.93 (0.07) | 3.04 (0.25) | 3.47 (0.41) | 4.01 (0.24) | 4.39 (0.09) | 3.03 (0.16) | 3.00 (0.39) | 15.64 *** | a, e < c, d f < d |
| Paperwork | 3.41 (0.07) | 3.51 (0.25) | 2.78 (0.33) | 4.09 (0.20) | 2.86 (0.08) | 5.03 (0.16) | 3.07 (0.39) | 35.58 *** | a, b, d, d, f < e b, d < c |
| Eating healthy at work | 3.78 (0.07) | 3.21 (0.22) | 3.53 (0.37) | 3.94 (0.21) | 3.97 (0.09) | 3.48 (0.16) | 3.39 (0.40) | 3.40 ** | a < d |
| Finding time to stay in good physical condition | 4.39 (0.07) | 3.90 (0.23) | 4.13 (0.39) | 4.66 (0.20) | 4.49 (0.08) | 4.23 (0.16) | 4.14 (0.36) | 1.96 | No significant differences |
| Fatigue (e.g., shift work, over-time) | 4.24 (0.07) | 3.44 (0.23) | 2.47 (0.34) | 4.34 (0.24) | 4.82 (0.09) | 3.27 (0.18) | 2.79 (0.42) | 25.76 *** | a < d b, e, f < c, d |
| Occupation-related health issues (e.g., back pain) | 3.95 (0.07) | 3.67 (0.27) | 2.78 (0.33) | 3.93 (0.23) | 4.13 (0.09) | 3.83 (0.17) | 3.36 (0.39) | 3.55 ** | b < d |
| Lack of understanding from family and friends about your work | 3.72 (0.07) | 2.55 (0.22) | 2.75 (0.37) | 3.55 (0.23) | 4.12 (0.09) | 3.46 (0.16) | 2.64 (0.38) | 12.81 *** | a < c, e a, b, e, f < d |
| Making friends outside the job | 3.01 (0.07) | 2.21 (0.21) | 2.38 (0.34) | 2.93 (0.22) | 3.37 (0.09) | 2.46 (0.15) | 2.75 (0.39) | 8.35 *** | a, e < d |
| Upholding a “higher image” in public | 2.92 (0.07) | 1.97 (0.18) | 2.28 (0.31) | 2.86 (0.20) | 3.20 (0.09) | 2.72 (0.16) | 2.50 (0.39) | 6.54 *** | a < d |
| Negative comments from the public | 3.43 (0.07) | 2.21 (0.19) | 2.47 (0.34) | 3.33 (0.22) | 3.87 (0.10) | 3.01 (0.16) | 2.18 (0.36) | 14.37 *** | a, b < c a, e, f < d |
| Limitations to your social life (e.g., who your friends are, where you socialize) | 3.21 (0.07) | 2.07 (0.18) | 2.31 (0.31) | 2.96 (0.20) | 3.57 (0.09) | 2.96 (0.16) | 2.86 (0.41) | 10.48 *** | a < e a, b, e < d |
| Feeling like you are always on the job | 3.33 (0.07) | 2.14 (0.20) | 2.22 (0.31) | 3.55 (0.22) | 3.63 (0.09) | 3.21 (0.17) | 2.25 (0.35) | 11.17 *** | a < c, e b < c a, b, e, f < d |
| Friends/family feel the effects of the stigma associated with your job | 3.10 (0.07) | 1.77 (0.15) | 2.56 (0.35) | 3.24 (0.20) | 3.50 (0.09) | 2.61 (0.15) | 2.36 (0.38) | 14.82 *** | a < c, d, e e, f < d |
| Total Mean Operational Stress Score, mean (SD) | 3.31 (0.05) | 2.60 (0.13) | 2.40 (0.19) | 3.37 (0.15) | 3.64 (0.06) | 2.89 (0.10) | 2.46 (0.23) | 19.17 *** | a, b, f < c a, b, e, f < d |
| Other Stressors | |||||||||
| Concern over job performance | 3.55 (0.07) | 2.88 (0.20) | 3.09 (0.39) | 3.79 (0.22) | 3.52 (0.09) | 4.12 (0.16) | 2.71 (0.42) | 5.88 *** | a, d, f < e |
| Communication across departments/ branches | 3.62 (0.07) | 3.30 (0.23) | 3.34 (0.40) | 4.09 (0.1) | 3.69 (0.09) | 3.42 (0.16) | 3.32 (0.42) | 1.82 | No significant differences |
| Working in close contact with the inmate/client population | 3.43 (0.07) | 2.75 (0.21) | 2.47 (0.29) | 2.83 (0.21) | 3.78 (0.09) | 3.40 (0.15) | 1.86 (0.29) | 11.36 *** | a, b, c, f < d f < e |
| Total Mean Other Stressors Score, mean (SD) | 3.53 (0.05) | 2.98 (0.15) | 2.97 (0.31) | 3.57 (0.16) | 3.66 (0.07) | 3.65 (0.12) | 2.63 (0.33) | 5.17 *** | a, f < d f < e |
| Occupational Stressor | PTSD a | Major Depressive Disorder | Generalized Anxiety | Panic Disorder | Alcohol Use Disorder b | Any Mental Disorder |
|---|---|---|---|---|---|---|
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Organizational Stressors | ||||||
| Dealing with co-workers | 1.37 *** (1.22, 1.54) | 1.58 *** (1.41, 1.77) | 1.55 *** (1.38, 1.74) | 1.51 *** (1.29, 1.77) | 1.27 * (1.04, 1.56) | 1.48 *** (1.33, 1.65) |
| The feeling that different rules apply to different people (e.g., favouritism) | 1.37 *** (1.22, 1.53) | 1.53 *** (1.38, 1.71) | 1.47 *** (1.31, 1.64) | 1.49 *** (1.26, 1.75) | 1.21 (0.997, 1.48) | 1.44 *** (1.30, 1.59) |
| Feeling like you always have to prove yourself to the organization | 1.49 *** (1.25, 1.54) | 1.42 *** (1.29, 1.57) | 1.46 *** (1.32, 1.62) | 1.48 *** (1.29, 1.71) | 1.12 (0.94, 1.33) | 1.48 *** (1.34, 1.64) |
| Excessive administrative duties | 1.30 *** (1.17, 1.45) | 1.48 *** (1.33, 1.64) | 1.40 *** (1.26, 1.56) | 1.51 *** (1.31, 1.75) | 1.17 (0.99, 1.39) | 1.48 *** (1.33, 1.65) |
| Constant change in policy/legislation | 1.41 *** (1.26, 1.58) | 1.50 *** (1.35, 1.67) | 1.53 *** (1.37, 1.71) | 1.49 *** (1.28, 1.75) | 1.28 * (1.06, 1.56) | 1.55 *** (1.40, 1.72) |
| Staff shortages | 1.33 *** (1.19, 1.50) | 1.38 *** (1.24, 1.54) | 1.35 *** (1.21, 1.50) | 1.34 *** (1.14, 1.57) | 1.14 (0.94, 1.39) | 1.39 *** (1.26, 1.54) |
| Bureaucratic red tape | 1.37 *** (1.22, 1.53) | 1.39 *** (1.26, 1.54) | 1.42 *** (1.28, 1.58) | 1.30 *** (1.13, 1.50) | 1.13 (0.94, 1.36) | 1.44 *** (1.31, 1.59) |
| Too much computer work | 1.15 * (1.03, 1.28) | 1.33 *** (1.19, 1.48) | 1.27 *** (1.14, 1.41) | 1.23 *** (1.07, 1.42) | 1.21 * (1.02, 1.44) | 1.27 *** (1.14, 1.42) |
| Lack of training on new equipment | 1.25 *** (1.14, 1.38) | 1.31 *** (1.20, 1.43) | 1.47 *** (1.33, 1.63) | 1.24 *** (1.09, 1.41) | 1.09 (0.91, 1.27) | 1.40 *** (1.27, 1.54) |
| Perceived pressure to volunteer free time | 1.25 *** (1.12, 1.39) | 1.26 *** (1.14, 1.40) | 1.24 *** (1.12, 1.37) | 1.21 *** (1.07, 1.38) | 1.01 (0.84, 1.21) | 1.25 *** (1.12, 1.40) |
| Dealing with supervisors | 1.39 *** (1.24, 1.55) | 1.54 *** (1.38, 1.71) | 1.50 *** (1.34, 1.68) | 1.50 *** (1.29, 1.75) | 1.14 (0.95, 1.36) | 1.52 *** (1.37, 1.69) |
| Inconsistent leadership style | 1.34 *** (1.20, 1.50) | 1.48 *** (1.33, 1.65) | 1.42 *** (1.27, 1.58) | 1.44 *** (1.22, 1.69) | 1.17 (0.96, 1.41) | 1.48 *** (1.34, 1.63) |
| Lack of resources | 1.41 *** (1.26, 1.57) | 1.40 *** (1.27, 1.55) | 1.40 *** (1.26, 1.55) | 1.31 *** (1.14, 1.52) | 1.13 (0.94, 1.35) | 1.55 *** (1.40, 1.71) |
| Unequal sharing of work responsibilities | 1.29 *** (1.17, 1.43) | 1.43 *** (1.30, 1.57) | 1.41 *** (1.28, 1.56) | 1.30 *** (1.14, 1.49) | 1.25 * (1.05, 1.49) | 1.44 *** (1.31, 1.58) |
| If you are sick or injured your co-workers seem to look down on you | 1.28 *** (1.18, 1.40) | 1.43 *** (1.32, 1.56) | 1.38 *** (1.26, 1.50) | 1.62 *** (1.43, 1.85) | 1.25 ** (1.08, 1.45) | 1.46 *** (1.33, 1.60) |
| Leaders over-emphasize the negatives (e.g., supervisor evaluations, public complaints) | 1.38 *** (1.26, 1.52) | 1.45 *** (1.33, 1.59) | 1.41 *** (1.29, 1.54) | 1.37 *** (1.20, 1.56) | 1.13 (0.96, 1.32) | 1.48 *** (1.35, 1.61) |
| Internal investigations | 1.31 *** (1.20, 1.42) | 1.28 *** (1.18, 1.38) | 1.22 *** (1.12, 1.32) | 1.24 *** (1.11, 1.38) | 1.12 (0.97, 1.29) | 1.28 *** (1.18, 1.39) |
| Dealing with the court system | 1.24 *** (1.12, 1.38) | 1.38 *** (1.25, 1.53) | 1.28 *** (1.15, 1.41) | 1.39 *** (1.22, 1.59) | 1.15 (0.97, 1.37) | 1.32 *** (1.19, 1.47) |
| The need to be accountable for doing your job | 1.33 *** (1.20, 1.47) | 1.35 *** (1.23, 1.48) | 1.36 *** (1.23, 1.49) | 1.39 *** (1.21, 1.59) | 1.03 (0.87, 1.21) | 1.37 *** (1.24, 1.50) |
| Inadequate equipment | 1.27 *** (1.16, 1.40) | 1.33 *** (1.22, 1.45) | 1.27 *** (1.16, 1.39) | 1.24 *** (1.10, 1.40) | 1.05 (0.90, 1.23) | 1.39 *** (1.27, 1.53) |
| Total Mean Organizational Stress Score | 2.10 *** (1.75, 2.53) | 2.63 *** (2.17, 3.19) | 2.54 *** (2.08, 3.09) | 2.51 *** (1.92, 3.28) | 1.45 * (1.08, 1.93) | 2.62 *** (2.17, 3.15) |
| Operational Stressors (PSP-Op) | ||||||
| Shift work | 1.27 *** (1.15, 1.41) | 1.28 *** (1.16, 1.41) | 1.37 *** (1.24, 1.53) | 1.33 *** (1.16, 1.52) | 1.17 * (1.01, 1.36) | 1.38 *** (1.25, 1.53) |
| Working alone at night | 1.25 *** (1.13, 1.38) | 1.21 *** (1.10, 1.33) | 1.23 *** (1.12, 1.35) | 1.23 *** (1.09, 1.38) | 1.06 (0.90, 1.24) | 1.27 *** (1.15, 1.41) |
| Over-time demands | 1.17 *** (1.06, 1.29) | 1.32 *** (1.20, 1.45) | 1.30 *** (1.18, 1.42) | 1.18 *** (1.05, 1.33) | 1.20 * (1.03, 1.40) | 1.37 *** (1.23, 1.51) |
| Risk of being injured on the job | 1.37 *** (1.23, 1.53) | 1.39 *** (1.25, 1.53) | 1.49 *** (1.34, 1.66) | 1.51 *** (1.31, 1.75) | 1.24 * (1.04, 1.48) | 1.46 *** (1.32, 1.63) |
| Work-related activities on days off (e.g., court, community events) | 1.30 *** (1.16, 1.46) | 1.33 *** (1.19, 1.48) | 1.39 *** (1.24, 1.55) | 1.43 *** (1.25, 1.64) | 1.09 (0.90, 1.32) | 1.35 *** (1.19, 1.53) |
| Traumatic events (e.g., motor vehicle accidents, domestics, death, injury) | 1.32 *** (1.20, 1.46) | 1.33 *** (1.22, 1.46) | 1.45 *** (1.32, 1.59) | 1.51 *** (1.33, 1.71) | 1.19 * (1.01, 1.40) | 1.48 *** (1.33, 1.64) |
| Managing your social life outside of work | 1.46 *** (1.31, 1.64) | 1.86 *** (1.65, 2.10) | 2.00 *** (1.76, 2.28) | 1.76 *** (1.50, 2.06) | 1.40 *** (1.17, 1.68) | 1.80 *** (1.60, 2.04) |
| Not enough time available to spend with friends and family | 1.36 *** (1.23, 1.51) | 1.49 *** (1.36, 1.65) | 1.64 *** (1.47, 1.82) | 1.46 *** (1.27, 1.67) | 1.27 ** (1.07, 1.50) | 1.65 *** (1.49, 1.83) |
| Paperwork | 1.21 *** (1.09, 1.34) | 1.34 *** (1.21, 1.47) | 1.34 *** (1.21, 1.48) | 1.23 *** (1.08, 1.40) | 1.23 * (1.04, 1.44) | 1.32 *** (1.20, 1.46) |
| Eating healthy at work | 1.36 *** (1.23, 1.50) | 1.58 *** (1.42, 1.75) | 1.45 *** (1.31, 1.61) | 1.42 *** (1.24, 1.63) | 1.28 ** (1.08, 1.53) | 1.49 *** (1.34, 1.64) |
| Finding time to stay in good physical condition | 1.41 *** (1.26, 1.57) | 1.61 *** (1.44, 1.80) | 1.62 *** (1.44, 1.81) | 1.53 *** (1.30, 1.80) | 1.22 * (1.01, 1.47) | 1.54 *** (1.39, 1.71) |
| Fatigue (e.g., shift work, over-time) | 1.39 *** (1.25, 1.54) | 1.62 *** (1.46, 1.80) | 1.59 *** (1.43, 1.78) | 1.40 *** (1.22, 1.62) | 1.34 ** (1.11, 1.61) | 1.58 *** (1.42, 1.75) |
| Occupation-related health issues (e.g., back pain) | 1.43 *** (1.30, 1.59) | 1.47 *** (1.34, 1.61) | 1.53 *** (1.39, 1.69) | 1.56 *** (1.35, 1.79) | 1.22 * (1.03, 1.44) | 1.58 *** (1.43, 1.74) |
| Lack of understanding from family and friends about your work | 1.48 *** (1.33, 1.64) | 1.54 *** (1.40, 1.70) | 1.55 *** (1.40, 1.71) | 1.53 *** (1.33, 1.76) | 1.51 *** (1.26, 1.82) | 1.67 *** (1.51, 1.85) |
| Making friends outside the job | 1.49 *** (1.35, 1.65) | 1.62 *** (1.47, 1.79) | 1.61 *** (1.46, 1.77) | 1.65 *** (1.44, 1.90) | 1.38 *** (1.18, 1.61) | 1.68 *** (1.51, 1.87) |
| Upholding a “higher image” in public | 1.41 *** (1.28, 1.55) | 1.40 *** (1.28, 1.53) | 1.37 *** (1.25, 1.50) | 1.46 *** (1.29, 1.66) | 1.21 * (1.03, 1.41) | 1.50 *** (1.35, 1.66) |
| Negative comments from the public | 1.35 *** (1.23, 1.48) | 1.37 *** (1.26, 1.49) | 1.42 *** (1.29, 1.55) | 1.50 *** (1.32, 1.71) | 1.12 (0.96, 1.30) | 1.36 *** (1.24, 1.48) |
| Limitations to your social life (e.g., who your friends are, where you socialize) | 1.43 *** (1.29, 1.58) | 1.58 *** (1.43, 1.74) | 1.62 *** (1.46, 1.79) | 1.58 *** (1.37, 1.82) | 1.45 *** (1.21, 1.72) | 1.64 *** (1.48, 1.83) |
| Feeling like you are always on the job | 1.44 *** (1.30, 1.59) | 1.43 *** (1.30, 1.56) | 1.54 *** (1.40, 1.70) | 1.54 *** (1.35, 1.75) | 1.30 *** (1.11, 1.53) | 1.55 *** (1.40, 1.71) |
| Friends/family feel the effects of the stigma associated with your job | 1.52 *** (1.37, 1.69) | 1.55 *** (1.41, 1.71) | 1.68 *** (1.51, 1.87) | 1.56 *** (1.35, 1.79) | 1.42 *** (1.19, 1.68) | 1.65 *** (1.49, 1.84) |
| Total Mean Operational Stress Score | 2.23 *** (1.86, 2.68) | 2.71 *** (2.25, 3.27) | 2.98 *** (2.43, 3.65) | 2.72 *** (2.12, 3.49) | 1.75 *** (1.34, 2.29) | 3.10 *** (2.53, 3.81) |
| Other Stressors | ||||||
| Concern over job performance | 1.44 *** (1.30, 1.60) | 1.63 *** (1.47, 1.81) | 1.58 *** (1.43, 1.75) | 1.64 *** (1.42, 1.90) | 1.16 (0.98, 1.37) | 1.59 *** (1.44, 1.76) |
| Communication across departments/branches | 1.26 *** (1.14, 1.38) | 1.32 *** (1.21, 1.44) | 1.40 *** (1.27, 1.53) | 1.30 *** (1.15, 1.46) | 1.17 * (1.001, 1.38) | 1.35 *** (1.24, 1.48) |
| Working in close contact with the inmate/client population | 1.37 *** (1.24, 1.52) | 1.38 *** (1.25,1.51) | 1.47 *** (1.33, 1.63) | 1.51 *** (1.32, 1.73) | 1.13 (0.96, 1.34) | 1.41 *** (1.28, 1.55) |
| Total Mean Other Stressors Score | 1.65 *** (1.45, 1.89) | 1.84 *** (1.61, 2.09) | 1.96 *** (1.71, 2.26) | 1.91 *** (1.59, 2.30) | 1.28 * (1.03, 1.59) | 1.87 *** (1.63, 2.14) |
| PTSD a | Major Depressive Disorder | Generalized Anxiety | Panic Disorder | Alcohol Use Disorder b | Any Mental Disorder | |
|---|---|---|---|---|---|---|
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Model 1 | ||||||
| Total Number of Traumatic Exposures | 1.17 *** (1.11, 1.23) | 1.09 *** (1.05, 1.14) | 1.07 ** (1.03, 1.12) | 1.10 ** (1.04, 1.18) | 1.00 (0.93, 1.09) | 1.09 *** (1.04, 1.13) |
| Model 2 | ||||||
| Mean Organizational Stress Score | 1.40 ** (1.10, 1.79) | 1.49 *** (1.18, 1.88) | 1.20 (0.93, 1.54) | 1.14 (0.79, 1.65) | 1.02 (0.67, 1.53) | 1.42 ** (1.13, 1.79) |
| Mean Operational Stress Score | 1.84 *** (1.46, 2.34) | 2.14 *** (1.71, 2.69) | 2.27 *** (1.79, 2.89) | 2.08 *** (1.49, 2.89) | 1.77 ** (1.22, 2.58) | 2.43 *** (1.91, 3.09) |
| Mean Other Stressors Score | 1.05 (0.88, 1.25) | 1.01 (0.85, 1.19) | 1.13 (0.95, 1.35) | 1.17 (0.92, 1.48) | 0.84 (0.64, 1.12) | 0.99 (0.83, 1.18) |
| Model 3 | ||||||
| Total Number of Traumatic Exposures | 1.11 *** (1.04, 1.17) | 1.00 (0.95, 1.05) | 0.97 (0.92, 1.03) | 1.01 (0.94, 1.09) | 0.94 (0.86, 1.02) | 1.00 (0.95, 1.05) |
| Mean Organizational Stress Score | 1.34 * (1.03, 1.76) | 1.64 *** (1.26, 2.12) | 1.29 (0.92, 1.03) | 1.29 (0.86, 1.95) | 0.93 (0.58, 1.50) | 1.55 *** (1.20, 2.00) |
| Mean Operational Stress Score | 1.74 *** (1.34, 2.26) | 1.93 *** (1.51, 2.48) | 2.24 *** (1.71, 2.92) | 2.00 *** (1.39, 2.89) | 1.99 ** (1.29, 3.05) | 2.37 *** (1.81, 3.12) |
| Mean Other Stressors Score | 1.07 (0.88, 1.30) | 1.06 (0.88, 1.28) | 1.20 (0.98, 1.46) | 1.21 (0.92, 1.59) | 0.90 (0.65, 1.24) | 0.99 (0.81, 1.21) |
| Model 4 | ||||||
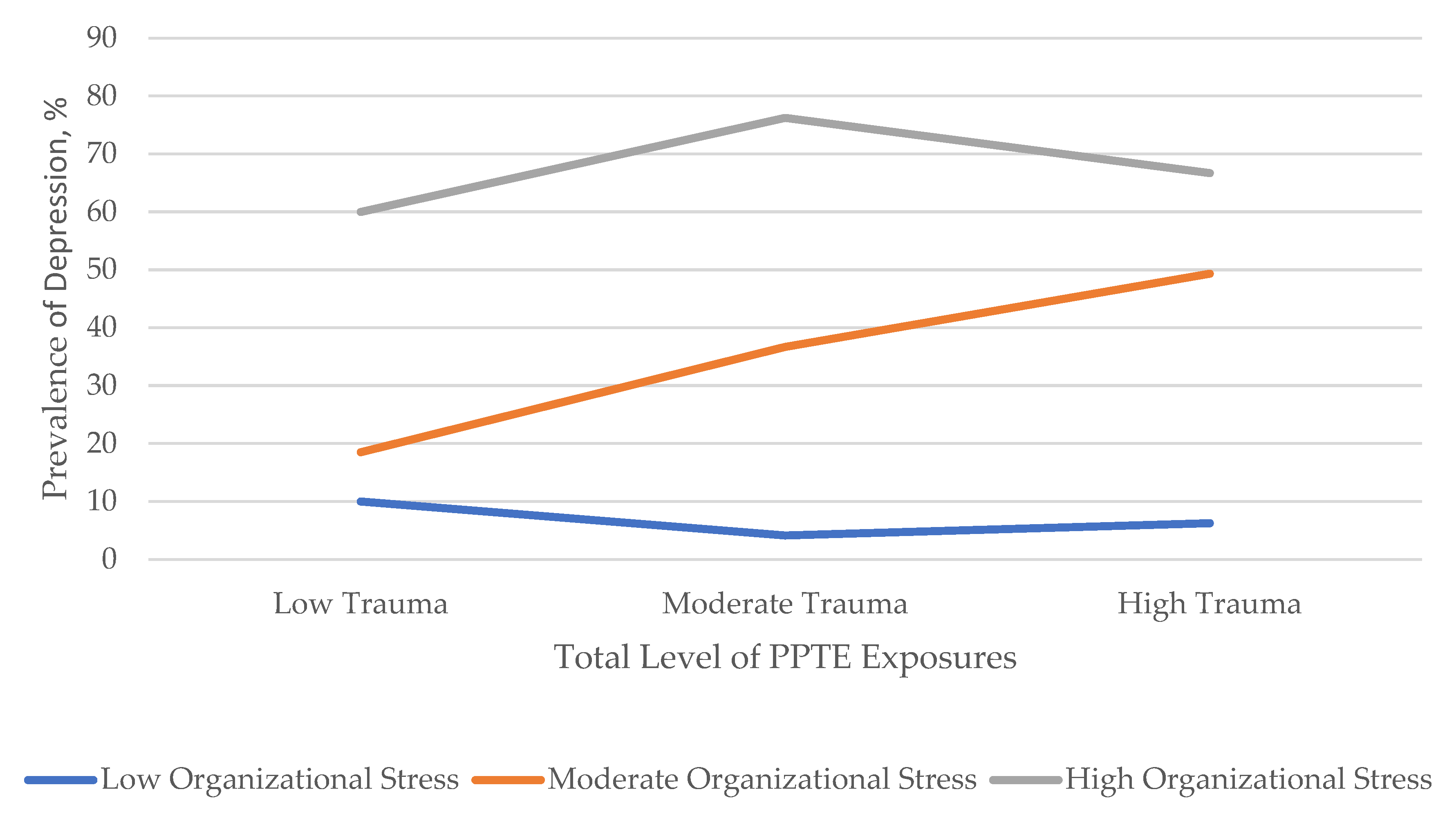
| Trauma Exposure by Organizational Stress Interaction Term | 0.99 (0.94, 1.04) | 1.05 * (1.01, 1.09) | 1.00 (0.96, 1.05) | 1.03 (0.97, 1.09) | 0.98 (0.91, 1.04) | 1.02 (0.97, 1.07) |
| Trauma Exposure by Operational Stress Interaction Term | 0.96 (0.92, 1.01) | 1.03 (0.99, 1.07) | 1.01 (0.97, 1.05) | 1.00 (0.96, 1.05) | 0.96 (0.91, 1.02) | 1.02 (0.97, 1.06) |
| Trauma Exposure by Other Stressors Interaction Term | 0.98 (0.94, 1.02) | 1.02 (0.99, 1.06) | 0.98 (0.94, 1.02) | 0.99 (0.95, 1.04) | 0.97 (0.92, 1.02) | 1.00 (0.96, 1.03) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konyk, K.; Ricciardelli, R.; Taillieu, T.; Afifi, T.O.; Groll, D.; Carleton, R.N. Assessing Relative Stressors and Mental Disorders among Canadian Provincial Correctional Workers. Int. J. Environ. Res. Public Health 2021, 18, 10018. https://doi.org/10.3390/ijerph181910018
Konyk K, Ricciardelli R, Taillieu T, Afifi TO, Groll D, Carleton RN. Assessing Relative Stressors and Mental Disorders among Canadian Provincial Correctional Workers. International Journal of Environmental Research and Public Health. 2021; 18(19):10018. https://doi.org/10.3390/ijerph181910018
Chicago/Turabian StyleKonyk, Katy, Rosemary Ricciardelli, Tamara Taillieu, Tracie O. Afifi, Dianne Groll, and R. Nicholas Carleton. 2021. "Assessing Relative Stressors and Mental Disorders among Canadian Provincial Correctional Workers" International Journal of Environmental Research and Public Health 18, no. 19: 10018. https://doi.org/10.3390/ijerph181910018
APA StyleKonyk, K., Ricciardelli, R., Taillieu, T., Afifi, T. O., Groll, D., & Carleton, R. N. (2021). Assessing Relative Stressors and Mental Disorders among Canadian Provincial Correctional Workers. International Journal of Environmental Research and Public Health, 18(19), 10018. https://doi.org/10.3390/ijerph181910018







