One-Year Changes in Activities of Daily Living, Usability, Falls and Concerns about Falling, and Self-Rated Health for Different Housing Adaptation Client Profiles
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Context and Design
2.2. Data Collection
2.2.1. Study Population
2.2.2. Outcomes
2.3. Client Profiles
2.4. Data Analysis
Potential Confounding
2.5. Ethics
3. Results
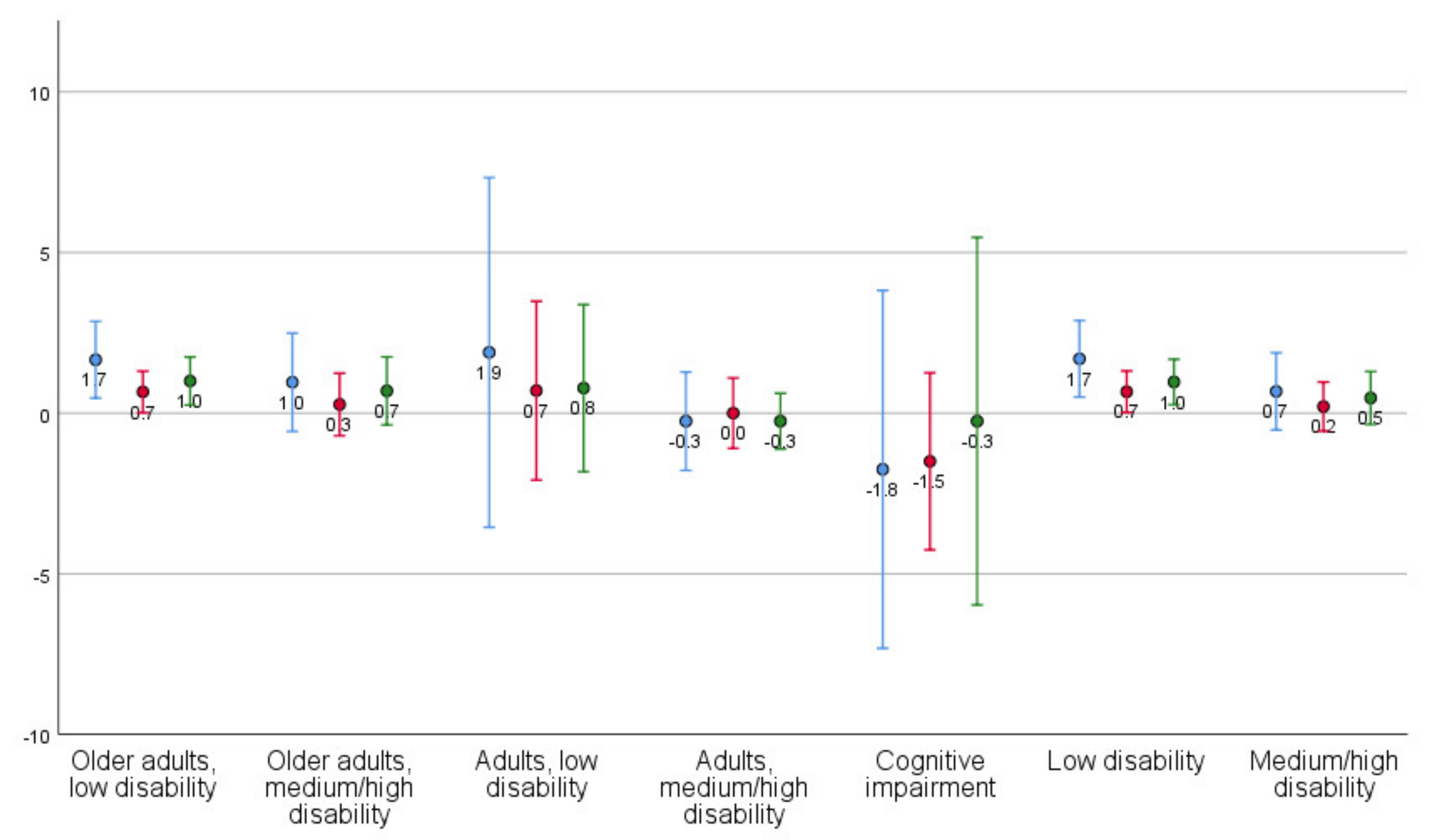
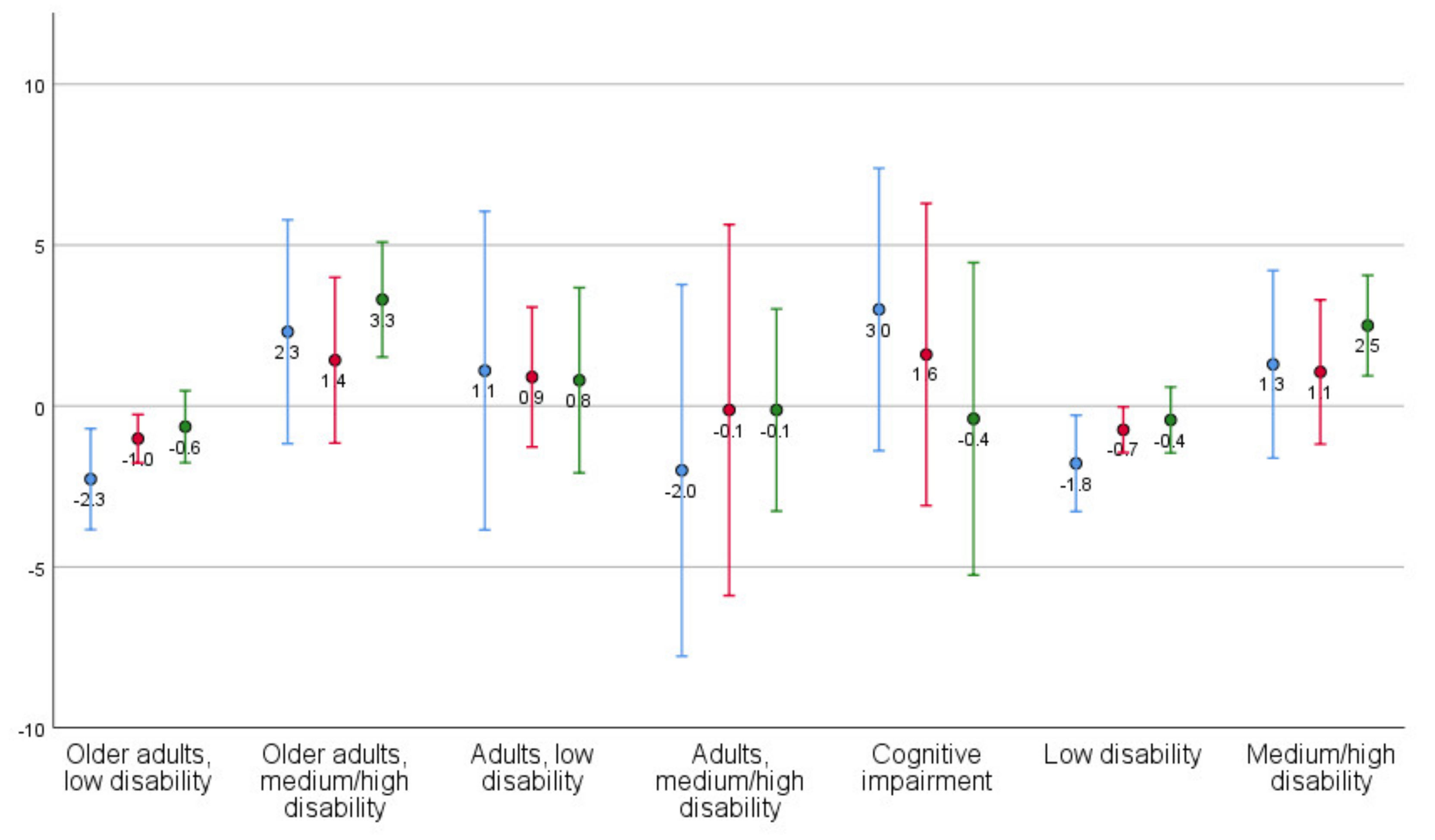
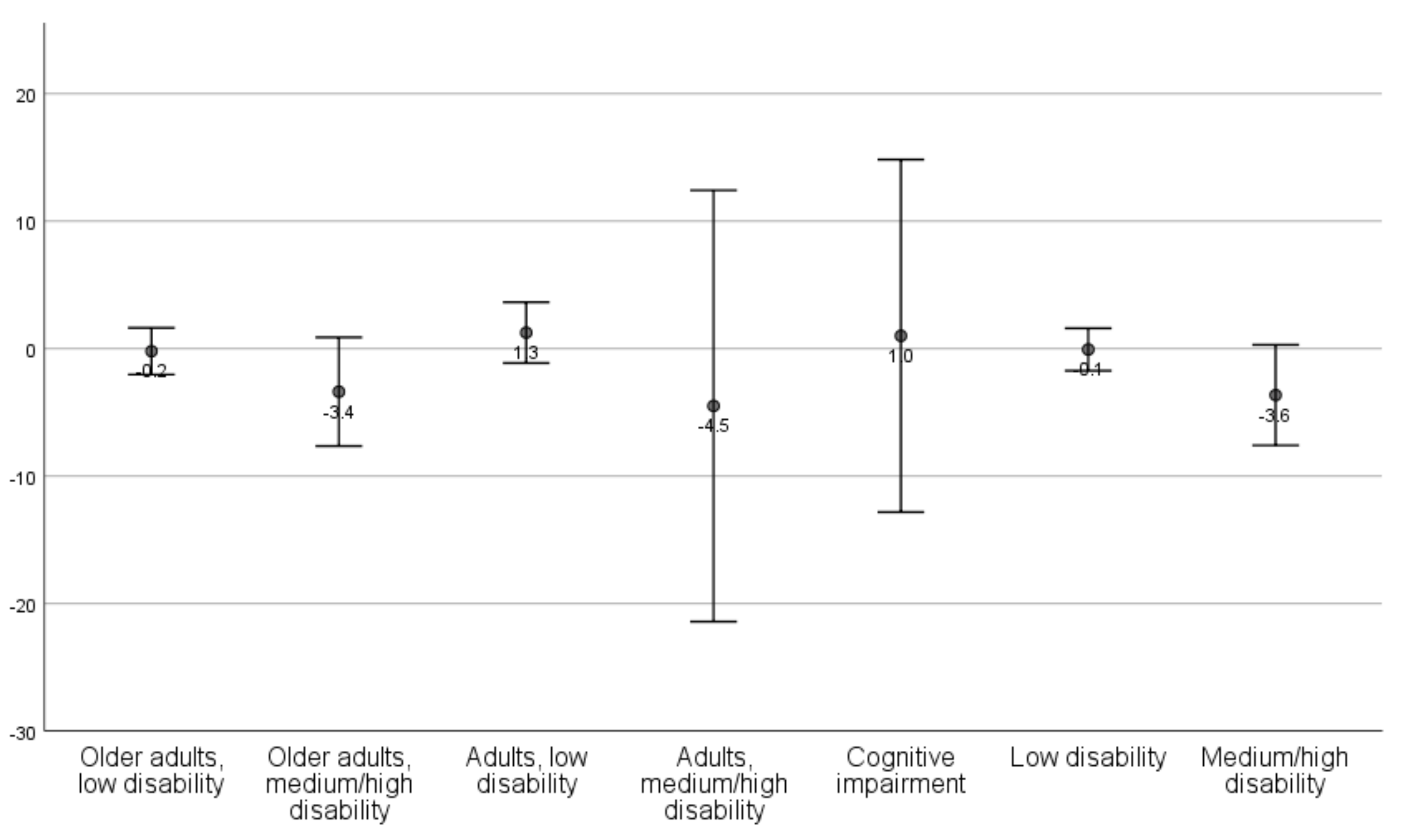
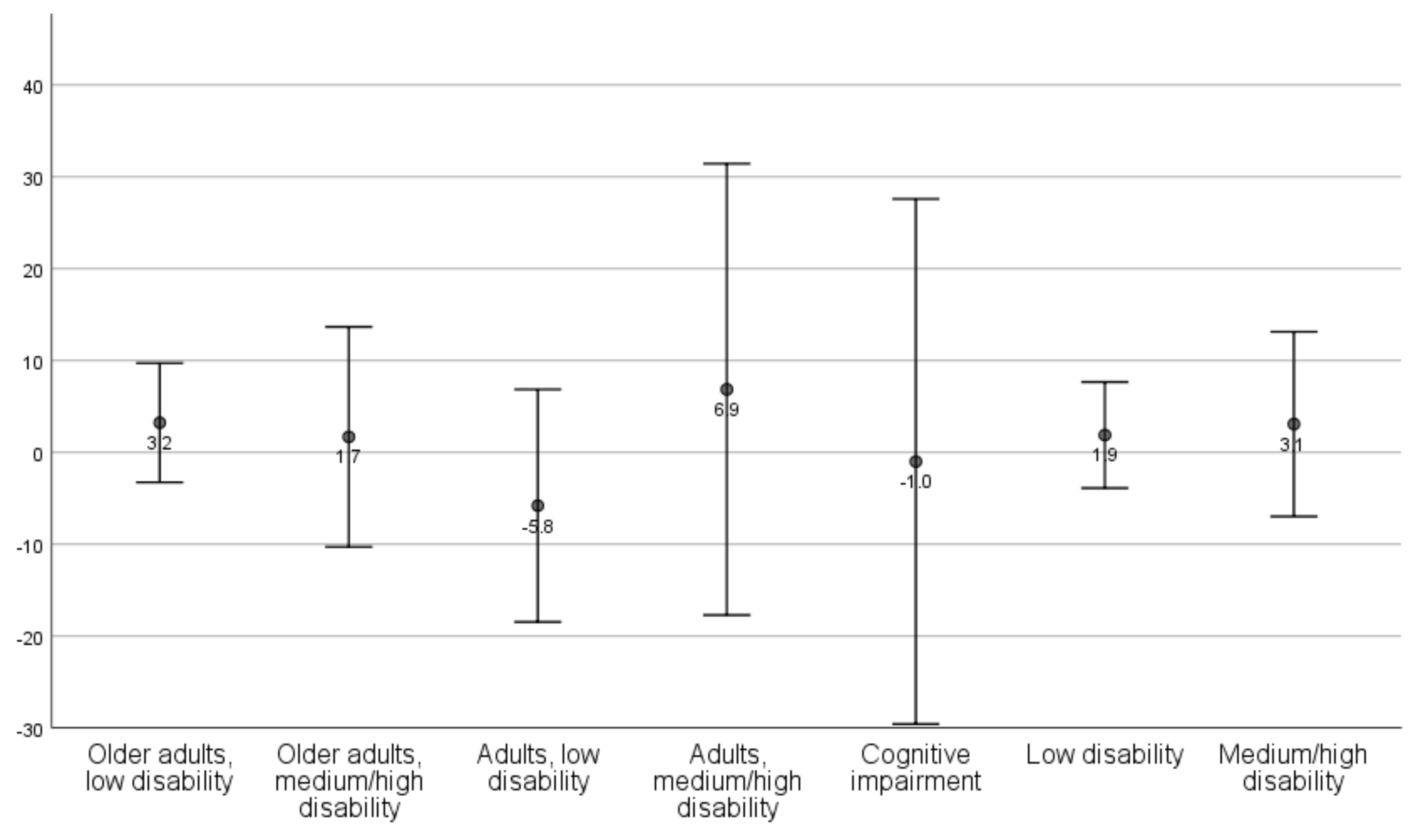
3.1. Changes in Outcomes Per Client Profile
| Older Adults, Low Disability | Older Adults, Medium/High Disability | Adults, Low Disability | Adults, Medium/High Disability | Cognitive Impairment | p-Value | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | n | M | SD | n | M | SD | n | M | SD | Unadj/Adj 1 | |
| ADL | ||||||||||||||||
| T1 | 59 | 9.8 | 5.7 | 26 | 12.9 | 6.2 | 10 | 7.7 | 3.5 | 8 | 19.5 | 3.4 | 5 | 8.2 | 5.0 | |
| T4 | 59 | 11.5 | 6.3 | 26 | 13.8 | 5.5 | 9 | 9.2 | 6.7 | 8 | 19.3 | 4.7 | 4 | 4.8 | 4.9 | 0.488/0.677 |
| Change | 59 | 1.7 | 4.6 | 26 | 1.0 | 3.8 | 9 | 1.9 | 7.1 | 8 | −0.2 | 1.8 | 4 | −1.7 | 3.5 | |
| P-ADL | ||||||||||||||||
| T1 | 59 | 3.3 | 3.0 | 26 | 4.5 | 3.4 | 10 | 2.3 | 1.8 | 8 | 8.6 | 2.8 | 5 | 3.2 | 2.3 | |
| T4 | 59 | 3.9 | 3.5 | 26 | 4.8 | 3.8 | 10 | 3.0 | 4.1 | 8 | 8.6 | 3.5 | 4 | 1.0 | 0.8 | 0.522/0.284 |
| Change | 59 | 0.7 | 2.5 | 26 | 0.3 | 2.4 | 10 | 0.7 | 3.9 | 8 | 0.0 | 1.3 | 4 | −1.5 | 1.7 | |
| I-ADL | ||||||||||||||||
| T1 | 59 | 6.5 | 3.3 | 26 | 8.4 | 3.3 | 10 | 5.4 | 2.1 | 8 | 10.9 | 1.0 | 5 | 5.0 | 3.1 | |
| T4 | 59 | 7.5 | 3.4 | 26 | 9.1 | 2.2 | 9 | 5.9 | 2.7 | 8 | 10.6 | 1.6 | 4 | 3.7 | 4.1 | 0.733/0.970 |
| Change | 59 | 1.0 | 2.9 | 26 | 0.7 | 2.6 | 9 | 0.8 | 3.4 | 8 | −0.2 | 1.0 | 4 | −0.2 | 3.6 | |
| Usability: Self-Care 2 | ||||||||||||||||
| T1 | 59 | 21.0 | 3.6 | 26 | 12.3 | 6.2 | 10 | 18.0 | 4.5 | 8 | 11.5 | 4.6 | 5 | 17.0 | 3.2 | |
| T4 | 59 | 18.8 | 6.0 | 26 | 14.7 | 6.3 | 10 | 19.1 | 4.8 | 8 | 9.5 | 6.6 | 5 | 20.0 | 1.2 | 0.037/0.072 |
| Change | 59 | −2.3 | 6.0 | 26 | 2.3 | 8.6 | 10 | 1.1 | 6.9 | 8 | −2.0 | 6.9 | 5 | 3.0 | 3.5 | |
| Usability: Social 3 | ||||||||||||||||
| T1 | 59 | 13.6 | 1.4 | 26 | 9.4 | 4.5 | 10 | 13.0 | 2.7 | 8 | 10.8 | 3.7 | 5 | 10.0 | 3.5 | |
| T4 | 59 | 12.6 | 2.8 | 26 | 10.8 | 3.6 | 10 | 13.9 | 1.4 | 8 | 10.6 | 5.3 | 5 | 11.6 | 0.9 | 0.144/0.340 |
| Change | 59 | −1.0 | 2.9 | 26 | 1.4 | 6.4 | 10 | 0.9 | 3.0 | 8 | −0.1 | 6.9 | 5 | 1.6 | 3.8 | |
| Usability: Outdoor Leisure 4 | ||||||||||||||||
| T1 | 59 | 9.8 | 3.2 | 26 | 4.3 | 3.0 | 10 | 9.1 | 1.4 | 8 | 6.3 | 3.2 | 5 | 11.0 | 2.6 | |
| T4 | 59 | 9.1 | 4.3 | 26 | 7.6 | 4.0 | 10 | 9.9 | 3.6 | 8 | 6.1 | 3.8 | 5 | 10.6 | 2.7 | 0.005/0.222 |
| Change | 59 | −0.6 | 4.3 | 26 | 3.3 | 4.4 | 10 | 0.8 | 4.0 | 8 | −0.1 | 3.8 | 5 | −0.4 | 3.9 | |
| Concerns about Falling | ||||||||||||||||
| T1 | 48 | 14.3 | 4.4 | 18 | 18.6 | 5.3 | 9 | 18.7 | 5.8 | 8 | 18.6 | 8.3 | 3 | 12.7 | 6.0 | |
| T4 | 46 | 13.9 | 4.8 | 18 | 14.9 | 5.2 | 4 | 18.3 | 7.8 | 4 | 14.0 | 7.3 | 5 | 15.6 | 4.7 | 0.330/0.200 |
| Change | 39 | −0.2 | 5.6 | 13 | −3.4 | 7.1 | 4 | 1.3 | 1.5 | 4 | −4.5 | 10.6 | 3 | 1.0 | 5.6 | |
| Self-Rated Health | ||||||||||||||||
| T1 | 59 | 61.7 | 18.5 | 22 | 51.0 | 19.6 | 10 | 59.8 | 18.1 | 8 | 42.5 | 22.7 | 5 | 55.0 | 14.1 | |
| T4 | 57 | 65.0 | 20.1 | 22 | 57.3 | 22.6 | 10 | 54.0 | 22.9 | 7 | 48.3 | 26.6 | 5 | 54.0 | 32.1 | 0.814/0.554 |
| Change | 57 | 3.2 | 24.5 | 19 | 1.7 | 24.8 | 10 | −5.8 | 17.7 | 7 | 6.9 | 26.6 | 5 | −1.0 | 23.0 | |
| Low Disability | Medium/High Disability | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | Unadj | Adj | ||
| ADL | T1 | 69 | 9.5 | 5.5 | 34 | 14.4 | 6.3 | ||
| T4 | 68 | 11.2 | 6.3 | 34 | 15.1 | 5.7 | |||
| Change | 68 | 1.7 | 4.9 | 34 | 0.7 | 3.4 | 0.284 | 0.940 | |
| P-ADL | T1 | 69 | 3.1 | 2.8 | 34 | 5.5 | 3.7 | ||
| T4 | 69 | 3.8 | 3.5 | 34 | 5.7 | 4.0 | |||
| Change | 69 | 0.7 | 2.7 | 34 | 0.2 | 2.2 | 0.388 | 0.817 | |
| I-ADL | T1 | 69 | 6.4 | 3.2 | 34 | 9.0 | 3.1 | ||
| T4 | 68 | 7.3 | 3.3 | 34 | 9.4 | 2.1 | |||
| Change | 68 | 1.0 | 2.9 | 34 | 0.5 | 2.4 | 0.389 | 0.676 | |
| Usability: Self-care | T1 | 69 | 20.6 | 3.9 | 34 | 12.1 | 5.8 | ||
| T4 | 69 | 18.8 | 5.8 | 34 | 13.4 | 6.7 | |||
| Change | 69 | −1.8 | 6.2 | 34 | 1.3 | 8.4 | 0.038 | 0.397 | |
| Usability: Social | T1 | 69 | 13.5 | 1.7 | 34 | 9.7 | 4.3 | ||
| T4 | 69 | 12.8 | 2.6 | 34 | 10.8 | 4.0 | |||
| Change | 69 | −0.7 | 3.0 | 34 | 1.1 | 6.4 | 0.054 | 0.244 | |
| Usability: Outdoor leisure | T1 | 69 | 9.7 | 3.0 | 34 | 4.8 | 3.1 | ||
| T4 | 69 | 9.2 | 4.2 | 34 | 7.3 | 4.0 | |||
| Change | 69 | −0.4 | 4.3 | 34 | 2.5 | 4.5 | 0.002 | 0.037 | |
| Concerns about falling | T1 | 57 | 15.0 | 4.8 | 26 | 18.6 | 6.2 | ||
| T4 | 50 | 14.2 | 5.1 | 22 | 14.7 | 5.4 | |||
| Change | 43 | −0.1 | 5.4 | 17 | −3.6 | 7.7 | 0.045 | 0.100 | |
| Self-rated health | T1 | 69 | 61.4 | 18.4 | 30 | 48.8 | 20.4 | ||
| T4 | 67 | 63.4 | 20.8 | 29 | 55.1 | 23.4 | |||
| Change | 67 | 1.9 | 23.7 | 26 | 3.1 | 24.9 | 0.830 | 0.324 | |
3.2. Differences in Changes in Outcomes between Client Profiles
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. World Population Ageing 2020 Highlights; UN: New York, NY, USA, 2020. [Google Scholar]
- Dalmer, N.K. A logic of choice: Problematizing the documentary reality of Canadian aging in place policies. J. Aging Stud. 2019, 48, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Abramsson, M.; Hagberg, J.-E. Housing plans of the oldest: Ageing in semi-rural areas in Sweden. J. Hous. Built Environ. 2019, 35, 27–43. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). World Report on Disability; WHO Press: Geneva, Switzerland, 2011. [Google Scholar]
- World Health Organization (WHO). International Classification of Functioning, Disability and Health, ICF; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- World Health Organization (WHO). World Report on Health; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Ekstam, L.; Carlsson, G.; Chiatti, C.; Nilsson, M.H.; Fänge, A.M. A research-based strategy for managing housing adaptations: Study protocol for a quasiexperimental trial. BMC Heal. Serv. Res. 2014, 14, 602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fänge, A.M.; Carlsson, G.; Axmon, A.; Thordardottir, B.; Chiatti, C.; Nilsson, M.H.; Ekstam, L. Effects of applying a standardized assessment and evaluation protocol for housing adaptations—Results from a quasi-experimental study. BMC Public Health 2019, 19, 1446. [Google Scholar] [CrossRef]
- Lag om bostadsanpassningsbidrag mm. (SFS 2018:222). Socialdepartementet. (Swedish Act on Housing Adaptation Grants etc. In Swedish). Available online: https://lagen.nu/2018:222 (accessed on 1 August 2021).
- Boverket. Bostadsanpassningsbidragen 2019. Available online: https://www.boverket.se/sv/om-boverket/publicerat-av-boverket/publikationer/2020/bostadsanpassningsbidragen-2019/ (accessed on 11 June 2021).
- Chase, C.A.; Mann, K.; Wasek, S.; Arbesman, M. Systematic review of the effect of home modification and fall prevention programs on falls and the performance of community-dwelling older adults. Am. J. Occup. Ther. 2012, 66, 284–291. [Google Scholar] [CrossRef] [Green Version]
- Carnemolla, P.; Bridge, C. A scoping review of home modification interventions—Mapping the evidence. Indoor Built Environ. 2018. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Dennis, M.P.; Corcoran, M.; Schinfeld, S.; Hauck, W.W. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J. Am. Geriatr. Soc. 2006, 54, 809–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salminen, A.-L.; Kanelisto, K.J.; Karhula, M.E. What components of rehabilitation are helpful from the perspective of individuals with multiple sclerosis? Disabil. Rehabil. 2014, 36, 1983–1989. [Google Scholar] [CrossRef]
- Stark, S.; Keglovits, M.; Arbesman, M.; Lieberman, D. Effect of home modification interventions on the participation of community-dwelling adults with health conditions: A systematic review. Am. J. Occup. Ther. 2017, 71, 7102290010p1–7102290010p11. [Google Scholar] [CrossRef]
- Gefenaite, G.; Björk, J.; Iwarsson, S.; Slaug, B.; Schmidt, S.M.; Nilsson, M.H. Longitudinal association between housing accessibility and activities of daily living: The role of self-efficacy and control in people ageing with Parkinson’s disease. BMC Geriatr. 2020, 20, 181. [Google Scholar] [CrossRef]
- Keall, M.D.; Pierse, N.; Howden-Chapman, P.; Cunningham, C.; Cunningham, M.; Guria, J.; Baker, M.G. Home modifications to reduce injuries from falls in the home injury prevention intervention (HIPI) study: A cluster-randomised controlled trial. Lancet 2015, 385, 231–238. [Google Scholar] [CrossRef]
- Kader, M.; Iwarsson, S.; Odin, P.; Nilsson, M.H. Fall-related activity avoidance in relation to a history of falls or near falls, fear of falling and disease severity in people with Parkinson’s disease. BMC Neurol. 2016, 16, 84. [Google Scholar] [CrossRef] [Green Version]
- Boström, L.; Chiatti, C.; Thordardottir, B.; Ekstam, L.; Fänge, A.M. Health-related quality of life among people applying for housing adaptations: Associated factors. Int. J. Environ. Res. Public Health 2018, 15, 2130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, J.; Shakil-ur-Rehman, S.; Sibtain, F. Effectiveness of home modification on quality of life on wheelchair user paraplegic population. Rawal Med. J. 2013, 38, 263–265. [Google Scholar]
- Elwyn, G.; Frosch, D.L.; Kobrin, S. Implementing shared decision-making: Consider all the consequences. Implement. Sci. 2015, 11, 114. [Google Scholar] [CrossRef] [Green Version]
- Chiatti, C.; Iwarsson, S. Evaluation of housing adaptation interventions: Integrating the economic perspective into occupational therapy practice. Scand. J. Occup. Ther. 2014, 21, 323–333. [Google Scholar] [CrossRef] [Green Version]
- Luther, A.; Chiatti, C.; Ekstam, L.; Thordardottir, B.; Fänge, A.M. Identifying and validating housing adaptation client profiles—A mixed methods study. Disabil. Rehabil. 2019, 42, 2027–2034. [Google Scholar] [CrossRef] [PubMed]
- Axmon, A.; Ekstam, L.; Slaug, B.; Schmidt, S.M.; Fänge, A.M. Detecting longitudinal changes in activities of daily living (ADL) dependence: Optimizing ADL staircase response choices. Br. J. Occup. Ther. 2019, 82, 646–652. [Google Scholar] [CrossRef]
- Thordardottir, B.; Ekstam, L.; Chiatti, C.; Fänge, A.M. Factors associated with participation frequency and satisfaction among people applying for a housing adaptation grant. Scand. J. Occup. Ther. 2015, 23, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Kempen, G.I.J.M.; Yardley, L.; Van Haastregt, J.C.M.; Zijlstra, G.A.R.; Beyer, N.; Hauer, K.; Todd, C. The Short FES-I: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2007, 37, 45–50. [Google Scholar] [CrossRef] [Green Version]
- Van Reenen, M.; Janssen, B. EQ-5D-5L User Guide. Basic Information on How to Use the EQ-5D-5L Instrument; EuroQol Research Foundation: Rotterdam, The Netherlands, 2015. [Google Scholar]
- Conner-Spady, B.L.; Marshall, D.A.; Bohm, E.; Dunbar, M.J.; Loucks, L.; Al Khudairy, A.; Noseworthy, T.W. Reliability and validity of the EQ-5D-5L compared to the EQ-5D-3L in patients with osteoarthritis referred for hip and knee replacement. Qual. Life Res. 2015, 24, 1775–1784. [Google Scholar] [CrossRef]
- Thordardottir, B.; Chiatti, C.; Ekstam, L.; Fänge, A.M. Heterogeneity of characteristics among housing adaptation clients in sweden—Relationship to participation and self-rated health. Int. J. Environ. Res. Public Health 2015, 13, 91. [Google Scholar] [CrossRef] [Green Version]
- Iwarsson, S.; Slaug, B. Housing Enabler—A Method for Rating/Screening and Analysing Accessibility Problem in Housing. A Manual for the Complete Instrument and Screening Tool; Veten & Skapen HB & Slaug Data Management: Lund, Sweden, 2010. [Google Scholar]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. JAGS J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Ellmers, T.J.; Cocks, A.J.; Young, W. Evidence of a Link Between Fall-Related Anxiety and High-Risk Patterns of Visual Search in Older Adults During Adaptive Locomotion. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2020, 75, 961–967. [Google Scholar] [CrossRef] [Green Version]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlsson, G.; Nilsson, M.H.; Ekstam, L.; Chiatti, C.; Fänge, A.M. Falls and fear of falling among persons who receive housing adaptation—Results from a quasi-experimental study in Sweden. Healthcare 2017, 5, 66. [Google Scholar] [CrossRef] [Green Version]
- Denkinger, M.D.; Lukas, A.; Nikolaus, T.; Hauer, K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: A systematic review. Am. J. Geriatr. Psychiatry 2015, 23, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Kornadt, A.E.; Kessler, E.-M.; Wurm, S.; Bowen, C.E.; Gabrian, M.; Klusmann, V. Views on ageing: A lifespan perspective. Eur. J. Ageing 2020, 17, 387–401. [Google Scholar] [CrossRef] [PubMed]
- Infurna, F.J.; Luthar, S.S. Re-evaluating the notion that resilience is commonplace: A review and distillation of directions for future research, practice and policy. Clin. Psychol. Rev. 2018, 65, 43–56. [Google Scholar] [CrossRef]
- Becker, S.; Bäumer, A.; Maetzler, W.; Nussbaum, S.; Tkaczynska, Z.; Sulzer, P.; Timmers, M.; Van Nueten, L.; Salvadore, G.; Brockmann, K.; et al. Association of cognitive activities of daily living (ADL) function and nonmotor burden in nondemented Parkinson’s disease patients. Neuropsychology 2020, 34, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Cordier, R.; Chen, Y.; Clemson, L.; Byles, J.; Mahoney, N. Subjective memory complaints and difficulty performing activities of daily living among older women in Australia. Aust. Occup. Ther. J. 2019, 66, 227–238. [Google Scholar] [CrossRef]
- Winblad, B.; Amouyel, P.; Andrieu, S.; Ballard, C.; Brayne, C.; Brodaty, H.; Cedazo-Minguez, A.; Dubois, B.; Edvardsson, D.; Feldman, H.; et al. Defeating Alzheimer’s disease and other dementias: A priority for European science and society. Lancet Neurol. 2016, 15, 455–532. [Google Scholar] [CrossRef] [Green Version]
- Lawton, M.P.; Nahemow, L. Ecology and the aging process. In The Psychology of Adult Development and Aging; Eisdorfer, C., Lawton, M.P., Eds.; American Psychological Association: Washington, DC, USA, 1973; pp. 619–674. [Google Scholar]
- Ahrentzen, S.; Tural, E. The role of building design and interiors in ageing actively at home. Build. Res. Inf. 2015, 43, 582–601. [Google Scholar] [CrossRef]
- Slaug, B.; Chiatti, C.; Oswald, F.; Kaspar, R.; Schmidt, S.M. Improved housing accessibility for older people in Sweden and Germany: Short term costs and long-term gains. Int. J. Environ. Res. Public Health 2017, 14, 964. [Google Scholar] [CrossRef]
- Stucki, G.; Zampolini, M.; Selb, M.; Ceravolo, M.G.; Delargy, M.; Varela Donoso, E.; Kiekens, C.; Christodoulou, N.; Study Group European Framework of Rehabilitation Service Types. European framework of rehabilitation services types: The perspective of the physical and rehabilitation medicine section and board of the European Union of medical specialists. Eur. J. Phys. Rehabil. Med. 2019, 55, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Papoutsi, G. Spreading and scaling up innovation and improvement. BMJ 2019, 365, l2068. [Google Scholar] [CrossRef] [Green Version]
- Weaver, R.H.; Burley, M. Identification of functional, social, and health needs of older residents in nonurban settings: A community risk assessment. J Aging Health 2020, 32, 1614–1624. [Google Scholar] [CrossRef]
- Wolf, D.A.; Freedman, V.A.; Ondrich, J.I.; Seplaki, C.; Spillman, B.C. Disability trajectories at the end of life: A “countdown” model. J. Gerontol. B Psych. Sci. Soc. Sci. 2015, 70, 745–752. [Google Scholar] [CrossRef] [Green Version]
| Age | ADL Dependence | Functional Limitations | Cognitive Impairment | Concerns About Falling | Usability of the Home | |
|---|---|---|---|---|---|---|
| Older adults with low level of disability | Old | Low | Low | No/mild | Low | High (all) |
| Older adults with medium/high level of disability | Old | Medium/High | Medium | Mild | Medium | Self-care: medium Social: medium Leisure: low/medium |
| Adults with low level of disability | Young | Low | Low | Mild/no | High | Self-care: high Social: high Leisure: low/medium |
| Adults of high level of disability | Young | High | High | Mild | High | Self-care: low Social: low Leisure: medium |
| Older adults with medium level of disability and cognitive impairment | Old | Medium | Medium/High | Moderate/Severe | Medium | Medium (all) |
| Total | Older Adults, Low Disability | Older Adults, Medium/High Disability | Adults, Low Disability | Adults, Medium/ High Disability | Cognitive Impairment | ||
|---|---|---|---|---|---|---|---|
| Age (years) | n | 108 | 59 | 26 | 10 | 8 | 5 |
| M (SD) | 75 (13) | 79 (7) | 80 (7) | 49 (6) | 54 (15) | 78 (8) | |
| Gender, n (%) | Male | 29 (27) | 11 (19) | 10 (38) | 3 (30) | 3 (38) | 2 (40) |
| Female | 79 (73) | 48 (81) | 16 (62) | 7 (70) | 5 (63) | 3 (60) | |
| Living situation, n (%) | Alone | 66 (61) | 41 (70) | 13 (50) | 5 (50) | 4 (50) | 3 (60) |
| With someone | 42 (39) | 18 (31) | 13 (50) | 5 (50) | 4 (50) | 2 (40) | |
| Worsening | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| n | % | n | % | |||
| Original client profile | ||||||
| Older adults, low disability | 35 | 69 | 16 | 31 | 1.00 (ref) | 1.00 (ref) |
| Older adults, medium/high disability | 7 | 39 | 11 | 61 | 3.44 (1.13–10.5) | 3.83 (1.02–14.3) |
| Adults, low disability | 7 | 70 | 3 | 30 | 0.94 (0.21–4.10) | 1.22 (0.24–6.10) |
| Adults, medium/high disability | 3 | 60 | 2 | 40 | 1.46 (0.22–9.60) | 9.54 (0.43–209) |
| Cognitive impairment | 2 | 67 | 1 | 33 | 1.09 (0.09–13.0) | 1.40 (0.06–32.0) |
| Aggregated client profiles | ||||||
| Low disability | 42 | 69 | 19 | 31 | 1.00 (ref) | 1.00 (ref) |
| Medium/high disability | 10 | 43 | 13 | 57 | 2.87 (1.07–7.71) | 3.60 (1.01–12.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malmgren Fänge, A.; Chiatti, C.; Axmon, A. One-Year Changes in Activities of Daily Living, Usability, Falls and Concerns about Falling, and Self-Rated Health for Different Housing Adaptation Client Profiles. Int. J. Environ. Res. Public Health 2021, 18, 9704. https://doi.org/10.3390/ijerph18189704
Malmgren Fänge A, Chiatti C, Axmon A. One-Year Changes in Activities of Daily Living, Usability, Falls and Concerns about Falling, and Self-Rated Health for Different Housing Adaptation Client Profiles. International Journal of Environmental Research and Public Health. 2021; 18(18):9704. https://doi.org/10.3390/ijerph18189704
Chicago/Turabian StyleMalmgren Fänge, Agneta, Carlos Chiatti, and Anna Axmon. 2021. "One-Year Changes in Activities of Daily Living, Usability, Falls and Concerns about Falling, and Self-Rated Health for Different Housing Adaptation Client Profiles" International Journal of Environmental Research and Public Health 18, no. 18: 9704. https://doi.org/10.3390/ijerph18189704






