Effects of Relaxed Lockdown on Pediatric ER Visits during SARS-CoV-2 Pandemic in Italy
Abstract
1. Introduction
2. Materials and Methods
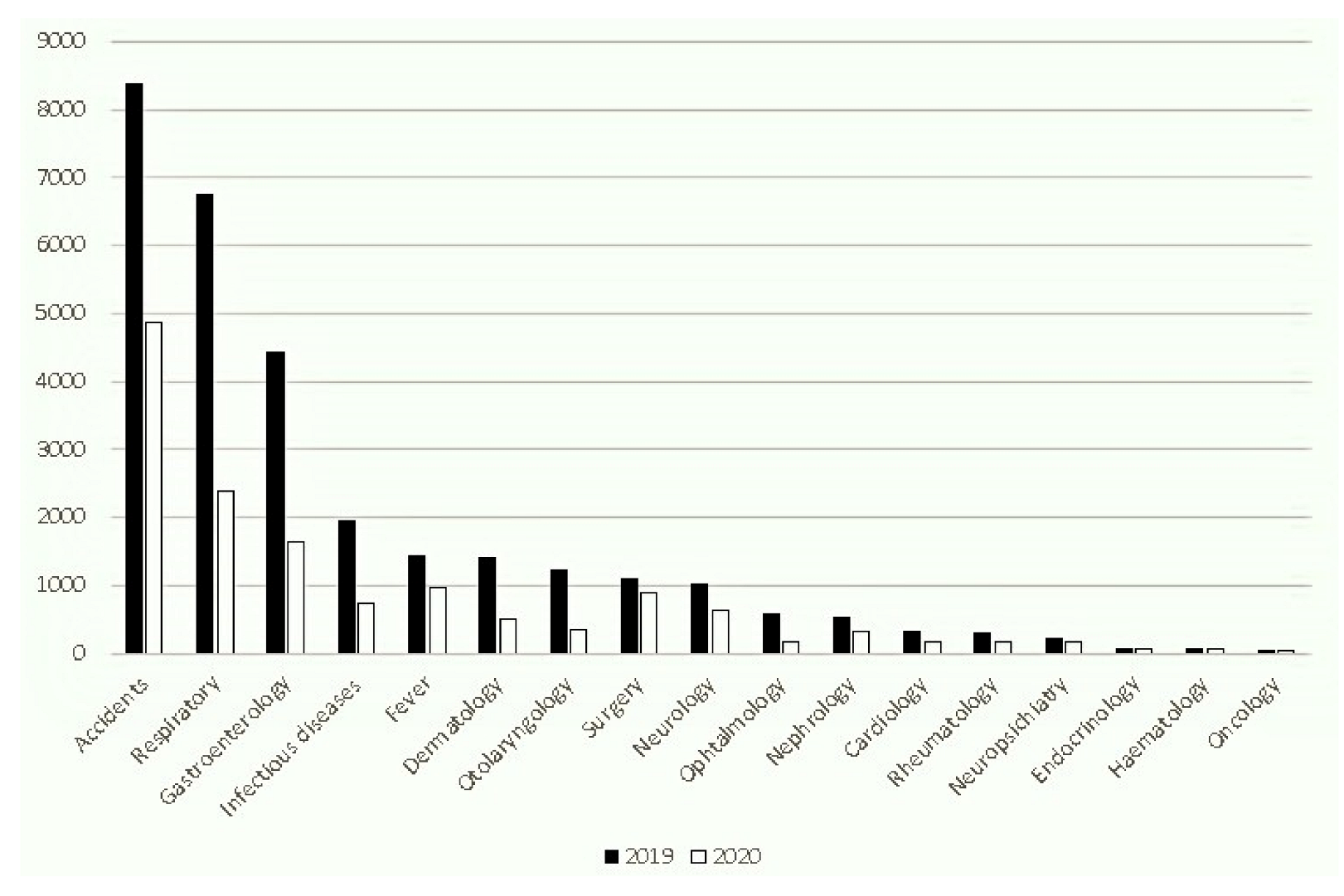
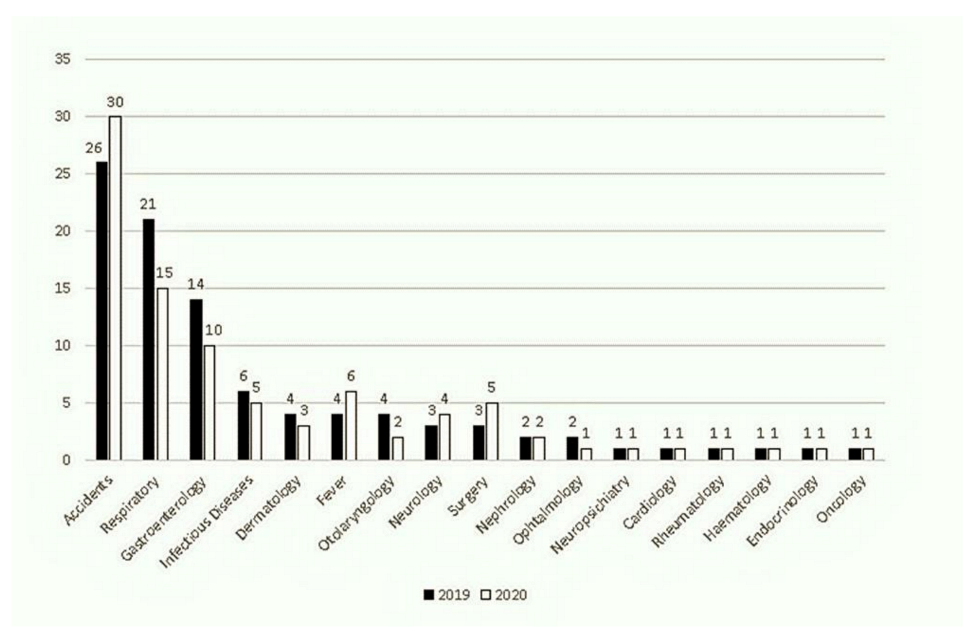
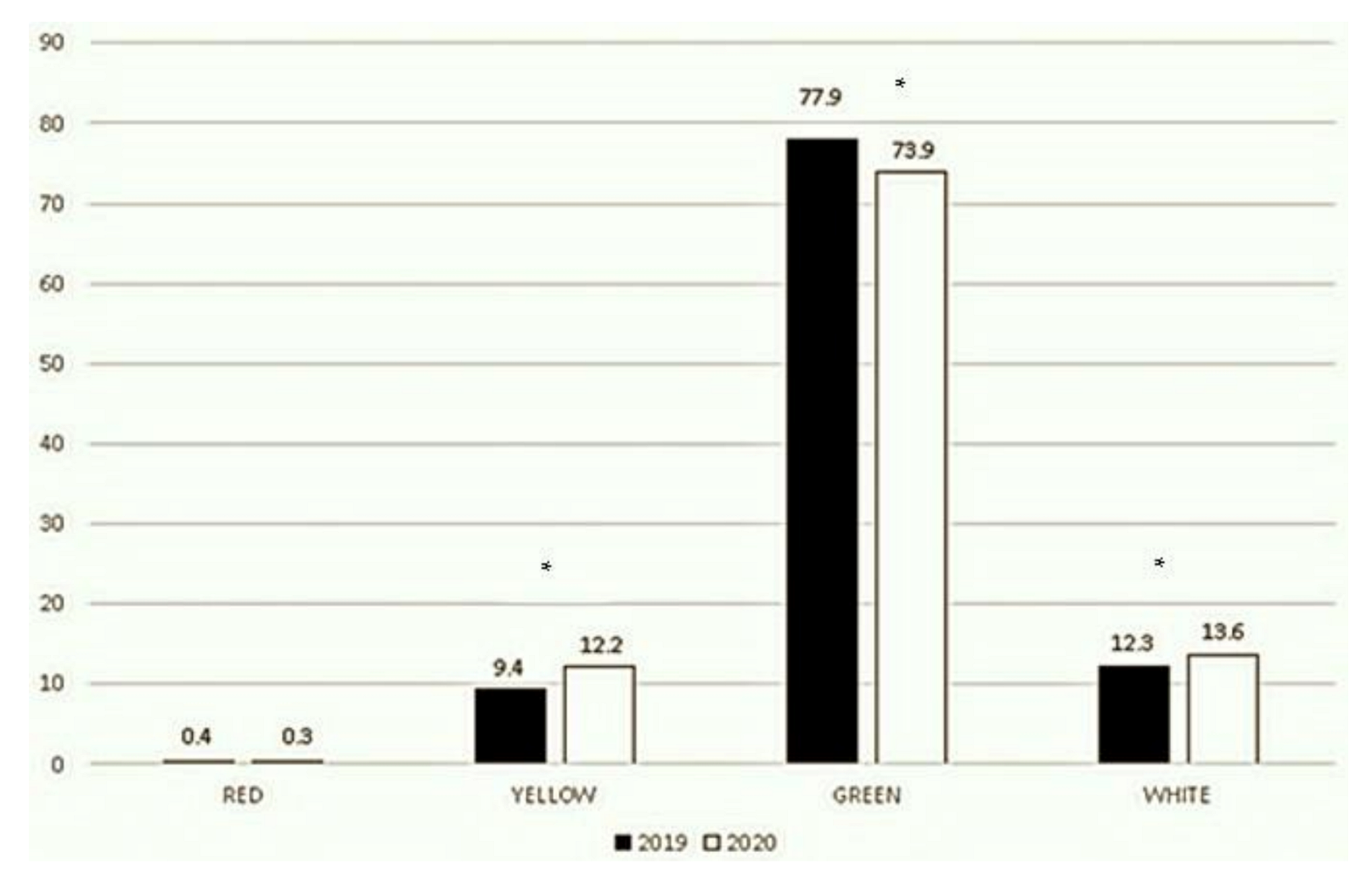
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Director—General’s Openings Remarks at the Media Briefing on COVID-19. 11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/whodirector-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 29 August 2021).
- Istituto Superiore di Sanità. Epicentro. Epidemia COVID-19. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard (accessed on 29 August 2021).
- Decreto del Presidente del Consiglio dei Ministri. 9 March 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg (accessed on 29 August 2021).
- Decreto del Presidente del Consiglio dei Ministri. 26 April 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/04/27/20A02352/sg (accessed on 29 August 2021).
- Decreto del Presidente del Consiglio dei Ministri. 7 August 2020. Available online: https://www.gazzettaufficiale.it/eli/id/2020/08/08/20A04399/sg (accessed on 29 August 2021).
- Matera, L.; Nenna, R.; Rizzo, V.; Ardenti Morini, F.; Banderali, G.; Calvani, M.; Calvi, M.; Cozzi, G.; Fabiani, E.; Falsaperla, R.; et al. SARS-CoV-2 Pandemic Impact on Pediatric Emergency Rooms: A Multicenter Study. Int. J. Environ. Res. Public Health 2020, 17, 8753. [Google Scholar] [CrossRef]
- Li, H.; Yu, G.; Duan, H.; Fu, J.; Shu, Q. Changes in Children’s Healthcare Visits During Coronavirus Disease-2019 Pandemic in Hangzhou, China. J. Pediatr. 2020, 224, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Ojetti, V.; Covino, M.; Brigida, M.; Petruzziello, C.; Saviano, A.; Migneco, A.; Candelli, M.; Franceschi, F. Non-COVID Diseases during the Pandemic: Where Have All Other Emergencies Gone? Medicina 2020, 56, 512. [Google Scholar] [CrossRef] [PubMed]
- Casalino, E.; Choquet, C.; Bouzid, D.; Peyrony, O.; Curac, S.; Fontaine, J.P.; Plaisance, P.; Chauvin, A.; Ghazali, D.A. Analysis of Emergency Department Visits and Hospital Activity during Influenza Season, COVID-19 Epidemic, and Lockdown Periods in View of Managing a Future Disaster Risk: A Multicenter Observational Study. Int. J. Environ. Res. Public Health 2020, 17, 8302. [Google Scholar] [CrossRef]
- Baum, A.; Schwartz, M.D. Admissions to Veterans Affairs Hospitals for Emergency Conditions During the COVID-19 Pandemic. JAMA 2020, 324, 96. [Google Scholar] [CrossRef] [PubMed]
- NHS England. A&E Attendances and Emergency Admissions 2019–2020: Adjusted Monthly. A&E Time Series. 2020. Available online: https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-andactivity/ae-attendances-and-emergency-admissions-2019-20/ (accessed on 12 April 2021).
- Castagneto-Gissey, L.; Casella, G.; Russo, M.F.; Del Corpo, G.; Iodice, A.; Lattina, I.; Ferrari, P.; Iannone, I.; Mingoli, A.; La Torre, F. Impact of COVID-19 outbreak on emergency surgery and emergency department admissions: An Italian level 2 emergency department experience. BJS 2020, 107, e374–e375. [Google Scholar] [CrossRef]
- Dopfer, C.; Wetzke, M.; Scharff, A.Z.; Mueller, F.; Dressler, F.; Baumann, U.; Sasse, M.; Hansen, G.; Jablonka, A.; Happle, C. COVID-19 related reduction in pediatric emergency healthcare utilization—A concerning trend. BMC Pediatr. 2020, 20, 427. [Google Scholar] [CrossRef]
- Poole, S.; Brendish, N.J.; Tanner, A.R.; Clark, T.W. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir. Med. 2020, 8, e92–e93. [Google Scholar] [CrossRef]
- Hsieh, C.C.; Lin, C.H.; Wang, W.Y.C.; Pauleen, D.J.; Chen, J.V. The outcome and implications of public precautionary measures in Taiwan—Declining respiratory disease cases in the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 4877. [Google Scholar] [CrossRef]
- Haapanen, M.; Renko, M.; Artama, M.; Kuitunen, I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children—A nationwide register study in Finland. EClinicalMedicine 2021, 34, 100807. [Google Scholar] [CrossRef]
- Angoulvant, F.; Ouldali, N.; Yang, D.D.; Filser, M.; Gajdos, V.; Rybak, A.; Guedj, R.; Soussan-Banini, V.; Basmaci, R.; Lefevre-Utile, A.; et al. Coronavirus disease 2019 pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections—A time series analysis. Clin. Infect. Dis. 2021, 72, 319. [Google Scholar] [CrossRef] [PubMed]
- McBride, J.A.; Eickhoff, J.; Wald, E.R. Impact of COVID-19 quarantine and school cancelation on other common infectious diseases. Pediatr. Infect. Dis. J. 2020, 39, e449–e452. [Google Scholar] [CrossRef]
- Olsen, S.J.; Azziz-Baumgartner, E.; Budd, A.P.; Brammer, L.; Sullivan, S.; Pineda, R.F.; Cohen, C.; Fry, A.M. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1305–1309. [Google Scholar] [CrossRef] [PubMed]
- Kuitunen, I.; Haapanen, M.; Artama, M.; Renko, M. Closing Finnish schools and day care centres had a greater impact on primary care than secondary care emergency department visits. Acta Paediatr. 2020, 110, 937–938. [Google Scholar] [CrossRef] [PubMed]
- Louhiala, P.J.; Jaakkola, N.; Ruotsalainen, R.; Jaakkola, J.J. Form of day care and respiratory infections among Finnish children. Am. J. Public Health 1995, 85, 1109–2212. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cauchemez, S.; Ferguson, N.M.; Wachtel, C.; Tegnell, A.; Saour, G.; Duncan, B.; Nicoll, A. Closure of schools during an influenza pandemic. Lancet Infect. Dis. 2009, 9, 473–481. [Google Scholar] [CrossRef]
- Panuccio, A.; Pinto, L.; Urbino, A.; Lubrano, R.; Guidi, B.; Zampogna, S.; Cantoni, B. I Nuovi Modelli di Triage. In Proceedings of the XII National Congress, Società Italiana di Medicina di Emergenza ed Urgenza Pediatrica (SIMEUP), Padova, Italy, 27–29 October 2016. [Google Scholar]
- Mauro, V.; Lorenzo, M.; Paolo, C.; Sergio, H. Correction to: Treat all COVID 19-positive patients, but do not forget those negative with chronic diseases. Intern. Emerg. Med. 2020, 15, 787–790. [Google Scholar] [CrossRef] [PubMed]
- Hautz, W.E.; Sauter, T.C.; Exadakytlos, A.K.; Krummrey, G.; Schauber, S.; Müller, M. Barriers to seeking emergency care during the COVID-19 pandemic may lead to higher morbidity and mortality—A retrospective study from a Swiss university hospital. Swiss Med. Wkly. 2020, 150, 20331. [Google Scholar] [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Lo Coco, G.; Gentile, A.; Bosnar, K.; Milovanoviic, I.; Bianco, A.; Drid, P.; Pišot, S. A Cross-Country Examination on the Fear of COVID-19 and the Sense of Loneliness during the First Wave of COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 2586. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Lynn, R.M.; Avis, J.L.; Lenton, S.; Amin-Chowdhury, Z.; Ladhani, S.N. Delayed access to care and late presentations in children during the COVID-19 pandemic: A snapshot survey of 4075 paediatricians in the UK and Ireland. Arch. Dis. Child. 2020, 106, e8. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, M.M.; D’Onofrio, G.; Paek, H.; Platts-Mills, T.F.; Soares, W.E.; Hoppe, J.A.; Genes, N.; Nath, B.; Melnick, E.R. Trends in Emergency Department Visits and Hospital Admissions in Health Care Systems in 5 States in the First Months of the COVID-19 Pandemic in the US. JAMA Intern. Med. 2020, 180, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Thornton, J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ 2020, 369, m1401. [Google Scholar]
- Isba, R.; Edge, R.; Jenner, R.; Broughton, E.; Francis, N.; Butler, J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch. Dis. Child. 2020, 105, 704. [Google Scholar] [CrossRef] [PubMed]
- Akuaake, L.M.; Hendrikse, C.; Spittal, G.; Evans, K.; Van Hoving, D.J. Cross-sectional study of paediatric case mix presenting to an emergency centre in Cape Town, South Africa, during COVID-19. BMJ Paediatr. Open 2020, 4, e000801. [Google Scholar] [CrossRef]
- Ciofi Degli Atti, M.L.; Campana, A.; Muda, A.O.; Concato, C.; Ravà, L.; Ricotta, L.; Reale, A.; Barbieri, M.; D’Argenio, P.; Lancella, L.; et al. Facing SARS-CoV-2 Pandemic at a COVID-19 Regional Children’s Hospital in Italy. Pediatr. Infect. Dis. J. 2020, 39, e221–e225. [Google Scholar] [CrossRef]
- Chaiyachati, B.H.; Agawu, A.; Zorc, J.J.; Balamuth, F. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J. Pediatr. 2020, 226, 274–277.e1. [Google Scholar] [CrossRef]
- Chong, S.L.; Soo, J.S.L.; Allen, J.C.; Ganapathy, S.; Lee, K.P.; Tyebally, A.; Yung, C.F.; Thoon, K.C.; Ng, Y.H.; Oh, J.Y.; et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020, 20, 562. [Google Scholar] [CrossRef]
- Van Brusselen, D.; De Troeyer, K.; Ter Haar, E.; Vander Auwera, A.; Poschet, K.; Van Nuijs, S.; Bael, A.; Stobbelaar, K.; Verhulst, S.; Van Herendael, B.; et al. Bronchiolitis in COVID-19 times: A nearly absent disease? Eur. J. Pediatr. 2021, 180, 1969–1973. [Google Scholar] [CrossRef] [PubMed]
- Scaramuzza, A.; Tagliaferri, F.; Bonetti, L.; Soliani, M.; Morotti, F.; Bellone, S.; Cavalli, C.; Rabbone, I. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch. Dis. Child. 2020, 105, 704–706. [Google Scholar] [CrossRef] [PubMed]
- Silvagni, D.; Baggio, L.; Lo Tartaro Meragliotta, P.; Soloni, P.; La Fauci, G.; Bovo, C.; Ielo, S.; Biban, P. Neonatal and Pediatric Emergency Room Visits in a Tertiary Center during the COVID-19 Pandemic in Italy. Pediatr. Rep. 2021, 13, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Jaehn, P.; Holmberg, C.; Uhlenbrock, G.; Pohl, A.; Finkenzeller, T.; Pawlik, M.T.; Quack, I.; Ernstberger, A.; Rockmann, F.; Schreyer, A.G. Differential trends of admissions in accident and emergency departments during the COVID-19 pandemic in Germany. BMC Emerg. Med. 2021, 21, 42. [Google Scholar] [CrossRef] [PubMed]
- Nourazari, S.; Davis, S.R.; Granovsky, R.; Austin, R.; Straff, D.J.; Joseph, J.W.; Sanchez, L.D. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am. J. Emerg. Med. 2021, 42, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Charlesworth, J.E.G.; Bold, R.; Pal, R. Using ICD-10 diagnostic codes to identify ‘missing’ paediatric patients during nationwide COVID-19 lockdown in Oxfordshire, UK. Eur. J. Pediatr. 2021, 26, 1–15. [Google Scholar]
- Dann, L.; Fitzsimons, J.; Gorman, K.M.; Hourihane, J.; Okafor, I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch. Dis. Child. 2020, 105, 810–811. [Google Scholar] [CrossRef] [PubMed]
- Hon, K.L.; Leung, A.K. Childhood accidents: Injuries and poisoning. Adv. Pediatr. 2010, 57, 33–62. [Google Scholar] [CrossRef]
- Mehta, N.S.; Mytton, O.T.; Mullins, E.W.S.; Fowler, T.A.; Falconer, C.L.; Murphy, O.B.; Langenberg, C.; Jayatunga, W.J.P.; Eddy, D.H.; Nguyen-Van-Tam, J.S. SARS-CoV-2 (COVID-19): What Do We Know About Children? A Systematic Review. Clin. Infect. Dis. 2020, 71, 2469–2479. [Google Scholar] [CrossRef]
- Viner, R.M.; Bonell, C.; Drake, L.; Jourdan, D.; Davies, N.; Baltag, V.; Jerrim, J.; Proimos, J.; Darzi, A. Reopening schools during the COVID-19 pandemic: Governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch. Dis. Child. 2021, 106, 111–113. [Google Scholar] [CrossRef]
- Fontanet, A.; Grant, R.; Greve-Isdahl, M.; Sridhar, D. Covid-19: Keeping schools as safe as possible. BMJ 2021, 372, n524. [Google Scholar] [CrossRef]
- Munro, A.P.S.; Faust, S.N. Children are not COVID-19 super spreaders: Time to go back to school. Arch. Dis. Child. 2020, 105, 618–619. [Google Scholar] [CrossRef]
- Gandini, S.; Rainisio, M.; Iannuzzo, M.L.; Bellerba, F.; Cecconi, F.; Scorrano, L. A cross-sectional and prospective cohort study of the role of schools in the SARS-CoV-2 second wave in Italy. Lancet Reg. Health-Eur. 2021, 5, 100092. [Google Scholar] [CrossRef] [PubMed]
- Heavey, L.; Casey, G.; Kelly, C.; Kelly, D.; McDarby, G. No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020. Eurosurveillance 2020, 25, 2000903. [Google Scholar] [CrossRef] [PubMed]
- Macartney, K.; Quinn, H.E.; Pillsbury, A.J.; Koirala, A.; Deng, L.; Winkler, N.; Katelaris, A.L.; O’Sullivan, M.V.; Dalton, C.; Wood, N.; et al. Transmission of SARS-CoV-2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc. Health 2020, 4, 807–816. [Google Scholar] [CrossRef]
- Ehrhardt, J.; Ekinci, A.; Krehl, H.; Meincke, M.; Finci, I.; Klein, J.; Geisel, B.; Wagner-Wiening, C.; Eichner, M.; Brockmann, S.O. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Württemberg, Germany. Eurosurveillance 2020, 25, 2001587. [Google Scholar] [CrossRef]
- Theuring, S.; Thielecke, M.; van Loon, W.; Hommes, F.; Huelso, C.; von der Haar, A.; Koerner, J.; Schmidt, M.; Boehringer, F.; Mall, M.A.; et al. SARS-CoV-2 infection and transmission in school settings during the second wave in Berlin, Germany: A cross-sectional study. medRxiv 2021. [Google Scholar] [CrossRef]
- Villani, A.; Coltella, L.; Ranno, S.; di Castelbianco, F.B.; Murru, P.M.; Sonnino, R.; Mazzone, T.; Piccioni, L.; Linardos, G.; Chiavelli, S.; et al. School in Italy: A safe place for children and adolescents. Ital. J. Pediatr. 2021, 47, 23. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Magaziotou, I.; Dedoukou, X.; Eleftheriou, E.; Raftopoulos, V.; Michos, A.; Lourida, A.; Panopoulou, M.; Stamoulis, K.; Papaevangelou, V.; et al. Children and Adolescents With SARS-CoV-2 Infection: Epidemiology, Clinical Course and Viral Loads. Pediatr. Infect. Dis. J. 2020, 39, e388–e392. [Google Scholar] [CrossRef]
- Van den Berg, P.; Schechter-Perkins, E.M.; Jack, R.S.; Epshtein, I.; Nelson, R.; Oster, E.; Branch-Elliman, W. Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: A retrospective, state-wide cohort study. Clin. Infect. Dis. 2021, 2021, ciab230. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.A.; Saliba, V.; Lopez Bernal, J.; Ramsay, M.E.; Ladhani, S.N. SARS-CoV-2 infection and transmission in educational settings: A prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect. Dis. 2021, 21, 344–353. [Google Scholar] [CrossRef]
- Willeit, P.; Krause, R.; Lamprecht, B.; Berghold, A.; Hanson, B.; Stelzl, E.; Stoiber, H.; Zuber, J.; Heinen, R.; Köhler, A.; et al. Prevalence of RT-qPCR-detected SARS-CoV-2 infection at schools: First results from the Austrian School-SARS-CoV-2 prospective cohort study. Lancet Reg. Health-Eur. 2021, 5, 100086. [Google Scholar] [CrossRef] [PubMed]
- Krishnaratne, S.; Pfadenhauer, L.M.; Coenen, M.; Geffert, K.; Jung-Sievers, C.; Klinger, C.; Kratzer, S.; Littlecott, H.; Movsisyan, A.; Rabe, J.E.; et al. Measures implemented in the school setting to contain the COVID-19 pandemic: A scoping review. Cochrane Database Syst. Rev. 2020, 12, CD013812. [Google Scholar]
- Couzin-Frankel, J.; Vogel, G.; Weiland, M. School Openings Across Globe Suggest Ways to Keep Coronavirus at Bay, Despite Outbreaks; American Association for the Advancement of Science: Washington, DC, USA, 2020. [Google Scholar]
- Araújo, L.A.; Veloso, C.F.; Souza, M.C.; Azevedo, J.M.C.; Tarro, G. The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J. Pediatr. 2020, 97, 369–377. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; Mázala-de-Oliveira, T.; da Silva Chagas, L.; Raony, Í.; Ferreira, E.S.; Giestal-de-Araujo, E.; Dos Santos, A.A.; Bomfim, P.O.S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110171. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- Kim, E.S.; Kwon, Y.; Choe, Y.H.; Kim, M.J. COVID-19-related school closing aggravate obesity and glucose intolerance in pediatric patients with obesity. Sci. Rep. 2021, 11, 5494. [Google Scholar] [CrossRef] [PubMed]
- Chanchlani, N.; Buchanan, F.; Gill, P.J. Addressing the indirect effects of COVID-19 on the health of children and young people. CMAJ 2020, 192, E921–E927. [Google Scholar] [CrossRef] [PubMed]
- Lachman, P. Where to make a difference: Research and the social determinants in pediatrics and child health in the COVID-19 era. Pediatr. Res. 2021, 89, 259–262. [Google Scholar] [CrossRef]

| Hospital | 2019 | 2020 | p-Value | |
|---|---|---|---|---|
| Umberto I–Rome | 2901 | 1338 | −54% | p < 0.001 |
| San Camillo de Lellis–Rome | 1587 | 711 | −55% | |
| Sant’Eugenio–Rome | 591 | 222 | −52% | |
| Santa Maria Goretti–Latina | 643 | 283 | −56% | |
| Vittorio Emanuele–Catania | 874 | 374 | −57% | |
| San Paolo–Milan | 1489 | 720 | −52% | |
| Burlo Garofalo–Trieste | 3041 | 1894 | −38% | |
| Ponte San Pietro–Bergamo | 1297 | 481 | −63% | |
| Papa Giovanni XXIII–Bergamo | 1952 | 864 | −56% | |
| Santobono-Pausilipon–Naples | 11,062 | 5032 | −54% | |
| Sant’Orsola–Bologna | 2709 | 1941 | −28% | |
| Fabrizio Spaziani–Frosinone | 1323 | 527 | −60% | |
| San Giovanni Battista–Foligno | 625 | 253 | −60% | |
| Gaspare Salesi–Ancona | 2474 | 1448 | −41% | |
| TOTAL | 32,568 | 16,088 | −51% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matera, L.; Nenna, R.; Ardenti Morini, F.; Banderali, G.; Calvani, M.; Calvi, M.; Cozzi, G.; Falsaperla, R.; Guidi, R.; Kantar, A.; et al. Effects of Relaxed Lockdown on Pediatric ER Visits during SARS-CoV-2 Pandemic in Italy. Int. J. Environ. Res. Public Health 2021, 18, 9547. https://doi.org/10.3390/ijerph18189547
Matera L, Nenna R, Ardenti Morini F, Banderali G, Calvani M, Calvi M, Cozzi G, Falsaperla R, Guidi R, Kantar A, et al. Effects of Relaxed Lockdown on Pediatric ER Visits during SARS-CoV-2 Pandemic in Italy. International Journal of Environmental Research and Public Health. 2021; 18(18):9547. https://doi.org/10.3390/ijerph18189547
Chicago/Turabian StyleMatera, Luigi, Raffaella Nenna, Francesca Ardenti Morini, Giuseppe Banderali, Mauro Calvani, Matteo Calvi, Giorgio Cozzi, Raffaele Falsaperla, Roberto Guidi, Ahmad Kantar, and et al. 2021. "Effects of Relaxed Lockdown on Pediatric ER Visits during SARS-CoV-2 Pandemic in Italy" International Journal of Environmental Research and Public Health 18, no. 18: 9547. https://doi.org/10.3390/ijerph18189547
APA StyleMatera, L., Nenna, R., Ardenti Morini, F., Banderali, G., Calvani, M., Calvi, M., Cozzi, G., Falsaperla, R., Guidi, R., Kantar, A., Lanari, M., Lubrano, R., Messini, B., Niccoli, A. A., Tipo, V., Midulla, F., & on behalf of the CICERO Group. (2021). Effects of Relaxed Lockdown on Pediatric ER Visits during SARS-CoV-2 Pandemic in Italy. International Journal of Environmental Research and Public Health, 18(18), 9547. https://doi.org/10.3390/ijerph18189547









