Increased Use of Porch or Backyard Nature during COVID-19 Associated with Lower Stress and Better Symptom Experience among Breast Cancer Patients
Abstract
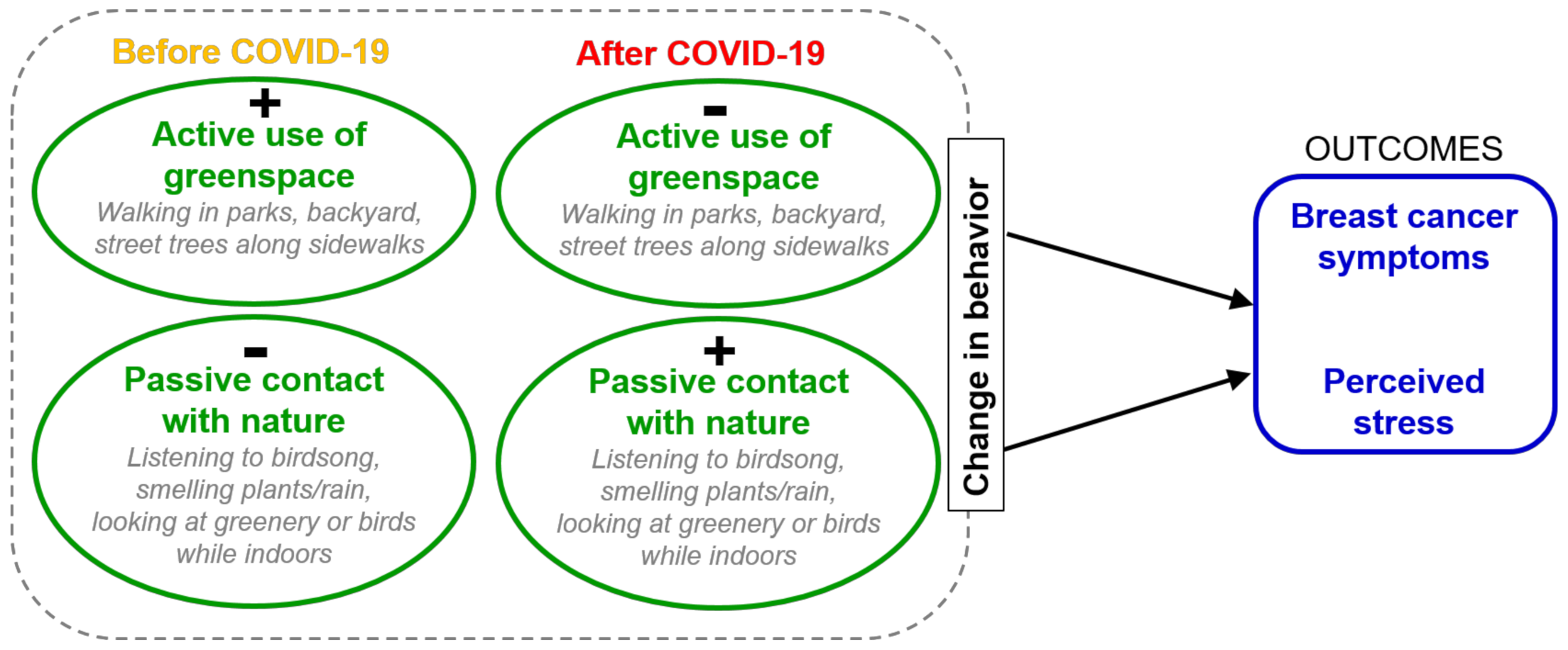
:1. Introduction
- how and to what extent engagement in outdoor physical activity, usage of parks, and at-home contact with nature changed during COVID-19 lockdowns;
- the effects of these changes on perceived stress and symptom experience;
- how physical activity behaviors changed, in order to understand the breadth of impact on activities in this population; and
- alternative indoor or near-home contacts with nature that were substituted for therapeutic outdoor physical activity in public places.
2. Methods
2.1. Survey Instrument
2.2. Statistical and Qualitative Data Analyses
3. Results
3.1. Demographics
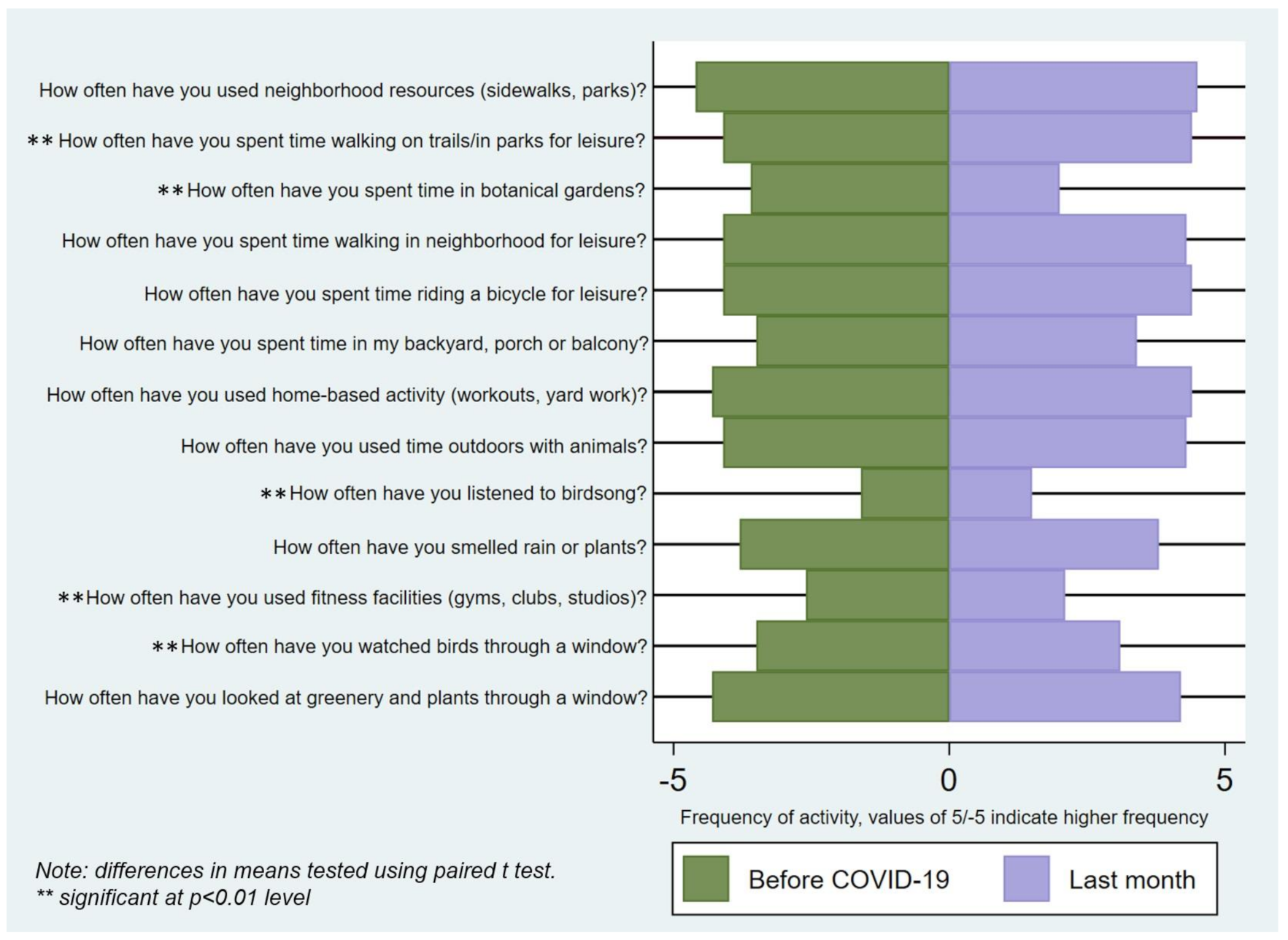
3.2. Changes in Engagement in Outdoor Physical Activity, Usage of Parks, and at-Home Contact with Nature during COVID-19 Lockdowns among Breast Cancer Patients
3.3. Effects of These Changes on Perceived Stress Score (PSS) and Symptom Experience
3.4. Alternative Indoor or Near-Home Contact with Nature Substitutes for Therapeutic Outdoor Physical Activity in Public Places
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- ASCO Report. The state of cancer care in America, 2014: A report by the American Society of Clinical Oncology. J. Oncol. 2014, 10, 119–142. [Google Scholar]
- Boon, H.S.; Olatunde, F.; Zick, S.M. Trends in complementary/alternative medicine use by breast cancer survivors: Comparing survey data from 1998 and 2005. BMC Womens Health 2007, 7, 4. Available online: http://www.biomedcentral.com/content/pdf/1472-6874-7-4.pdf (accessed on 27 August 2021). [CrossRef] [PubMed] [Green Version]
- Wu, Y.; Zhang, D.; Kang, S. Physical activity and risk of breast cancer: A meta-analysis of prospective studies. Breast Cancer Res. Treat. 2012, 137, 869–882. [Google Scholar] [CrossRef]
- Friedenreich, C.M. Physical Activity and Breast Cancer: Review of the Epidemiologic Evidence and Biologic Mechanisms. New Perspect. Mol. Clin. Manag. Gastrointest. Tumors 2010, 188, 125–139. [Google Scholar]
- Jurdana, M. Physical activity and cancer risk. Actual knowledge and possible biological mechanisms. Radiol. Oncol. 2021, 55, 7–17. [Google Scholar] [CrossRef] [PubMed]
- McTiernan, A. Weight, physical activity and breast cancer survival. Proc. Nutr. Soc. 2018, 77, 403–411. [Google Scholar] [CrossRef] [Green Version]
- WHO. Urban Green Spaces and Health. A Review of the Evidence; Egorov, A.I., Mudu, P., Braubach, M., Martuzzi, M., Eds.; WHO Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Hartig, T.; Mitchell, R.; de Vries, S.; Frumkin, H. Nature and health. Annu Rev Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef] [Green Version]
- Coon, J.T.; Boddy, K.; Stein, K.; Whear, R.; Barton, J.; Depledge, M. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. J. Epidemiol. Community Health 2011, 65, A38. [Google Scholar] [CrossRef]
- Beyer, K.M.M.; Szabo, A.; Hoormann, K.; Stolley, M. Time spent outdoors, activity levels, and chronic disease among American adults. J. Behav. Med. 2018, 41, 494–503. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Hart, J.E.; Banay, R.F.; Laden, F. Exposure to Greenness and Mortality in a Nationwide Prospective Cohort Study of Women. Environ. Health Perspect. 2016, 124, 1344–1352. [Google Scholar] [CrossRef] [Green Version]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef]
- South, E.C.; Hohl, B.C.; Kondo, M.C.; MacDonald, J.M.; Branas, C.C. Effect of greening vacant land on mental health of community-dwelling adults: A cluster randomized trial. JAMA Network Open 2018, 1, e180298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, D.R.; Rovniak, L.S.; Kraschnewski, J.L.; Hanson, R.; Sciamanna, C.N. A growing opportunity: Community gardens affiliated with US hospitals and academic health centers. Prev. Med. Rep. 2015, 2, 35–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunter, R.; Cleland, C.; Cleary, A.; Droomers, M.; Wheeler, B.; Sinnett, D.; Nieuwenhuijsen, M.; Braubach, M. Environmental, health, wellbeing, social and equity effects of urban green space interventions: A meta-narrative evidence synthesis. Environ. Int. 2019, 130, 104923. [Google Scholar] [CrossRef] [PubMed]
- Kondo, M.C.; Fluehr, J.M.; McKeon, T.P.; Branas, C.C. Urban Green Space and Its Impact on Human Health. Int. J. Environ. Res. Public Health 2018, 15, 445. [Google Scholar] [CrossRef] [Green Version]
- Egorov, A.I.; Griffin, S.M.; Converse, R.R.; Styles, J.N.; Sams, E.A.; Wilson, A.; Jackson, L.E.; Wade, T.J. Vegetated land cover near residence is associated with reduced allostatic load and improved bi-omarkers of neuroendocrine, metabolic and immune functions. Environ Res 2017, 158, 508–521. [Google Scholar] [CrossRef] [PubMed]
- Ulmer, J.M.; Wolf, K.L.; Backman, D.R.; Tretheway, R.L.; Blain, C.J.; O’Neil-Dunne, J.P.; Frank, L.D. Multiple health benefits of urban tree canopy: The mounting evidence for a green prescription. Health Place 2016, 42, 54–62. [Google Scholar] [CrossRef]
- Kardan, O.; Gozdyra, P.; Misic, B.; Moola, F.; Palmer, L.; Paus, T.; Berman, M.G. Neighborhood greenspace and health in a large urban center. Sci. Rep. 2015, 5, 11610. [Google Scholar] [CrossRef] [Green Version]
- Neilson, H.K.; Conroy, S.M.; Friedenreich, C.M. The Influence of Energetic Factors on Biomarkers of Postmen-opausal Breast Cancer Risk. Curr. Nutr. Rep. 2014, 3, 22–34. [Google Scholar] [CrossRef] [Green Version]
- Mao, G.-X.; Cao, Y.-B.; Lan, X.-G.; He, Z.-H.; Chen, Z.-M.; Wang, Y.-Z.; Hu, X.-L.; Lv, Y.-D.; Wang, G.-F.; Yan, J. Therapeutic effect of forest bathing on human hypertension in the elderly. J. Cardiol. 2012, 60, 495–502. [Google Scholar] [CrossRef] [Green Version]
- Midouhas, E.; Kokosi, T.; Flouri, E. Neighbourhood-level air pollution and greenspace and inflammation in adults. Health Place 2019, 58, 102167. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Miyazaki, Y. Physiological Effects of Nature Therapy: A Review of the Research in Japan. Int. J. Environ. Res. Public Health 2016, 13, 781. [Google Scholar] [CrossRef] [PubMed]
- Pretty, J.; Rogerson, M.; Barton, J. Green Mind Theory: How Brain-Body-Behaviour Links into Natural and Social Environments for Healthy Habits. Int. J. Environ. Res. Public Health 2017, 14, 706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsao, T.-M.; Tsai, M.-J.; Hwang, J.-S.; Cheng, W.-F.; Wu, C.-F.; Chou, C.-C.; Su, T.-C. Health effects of a forest environment on natural killer cells in humans: An observational pilot study. Oncotarget 2018, 9, 16501–16511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olafsdottir, G.; Cloke, P.; Vogele, C. Place, green exercise and stress: An exploration of lived experience and re-storative effects. Health Place 2017, 46, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Pretty, J.; Peacock, J.; Sellens, M.; Griffin, M. The mental and physical health outcomes of green exercise. Int. J. Environ. Health Res. 2005, 15, 319–337. [Google Scholar] [CrossRef] [PubMed]
- Winzer, B.M.; Whiteman, D.; Reeves, M.M.; Paratz, J.D. Physical activity and cancer prevention: A systematic review of clinical trials. Cancer Causes Control. 2011, 22, 811–826. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.C.; Johnson, M.P.; Schorpp, K.M.; Boen, C.E.; Harris, K.M. Young Adult Risk Factors for Cancer: Obesity, Inflammation, and Sociobehavioral Mechanisms. Am. J. Prev. Med. 2017, 53, S21–S29. [Google Scholar] [CrossRef] [Green Version]
- Campbell, K.L.; Landells, C.E.; Fan, J.; Brenner, D.R. A Systematic Review of the Effect of Lifestyle Interventions on Adipose Tissue Gene Expression: Implications for Carcinogenesis. Obesity 2017, 25, S40–S51. [Google Scholar] [CrossRef] [Green Version]
- Goodwin, P.J.; Ambrosone, C.B.; Hong, C.-C. Modifiable Lifestyle Factors and Breast Cancer Outcomes: Current Controversies and Research Recommendations. Adv. Exp. Med. Biol. 2015, 862, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Fair, A.M.; Montgomery, K. Energy Balance, Physical Activity, and Cancer Risk. Methods Mol. Biol. 2009, 472, 57–88. [Google Scholar] [CrossRef]
- Cox, D.T.C.; Shanahan, D.F.; Hudson, H.L.; Plummer, K.E.; Siriwardena, G.M.; Fuller, R.A.; Anderson, K.; Hancock, S.; Gaston, K.J. Doses of Neighborhood Nature: The Benefits for Mental Health of Living with Nature. BioScience 2017, 67, 147–155. [Google Scholar] [CrossRef]
- Shanahan, D.F.; Bush, R.; Gaston, K.J.; Lin, B.; Dean, J.; Barber, E.; Fuller, R. Health Benefits from Nature Experiences Depend on Dose. Sci. Rep. 2016, 6, 28551. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.K.; Barton, J.; Gladwell, V.F. Viewing Nature Scenes Positively Affects Recovery of Autonomic Function Following Acute-Mental Stress. Environ. Sci. Technol. 2013, 47, 5562–5569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gladwell, V.F.; Brown, D.K.; Barton, J.L.; Tarvainen, M.P.; Kuoppa, P.; Pretty, J.; Suddaby, J.M.; Sandercock, G.R.H. The effects of views of nature on autonomic control. Graefe’s Arch. Clin. Exp. Ophthalmol. 2012, 112, 3379–3386. [Google Scholar] [CrossRef] [PubMed]
- Kotabe, H.P.; Kardan, O.; Berman, M.G. The nature-disorder paradox: A perceptual study on how nature is dis-orderly yet aesthetically preferred. J. Exp. Psychol. Gen. 2017, 146, 1126–1142. [Google Scholar] [CrossRef] [PubMed]
- McDermott, J.H. Auditory Preferences and Aesthetics. In Neuroscience of Preference and Choice: Cognitive and Neural, Mechanisms; Sharot, T., Dolan, R., Eds.; Elsevier: London, UK, 2012; pp. 227–256. [Google Scholar]
- Alvarsson, J.J.; Wiens, S.; Nilsson, M. Stress Recovery during Exposure to Nature Sound and Environmental Noise. Int. J. Environ. Res. Public Health 2010, 7, 1036–1046. [Google Scholar] [CrossRef]
- Zandieh, R.; Martinez, J.; Flacke, J.; Jones, P.; van Maarseveen, M. Older Adults’ Outdoor Walking: Inequalities in Neighbourhood Safety, Pedestrian Infrastructure and Aesthetics. Int. J. Environ. Res. Public Health 2016, 13, 1179. [Google Scholar] [CrossRef] [Green Version]
- Berman, M.G.; Kross, E.; Krpan, K.M.; Askren, M.K.; Burson, A.; Deldin, P.J.; Kaplan, S.; Sherdell, L.; Gotlib, I.H.; Jonides, J. Interacting with nature improves cognition and affect for individuals with depression. J. Affect. Disord. 2012, 140, 300–305. [Google Scholar] [CrossRef] [Green Version]
- Bodin, T.; Björk, J.; Ardö, J.; Albin, M. Annoyance, Sleep and Concentration Problems due to Combined Traffic Noise and the Benefit of Quiet Side. Int. J. Environ. Res. Public Health 2015, 12, 1612–1628. [Google Scholar] [CrossRef]
- Buxton, R.T.; Pearson, A.L.; Allou, C.; Fristrup, K.; Wittemyer, G. A synthesis of health benefits of natural sounds and their distribution in national parks. Proc. Natl. Acad. Sci. USA 2021, 118. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.W.; Gladkikh, T.M.; Hackenburg, D.M.; Gould, R.K. COVID-19 and human-nature relationships: Vermonters’ activities in nature and associated nonmaterial values during the pandemic. PLoS ONE 2020, 15, e0243697. [Google Scholar] [CrossRef] [PubMed]
- Guven, D.C.; Sahin, T.K.; Aktepe, O.H.; Yildirim, H.C.; Aksoy, S.; Kilickap, S. Perspectives, Knowledge, and Fears of Cancer Patients About COVID-19. Front. Oncol. 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Nisbet, E.K.; Zelenski, J.M. The NR-6: A new brief measure of nature relatedness. Front. Psychol. 2013, 4, 813. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Cleeland, C.S. Symptom Burden: Multiple Symptoms and Their Impact as Patient-Reported Outcomes. J. Natl. Cancer Inst. Monogr. 2007, 2007, 16–21. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Zhao, F.; Chang, V.; Sloan, J.A.; O’Mara, A.M.; Gilman, P.B.; Weiss, M.; Mendoza, T.R.; Lee, J.-W.; Fisch, M.J. The symptom burden of cancer: Evidence for a core set of cancer-related and treatment-related symptoms from the Eastern Cooperative Oncology Group Symptom Outcomes and Practice Patterns study. Cancer 2013, 119, 4333–4340. [Google Scholar] [CrossRef] [PubMed]
- Cleeland, C.S.; Mendoza, T.R.; Wang, X.S.; Chou, C.; Harle, M.T.; Morrissey, M.; Engstrom, M.C. Assessing symptom distress in cancer patients: The M.D. Anderson Symptom Inventory. Cancer 2000, 89, 1634–1646. [Google Scholar] [CrossRef]
- Mendoza, T.R.; Wang, X.S.; Lu, C.; Palos, G.R.; Liao, Z.; Mobley, G.M.; Kapoor, S.; Cleeland, C.S. Measuring the symptom burden of lung cancer the validity and utility of the lung cancer module of the M.D. Anderson Symptom Inventory. Oncologist 2011, 16, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Lev, E.; Kahn, P.H.J.; Chen, H.; Esperum, G. Relatively Wild Urban Parks Can Promote Human Resilience and Flourishing: A Case Study of Discovery Park, Seattle, Washington. Front. Sustain. Cities 2020, 2. [Google Scholar] [CrossRef]
- Mendoza, T.R.; Zhao, F.; Cleeland, C.S.; Wagner, L.I.; Patrick-Miller, L.J.; Fisch, M.J. The Validity and Utility of the M. D. Anderson Symptom Inventory in Patients with Breast Cancer: Evidence from the Symptom Outcomes and Practice Patterns Data from the Eastern Cooperative Oncology Group. Clin. Breast Cancer 2013, 13, 325–334. [Google Scholar] [CrossRef] [Green Version]
- Robinson, J.M.; Brindley, P.; Cameron, R.; MacCarthy, D.; Jorgensen, A. Nature’s role in supporting health during the COVID-19 pandemic: A geospatial and socioec-ological study. Environ. Res. Public Health 2021, 18, 2227. [Google Scholar] [CrossRef]
- Randler, C.; Tryjanowski, P.; Jokimaki, J.; Kaisanlahti-Jokimaki, M.L.; Staller, N. SARS-CoV2 (COVID-19) Pandemic Lockdown Influences Nature-Based Recreational Activity: The Case of Birders. Int. J. Environ. Res. Public Health 2020, 17, 7310. [Google Scholar] [CrossRef]
- Pearson, A.L.; Horton, T.H.; Pfeiffer, K.A.; Buxton, R.T.; Gardner, J.; Liu, W.; Hunter, R.F.; White, M.P. Contact with nature as a mental health buffer for lower income communities during the COVID-19 pandemic. Front. Sustain. Cities 2021, 3, 688473. [Google Scholar] [CrossRef]
- Taft, S.B. Therapeutic horticulture for people living with cancer: The Healing Gardens program at Lifeline in Seattle. J. Ther. Hortic. 2004, 15, 16. [Google Scholar]
- Morris, S.L.; Newhouse, I.; Larocque, T.; Gillis, K.-J.; Smith, L.; Nisbet, E.K. Becoming One with Nature: A Nature Intervention for Individuals Living with Cancer Participating in a Ten-Week Group Exercise and Wellness Program. Int. J. Exerc. Sci. 2021, 14, 498–518. [Google Scholar] [PubMed]
- Sahlin, E.; Ahlborg, G., Jr.; Matuszczyk, J.V.; Grahn, P. Nature-based stress management course for individuals at risk of adverse health effects from work-related stress-effects on stress related symptoms, workability and sick leave. Int. J. Environ. Res. Public Health 2014, 11, 6586–6611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pouso, S.; Borja, Á.; Fleming, L.E.; Gómez-Baggethun, E.; White, M.P.; Uyarra, M.C. Maintaining contact with blue-green spaces during the COVID-19 pandemic associated with positive mental health. Sci. Total Environ. 2020, 756, 143984. [Google Scholar] [CrossRef]
- Dzhambov, A.M.; Lercher, P.; Browning, M.H.E.M.; Stoyanov, D.; Petrova, N.; Novakov, S.; Dimitrova, D.D. Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environ. Res. 2021, 196, 110420. [Google Scholar] [CrossRef]
- Poortinga, W.; Bird, N.; Hallingberg, B.; Phillips, R.; Williams, D. The role of perceived public and private green space in subjective health and wellbeing during and after the first peak of the COVID-19 outbreak. Landsc. Urban. Plan. 2021, 211, 104092. [Google Scholar] [CrossRef]
- Spencer, L.H.; Lynch, M.; Lawrence, C.L.; Edwards, R.T. A Scoping Review of How Income Affects Accessing Local Green Space to Engage in Outdoor Physical Activity to Improve Well-Being: Implications for Post-COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 9313. [Google Scholar] [CrossRef] [PubMed]
| Low Income | Middle Income | High Income | Total | ||
|---|---|---|---|---|---|
| n = 5 | n = 18 | n = 33 | n = 56 | ||
| Age (in years), mean (sd) | 64.6 (11.6) | 64.4 (12.3) | 62.2 (9.9) | 63.1 (10.7) | |
| Female, n (%) | 5 (100) | 18 (100) | 32 (97.0) | 55 (98.2) | |
| Married/partnered, n (%) | 0 (0) | 7 (38.9) | 24 (72.7) | 31 (55.4) | |
| Number of kids at home, mean (sd) | 0 (0) | 0 (0) | 0.1 (0.3) | 0.04 (0.3) | |
| Ethnicity, n (%) | White | 5 (100) | 15 (83.3) | 29 (87.9) | 49 (87.5) |
| Hispanic/Latino | 0 (0) | 1 (5.6) | 0 (0) | 1 (1.8) | |
| Black/African American | 0 (0) | 1 (5.6) | 3 (10.0) | 4 (7.1) | |
| Native American/American Indian | 0 (0) | 1 (5.6) | 1 (3.0) | 2 (3.6) | |
| Asian/Pacific Islander | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Other | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Income, n (%) | Low: <$30,000/year | 5 (8.9) | |||
| Middle: $30,000–$59,999/year | 18 (32.1) | ||||
| High: $60,000+/year | 33 (58.9) | ||||
| Education, n (%) | Less than college degree | 3 (60.0) | 6 (33.3) | 2 (6.1) | 11 (19.6) |
| College degree | 1 (20.0) | 5 (27.8) | 9 (27.2) | 15 (26.8) | |
| Graduate/Professional degree | 1 (20.0) | 7 (38.9) | 22 (66.7) | 30 (53.6) | |
| Age at diagnosis, mean (sd) | 55.0 (13.0) | 55.2 (13.2) | 52.9 (9.9) | 53.8 (11.1) | |
| Stage at diagnosis, mean (sd) | 2.8 (1.8) | 2.6 (1.2) | 2.6 (1.1) | 2.6 (1.2) | |
| Experienced disruptions in care during COVID-19, n (%) | 0 (0) | 6 (33.3) | 4 (12.1) | 10 (17.9) | |
| Diagnoses, n (%) | Bilateral | 0 (0) | 1 (5.6) | 4 (12.1) | 5 (8.9) |
| Unilateral | 3 (60.0) | 14 (77.8) | 29 (87.9) | 46 (82.1) | |
| Recurrent | 0 (0) | 2 (11.1) | 1 (3.0) | 3 (5.4) | |
| Metastatic | 1 (20.0) | 3 (16.7) | 6 (18.2) | 10 (17.9) | |
| Inflammatory | 0 (0) | 1 (5.6) | 1 (3.0) | 2 (3.6) | |
| BRAC1 or BRAC2 genes | 0 (0) | 2 (11.1) | 2 (6.1) | 4 (7.1) | |
| Hormone receptor positive | 2 (40.0) | 11 (61.1) | 24 (72.7) | 37 (66.1) | |
| Hormone receptor negative | 1 (20.0) | 2 (11.1) | 2 (6.1) | 5 (8.9) | |
| Mother diagnosed with breast cancer | 1 (20.0) | 2 (11.1) | 10 (33.3) | 13 (23.2) | |
| Mother’s mother diagnosed with breast cancer | 1 (20.0) | 3 (16.7) | 2 (6.1) | 6 (10.7) | |
| Father’s mother diagnosed with breast cancer | 0 (0) | 0 (0) | 1 (3.0) | 1 (1.8) | |
| Treatment, n (%) | Chemotherapy | 3 (60.0) | 7 (38.9) | 14 (42.4) | 24 (42.9) |
| Radiation | 3 (60.0) | 15 (83.3) | 16 (48.5) | 34 (60.7) | |
| Surgery | 4 (80.0) | 16 (88.9) | 30 (90.9) | 50 (89.3) | |
| Hormonal therapy | 3 (60.0) | 12 (66.7) | 17 (51.5) | 32 (57.1) | |
| Targeted therapy | 0 (0) | 2 (11.1) | 5 (15.2) | 7 (12.5) | |
| Immunotherapy | 1 (20.0) | 1 (5.6) | 1 (3.0) | 3 (5.4) | |
| Complementary therapies (e.g., meditation) | 1 (20.0) | 2 (11.1) | 5 (15.2) | 8 (14.3) | |
| None | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Positive test for COVID-19, n (%) | 0 (0) | 0 (0) | 6 (18.2) | 6 (10.7) | |
| Nature-relatedness score, mean (sd) | 4.0 (0.4) | 3.7 (0.8) | 3.7 (0.7) | 3.7 (0.7) | |
| Perceived stress score, mean (sd) | 31.6 (7.3) | 26.6 (8.0) | 23.5 (6.9) | 25.2 (7.5) | |
| Overall symptom distress, mean (sd) | 4.6 (3.5) | 3.9 (2.6) | 2.3 (2.0) | 3.0 (2.5) | |
| Symptom severity, mean (sd) | 3.8 (1.6) | 2.5 (1.8) | 1.9 (1.5) | 2.2 (1.7) | |
| Quality of life-spiritual, mean (sd) | 35.8 (4.9) | 39.4 (9.9) | 38.3 (10.4) | 38.5 (9.8) | |
| Quality of life-fitness, mean (sd) | 15.4 (3.2) | 14.8 (6.7) | 18.2 (5.0) | 16.9 (5.6) | |
| Perceived Stress Score | Symptom Distress | Symptom Severity | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef | se | 95% CI | p-Value | Coef | se | 95% CI | p-Value | Coef | se | 95% CI | p-Value | ||||
| Change in use of parks/trails | −2.30 | 0.86 | −4.03 | −0.57 | 0.010 ** | −0.23 | 0.31 | −0.85 | 0.39 | 0.454 | −0.31 | 0.21 | −0.73 | 0.10 | 0.136 |
| Age | −0.15 | 0.08 | −0.32 | 0.02 | 0.085 * | −0.01 | 0.03 | −0.07 | 0.05 | 0.815 | −0.02 | 0.02 | −0.06 | 0.02 | 0.347 |
| Married/partnered 2020 | 4.74 | 2.01 | 0.70 | 8.79 | 0.022 ** | 0.95 | 0.72 | −0.50 | 2.40 | 0.195 | 0.70 | 0.48 | −0.27 | 1.66 | 0.155 |
| Low income | 13.57 | 3.41 | 6.72 | 20.42 | <0.001 ** | 3.05 | 1.22 | 0.59 | 5.51 | 0.016 ** | 2.72 | 0.82 | 1.08 | 4.36 | 0.002 ** |
| Middle income | 4.42 | 1.99 | 0.41 | 8.42 | 0.031 ** | 1.87 | 0.72 | 0.43 | 3.31 | 0.012 ** | 0.86 | 0.48 | −0.10 | 1.82 | 0.078 * |
| High income | ref | ref | ref | ||||||||||||
| Stage breast cancer diagnosis | 0.20 | 0.75 | −1.31 | 1.71 | 0.793 | 0.48 | 0.27 | −0.07 | 1.02 | 0.084 * | 0.34 | 0.18 | −0.02 | 0.71 | 0.062 * |
| Change in use of botanical gardens | −1.21 | 1.28 | −3.77 | 1.35 | 0.346 | −0.52 | 0.43 | −1.38 | 0.34 | 0.232 | −0.51 | 0.29 | −1.08 | 0.06 | 0.081 * |
| Age | −0.13 | 0.09 | −0.31 | 0.05 | 0.162 | 0.00 | 0.03 | −0.06 | 0.06 | 0.984 | −0.01 | 0.02 | −0.05 | 0.03 | 0.576 |
| Married/partnered 2020 | 5.09 | 2.13 | 0.81 | 9.37 | 0.021 ** | 0.97 | 0.71 | −0.46 | 2.41 | 0.180 | 0.73 | 0.48 | −0.23 | 1.69 | 0.131 |
| Low income | 12.51 | 3.59 | 5.29 | 19.72 | 0.001 ** | 3.05 | 1.20 | 0.63 | 5.47 | 0.015 ** | 2.67 | 0.80 | 1.05 | 4.28 | 0.002 ** |
| Middle income | 4.73 | 2.15 | 0.42 | 9.04 | 0.032 ** | 1.76 | 0.72 | 0.31 | 3.20 | 0.018 ** | 0.77 | 0.48 | −0.19 | 1.74 | 0.115 |
| High income | ref | ref | ref | ||||||||||||
| Stage breast cancer diagnosis | 0.15 | 0.80 | −1.46 | 1.75 | 0.856 | 0.48 | 0.27 | −0.06 | 1.02 | 0.079 * | 0.34 | 0.18 | −0.01 | 0.70 | 0.059 * |
| Change in use of backyard or porch | −2.69 | 1.07 | −4.85 | −0.53 | 0.016 ** | −0.80 | 0.37 | −1.54 | −0.06 | 0.034 ** | −0.52 | 0.25 | −1.03 | −0.02 | 0.041 ** |
| Age | −0.11 | 0.09 | −0.29 | 0.06 | 0.191 | 0.00 | 0.03 | −0.06 | 0.06 | 0.919 | −0.01 | 0.02 | −0.05 | 0.03 | 0.535 |
| Married/partnered 2020 | 5.70 | 2.04 | 1.60 | 9.79 | 0.007 ** | 1.16 | 0.70 | −0.24 | 2.56 | 0.103 | 0.86 | 0.47 | −0.09 | 1.81 | 0.076 * |
| Low income | 13.40 | 3.43 | 6.51 | 20.29 | <0.001 ** | 3.27 | 1.17 | 0.92 | 5.63 | 0.008 ** | 2.77 | 0.80 | 1.16 | 4.37 | 0.001 ** |
| Middle income | 4.81 | 1.99 | 0.81 | 8.82 | 0.020 ** | 1.84 | 0.68 | 0.47 | 3.21 | 0.010 ** | 0.89 | 0.46 | −0.04 | 1.82 | 0.061 * |
| High income | ref | ref | |||||||||||||
| Stage breast cancer diagnosis | 0.54 | 0.78 | −1.02 | 2.10 | 0.489 | 0.59 | 0.27 | 0.06 | 1.13 | 0.030 ** | 0.42 | 0.18 | 0.05 | 0.78 | 0.026 ** |
| Change in bird watching | 1.67 | 1.29 | −0.92 | 4.26 | 0.200 | 0.26 | 0.44 | −0.63 | 1.14 | 0.562 | −0.25 | 0.30 | −0.85 | 0.34 | 0.398 |
| Age | −0.17 | 0.09 | −0.35 | 0.01 | 0.07 * | −0.01 | 0.03 | −0.07 | 0.05 | 0.745 | −0.02 | 0.02 | −0.06 | 0.03 | 0.438 |
| Married/partnered 2020 | 4.84 | 2.12 | 0.57 | 9.11 | 0.027 ** | 0.94 | 0.73 | −0.52 | 2.40 | 0.200 | 0.79 | 0.49 | −0.19 | 1.78 | 0.113 |
| Low income | 11.20 | 3.62 | 3.92 | 18.48 | 0.003 ** | 2.76 | 1.24 | 0.27 | 5.25 | 0.031 ** | 2.68 | 0.84 | 0.99 | 4.36 | 0.002 ** |
| Middle income | 5.41 | 2.08 | 1.23 | 9.60 | 0.012 ** | 1.99 | 0.71 | 0.55 | 3.42 | 0.008 ** | 0.93 | 0.48 | −0.04 | 1.90 | 0.060 * |
| High income | ref | ref | ref | ||||||||||||
| Stage breast cancer diagnosis | 0.29 | 0.80 | −1.32 | 1.90 | 0.719 | 0.49 | 0.27 | −0.06 | 1.05 | 0.078 * | 0.31 | 0.19 | −0.07 | 0.68 | 0.104 |
| Change in listening to birdsong | 0.48 | 1.28 | −2.08 | 3.04 | 0.709 | −0.32 | 0.43 | −1.18 | 0.54 | 0.462 | −0.45 | 0.29 | −1.02 | 0.12 | 0.121 |
| Age | −0.15 | 0.09 | −0.34 | 0.03 | 0.099 * | 0.00 | 0.03 | −0.06 | 0.06 | 0.941 | −0.01 | 0.02 | −0.05 | 0.03 | 0.554 |
| Married/partnered 2020 | 5.04 | 2.16 | 0.70 | 9.37 | 0.024 ** | 1.05 | 0.73 | −0.41 | 2.51 | 0.154 | 0.83 | 0.48 | −0.14 | 1.81 | 0.090 * |
| Low income | 12.03 | 3.62 | 4.75 | 19.31 | 0.002 ** | 3.01 | 1.22 | 0.56 | 5.45 | 0.017 ** | 2.67 | 0.81 | 1.04 | 4.29 | 0.002 ** |
| Middle income | 5.30 | 2.13 | 1.02 | 9.57 | 0.016 ** | 1.88 | 0.72 | 0.44 | 3.32 | 0.012 ** | 0.86 | 0.48 | −0.10 | 1.82 | 0.077 * |
| High income | ref | ref | ref | ||||||||||||
| Stage breast cancer diagnosis | 0.19 | 0.83 | −1.47 | 1.86 | 0.817 | 0.42 | 0.28 | −0.14 | 0.98 | 0.139 | 0.26 | 0.19 | −0.11 | 0.63 | 0.162 |
| Change in smelling rain or plants | −0.53 | 1.39 | −3.33 | 2.27 | 0.704 | −0.11 | 0.47 | −1.06 | 0.84 | 0.818 | −0.08 | 0.32 | −0.72 | 0.56 | 0.804 |
| Age | −0.14 | 0.09 | −0.32 | 0.05 | 0.139 | −0.01 | 0.03 | −0.07 | 0.06 | 0.864 | −0.02 | 0.02 | −0.06 | 0.02 | 0.404 |
| Married/partnered 2020 | 5.29 | 2.19 | 0.90 | 9.69 | 0.019 ** | 1.02 | 0.74 | −0.46 | 2.51 | 0.173 | 0.77 | 0.50 | −0.23 | 1.78 | 0.130 |
| Low income | 12.48 | 3.69 | 5.07 | 19.89 | 0.001 ** | 2.97 | 1.25 | 0.47 | 5.47 | 0.021 ** | 2.57 | 0.84 | 0.88 | 4.27 | 0.004 ** |
| Middle income | 5.08 | 2.13 | 0.81 | 9.35 | 0.021 ** | 1.93 | 0.72 | 0.49 | 3.37 | 0.010 ** | 0.95 | 0.49 | −0.03 | 1.93 | 0.058 * |
| High income | ref | ref | ref | ||||||||||||
| Stage breast cancer diagnosis | 0.14 | 0.80 | −1.48 | 1.75 | 0.867 | 0.47 | 0.27 | −0.07 | 1.02 | 0.089 * | 0.34 | 0.18 | −0.03 | 0.71 | 0.075 * |
| Change in use of gyms | 1.17 | 0.74 | −0.31 | 2.66 | 0.119 | 0.40 | 0.25 | −0.11 | 0.90 | 0.119 | 0.36 | 0.17 | 0.03 | 0.69 | 0.034 ** |
| Age | −0.13 | 0.09 | −0.31 | 0.04 | 0.134 | 0.00 | 0.03 | −0.06 | 0.06 | 0.929 | −0.02 | 0.02 | −0.05 | 0.02 | 0.451 |
| Married/partnered 2020 | 5.97 | 2.16 | 1.62 | 10.31 | 0.008 ** | 1.27 | 0.73 | −0.19 | 2.74 | 0.087 * | 1.01 | 0.48 | 0.03 | 1.98 | 0.043 ** |
| Low income | 13.08 | 3.56 | 5.92 | 20.23 | 0.001 ** | 3.21 | 1.20 | 0.80 | 5.63 | 0.01 ** | 2.80 | 0.80 | 1.20 | 4.41 | 0.001 ** |
| Middle income | 4.85 | 2.07 | 0.69 | 9.01 | 0.023 ** | 1.84 | 0.70 | 0.43 | 3.24 | 0.011 ** | 0.86 | 0.46 | −0.07 | 1.79 | 0.070 * |
| High income | ref | ref | ref | ||||||||||||
| Stage breast cancer diagnosis | 0.13 | 0.78 | −1.45 | 1.70 | 0.873 | 0.47 | 0.26 | −0.06 | 1.00 | 0.082 * | 0.34 | 0.18 | −0.02 | 0.69 | 0.062 * |
| Low Symptom Distress (<5) | High Symptom Distress (≥5) | Total | |
|---|---|---|---|
| n = 44 | n = 12 | n = 56 | |
| I enjoy watching nature through a window. | 36 (81.8) | 11 (91.7) | 46 (83.9) |
| I enjoy listening to nature through a window. | 27 (61.4) | 10 (83.3) | 37 (66.1) |
| I enjoy looking at images of nature. | 31 (70.5) | 9 (75.0) | 40 (71.4) |
| I enjoy listening to natural sounds through recordings (e.g., water, birds). | 14 (31.8) | 7 (58.3) | 21 (37.5) |
| I enjoy growing indoor plants. | 25 (56.8) | 7 (58.3) | 32 (57.1) |
| I enjoy virtual reality of nature scenes. | 10 (22.7) | 4 (33.3) | 14 (25.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pearson, A.L.; Breeze, V.; Reuben, A.; Wyatt, G. Increased Use of Porch or Backyard Nature during COVID-19 Associated with Lower Stress and Better Symptom Experience among Breast Cancer Patients. Int. J. Environ. Res. Public Health 2021, 18, 9102. https://doi.org/10.3390/ijerph18179102
Pearson AL, Breeze V, Reuben A, Wyatt G. Increased Use of Porch or Backyard Nature during COVID-19 Associated with Lower Stress and Better Symptom Experience among Breast Cancer Patients. International Journal of Environmental Research and Public Health. 2021; 18(17):9102. https://doi.org/10.3390/ijerph18179102
Chicago/Turabian StylePearson, Amber L., Victoria Breeze, Aaron Reuben, and Gwen Wyatt. 2021. "Increased Use of Porch or Backyard Nature during COVID-19 Associated with Lower Stress and Better Symptom Experience among Breast Cancer Patients" International Journal of Environmental Research and Public Health 18, no. 17: 9102. https://doi.org/10.3390/ijerph18179102
APA StylePearson, A. L., Breeze, V., Reuben, A., & Wyatt, G. (2021). Increased Use of Porch or Backyard Nature during COVID-19 Associated with Lower Stress and Better Symptom Experience among Breast Cancer Patients. International Journal of Environmental Research and Public Health, 18(17), 9102. https://doi.org/10.3390/ijerph18179102







