Translation of the Weight-Related Behaviours Questionnaire into a Short-Form Psychosocial Assessment Tool for the Detection of Women at Risk of Excessive Gestational Weight Gain
Abstract
:1. Introduction
The Weight-Related Behaviours Questionnaire
2. Materials and Methods
2.1. Study Design
2.2. Population Sample and Data Collection
2.3. WRB-Q Items and Scales of Measurement
- Weight locus of control (WLOC)—4 questionnaire items (5-point Likert scale ranging from “strongly agree to strongly disagree” with a neutral option where 3 indicates “neither agree or disagree”), indicating whether a woman feels she has control over her body weight (internal WLOC) or if body weight is something a woman feels she has little control over (external WLOC);
- Self-efficacy—8 questionnaire items (5-point Likert scale, “very sure to very unsure”, where 3 indicates “neither sure or unsure”), indicating levels of confidence for diet, exercise and postpartum weight loss behaviour change;
- Attitudes towards weight gain—13 questionnaire items (5-point Likert scale, “strongly agree to strongly disagree”, where 3 is “neither agree or disagree”), indicating personal attitudes towards gaining weight during pregnancy or weight gain avoidance;
- Body image—4 questionnaire items (2 items—4-point scale ranging from “very satisfied to very dissatisfied” with no neutral option and 2 items—reported on a scale of ”too heavy, about right and too light), indicating personal satisfaction with body weight and shape and perception of body weight and shape;
- Feelings about the motherhood role—7 questionnaire items (5-point Likert scale, “strongly agree to strongly disagree”, where 3 is “neither agree or disagree”), indicating positive and negative perceptions of motherhood;
- Career orientation—13 questionnaire items (4-point Likert scale “strongly agree to strongly disagree”, no neutral option), indicating preference towards career or family [27].
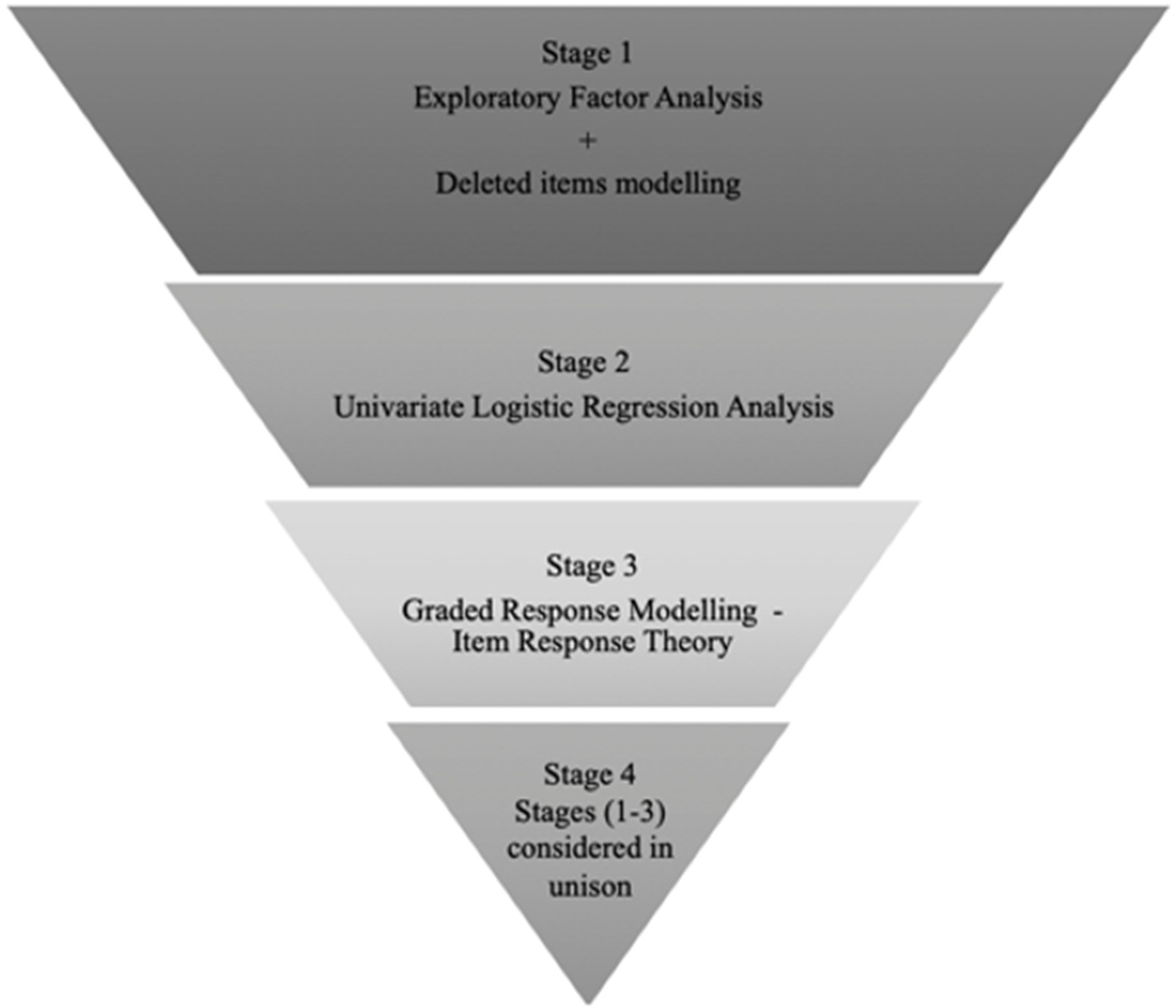
2.4. Scale Reduction Analysis
2.4.1. Stage 1
2.4.2. Stage 2
2.4.3. Stage 3
2.4.4. Stage 4
3. Results
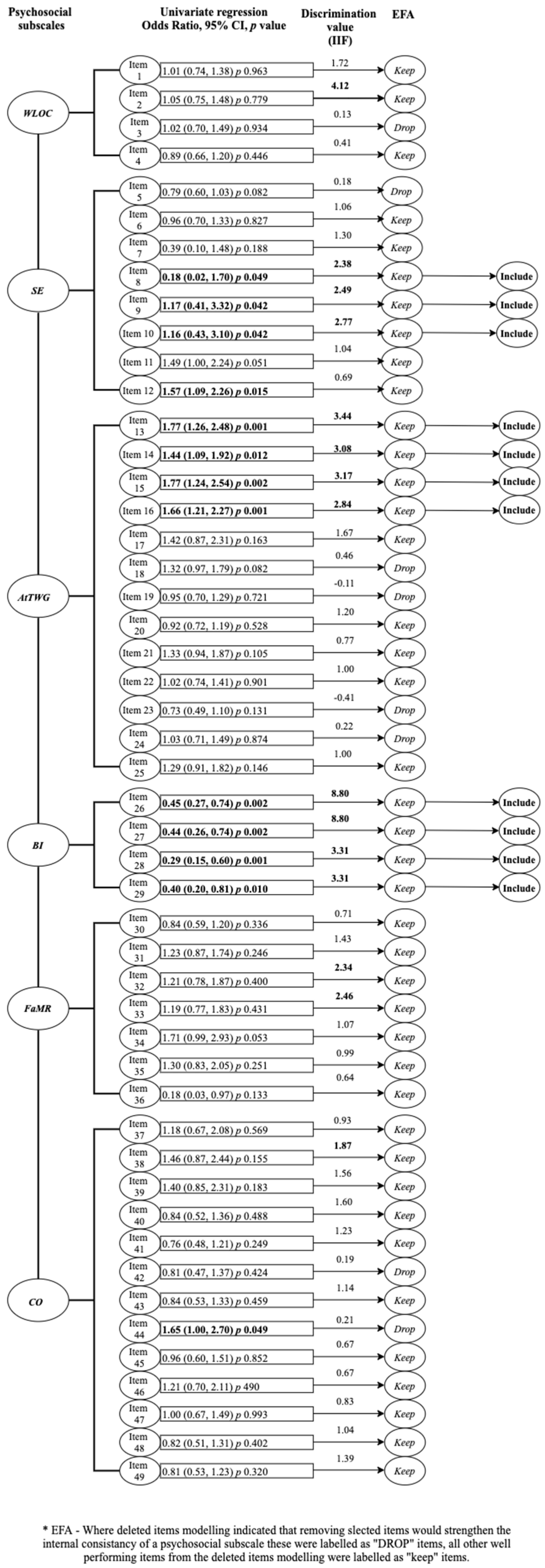
3.1. Stage 1
3.2. Stage 2
3.3. Stage 3
3.4. Stage 4
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Thousanddays.org. 1000 Days. Available online: https://thousanddays.org/ (accessed on 7 September 2020).
- National Health and Medical Research Council. Australian Government Department of Health Clinical Practice Guidelines: Pregnancy Care; Australian Government Department of Health: Canberra, Australia, 2018. [Google Scholar]
- Institute of Medicine (US); National Research Council (US) Committee to Re-examine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Re-examining the Guidelines; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Slater, K.; Rollo, M.E.; Szewczyk, Z.; Ashton, L.; Schumacher, T.; Collins, C. Do the Dietary Intakes of Pregnant Women Attending Public Hospital Antenatal Clinics Align with Australian Guide to Healthy Eating Recommendations? Nutrients 2020, 12, 2438. [Google Scholar] [CrossRef]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef] [PubMed]
- Hutcheon, J.A.; Stephansson, O.; Cnattingius, S.; Bodnar, L.M.; Wikström, A.-K.; Johansson, K. Pregnancy weight gain before diagnosis and risk of preeclampsia: A population-based cohort study in nulliparous women. Hypertension 2018, 72, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.; Voerman, E.; Amiano, P.; Barros, H.; Beilin, L.J.; Bergström, A.; Charles, M.A.; Chatzi, L.; Chevrier, C.; Chrousos, G.P. Impact of maternal body mass index and gestational weight gain on pregnancy complications: An individual participant data meta-analysis of European, North American and Australian cohorts. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 984–995. [Google Scholar] [CrossRef] [PubMed]
- Hedderson, M.M.; Gunderson, E.P.; Ferrara, A. Gestational weight gain and risk of gestational diabetes mellitus. Obstet. Gynecol. 2010, 115, 597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrera, C.; Valenzuela, R.; Chamorro, R.; Bascuñán, K.; Sandoval, J.; Sabag, N.; Valenzuela, F.; Valencia, M.-P.; Puigrredon, C.; Valenzuela, A. The impact of maternal diet during pregnancy and lactation on the fatty acid composition of erythrocytes and breast milk of Chilean women. Nutrients 2018, 10, 839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Safi-Stibler, S.; Gabory, A. Epigenetics and the Developmental Origins of Health and Disease: Parental environment signalling to the epigenome, critical time windows and sculpting the adult phenotype. Semin. Cell Dev. Biol. 2020, 97, 172–180. [Google Scholar] [CrossRef]
- Barker, D.J.P. The developmental origins of adult disease. J. Am. Coll. Nutr. 2004, 23, 588S–595S. [Google Scholar] [CrossRef]
- Nyirenda, M.J.; Byass, P. Pregnancy, programming, and predisposition. Lancet Glob. Health 2019, 7, e404–e405. [Google Scholar] [CrossRef] [Green Version]
- Farpour-Lambert, N.J.; Ells, L.J.; Martinez de Tejada, B.; Scott, C. Obesity and weight gain in pregnancy and postpartum: An evidence review of lifestyle interventions to inform maternal and child health policies. Front. Endocrinol. 2018, 9, 546. [Google Scholar] [CrossRef] [Green Version]
- Fealy, S.; Davis, D.; Foureur, M.; Attia, J.; Hazelton, M.; Hure, A. The return of weighing in pregnancy: A discussion of evidence and practice. Women Birth 2020, 33, 119–124. [Google Scholar] [CrossRef]
- Dolatian, M.; Sharifi, N.; Mahmoodi, Z.; Fathnezhad-kazemi, A.; Bahrami-vazir, E.; Rashidian, T. Weight gain during pregnancy and its associated factors: A Path analysis. Nurs. Open 2020, 7, 1568–1577. [Google Scholar] [CrossRef] [PubMed]
- Bergmeier, H.; Hill, B.; Haycraft, E.; Blewitt, C.; Lim, S.; Meyer, C.; Skouteris, H. Maternal body dissatisfaction in pregnancy, postpartum and early parenting: An overlooked factor implicated in maternal and childhood obesity risk. Appetite 2020, 147, 104525. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; Skouteris, H.; Fuller-Tyszkiewicz, M.; Kothe, E.J.; McPhie, S. A path model of psychosocial and health behaviour change predictors of excessive gestational weight gain. J. Reprod. Infant Psychol. 2016, 34, 139–161. [Google Scholar] [CrossRef]
- Hartley, E.; McPhie, S.; Skouteris, H.; Fuller-Tyszkiewicz, M.; Hill, B. Psychosocial risk factors for excessive gestational weight gain: A systematic review. Women Birth 2015, 28, e99–e109. [Google Scholar] [CrossRef]
- Kapadia, M.Z.; Gaston, A.; Van Blyderveen, S.; Schmidt, L.; Beyene, J.; McDonald, H.; McDonald, S.D. Psychological antecedents of excess gestational weight gain: A systematic review. BMC Pregnancy Childbirth 2015, 15, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Jersey, S.J.; Mallan, K.M.; Callaway, L.K.; Daniels, L.A.; Nicholson, J.M. Prospective relationships between health cognitions and excess gestational weight gain in a cohort of healthy and overweight pregnant women. J. Acad. Nutr. Diet. 2017, 117, 1198–1209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fealy, S.; Attia, J.; Leigh, L.; Oldmeadow, C.; Hazelton, M.; Foureur, M.; Collins, C.; Smith, R.; Hure, A. Demographic and social-cognitive factors associated with gestational weight gain in an Australian pregnancy cohort. Eat. Behav. 2020, 101430. [Google Scholar] [CrossRef]
- Fuller-Tyszkiewicz, M.; Skouteris, H.; Watson, B.E.; Hill, B. Body dissatisfaction during pregnancy: A systematic review of cross-sectional and prospective correlates. J. Health Psychol. 2013, 18, 1411–1421. [Google Scholar] [CrossRef]
- Cox, J.; Holden, J.; Sagovsky, R. Edinburgh postnatal depression scale (EPDS). Br J Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Muktabhant, B.; Lawrie, T.A.; Lumbiganon, P.; Laopaiboon, M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst. Rev. 2015, 6, CD007145. [Google Scholar] [CrossRef]
- Vincze, L.; Rollo, M.; Hutchesson, M.; Hauck, Y.; MacDonald-Wicks, L.; Wood, L.; Callister, R.; Collins, C. Interventions including a nutrition component aimed at managing gestational weight gain or postpartum weight retention: A systematic review and meta-analysis. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 297–364. [Google Scholar] [CrossRef] [PubMed]
- Dryer, R.; von der Schulenburg, I.G.; Brunton, R. Body dissatisfaction and Fat Talk during pregnancy: Predictors of distress. J. Affect. Disord. 2020, 267, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Kendall, A.; Olson, C.M.; Frongillo, E.A., Jr. Evaluation of psychosocial measures for understanding weight-related behaviors in pregnant women. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2001, 23, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Saltzer, E.B. The weight locus of control (WLOC) scale: A specific measure for obesity research. J. Personal. Assess. 1982, 46, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.L.; Jennings, G.E.; Massey, L. Development of an assessment form: Attitude toward weight gain during pregnancy. J. Am. Diet. Assoc. 1985, 85, 946–949. [Google Scholar]
- Hofstetter, C.R.; Sallis, J.F.; Hovell, M.F. Some health dimensions of self-efficacy: Analysis of theoretical specificity. Soc. Sci. Med. 1990, 31, 1051–1056. [Google Scholar] [CrossRef]
- Devine, C.M.; Olson, C.M.; Sobal, J.; Acharya, M. Becoming a mother: Perceptions about changes in weight and shape. In Proceedings of the Society for Nutrition Education Annual Meeting, Portland, OR, USA, 18–22 July 1994. [Google Scholar]
- Devine, C.M.; Bove, C.F.; Olson, C.M. Continuity and change in women’s weight orientations and lifestyle practices through pregnancy and the postpartum period: The influence of life course trajectories and transitional events. Soc. Sci. Med. 2000, 50, 567–582. [Google Scholar] [CrossRef]
- Hackley, B.; Kennedy, H.P.; Berry, D.C.; Melkus, G.D.E. A Mixed-Methods Study on Factors Influencing Prenatal Weight Gain in Ethnic-Minority Women. J. Midwifery Women’s Health 2014, 59, 388–398. [Google Scholar] [CrossRef]
- McDonald, S.D.; Park, C.K.; Timm, V.; Schmidt, L.; Neupane, B.; Beyene, J. What Psychological, Physical, Lifestyle, And Knowledge Factors Are Associated With Excess or Inadequate Weight Gain During Pregnancy? A Cross-Sectional Survey. J. Obstet. Gynaecol. Can. 2013, 35, 1071–1082. [Google Scholar] [CrossRef]
- Van der Wijden, C.L.; Steinbach, S.; van der Ploeg, H.P.; van Mechelen, W.; van Poppel, M.N.M. A longitudinal study on the relationship between eating style and gestational weight gain. Appetite 2014, 83, 304–308. [Google Scholar] [CrossRef]
- Hinton, P.S.; Olson, C.M. Postpartum exercise and food intake: The Importance of behavior-specific self-efficacy. J. Am. Diet. Assoc. 2001, 101, 1430–1437. [Google Scholar] [CrossRef]
- Hinton, P.S.; Olson, C.M. Predictors of Pregnancy-Associated Change in Physical Activity in a Rural White Population. Matern. Child Health J. 2001, 5, 7–14. [Google Scholar] [CrossRef]
- Lipsky, L.M.; Strawderman, M.S.; Olson, C.M. Weight-related self-efficacy in relation to maternal body weight from early pregnancy to 2 years post-partum. Matern. Child Nutr. 2016, 12, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Légaré, F.; Ratté, S.; Gravel, K.; Graham, I.D. Barriers and facilitators to implementing shared decision-making in clinical practice: Update of a systematic review of health professionals’ perceptions. Patient Educ. Couns. 2008, 73, 526–535. [Google Scholar] [CrossRef]
- Connell, T.; Barnett, B.; Waters, D. Barriers to antenatal psychosocial assessment and depression screening in private hospital settings. Women Birth 2018, 31, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Ockenden, H.; Gunnell, K.; Giles, A.; Nerenberg, K.; Goldfield, G.; Manyanga, T.; Adamo, K. Development and preliminary validation of a comprehensive questionnaire to assess women’s knowledge and perception of the current weight gain guidelines during pregnancy. Int. J. Environ. Res. Public Health 2016, 13, 1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hure, A.; Collins, C.; Giles, W.; Wright, I.; Smith, R. Protocol for the Women And Their Children’s Health (WATCH) Study: A Cohort of Pregnancy and Beyond. J. Epidemiol. 2012, 22, 267–275. [Google Scholar] [CrossRef]
- Kaushik, V.; Walsh, C.A. Pragmatism as a research paradigm and its implications for social work research. Soc. Sci. 2019, 8, 255. [Google Scholar] [CrossRef]
- Fealy, S.; Attia, J.; Leigh, L.; Oldmeadow, C.; Hazelton, M.; Foureur, M.; Collins, C.; Smith, R.; Hure, A. A revalidation of the Weight-Related Behaviours Questionnaire within an Australian pregnancy cohort. Midwifery 2021, 97, 102951. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53. [Google Scholar] [CrossRef]
- Edelen, M.O.; Reeve, B.B. Applying item response theory (IRT) modeling to questionnaire development, evaluation, and refinement. Qual. Life Res. 2007, 16, 5. [Google Scholar] [CrossRef]
- Verhoeven, K.J.; Simonsen, K.L.; McIntyre, L.M. Implementing false discovery rate control: Increasing your power. Oikos 2005, 108, 643–647. [Google Scholar] [CrossRef]
- Riquin, E.; Lamas, C.; Nicolas, I.; Lebigre, C.D.; Curt, F.; Cohen, H.; Legendre, G.; Corcos, M.; Godart, N. A key for perinatal depression early diagnosis: The body dissatisfaction. J. Affect. Disord. 2019, 245, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Shikora, S. Fighting Weight Bias and Obesity Stigma: A Call for Action. Obes. Surg. 2020, 30, 1623–1624. [Google Scholar] [CrossRef] [PubMed]
- Vanstone, M.; Kandasamy, S.; Giacomini, M.; DeJean, D.; McDonald, S.D. Pregnant women’s perceptions of gestational weight gain: A systematic review and meta-synthesis of qualitative research. Matern. Child Nutr. 2017, 13, e12374. [Google Scholar] [CrossRef] [PubMed]
- De Jersey, S.J.; Guthrie, T.; Tyler, J.; Ling, W.Y.; Powlesland, H.; Byrne, C.; New, K. A mixed method study evaluating the integration of pregnancy weight gain charts into antenatal care. Matern. Child Nutr. 2019, 15, e12750. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.; Ginsburg, G.; Simmons, L. Personalized medicine in women’s obesity prevention and treatment: Implications for research, policy and practice. Obes. Rev. 2013, 14, 145–161. [Google Scholar] [CrossRef]
- Sahin, A.; Anil, D. The effects of test length and sample size on item parameters in item response theory. Educ. Sci. Theory Pract. 2017, 17, 321–335. [Google Scholar] [CrossRef] [Green Version]
| Self-Efficacy How Sure Are You That You Can? | Very Sure | Sure | Neither Sure nor Unsure | Unsure | Very Unsure |
|---|---|---|---|---|---|
| Eat balanced meals | 1 | 2 | 3 | 4 | 5 |
| Eat foods that are good for you & avoid foods that are not. | 1 | 2 | 3 | 4 | 5 |
| Eat foods that are good for you even when family or social life takes a lot of your time… | 1 | 2 | 3 | 4 | 5 |
| Attitudes towards Weight Gain Circle the Response That Best Represents How You Feel: | Strongly Agree | Agree | Neither Agree nor Disagree | Disagree | Strongly Disagree |
| The weight I gain during my pregnancy makes me feel ugly | 1 | 2 | 3 | 4 | 5 |
| I worry that I may get fat during this pregnancy. | 1 | 2 | 3 | 4 | 5 |
| I am embarrassed at how big I have gotton during this pregnancy. | 1 | 2 | 3 | 4 | 5 |
| I’m embarrassed whenever the nurse weighs me. | 1 | 2 | 3 | 4 | 5 |
| Body Image | |||||
| Circle the Response That Best Represents How You Feel: | Very Satisfied | Satisfied | Dissatisfied | Very Dissatisfied | |
| How satisfied are you with your current shape? | 0 | 1 | 2 | 3 | |
| How satisfied are you with your current weight? | 0 | 1 | 2 | 3 | |
| Too Heavy | About Right | Too Light | |||
| Do you consider your current weight to be… | 0 | 1 | 2 | ||
| Do you consider your current body shape to be… | 0 | 1 | 2 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fealy, S.; Leigh, L.; Hazelton, M.; Attia, J.; Foureur, M.; Oldmeadow, C.; Collins, C.E.; Smith, R.; Hure, A.J. Translation of the Weight-Related Behaviours Questionnaire into a Short-Form Psychosocial Assessment Tool for the Detection of Women at Risk of Excessive Gestational Weight Gain. Int. J. Environ. Res. Public Health 2021, 18, 9522. https://doi.org/10.3390/ijerph18189522
Fealy S, Leigh L, Hazelton M, Attia J, Foureur M, Oldmeadow C, Collins CE, Smith R, Hure AJ. Translation of the Weight-Related Behaviours Questionnaire into a Short-Form Psychosocial Assessment Tool for the Detection of Women at Risk of Excessive Gestational Weight Gain. International Journal of Environmental Research and Public Health. 2021; 18(18):9522. https://doi.org/10.3390/ijerph18189522
Chicago/Turabian StyleFealy, Shanna, Lucy Leigh, Michael Hazelton, John Attia, Maralyn Foureur, Christopher Oldmeadow, Clare E. Collins, Roger Smith, and Alexis J. Hure. 2021. "Translation of the Weight-Related Behaviours Questionnaire into a Short-Form Psychosocial Assessment Tool for the Detection of Women at Risk of Excessive Gestational Weight Gain" International Journal of Environmental Research and Public Health 18, no. 18: 9522. https://doi.org/10.3390/ijerph18189522
APA StyleFealy, S., Leigh, L., Hazelton, M., Attia, J., Foureur, M., Oldmeadow, C., Collins, C. E., Smith, R., & Hure, A. J. (2021). Translation of the Weight-Related Behaviours Questionnaire into a Short-Form Psychosocial Assessment Tool for the Detection of Women at Risk of Excessive Gestational Weight Gain. International Journal of Environmental Research and Public Health, 18(18), 9522. https://doi.org/10.3390/ijerph18189522






