Effectiveness of a Dental Intervention to Improve Oral Health among Home Care Recipients: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Intervention
2.2. Outcome Assessment
2.3. Sample Size Calculation
2.4. Record Linkage
2.5. Statistical Analysis
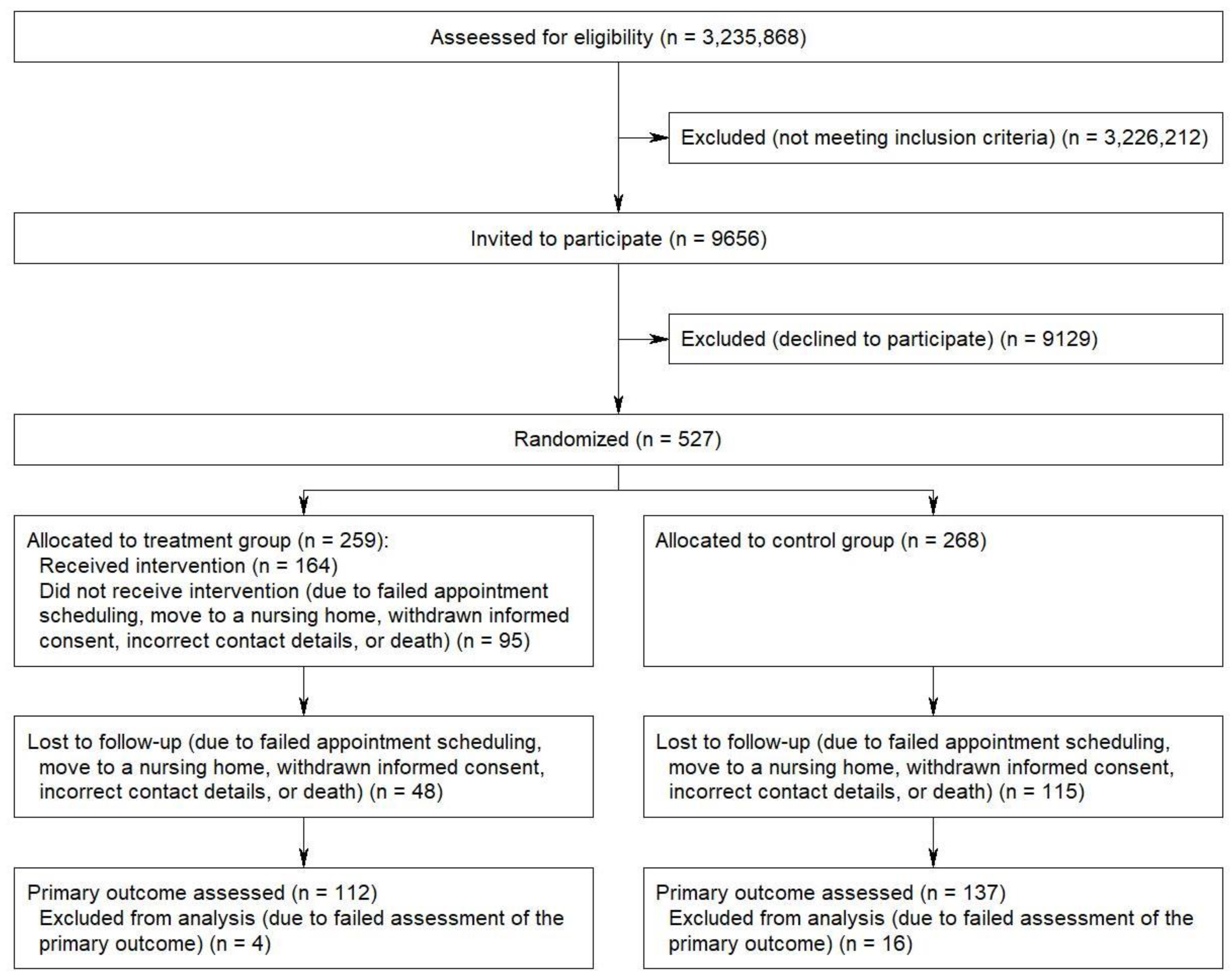
3. Results
3.1. Baseline Characteristics
3.2. Intervention Provided at t0
3.3. Primary Outcome Assessed at t1
3.4. Secondary Outcomes Assessed at t1
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van De Rijt, L.J.M.; Stoop, C.C.; Weijenberg, R.A.F.; De Vries, R.; Feast, A.R.; Sampson, E.L.; Lobbezoo, F. The Influence of Oral Health Factors on the Quality of Life in Older People: A Systematic Review. Gerontologist 2019, 60, e378–e394. [Google Scholar] [CrossRef]
- Zenthöfer, A.; Ehret, J.; Zajac, M.; Kilian, S.; Rammelsberg, P.; Klotz, A.-L. The Effects of Dental Status and Chewing Efficiency on the Oral-Health-Related Quality of Life of Nursing-Home Residents. Clin. Interv. Aging 2020, 15, 2155–2164. [Google Scholar] [CrossRef]
- Lertpimonchai, A.; Rattanasiri, S.; Vallibhakara, S.; Attia, J.; Thakkinstian, A. The association between oral hygiene and periodontitis: A systematic review and meta-analysis. Int. Dent. J. 2017, 67, 332–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffin, S.; Regnier, E.; Griffin, P.; Huntley, V. Effectiveness of Fluoride in Preventing Caries in Adults. J. Dent. Res. 2007, 86, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Göstemeyer, G.; Baker, S.R.; Schwendicke, F. Barriers and facilitators for provision of oral health care in dependent older people: A systematic review. Clin. Oral Investig. 2019, 23, 979–993. [Google Scholar] [CrossRef] [PubMed]
- Kapp, S.; Herzberg, A.; Czwikla, J.; Schmelzer, C.; Kalwitzki, T.; Nitschke, I.; Rothgang, H. Mundgesundheit bei Pflegebedürftigen—Wie können Versorgungsmaßnahmen ankommen? Gesundh. Soz. 2018, 72, 23–29. [Google Scholar] [CrossRef]
- Dörfer, C.; Benz, C.; Aida, J.; Campard, G. The relationship of oral health with general health and NCDs: A brief review. Int. Dent. J. 2017, 67, 14–18. [Google Scholar] [CrossRef] [Green Version]
- Van Der Putten, G.-J.; De Visschere, L.; Van Der Maarel-Wierink, C.; Vanobbergen, J.; Schols, J. The importance of oral health in (frail) elderly people—A review. Eur. Geriatr. Med. 2013, 4, 339–344. [Google Scholar] [CrossRef]
- Van Lancker, A.; Verhaeghe, S.; Van Hecke, A.; Vanderwee, K.; Goossens, J.; Beeckman, D. The association between malnutrition and oral health status in elderly in long-term care facilities: A systematic review. Int. J. Nurs. Stud. 2012, 49, 1568–1581. [Google Scholar] [CrossRef] [PubMed]
- Wong, F.M.F.; Ng, Y.T.Y.; Leung, W.K. Oral Health and Its Associated Factors Among Older Institutionalized Residents—A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 4132. [Google Scholar] [CrossRef] [Green Version]
- Maille, G.; Serre, B.S.; Ferrandez, A.-M.; Ruquet, M. Use of care and the oral health status of people aged 60 years and older in France: Results from the National Health and Disability Survey. Clin. Interv. Aging 2017, 12, 1159–1166. [Google Scholar] [CrossRef] [Green Version]
- Zenthöfer, A.; Baumgart, D.; Cabrera, T.; Rammelsberg, P.; Schröder, J.; Corcodel, N.; Hassel, A.J. Poor dental hygiene and periodontal health in nursing home residents with dementia: An observational study. Odontology 2017, 105, 208–213. [Google Scholar] [CrossRef]
- Nitschke, I.; Micheelis, W. Krankheits- und Versorgungsprävalenzen bei Älteren Senioren mit Pflegebedarf. In Fünfte Deutsche Mundgesundheitsstudie (DMS V); Jordan, A.R., Micheelis, W., Eds.; Deutscher Zahnärzte Verlag DÄV: Köln, Germany, 2016; pp. 557–578. [Google Scholar]
- Rothgang, H.; Müller, R.; Mundhenk, R.; Unger, R. BARMER GEK Pflegereport 2014: Schwerpunkt: Zahnärztliche Versorgung Pflegebedürftiger; Asgard-Verlagsservice GmbH: Siegburg, Germany, 2014. [Google Scholar]
- Hertrampf, K.; Schlattmann, P.; Meyer, G.; Gassmann, G.; Abraham, J.; Hammen, V.; Schwendicke, F. Oral health improvement for nursing home residents through delegated remotivation and reinstruction (MundZaRR Study): Study protocol of a cluster-randomised controlled trial. BMJ Open 2020, 10, e035999. [Google Scholar] [CrossRef] [PubMed]
- Hoben, M.; Kent, A.; Kobagi, N.; Huynh, K.T.; Clarke, A.; Yoon, M.N. Effective strategies to motivate nursing home residents in oral care and to prevent or reduce responsive behaviors to oral care: A systematic review. PLoS ONE 2017, 12, e0178913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albrecht, M.; Kupfer, R.; Reissmann, D.R.; Mühlhauser, I.; Köpke, S. Oral health educational interventions for nursing home staff and residents. Cochrane Database Syst. Rev. 2016, 9, CD010535. [Google Scholar] [CrossRef]
- Strömberg, E.; Hagman-Gustafsson, M.; Holmén, A.; Wårdh, I.; Gabre, P. Oral status, oral hygiene habits and caries risk factors in home-dwelling elderly dependent on moderate or substantial supportive care for daily living. Community Dent. Oral Epidemiol. 2011, 40, 221–229. [Google Scholar] [CrossRef]
- Dolan, T.A.; Atchison, K.; Huynh, T.N. Access to Dental Care among Older Adults in the United States. J. Dent. Educ. 2005, 69, 961–974. [Google Scholar] [CrossRef] [PubMed]
- OECD. Who Cares? Attracting and Retaining Care Workers for the Elderly; OECD Health Policy Studies; OECD Publishing: Paris, France, 2020.
- Nitschke, I.; Hahnel, S.; Jockusch, J. Health-Related Social and Ethical Considerations towards the Utilization of Dental Medical Services by Seniors: Influencing and Protective Factors, Vulnerability, Resilience and Sense of Coherence. Int. J. Environ. Res. Public Health 2021, 18, 2048. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Zahnärztinnen und Zahnärzte (Primärquelle: Mitgliederstatistiken der (Landes-) Zahnärztekammern, Bundeszahnärztekammer Arbeitsgemeinschaft der Deutschen Zahnärztekammern e.V.). Available online: www.gbe-bund.de (accessed on 24 September 2019).
- Chalmers, J.M.; King, P.L.; Spencer, A.J.; Wright, F.A.C.; Carter, K. The Oral Health Assessment Tool—Validity and reliability. Aust. Dent. J. 2005, 50, 191–199. [Google Scholar] [CrossRef] [Green Version]
- Klotz, A.-L.; Zajac, M.; Ehret, J.; Hassel, A.J.; Rammelsberg, P.; Zenthöfer, A. Development of a German version of the Oral Health Assessment Tool. Aging Clin. Exp. Res. 2019, 32, 165–172. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Miglioretti, D.L.; LeResche, L.; Koepsell, T.D.; Hujoel, P.; Micheelis, W. German short forms of the Oral Health Impact Profile. Community Dent. Oral Epidemiol. 2006, 34, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Meyle, J.; Jepsen, S. Der parodontale screening-index (PSI). Parodontologie 2000, 11, 17–21. [Google Scholar]
- Ziebolz, D.; Szabadi, I.; Rinke, S.; Hornecker, E.; Mausberg, R.F. Initial periodontal screening and radiographic findings—A comparison of two methods to evaluate the periodontal situation. BMC Oral Health 2011, 11, 3. [Google Scholar] [CrossRef] [Green Version]
- Simpelaere, I.S.; Van Nuffelen, G.; Vanderwegen, J.; Wouters, K.; DE Bodt, M. Oral health screening: Feasibility and reliability of the oral health assessment tool as used by speech pathologists. Int. Dent. J. 2016, 66, 178–189. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. Pflegestatistik 2013. Pflege im Rahmen der Pflegeversicherung. Deutschlandergebnisse; Statistisches Bun-desamt: Wiesbaden, Germany, 2015.
- Kapp, S.; Herzberg, A.; Czwikla, J.; Schmelzer, C.; Hoffmann, F.; Nitschke, I.; Rothgang, H. Verbesserung der Mundgesundheit bei Pflegebedürftigen in häuslicher Pflege: Welche weiteren Schritte sind notwendig? Gesundh. Soz. 2020, 74, 33–38. [Google Scholar] [CrossRef]
- Van Ho, B.; Weijenberg, R.A.F.; Van Der Maarel-Wierink, C.D.; Visscher, C.M.; Van Der Putten, G.-J.; Scherder, E.J.A.; Lobbezoo, F. Effectiveness of the implementation project ‘Don’t forget the mouth!’ of community dwelling older people with dementia: A prospective longitudinal single-blind multicentre study protocol (DFTM!). BMC Oral Health 2019, 19, 91. [Google Scholar] [CrossRef]
- Lewis, A.; Kitson, A.; Harvey, G. Improving oral health for older people in the home care setting: An exploratory implementation study. Australas. J. Ageing 2016, 35, 273–280. [Google Scholar] [CrossRef]
- Nitschke, I.; Reiber, T. Orale Gesundheit. In Geriatrie für Hausärzte; Stoppe, G., Mann, E., Eds.; Verlag Hans Huber: Bern, Germany, 2009; pp. 158–167. [Google Scholar]
- Niesten, D.; Gerritsen, A.E.; Leve, V. Barriers and facilitators to integrate oral health care for older adults in general (basic) care in East Netherlands. Part 1: Normative integration. Gerodontology 2021, 38, 154–165. [Google Scholar] [CrossRef]
- Griffin, S.O.; Jones, J.A.; Brunson, D.; Griffin, P.M.; Bailey, W.D. Burden of Oral Disease Among Older Adults and Implications for Public Health Priorities. Am. J. Public Health 2012, 102, 411–418. [Google Scholar] [CrossRef]
- Diese acht Expertenstandards Sollten Sie Kennen. Available online: www.pflegen-online.de/diese-acht-expertenstandards-sollten-sie-kennen (accessed on 5 May 2021).
- Wang, T.-F.; Huang, C.-M.; Chou, C.; Yu, S. Effect of oral health education programs for caregivers on oral hygiene of the elderly: A systemic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 1090–1096. [Google Scholar] [CrossRef]
- De Lugt-Lustig, K.H.; Vanobbergen, J.N.; Van Der Putten, G.-J.; De Visschere, L.M.; Schols, J.M.; De Baat, C. Effect of oral healthcare education on knowledge, attitude and skills of care home nurses: A systematic literature review. Community Dent. Oral Epidemiol. 2014, 42, 88–96. [Google Scholar] [CrossRef]
- Weening, L.; Waal, G.H.-D.; van Dusseldorp, L.; van Achterberg, T.; Schoonhoven, L. Oral health care in older people in long term care facilities: A systematic review of implementation strategies. Int. J. Nurs. Stud. 2013, 50, 569–582. [Google Scholar] [CrossRef] [PubMed]
- Barbe, A.G.; Küpeli, L.S.; Hamacher, S.; Noack, M.J. Impact of regular professional toothbrushing on oral health, related quality of life, and nutritional and cognitive status in nursing home residents. Int. J. Dent. Hyg. 2020, 18, 238–250. [Google Scholar] [CrossRef]
- Schwindling, F.S.; Krisam, J.; Hassel, A.J.; Rammelsberg, P.; Zenthöfer, A. Long-term success of oral health intervention among care-dependent institutionalized seniors: Findings from a controlled clinical trial. Community Dent. Oral Epidemiol. 2017, 46, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Nihtilä, A.; Tuuliainen, E.; Komulainen, K.; Autonen-Honkonen, K.; Nykänen, I.; Hartikainen, S.; Ahonen, R.; Tiihonen, M.; Suominen, A.L. Preventive oral health intervention among old home care clients. Age Ageing 2017, 46, 846–851. [Google Scholar] [CrossRef] [Green Version]
- Gomez-Rossi, J.; Hertrampf, K.; Abraham, J.; Gaßmann, G.; Meyer, G.; Schlattmann, P.; Göstemeyer, G.; Schwendicke, F. Interventions to improve oral health of older people: A scoping review. J. Dent. 2020, 101, 103451. [Google Scholar] [CrossRef] [PubMed]
- Janssens, B.; Vanobbergen, J.; Petrovic, M.; Jacquet, W.; Schols, J.M.; De Visschere, L. The impact of a preventive and curative oral healthcare program on the prevalence and incidence of oral health problems in nursing home residents. PLoS ONE 2018, 13, e0198910. [Google Scholar] [CrossRef] [Green Version]
- Komulainen, K.; Ylöstalo, P.; Syrjälä, A.-M.; Ruoppi, P.; Knuuttila, M.; Sulkava, R.; Hartikainen, S. Oral health intervention among community-dwelling older people: A randomised 2-year intervention study. Gerodontology 2013, 32, 62–72. [Google Scholar] [CrossRef]
- Miegel, K.; Wachtel, T. Improving the oral health of older people in long-term residential care: A review of the literature. Int. J. Older People Nurs. 2009, 4, 97–113. [Google Scholar] [CrossRef] [PubMed]
- Nitschke, I.; Ilgner, A.; Muller, F. Barriers to provision of dental care in long-term care facilities: The confrontation with ageing and death. Gerodontology 2005, 22, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Lauritano, D.; Moreo, G.; Della Vella, F.; Di Stasio, D.; Carinci, F.; Lucchese, A.; Petruzzi, M. Oral Health Status and Need for Oral Care in an Aging Population: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 4558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozas, N.S.; Sadowsky, J.M.; Jeter, C.B. Strategies to improve dental health in elderly patients with cognitive impairment. J. Am. Dent. Assoc. 2017, 148, 236–245.e3. [Google Scholar] [CrossRef]
- Siegel, E.; Cations, M.; Wright, C.; Naganathan, V.; Deutsch, A.; Aerts, L.; Brodaty, H. Interventions to improve the oral health of people with dementia or cognitive impairment: A review of the literature. J. Nutr. Health Aging 2016, 21, 874–886. [Google Scholar] [CrossRef] [PubMed]
| Category | Treatment Group (n = 259) | Control Group (n = 268) | p-Value Assessed in the Treatment Group vs. Assessed in the Control Group | ||||
|---|---|---|---|---|---|---|---|
| Primary Outcome Assessed (n = 112) | Primary Outcome Not Assessed (n = 147) | p-Value Assessed vs. Not Assessed | Primary Outcome Assessed (n = 137) | Primary Outcome Not Assessed (n = 131) | p-Value Assessed vs. Not Assessed | ||
| % | % | % | % | ||||
| Sex | |||||||
| male | 42.9 | 54.4 | 53.3 | 47.3 | |||
| female | 57.1 | 45.6 | 0.0652 | 46.7 | 52.7 | 0.3296 | 0.1015 |
| Age group | |||||||
| <60 years | 25.0 | 12.2 | 25.5 | 16.8 | |||
| 60–74 years | 25.0 | 17.0 | 24.1 | 16.0 | |||
| 75–84 years | 34.8 | 41.5 | 31.4 | 38.2 | |||
| 85+ years | 15.2 | 29.3 | 0.0029 | 19.0 | 29.0 | 0.0406 | 0.8580 |
| mean (SD) | 69.2 (18.4) | 76.6 (14.5) | 0.0003 | 68.6 (19.0) | 74.4 (16.5) | 0.0036 | 0.9647 |
| Long-term care grade | |||||||
| 1/2 | 50.0 | 48.3 | 56.2 | 45.0 | |||
| 3 | 26.8 | 31.3 | 29.2 | 27.5 | |||
| 4/5 | 23.2 | 20.4 | 0.7015 | 14.6 | 27.5 | 0.0297 | 0.2179 |
| Type of LTC benefits | |||||||
| only informal care | 76.8 | 72.1 | 74.5 | 74.0 | |||
| also formal care | 23.2 | 27.9 | 0.3945 | 25.5 | 26.0 | 0.9393 | 0.6702 |
| Category | Treatment Group (n = 112) | Control Group (n = 137) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| 0 = Healthy | 1 = Changes | 2 = UnHealthy | 0 = Healthy | 1 = Changes | 2 = Unhealthy | ||
| % | % | % | % | % | % | ||
| Lips | 90.2 | 8.0 | 1.8 | 83.8 | 14.7 | 1.5 | 0.2693 |
| Tongue | 79.1 | 18.2 | 2.7 | 75.9 | 21.2 | 2.9 | 0.8901 |
| Gums and tissues | 57.7 | 33.3 | 9.0 | 45.6 | 38.2 | 16.2 | 0.1015 |
| Saliva | 67.9 | 22.3 | 9.8 | 75.9 | 21.2 | 2.9 | 0.0651 |
| Natural teeth a | 48.9 | 40.2 | 10.9 | 48.7 | 35.0 | 16.2 | 0.4867 |
| Dentures b | 59.7 | 31.2 | 9.1 | 61.0 | 26.8 | 12.2 | 0.7311 |
| Oral cleanliness | 50.9 | 34.8 | 14.3 | 38.0 | 37.2 | 24.8 | 0.0534 |
| Dental pain | 92.9 | 7.1 | 0.0 | 88.2 | 8.8 | 2.9 | 0.1971 |
| Dimension and Item | Treatment Group (n = 112) | Control Group (n = 137) | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 = Never | 1 = Hardly Ever | 2 = Occa-sionally | 3 = Fairly Often | 4 = Very Often | 0 = Never | 1 = Hardly Ever | 2 = Occa-sionally | 3 = Fairly Often | 4 = Very Often | ||
| % | % | % | % | % | % | % | % | % | % | ||
| Functional limitation | |||||||||||
| Trouble pronouncing words | 73.9 | 12.6 | 7.2 | 0.0 | 6.3 | 75.2 | 9.5 | 8.0 | 2.2 | 5.1 | 0.5243 |
| Taste worse | 75.2 | 10.1 | 3.7 | 6.4 | 4.6 | 75.2 | 5.8 | 10.9 | 1.5 | 6.6 | 0.0389 |
| Physical pain | |||||||||||
| Painful aching | 69.6 | 10.7 | 8.9 | 8.0 | 2.7 | 61.3 | 9.5 | 15.3 | 6.6 | 7.3 | 0.2415 |
| Uncomfortable to eat | 56.3 | 10.7 | 16.1 | 10.7 | 6.3 | 66.4 | 7.3 | 7.3 | 7.3 | 11.7 | 0.0652 |
| Psychological discomfort | |||||||||||
| Self-conscious | 67.0 | 8.9 | 12.5 | 8.0 | 3.6 | 70.8 | 8.8 | 8.0 | 5.1 | 7.3 | 0.4475 |
| Tense | 69.1 | 11.8 | 10.0 | 5.5 | 3.6 | 70.1 | 9.5 | 8.8 | 8.0 | 3.6 | 0.9081 |
| Physical disability | |||||||||||
| Diet unsatisfactory | 76.6 | 10.8 | 4.5 | 3.6 | 4.5 | 83.9 | 6.6 | 1.5 | 4.4 | 3.6 | 0.4111 |
| Interrupt meals | 77.7 | 9.8 | 7.1 | 2.7 | 2.7 | 81.6 | 10.3 | 2.2 | 3.7 | 2.2 | 0.4473 |
| Psychological disability | |||||||||||
| Difficult to relax | 66.7 | 9.0 | 13.5 | 6.3 | 4.5 | 70.6 | 11.0 | 5.1 | 8.1 | 5.1 | 0.2393 |
| Been embarrassed | 70.3 | 14.4 | 9.0 | 3.6 | 2.7 | 74.5 | 6.6 | 10.2 | 5.1 | 3.6 | 0.3511 |
| Social disability | |||||||||||
| Irritable with others | 77.5 | 9.0 | 9.0 | 4.5 | 0.0 | 84.6 | 6.6 | 5.1 | 2.2 | 1.5 | 0.3309 |
| Difficulty doing jobs | 66.4 | 10.9 | 7.3 | 7.3 | 8.2 | 83.9 | 4.4 | 2.9 | 4.4 | 4.4 | 0.0292 |
| Handicap | |||||||||||
| Life unsatisfying | 60.9 | 10.9 | 7.3 | 17.3 | 3.6 | 67.2 | 8.8 | 10.2 | 6.6 | 7.3 | 0.0646 |
| Unable to function | 71.2 | 10.8 | 6.3 | 6.3 | 5.4 | 86.1 | 4.4 | 4.4 | 2.9 | 2.2 | 0.0586 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czwikla, J.; Herzberg, A.; Kapp, S.; Kloep, S.; Rothgang, H.; Nitschke, I.; Haffner, C.; Hoffmann, F. Effectiveness of a Dental Intervention to Improve Oral Health among Home Care Recipients: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 9339. https://doi.org/10.3390/ijerph18179339
Czwikla J, Herzberg A, Kapp S, Kloep S, Rothgang H, Nitschke I, Haffner C, Hoffmann F. Effectiveness of a Dental Intervention to Improve Oral Health among Home Care Recipients: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(17):9339. https://doi.org/10.3390/ijerph18179339
Chicago/Turabian StyleCzwikla, Jonas, Alexandra Herzberg, Sonja Kapp, Stephan Kloep, Heinz Rothgang, Ina Nitschke, Cornelius Haffner, and Falk Hoffmann. 2021. "Effectiveness of a Dental Intervention to Improve Oral Health among Home Care Recipients: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 17: 9339. https://doi.org/10.3390/ijerph18179339
APA StyleCzwikla, J., Herzberg, A., Kapp, S., Kloep, S., Rothgang, H., Nitschke, I., Haffner, C., & Hoffmann, F. (2021). Effectiveness of a Dental Intervention to Improve Oral Health among Home Care Recipients: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(17), 9339. https://doi.org/10.3390/ijerph18179339






