From Digital Mental Health to Digital Social and Emotional Wellbeing: How Indigenous Community-Based Participatory Research Influenced the Australian Government’s Digital Mental Health Agenda
Abstract
:1. Introduction
- The e-Mental Health in Practice project (eMHPrac)
- Digital mental health (d-MH)
- The Indigenous concept of social and emotional wellbeing (SEWB)
- Digital social and emotional wellbeing (d-SEWB)
- Community-based participatory research (CBPR)
1.1. The e-Mental Health in Practice Project (eMHPrac)
1.2. Digital Mental Health (d-MH)
1.3. The Indigenous Concept of Social and Emotional Wellbeing
1.4. Digital Social and Emotional Wellbeing (d-SEWB)
1.5. Community-Based Participatory Research
1.6. Aims of the Paper
- Provide concrete illustrations of the range of CBPR approaches used.
- Describe some of the key local and national project outcomes, and how these were linked to the CBPR processes. These links are illustrated in the Results section.
- Draw out some of the key implications for projects within Indigenous communities: in particular, implications for transforming top-down governments projects, maximising community involvement, providing adequate funding and timelines, building trusting relationships leading to co-learning, building Indigenous capacity and leadership, and prioritising time for team reflection.
- Make visible the contributions of the community partners to the intellectual, ethical and cultural integrity of the project.
2. Materials and Methods
2.1. The CBPR Partners
2.2. Data Collection Methods and Analysis
- Meeting notes from the Ngayundi Aboriginal Health Council
- Meeting notes from the Advisory Group and interviews with two members who were community leaders
- Written feedback from the AH&MRC Ethics Committee
- Transcripts and thematic analysis of audio recordings of the Learning Circle discussions
- Interviews with Workshop Trainers and their written reports
- Interviews with Workshop Participants
2.3. The University Centre for Rural Health Team
2.4. The d-SEWB Training Programs and the WellMob Website
3. Results
3.1. The Roles and Contributions of the Community Partners in Supporting the Research
3.2. Impacts of the Community Partnerships on the Design and Implementation of the Project
- Changing the conceptual framework of the project from digital mental health (d-MH) to digital social and emotional wellbeing (d-SEWB)
- Expanding the range and types of digital resources to encompass Indigenous SEWB domains
- Successfully advocating for an Indigenous-specific online therapy program
- Providing key inputs into the development and design of the R U Appy and Ur Mobile for Wellbeing training programs
- Successfully advocating for the development of what is now the WellMob website, the first Indigenous-specific “one-stop shop” portal of d-SEWB resources.
3.2.1. Changing the Conceptual Framework of the Project from Digital Mental Health (d-MH) to Digital Social and Emotional Wellbeing (d-SEWB)
3.2.2. Expanding the Range and Types of Digital Resources to Encompass the SEWB Domains
3.2.3. Successfully Advocating for an Aboriginal-Specific Online Therapy Program
3.2.4. Providing Key Inputs into the Development and Design of the R U Appy and Ur Mobile: A Tool 4 Wellbeing Training Programs
3.2.5. Successfully Advocating for Wellmob, a ‘One Stop Shop’ SEWB Website
4. Discussion
4.1. Creating Alignment of Project Goals across Community, Researchers and Government
4.2. Addressing d-MH/d-SEWB Issues of Equity for Indigenous Peoples
4.3. The Role of Community-Based Participatory Research (CBPR) in Indigenous Projects
4.4. Six Learning Outcomes
4.4.1. Community Involvement Is Central to Effective Outcomes
4.4.2. Providing Adequate Funding and Timelines Enables Meaningful Community Input
4.4.3. Set out to Create Co-Learning Hubs
4.4.4. Project Outcomes Are Greatly Enhanced by Building Local Capacity
4.4.5. Time for Reflection Needs to Be Intrinsic to CBPR Processes
4.4.6. Advocacy Is an Important Component of CBPR Processes
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singer, J.; Bennett-Levy, J.; Rotumah, D. “You didn’t just consult community, you involved us”: Transformation of a ‘top-down’ Aboriginal mental health project into a ‘bottom-up’ community-driven process. Australas. Psychiatry 2015, 23, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Gee, G.; Dudgeon, P.; Schultz, C.; Hart, A.; Kelly, K. Aboriginal and Torres Strait Islander social and emotional wellbeing and mental health. In Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice, 2nd ed.; Dudgeon, P., Milroy, H., Walker, R., Eds.; Commonwealth of Australia: Canberra, Australia, 2014; pp. 55–68. [Google Scholar]
- Department of Health and Ageing. E-Mental Health Strategy for Australia; Commonwealth of Australia: Canberra, Australia, 2012.
- Andersson, G. Internet-delivered psychological treatments. Annu. Rev. Clin. Psychol. 2016, 12, 157–179. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Titov, N.; Dear, B.F.; Staples, L.G.; Bennett-Levy, J.; Klein, B.; Rapee, R.M.; Shann, C.; Richards, D.; Andersson, G.; Ritterband, L.; et al. MindSpot Clinic: An accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015, 66, 1043–1050. [Google Scholar] [CrossRef]
- Perini, S.; Andrews, G.; Titov, N. Clinician-assisted Internet-based treatment is effective for depression: Randomized controlled trial. Aust. New Zealand J. Psychiatry 2009, 43, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Klein, B.; Richards, J.C.; Austin, D.W. Efficacy of internet therapy for panic disorder. J. Behav. Ther. Exp. Psychiatry 2006, 37, 213–238. [Google Scholar] [CrossRef] [PubMed]
- Christensen, H.; Griffiths, K.M.; Jorm, A.F. Delivering interventions for depression by using the internet: Randomised controlled trial. Br. Med. J. 2004, 328, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dingwall, K.M.; Puszka, S.; Sweet, M.; Mills, P.P.; Nagel, T. Evaluation of a culturally adapted training course in Indigenous e-mental health. Australas. Psychiatry 2015, 23, 630–635. [Google Scholar] [CrossRef]
- Povey, J.; Mills, P.P.; Dingwall, K.M.; Lowell, A.; Singer, J.; Rotumah, D.; Bennett-Levy, J.; Nagel, T. Acceptability of mental health apps for Aboriginal and Torres Strait Islander Australians: A qualitative study. J. Med. Internet Res. 2016, 18, e65. [Google Scholar] [CrossRef]
- Tighe, J.; Shand, F.; Ridani, R.; Mackinnon, A.; De La Mata, N.; Christensen, H. Ibobbly mobile health intervention for suicide prevention in Australian Indigenous youth: A pilot randomised controlled trial. BMJ Open 2017, 7, e013518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dudgeon, P.; Milroy, H.; Walker, R. Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice; Commonwealth of Australia: Canberra, Australia, 2014. [Google Scholar]
- Dudgeon, P.; Bray, A.; Darlaston-Jones, D.; Walker, R. Aboriginal Participatory Action Research: An Indigenous Research Methodology Strengthening Decolonisation and Social and Emotional Wellbeing; Lowitja Institute: Melbourne, Australia, 2020. [Google Scholar]
- Kelly, K.; Dudgeon, P.; Gee, G.; Glaskin, B. Living on the Edge: Social and Emotional Wellbeing and Risk and Protective Factors for Serious Psychological Distress among Aboriginal and Torres Strait Islander People, Discussion Paper No.10; Cooperative Research Centre for Aboriginal Health: Darwin, Australia, 2009. [Google Scholar]
- Dudgeon, P.; Walker, R. Decolonising Australian psychology: Discourses, strategies, and practice. J. Soc. Political Psychol. 2015, 3, 276–297. [Google Scholar] [CrossRef]
- Dudgeon, P.; Bray, A.; D’Costa, B.; Walker, R. Decolonising psychology: Validating social and emotional wellbeing. Aust. Psychol. 2017, 52, 316–325. [Google Scholar] [CrossRef]
- Garvey, D. A review of the Social and Emotional Wellbeing of Indigenous Australian Peoples—Considerations, Challenges and Opportunities. 2008. Available online: http://www.healthinfonet.ecu.edu.au/sewb_review (accessed on 28 June 2021).
- Minkler, M.; Wallerstein, N. Community-Based Participatory Research for Health: From Process to Outcomes, 2nd ed.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Wilson, E. Community-based participatory action research. In Handbook of Research Methods in Health Social Sciences; Liamputtong, P., Ed.; Springer: Heidelberg, Germany, 2019; pp. 285–298. [Google Scholar]
- Holkup, P.A.; Tripp-Reimer, T.; Salois, E.M.; Weinert, C. Community-based participatory research: An approach to intervention research with a Native American community. ANS Adv. Nurs. Sci. 2004, 27, 162–175. [Google Scholar] [CrossRef] [PubMed]
- Shalowitz, M.U.; Isacco, A.; Barquin, N.; Clark-Kauffman, E.; Delger, P.; Nelson, D.; Quinn, A.; Wagenaar, K.A. Community-based participatory research: A review of the literature with strategies for community engagement. J. Dev. Behav. Pediatrics 2009, 30, 350–361. [Google Scholar] [CrossRef]
- Winterbauer, N.L.; Bekemeier, B.; VanRaemdonck, L.; Hoover, A.G. Applying community-based participatory research partnership principles to public health practice-based research networks. Sage Open 2016, 6, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing partnership approaches to improve public health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [Green Version]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Educ. Health 2001, 14, 182–197. [Google Scholar]
- Israel, B.A.; Schultz, A.J.; Parker, E.A.; Becker, A.B.; Allen, A.J.; Guzman, J.R.; Lichtenstein, R. Critical issues in developing and following CBPR principles. In Community-Based Participatory Research for Health: From Process to Outcomes; Minkler, M., Wallerstein, N., Eds.; Jossey-Bass: San Francisco, CA, USA, 2017; pp. 47–66. [Google Scholar]
- Snijder, M.; Wagemakers, A.; Calabria, B.; Byrne, B.; O’Neill, J.; Bamblett, R.; Munro, A.; Shakeshaft, A. ‘We walked side by side through the whole thing’: A mixed-methods study of key elements of community-based participatory research partnerships between rural Aboriginal communities and researchers. Aust. J. Rural Health 2020, 28, 338–350. [Google Scholar] [CrossRef]
- Lin, C.Y.; Loyola-Sanchez, A.; Boyling, E.; Barnabe, C. Community engagement approaches for Indigenous health research: Recommendations based on an integrative review. BMJ Open 2020, 10, e039736. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, L.M.; Paradies, Y.C.; Eades, S.; Chong, A.; Maple-Brown, L.; Morris, P.; Bailie, R.; Cass, A.; Roberts-Thomson, K.; Brown, A. Ten principles relevant to health research among Indigenous Australian populations. Med. J. Aust. 2012, 197, 19–20. [Google Scholar] [CrossRef] [Green Version]
- Bennett-Levy, J.; Singer, J.; DuBois, S.; Hyde, K. Translating e-mental health into practice: What are the barriers and enablers to e-mental health implementation by Aboriginal and Torres Strait Islander health professionals? J. Med. Internet Res. 2017, 19, e1. [Google Scholar] [CrossRef]
- Bird, J.; Rotumah, D.; Bennett-Levy, J.; Singer, J. Diversity in eMental Health practice: An exploratory qualitative study of Aboriginal and Torres Strait Islander service providers. JMIR Ment. Health 2017, 4, e17. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Titov, N.; Schofield, C.; Staples, L.; Dear, B.F.; Nielssen, O. A comparison of Indigenous and non-Indigenous users of MindSpot: An Australian digital mental health service. Australas. Psychiatry 2019, 27, 352–357. [Google Scholar] [CrossRef]
- Dingwall, K.M.; Puszka, S.; Sweet, M.; Nagel, T. “Like drawing into sand”: Acceptability, feasibility, and appropriateness of a new e-mental health resource for service providers working with Aboriginal and Torres Strait Islander People. Aust. Psychol. 2015, 50, 60–69. [Google Scholar] [CrossRef]
- Walker, R.; Usher, K.; Jackson, D.; Reid, C.; Hopkins, K.; Shepherd, C.; Smallwood, R.; Marriott, R. Connection to... addressing digital inequities in supporting the well-being of young Indigenous Australians in the wake of COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2141. [Google Scholar] [CrossRef] [PubMed]
- Strudwick, G.; Sockalingam, S.; Kassam, I.; Sequeira, L.; Bonato, S.; Youssef, A.; Mehta, R.; Green, N.; Agic, B.; Soklaridis, S.; et al. Digital interventions to support population mental health in Canada during the COVID-19 pandemic: Rapid review. JMIR Ment. Health 2021, 8, e26550. [Google Scholar] [CrossRef] [PubMed]
- Roland, J.; Lawrence, E.; Insel, T.; Christensen, H. The Digital Mental Health Revolution: Transforming Care through Innovation and Scale-Up; World Innovation Summit for Health: Doha, Qatar, 2020. [Google Scholar]
- Andersson, G.; Carlbring, P. Cognitive behavioral therapy delivered using the internet. In Handbook of Cognitive Behavioral Therapy: Applications; Wenzel, A., Ed.; American Psychological Association: Washington, DC, USA, 2021; pp. 607–631. [Google Scholar]
- Wang, L.; Fagan, C.; Yu, C. Popular mental health apps (MH apps) as a complement to telepsychotherapy: Guidelines for consideration. J. Psychother. Integr. 2020, 30, 265–273. [Google Scholar] [CrossRef]
- Brown, K.A.; Toombs, M.; Nasir, B.; Kisely, S.; Ranmuthugala, G.; Brennan-Olsen, S.L.; Nicholson, G.C.; Gill, N.S.; Hayman, N.S.; Kondalsamy-Chennakesavan, S.; et al. How can mobile applications support suicide prevention gatekeepers in Australian Indigenous communities? Soc. Sci. Med. 2020, 258, 113015. [Google Scholar] [CrossRef] [PubMed]
- Christopher, S.; Saha, R.; Lachapelle, P.; Jennings, D.; Colclough, Y.; Cooper, C.; Cummins, C.; Eggers, M.J.; Fourstar, K.; Harris, K.; et al. Applying indigenous community-based participatory research principles to partnership development in health disparities research. Fam. Community Health 2011, 34, 246–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morton Ninomiya, M.E.; Pollock, N.J. Reconciling community-based Indigenous research and academic practices: Knowing principles is not always enough. Soc. Sci. Med. 2017, 172, 28–36. [Google Scholar] [CrossRef]
- Tremblay, M.C.; Martin, D.H.; McComber, A.M.; McGregor, A.; Macaulay, A.C. Understanding community-based participatory research through a social movement framework: A case study of the Kahnawake Schools Diabetes Prevention Project. BMC Public Health 2018, 18, 487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, M.; Brown, A.; Dudgeon, P.; McPhee, R.; Coffin, J.; Pearson, G.; Lin, A.; Newnham, E.; King Baguley, K.; Webb, M.; et al. Our journey, our story: A study protocol for the evaluation of a co-design framework to improve services for Aboriginal youth mental health and well-being. BMJ Open 2021, 11, e042981. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.; Dudgeon, P.; Holland, C.; Kelly, K.; Scrine, C.; Walker, R. Using participatory action research to prevent suicide in Aboriginal and Torres Strait Islander communities. Aust. J. Prim. Health 2014, 20, 345–349. [Google Scholar] [CrossRef]
- Themba-Nixon, M.; Minkler, M.; Freudenberg, N. The role of CBPR in policy advocacy. In Community-Based Participatory Research for Health: From Process to Outcomes; Minkler, M., Wallerstein, N., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 307–322. [Google Scholar]
- Newby, J.M.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE 2020, 15, e0236562. [Google Scholar] [CrossRef]
- Raphiphatthana, B.; Sweet, M.; Puszka, S.; Whitty, M.; Dingwall, K.; Nagel, T. Evaluation of electronic mental health implementation in Northern Territory services using the integrated “Promoting Action on Research Implementation in Health Services” framework: Qualitative study. JMIR Ment. Health 2020, 7, e14835. [Google Scholar] [CrossRef]
- Raphiphatthana, B.; Sweet, M.; Puszka, S.; Dingwall, K.; Nagel, T. Evaluation of a three-phase implementation program in enhancing e-mental health adoption within Indigenous primary healthcare organisations. BMC Health Serv. Res. 2020, 20, 576. [Google Scholar] [CrossRef] [PubMed]
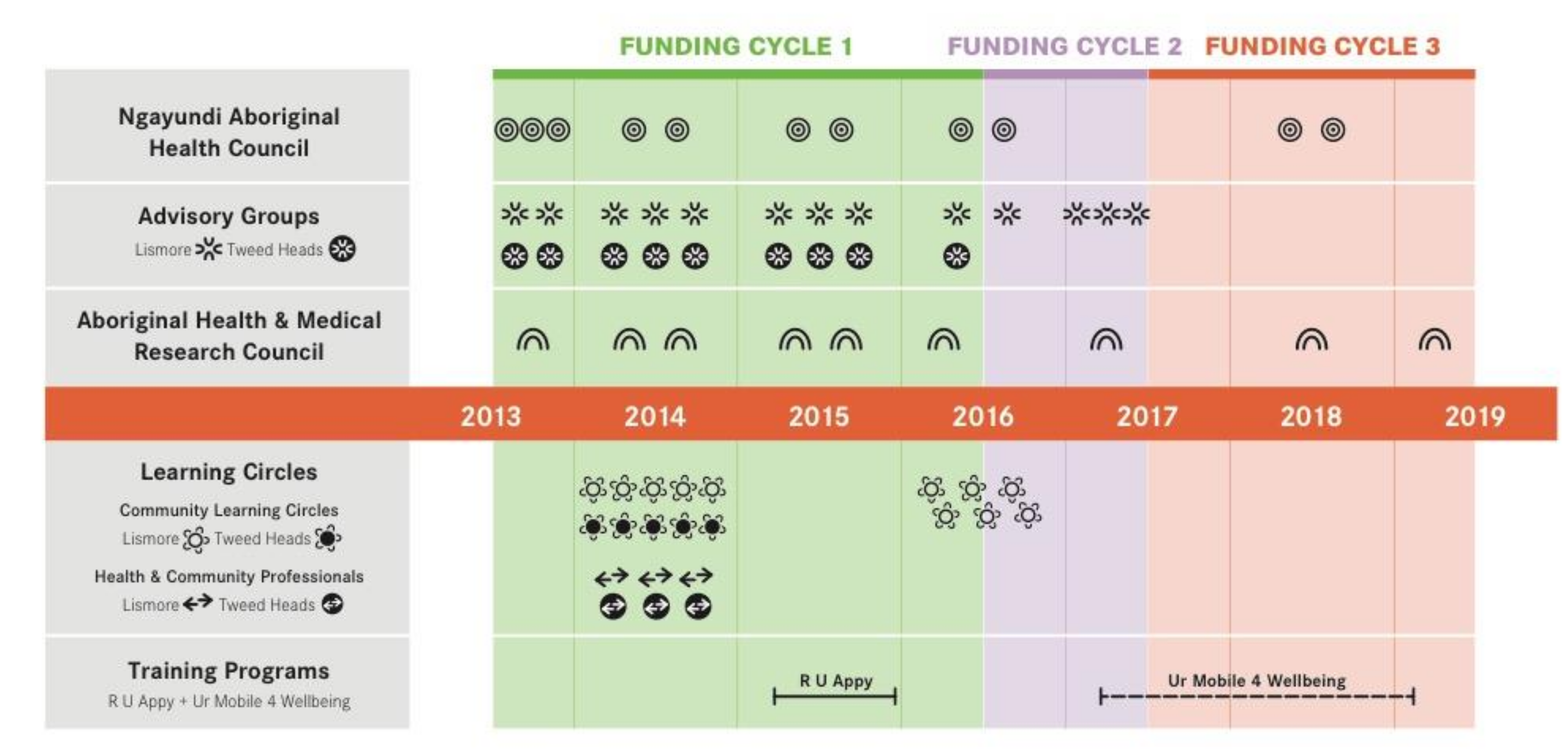
| Community Partners | Years; Numbers of Data Collection Events | Data Management |
|---|---|---|
| Ngayundi Aboriginal Health Council | 2013–2018 11 meetings | Review of written meeting notes |
| Advisory Group (AG) | 2013–2019 22 meetings | Written meeting notes from each AG. Circulated to all AG members as part of iterative process. Included as Appendices in reports to Dept of Health. Transcribed interviews with 2 AG community leaders by author JS. |
| AH & MRC Ethics Committee | 2013–2019 9 applications | Ethics applications and amendments enabled AH&MRC ongoing review of research, cultural protocols and governance structures. |
| Learning Circles | 2014: 16 sessions/36 participants 2016: 6 sessions/7 participants | Audio recordings for 16 sessions. Transcription and thematic analysis by JS. Key themes in reports to Dept of Health and Mindspot. 6 participant interviews and thematic analysis by JS. Key themes in report to Dept of Health. |
| Workshop Participants | 2015: Interviews with the 2 trainers, and their written reports 2016: Interviews with the 16 participants | Transcription and thematic analysis of interviews and written reports by JS, credibility check by author JB-L. Reported in publication [30]. Transcripts and thematic analysis of interviews by Jennifer Bird and author DR. Reported in publication [31]. |
| R U Appy Training 2015 | Ur Mobile: A Tool 4 Wellbeing Training 2017–2019 | WellMob Website 2020–Ongoing |
|---|---|---|
| What: 3-day workshop, plus follow-up support Where: Lismore and Tweed Heads How many: 5 programs Program: Day 1—Orientation to digital technologies Day 2—Learn about the Stay Strong app Day 3—Using Stay Strong in practice, including skill devel- opment in micro-counselling, risk assessment and referral skills and goal setting. Follow-up Support—Monthly ‘booster’ sessions for 5 months | What: Half-day workshop to build resource library, sometimes combined with Stay Strong skills building workshop Where: NSW How many: 13 workshops Program: Half-day: Build a d-SEWB resource library by developing technology skills to search, assess and save d-SEWB resources in the device of choice Half-day (optional): Using Stay Strong in Practice | What: Australia’s first ‘one-stop-shop’ website for Indigenous-specific SEWB resources, including videos, apps, podcasts, websites, online programs, social media Where: www.wellmob.org.au (accessed on 29 June 2021) Who: Indigenous frontline workers and communities, and others working with Indigenous people Why: Feedback from Community Partners about the need for a SEWB website ‘made by and for mob’ |
| Ngayundi Aboriginal Health Council | Who? Indigenous representatives from across Bundjalung country. Primarily a Community Elders Council, it also involved Indigenous HCPs including CEOs, program managers from Government and NGO services, and was open to all Indigenous people interested to attend. Number of attendees varied from around 20–40 at different meetings. What? Regional governance role to review and monitor various health and wellbeing programs proposed for the local community. This included guidance on the project design, research methods and engagement strategies, as well as formal endorsement of the project. Where? Meetings rotated around Bundjalung Country, e.g., Tweed Heads, Lismore, Ballina, Casino, Kyogle, Fingal Heads |
| Indigenous Advisory Groups (AGs) | Who? Included service managers, Elders, Indigenous HCPs, and community members with lived experience. 6–10 members in the 2 AGs—see below. What? The project’s “in-house brains trust”, crucial in shaping community involvement strategies; in particular, the recruitment to the Learning Circles and engagement of/with local service managers; made significant contributions to ensuring appropriate cultural protocols were in place; and to the structure, design and content of the training package. Where? AGs in 2 locations across the Bundjalung nation: Lismore/Widjabul-Wyabul country and Tweed Heads/Minjungbal country. |
| Learning Circles | Who? Community members and Health and Community Professionals (HCPs) 2014: two cohorts (n = 32): community members (n = 16) and HCPs (n = 16) 2016: one mixed group of community members and HCPs (n = 7) What? Purpose: to enable an immersive experience over time in order to: (1) user-test and provide feedback on a variety of d-SEWB resources (2) to provide advice about the structure, design and cultural appropriateness of the R U Appy and Ur Mobile for Wellbeing d-SEWB training programs. Where? 2 locations, Lismore, Tweed Heads How often? 2014: three-hour LC sessions for Community Members ran over 5 consecutive weeks, across the two locations (15 hrs total); the LC for HCPs were over 3 weeks due to work commitments (9 h). 2016: three-hour LC sessions over 6 weeks for mixed group ran in one location, Lismore (18 h). |
| Workshop Participants | Who? Over 300 Indigenous and non-Indigenous HCPs attended the R U Appy and Ur Mobile: A Tool 4 Wellbeing programs. Detailed feedback was obtained from 28 Indigenous HCPs who attended “booster sessions” following the R U Appy 3-day training program (2015). What? Report and analysis of participants’ feedback are described in previous papers [30,31] Where? 6 booster groups across 4 regions on Bundjalung Country How often? Up to 5 booster sessions over 5 months |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bennett-Levy, J.; Singer, J.; Rotumah, D.; Bernays, S.; Edwards, D. From Digital Mental Health to Digital Social and Emotional Wellbeing: How Indigenous Community-Based Participatory Research Influenced the Australian Government’s Digital Mental Health Agenda. Int. J. Environ. Res. Public Health 2021, 18, 9757. https://doi.org/10.3390/ijerph18189757
Bennett-Levy J, Singer J, Rotumah D, Bernays S, Edwards D. From Digital Mental Health to Digital Social and Emotional Wellbeing: How Indigenous Community-Based Participatory Research Influenced the Australian Government’s Digital Mental Health Agenda. International Journal of Environmental Research and Public Health. 2021; 18(18):9757. https://doi.org/10.3390/ijerph18189757
Chicago/Turabian StyleBennett-Levy, James, Judy Singer, Darlene Rotumah, Sarah Bernays, and David Edwards. 2021. "From Digital Mental Health to Digital Social and Emotional Wellbeing: How Indigenous Community-Based Participatory Research Influenced the Australian Government’s Digital Mental Health Agenda" International Journal of Environmental Research and Public Health 18, no. 18: 9757. https://doi.org/10.3390/ijerph18189757
APA StyleBennett-Levy, J., Singer, J., Rotumah, D., Bernays, S., & Edwards, D. (2021). From Digital Mental Health to Digital Social and Emotional Wellbeing: How Indigenous Community-Based Participatory Research Influenced the Australian Government’s Digital Mental Health Agenda. International Journal of Environmental Research and Public Health, 18(18), 9757. https://doi.org/10.3390/ijerph18189757






