Non-Conveyance Due to Patient-Initiated Refusal in Emergency Medical Services: A Retrospective Population-Based Registry Analysis Study in Riyadh Province, Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Collection
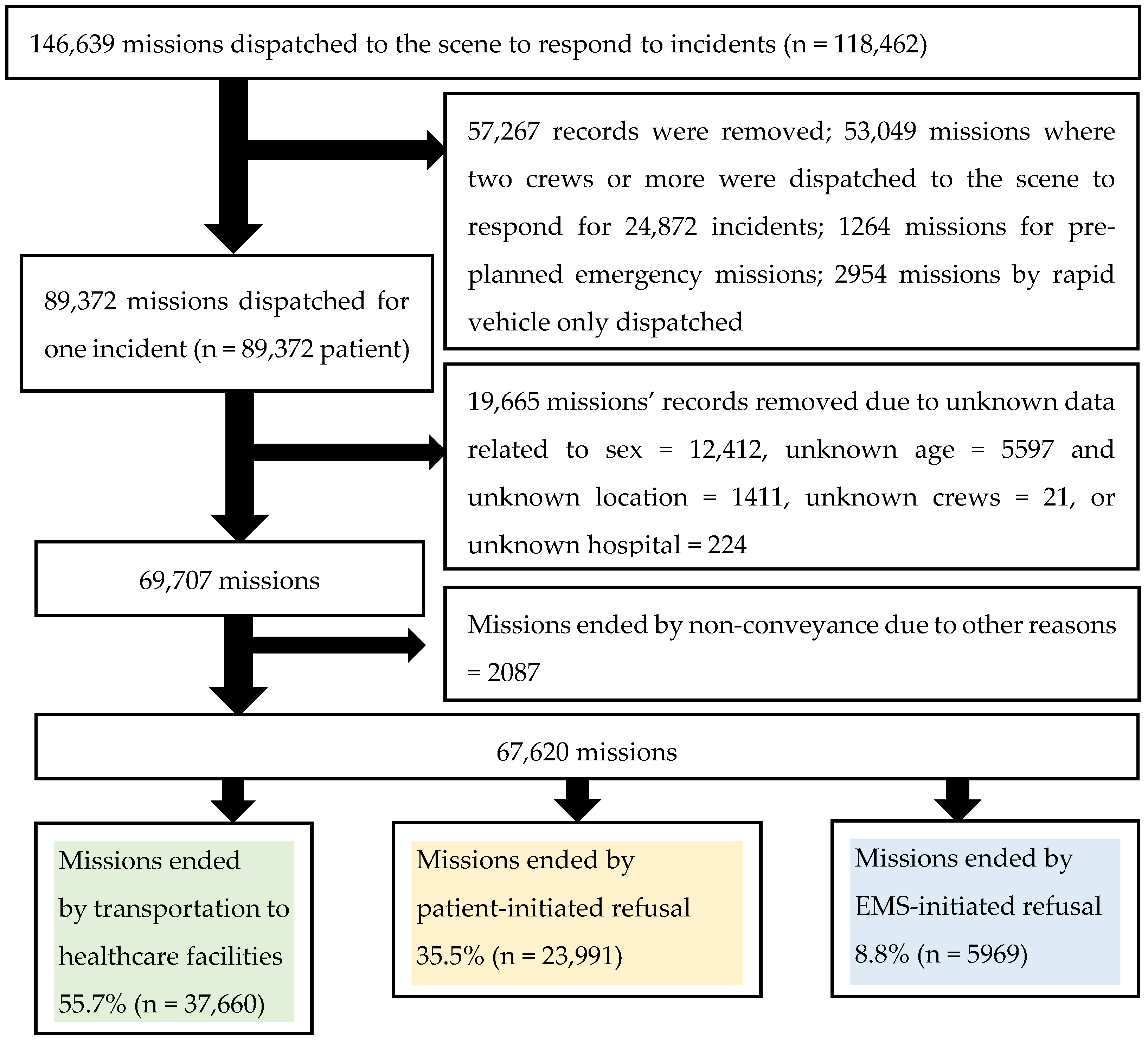
2.3. Selection of Participants
2.4. Methods of Measurement
2.5. Primary Data Analysis
3. Results
3.1. Characteristics of Study Subjects
3.2. Main Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Hara, R.; Johnson, M.; Siriwardena, A.N.; Weyman, A.; Turner, J.; Shaw, D.; Mortimer, P.; Newman, C.; Hirst, E.; Storey, M.; et al. A qualitative study of systemic influences on paramedic decision making: Care transitions and patient safety. J. Health Serv. Res. Policy 2015, 20, 45–53. [Google Scholar] [CrossRef]
- Knapp, B.J.M.D.; Kerns, B.L.M.D.; Riley, I.M.; Powers, J.D.O. EMS-Initiated Refusal of Transport: The Current State of Affairs. J. Emerg. Med. 2009, 36, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.; Minnon, J.; Schneider, S.; Vaughn, J. Prevalence of Methicillin-Resistant Staphylococcus Aureus in Ambulances in Southern Maine. Prehospital Emerg. Care 2010, 14, 176–181. [Google Scholar] [CrossRef]
- Taylor-Robinson, A.W. Contamination of Emergency Medical Vehicles and Risk of Infection to Paramedic First Responders and Patients by Antibiotic-Resistant Bacteria: Risk Evaluation and Recommendations from Ambulance Case Studies. In Healthcare Access-Regional Overviews; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- O’Cathain, A.; Knowles, E.; Bishop-Edwards, L.; Coster, J.; Crum, A.; Jacques, R.; James, C.; Lawson, R.; Marsh, M.; O’Hara, R. Understanding variation in ambulance service non-conveyance rates: A mixed methods study. Health Serv. Deliv. Res. 2018. [Google Scholar] [CrossRef]
- Tohira, H.; Fatovich, D.; Williams, T.A.; Bremner, A.P.; Arendts, G.; Rogers, I.R.; Celenza, A.; Mountain, D.; Cameron, P.; Sprivulis, P.; et al. Is it Appropriate for Patients to be Discharged at the Scene by Paramedics? Prehospital Emerg. Care 2016, 20, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Knight, S.; Olson, L.M.; Cook, L.J.; Mann, N.C.; Corneli, H.M.; Dean, J.M. Against all advice: An analysis of out-of-hospital refusals of care. Ann. Emerg. Med. 2003, 42, 689–696. [Google Scholar] [CrossRef]
- Fraess-Phillips, A.J. Can Paramedics Safely Refuse Transport of Non-Urgent Patients? Prehospital Disaster Med. 2016, 31, 667–674. [Google Scholar] [CrossRef]
- Snooks, H.; Kearsley, N.; Dale, J.; Halter, M.; Redhead, J.; Cheung, W.Y. Towards primary care for non-serious 999 callers: Results of a controlled study of "Treat and Refer" protocols for ambulance crews. Qual. Saf. Health Care 2004, 13, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Lederman, J.; Löfvenmark, C.; Djärv, T.; Lindström, V.; Elmqvist, C. Assessing non-conveyed patients in the ambulance service: A phenomenological interview study with Swedish ambulance clinicians. BMJ Open 2019, 9, e030203. [Google Scholar] [CrossRef]
- Ebben, R.H.A.; Vloet, L.C.M.; Speijers, R.F.; Tönjes, N.W.; Loef, J.; Pelgrim, T.; Hoogeveen, M.; Berben, S.A.A. A patient-safety and professional perspective on non-conveyance in ambulance care: A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 71. [Google Scholar] [CrossRef]
- Hjälte, L.; Suserud, B.O.; Herlitz, J.; Karlberg, I. Why are people without medical needs transported by ambulance? A study of indications for pre-hospital care. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2007, 14, 151–156. [Google Scholar] [CrossRef]
- Hipskind, J.E.; Gren, J.M.; Barr, D.J. Patients who refuse transportation by ambulance: A case series. Prehospital Disaster Med. 2014, 12, 45–50. [Google Scholar] [CrossRef]
- Alicandro, J.; Hollander, J.E.; Henry, M.C.; Sciammarella, J.; Stapleton, E.; Gentile, D. Impact of Interventions for Patients Refusing Emergency Medical Services Transport. Acad. Emerg. Med. 1995, 2, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Keene, T.; Davis, M.; Brook, C. Characteristics and Outcomes of Patients Assessed by Paramedics and Not Transported to Hospital: A Pilot Study. Australas. J. Paramed. 2015, 12. [Google Scholar] [CrossRef]
- Vilke, G.M.; Sardar, W.; Fisher, R.; Dunford, J.D.; Chan, T.C. Follow-up of elderly patients who refuse transport after accessing 9-1-1. Prehospital Emerg. Care 2002, 6, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Kahalé, J.; Osmond, M.H.; Nesbitt, L.; Stiell, I.G. What Are the Characteristics and Outcomes of Nontransported Pediatric Patients? Prehospital Emerg. Care 2006, 10, 28–34. [Google Scholar] [CrossRef]
- O’Cathain, A.; Jacques, R.; Stone, T.; Turner, J. Why do ambulance services have different non-transport rates? A national cross sectional study. PLoS ONE 2018, 13, e0204508. [Google Scholar] [CrossRef] [PubMed]
- Dawoud, S.O.; Ahmad, A.M.; Alsharqi, O.Z.; Al-Raddadi, R.M. Utilization of the Emergency Department and Predicting Factors Associated With Its Use at the Saudi Ministry of Health General Hospitals. Glob. J. Health Sci. 2016, 8, 90–106. [Google Scholar] [CrossRef]
- Moafa, H.N.; van Kuijk, S.M.J.; Alqahtani, D.M.; Moukhyer, M.E.; Haak, H.R. Disparities between Rural and Urban Areas of the Central Region of Saudi Arabia in the Utilization and Time-Centeredness of Emergency Medical Services. Int. J. Environ. Res. Public Health 2020, 17, 7944. [Google Scholar] [CrossRef]
- Alrazeeni, D.M.; Sheikh, S.A.; Mobrad, A.; Al Ghamdi, M.; Abdulqader, N.; Al Gadgab, M.; Al Qahtani, M.; Al Khaldi, B. Epidemiology of non-transported emergency medical services calls in Saudi Arabia. Saudi Med. J. 2016, 37, 575–578. [Google Scholar] [CrossRef]
- Ahmed Ramdan, M.A.; Stuart, W.; John, F.; Amanda, N. Nontransported Cases after Emergency Medical Service Callout in the Rural and Urban Areas of the Riyadh Region. Saudi J. Med. Med. Sci. 2021, 9, 38–44. [Google Scholar]
- The General Authority for Statistics in Saudi Arabia. Saudi Arabian Census Report for 2010. Available online: https://www.stats.gov.sa/en/73 (accessed on 23 May 2021).
- Marks, P.J.; Daniel, T.D.; Afolabi, O.; Spiers, G.; Nguyen-Van-Tam, J.S. Emergency (999) calls to the ambulance service that do not result in the patient being transported to hospital: An epidemiological study. Emerg. Med. J. EMJ 2002, 19, 449–452. [Google Scholar] [CrossRef]
- Dejean, D.; Giacomini, M.; Welsford, M.; Schwartz, L.; Decicca, P. Inappropriate Ambulance Use: A Qualitative Study of Paramedics’ Views. Healthc Policy 2016, 11, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, C.; Ohshige, K.; Kubota, K.; Tochikubo, O. Influence of socioeconomic factors on medically unnecessary ambulance calls. BMC Health Serv. Res. 2007, 7, 120. [Google Scholar] [CrossRef] [PubMed]
- Kirkby, H.M.; Roberts, L.M. Inappropriate 999 calls: An online pilot survey. Emerg. Med. J. 2012, 29, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Marilene Nonnemacher, L.; Denise Elvira Pires de, P.; Soraia Dornelles, S.; Fabricio Pagani, P. Analysis of calls to the Mobile First-Aid Medical Services in a Brazilian capital city. Rev. Rene 2015, 15. [Google Scholar] [CrossRef]
- Hamam, A.F.; Bagis, M.H.; AlJohani, K.; Tashkandi, A.H. Public awareness of the EMS system in Western Saudi Arabia: Identifying the weakest link. Int. J. Emerg. Med. 2015, 8, 35. [Google Scholar]
- Moafa, H.N.; Kuijk, S.; Franssen, G.; Moukhyer, M.E.; Haak, H.R. What is known about the quality of out-of-hospital emergency medical services in the Arabian Gulf States? A systematic review. PLoS ONE 2019, 14, e0226230. [Google Scholar] [CrossRef]
- Ebben, R.H.A.; Castelijns, M.; Frenken, J.; Vloet, L.C.M. Characteristics of non-conveyance ambulance runs: A retrospective study in the Netherlands. World J. Emerg. Med. 2019, 10, 239–243. [Google Scholar] [CrossRef]
- Goldstein, J.; Jensen, J.L.; Carter, A.J.E.; Travers, A.H.; Rockwood, K. The Epidemiology of Prehospital Emergency Responses for Older Adults in a Provincial EMS System. CJEM 2015, 17, 491–496. [Google Scholar] [CrossRef] [PubMed]
- King, R.; Oprescu, F.; Lord, B.; Flanagan, B. Patient experience of non-conveyance following emergency ambulance service response: A scoping review of the literature. Australas. Emerg. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Waldron, R.M.D.; Finalle, C.M.D.; Tsang, J.M.P.H.; Lesser, M.P.; Mogelof, D.M.D. Effect of Gender on Prehospital Refusal of Medical Aid. J. Emerg. Med. 2012, 43, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Holder, P.; Arthur, A.O.; Thiems, G.; Redmon, T.; Thomas, M.; Goodloe, J.M.; Reginald, T.J.; Thomas, S.H. Patients Refusing Prehospital Transport Are Increasingly Likely to Be Geriatric. Emerg. Med. Int. 2012, 2012, 905976. [Google Scholar] [CrossRef] [PubMed]
- Cantwell, K.; Morgans, A.; Smith, K.; Livingston, M.; Dietze, P. Differences in emergency ambulance demand between older adults living in residential aged care facilities and those living in the community in Melbourne, Australia. Australas. J. Ageing 2017, 36, 212–221. [Google Scholar] [CrossRef]
- Evans, C.S.; Platts-Mills, T.F.; Fernandez, A.R.; Grover, J.M.; Cabanas, J.G.; Patel, M.D.; Vilke, G.M.; Brice, J.H. Repeated Emergency Medical Services Use by Older Adults: Analysis of a Comprehensive Statewide Database. Ann. Emerg. Med. 2017, 70, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.M.C.; Wasserman, E.B.; Li, T.; Amidon, A.; Abbott, M.; Shah, M.N. The Effect of Older Age on EMS Use for Transportation to an Emergency Department. Prehospital Disaster Med. 2017, 32, 261–268. [Google Scholar] [CrossRef]
- Platts-Mills, T.F.; Leacock, B.; Cabañas, J.G.; Shofer, F.S.; McLean, S.A. Emergency Medical Services Use by the Elderly: Analysis of a Statewide Database. Prehospital Emerg. Care 2010, 14, 329–333. [Google Scholar] [CrossRef]
- Hjalmarsson, A.; Holmberg, M.; Asp, M.; Östlund, G.; Nilsson, K.W.; Kerstis, B. Characteristic patterns of emergency ambulance assignments for older adults compared with adults requiring emergency care at home in Sweden: A total population study. BMC Emerg. Med. 2020, 20, 94. [Google Scholar] [CrossRef] [PubMed]
- Oosterwold, J.; Sagel, D.; Berben, S.; Roodbol, P.; Broekhuis, M. Factors influencing the decision to convey or not to convey elderly people to the emergency department after emergency ambulance attendance: A systematic mixed studies review. BMJ Open 2018, 8, e021732. [Google Scholar] [CrossRef]
- Verdile, V.P.; Tutsock, G.; Paris, P.M.; Kennedy, R.A. Out-of-Hospital Deliveries: A Five-Year Experience. Prehospital Disaster Med. 1995, 10, 10–13. [Google Scholar] [CrossRef] [PubMed]
- McLelland, G.; Morgans, A.; McKenna, L. Victorian paramedics’ encounters and management of women in labour: An epidemiological study. BMC Pregnancy Childbirth 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Strehlow, M.C.; Newberry, J.A.; Bills, C.B.; Min, H.; Evensen, A.E.; Leeman, L.; Pirrotta, E.A.; Rao, G.V.R.; Mahadevan, S.V. Characteristics and outcomes of women using emergency medical services for third-trimester pregnancy-related problems in India: A prospective observational study. BMJ Open 2016, 6, e011459. [Google Scholar] [CrossRef] [PubMed]
- Khattab, E.; Sabbagh, A.; Aljerian, N.; Binsalleeh, H.; Almulhim, M.; Alqahtani, A.; Alsalamah, M. Emergency medicine in Saudi Arabia: A century of progress and a bright vision for the future. Int. J. Emerg. Med. 2019, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Mandil, A.M.; Alhayyan, R.M.; Alshalawi, A.A.; Alemran, A.S.; Alayed, M.M. Preference of physicians’ gender among male and female primary health care clinic attendees in a university hospital in Saudi Arabia. Saudi Med. J. 2015, 36, 1011. [Google Scholar] [CrossRef]
- Alqufly, A.E.; Alharbi, B.M.; Alhatlany, K.K.; Alhajjaj, F.S. Muslim female gender preference in delaying the medical care at emergency department in Qassim Region, Saudi Arabia. J Fam. Med Prim Care 2019, 8, 1658–1663. [Google Scholar] [CrossRef]
- Snooks, H.A.; Kearsley, N.; Dale, J.; Halter, M.; Redhead, J.; Foster, J. Gaps between policy, protocols and practice: A qualitative study of the views and practice of emergency ambulance staff concerning the care of patients with non-urgent needs. Qual. Saf. Health Care 2005, 14, 251. [Google Scholar] [CrossRef]
- International Federation of Red Cross and Red Crescent Societies. Saudi Red Crescent Authority. Available online: https://www.ifrc.org/en/what-we-do/where-we-work/middle-east-and-north-africa/saudi-arabian-red-crescent-society/ (accessed on 22 June 2021).
| Variable | Number N = 67,620 | Conveyed Cases N = 37,660 (55.7%) & | Patient-Initiated Refusal for Non-Conveyance N= 23,991 (35.5%) & | EMS-Initiated Refusal for Non-Conveyance N = 5969 (8.8%) & |
|---|---|---|---|---|
| Sex | ||||
| Male | 43,258 | 23,823 (55.1) | 15,346 (35.5) | 4089 (9.5) |
| Female | 24,362 | 13,837 (56.8) | 8645 (35.5) | 1880 (7.7) |
| Age category | ||||
| Child ≤ 15 y | 2714 | 1388 (51.1) | 1048 (38.6) | 278 (10.2) |
| Adult | 41,908 | 21,410 (51.1) | 16,205 (38.7) | 4293 (10.2) |
| Elderly ≥ 60 y | 22,998 | 14,862 (64.6) | 6738 (29.3) | 1398 (6.1) |
| Geographical location | ||||
| Riyadh city | 55,991 | 29,494 (52.7) | 21,437 (38.3) | 5060 (9.0) |
| Small cities | 8899 | 6360 (71.5) | 1873 (21.0) | 666 (7.5) |
| Rural ≤ 5000 | 2730 | 1806 (66.2) | 681 (24.9) | 243 (8.9) |
| EMS Shift | ||||
| Daytime | 37,544 | 21,350 (56.9) | 12,982 (34.6) | 3212 (8.6) |
| Nighttime | 30,076 | 16,310 (54.2) | 11,009 (36.6) | 2757 (9.2) |
| Week | ||||
| Weekday | 48,618 | 27,178 (55.9) | 17,264 (35.5) | 4176 (8.6) |
| Weekend | 19,002 | 10,482 (55.2) | 6727 (35.4%) | 1793 (9.4) |
| Time of call | ||||
| Rest time | 50,104 | 27,559 (55.0) | 18,008 (35.9) | 4537 (9.1) |
| Office time | 17,516 | 10,101 (57.7) | 5983 (34.2) | 1432 (8.2) |
| Emergency type | ||||
| Non-emergencies | 26,398 | 15,232 (57.7) | 9227 (35.0) | 1939 (7.3) |
| Medical | 25,817 | 13,241 (51.3) | 10,111(39.2) | 2465 (9.5) |
| Trauma | 14,040 | 8252 (58.8) | 4324 (30.8) | 1464 (10.4) |
| Psychiatric | 697 | 378 (54.2) | 236 (33.9) | 83 (11.9) |
| Gynecological | 668 | 557 (83.4) | 93 (13.9) | 18 (2.7) |
| Crew type | ||||
| BLS | 50,190 | 28,499 (56.8) | 17,365 (34.6) | 4326 (8.6) |
| ALS | 17,430 | 9161 (52.6) | 6626 (38.0) | 1643 (9.4) |
| Urgency level | ||||
| High-priority | 29,447 | 15,893 (54.0) | 10,680 (36.3) | 2874 (9.8) |
| Intermediate | 11,744 | 6516 (55.5) | 4074 (34.7) | 1154 (9.8) |
| Low-priority | 26,429 | 15,251 (57.7) | 9237 (35.0) | 1941 (7.3) |
| Time Line | Conveyed Cases 37,660 | Non-Conveyed Cases 23,991 | p-Value |
|---|---|---|---|
| Response time median (IQR) | 18.3 (13.1–25.5) | 18.8 (13.8–26.0) | < 0.001 |
| On-scene time median (IQR) | 19.3 (12.0–27.5) | 22.2 (15.4–31.8) | < 0.001 |
| Total time † median (IQR) | 39.4 (29.3–51.1) | 43.2 (33.4–55.8) | < 0.001 |
| Variable | N(%) of NC due to PIR, N = 23,991 | Crude | Adjusted * | ||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Sex | |||||
| Male (ref) | 15,346 (64.0) | ||||
| Female | 8645 (36.0) | 0.97 (0.94–1.00) | 0.075 | 1.01 (0.99–1.07) | 0.115 |
| Age | |||||
| Adult (ref) | 1048 (4.4) | ||||
| Child < 15 y | 16,205 (67.5) | 1.00 (0.92–1.08) | 0.954 | 0.96 (0.90–1.06) | 0.560 |
| Elderly ≥ 60 y | 6738 (28.1) | 0.60 (0.58–0.62) | < 0.001 | 0.53 (0.51–0.55) | <0.001 |
| Location | |||||
| Riyadh city (ref) | 21,437 (89.4) | ||||
| Small cities < 500K | 1873 (7.8) | 0.41 (0.38–0.43) | <0.001 | 0.40 (0.38–0.43) | <0.001 |
| Rural ≤ 5000 people | 681 (2.8) | 0.52 (0.47–0.57) | <0.001 | 0.50 (0.45–0.55) | <0.001 |
| EMS Shift | |||||
| Daytime (ref) | 12,982 (54.1) | ||||
| Nighttime | 11,009 (45.9) | 1.11 (1.08–1.15) | <0.001 | 1.05 (1.01–1.09) | 0.007 |
| Week | |||||
| Weekday (ref) | 17,264 (72.0) | ||||
| Weekend | 6727 (28) | 1.01 (0.98–1.05) | 0.577 | 0.99 (0.95–1.03) | 0.538 |
| Time of call | |||||
| Rest time (ref) | 18,008 (75.1) | ||||
| Office time | 5983 (24.9) | 0.91 (0.87–0.94) | <0.001 | 0.94 (0.90–0.99) | 0.009 |
| Emergency type | |||||
| Non-emergencies (ref) | 9227 (38.5) | ||||
| Medical | 10,111 (42.1) | 1.26 (1.21–1.31) | <0.001 | 0.83 (0.38–1.81) | 0.632 |
| Trauma | 4324 (18.0) | 0.87 (0.83–0.91) | <0.001 | 0.48 (0.22–1.05) | 0.065 |
| Psychiatric | 236 (1.0) | 1.03 (0.88–1.22) | 0.719 | 0.48 (0.22–1.07) | 0.074 |
| Gynecological | 93 (0.4) | 0.28 (0.22–0.34) | <0.001 | 0.14 (0.06–0.30) | <0.001 |
| Crews type | |||||
| BLS (ref) | 17,365 (72.4) | ||||
| ALS | 6626 (27.6) | 1.19 (1.14–1.23) | <0.001 | 0.97 (0.93–1.01) | 0.104 |
| Urgency level | |||||
| High priority (ref) | 10,680 (44.5) | ||||
| Intermediate | 4074 (17.0) | 0.93 (0.89–0.97) | 0.002 | 0.99 (0.94–1.04) | 0.706 |
| Low priority | 9237 (38.5) | 0.90 (0.87–0.93) | <0.001 | 0.65 (0.30–1.42) | 0.282 |
| EMS Time | |||||
| Response time | 1.00 (1.00–1.01) | <0.001 | 1.00 (1.00–1.01) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moafa, H.N.; van Kuijk, S.M.J.; Moukhyer, M.E.; Alqahtani, D.M.; Haak, H.R. Non-Conveyance Due to Patient-Initiated Refusal in Emergency Medical Services: A Retrospective Population-Based Registry Analysis Study in Riyadh Province, Saudi Arabia. Int. J. Environ. Res. Public Health 2021, 18, 9252. https://doi.org/10.3390/ijerph18179252
Moafa HN, van Kuijk SMJ, Moukhyer ME, Alqahtani DM, Haak HR. Non-Conveyance Due to Patient-Initiated Refusal in Emergency Medical Services: A Retrospective Population-Based Registry Analysis Study in Riyadh Province, Saudi Arabia. International Journal of Environmental Research and Public Health. 2021; 18(17):9252. https://doi.org/10.3390/ijerph18179252
Chicago/Turabian StyleMoafa, Hassan N., Sander M. J. van Kuijk, Mohammed E. Moukhyer, Dhafer M. Alqahtani, and Harm R. Haak. 2021. "Non-Conveyance Due to Patient-Initiated Refusal in Emergency Medical Services: A Retrospective Population-Based Registry Analysis Study in Riyadh Province, Saudi Arabia" International Journal of Environmental Research and Public Health 18, no. 17: 9252. https://doi.org/10.3390/ijerph18179252
APA StyleMoafa, H. N., van Kuijk, S. M. J., Moukhyer, M. E., Alqahtani, D. M., & Haak, H. R. (2021). Non-Conveyance Due to Patient-Initiated Refusal in Emergency Medical Services: A Retrospective Population-Based Registry Analysis Study in Riyadh Province, Saudi Arabia. International Journal of Environmental Research and Public Health, 18(17), 9252. https://doi.org/10.3390/ijerph18179252






