Long-Term Neurological and Psychological Distress Symptoms among Smallholder Farmers in Costa Rica with a History of Acute Pesticide Poisoning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Occupational Pesticide Exposure and Sociodemographic Characteristics
2.3. APPs and Associated Neurological and Psychological Distress Symptoms
2.4. Statistical Analyses
3. Results
3.1. Descriptive Statistics of the Study Population
3.2. Sociodemographic Predictors of Having Experienced an APP
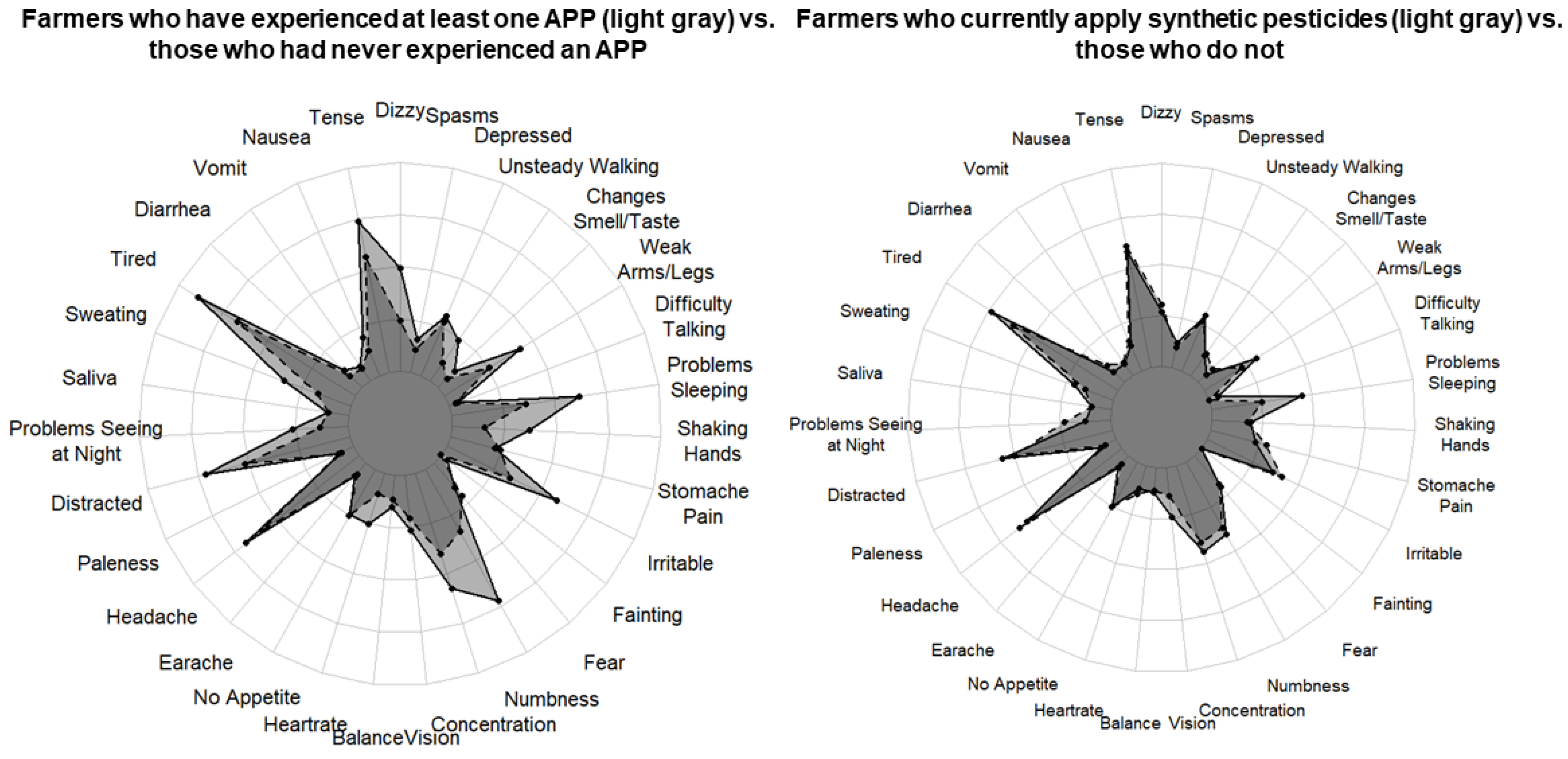
3.3. Self-Reported Neurological Symptoms During the 12 Months Prior to Interview
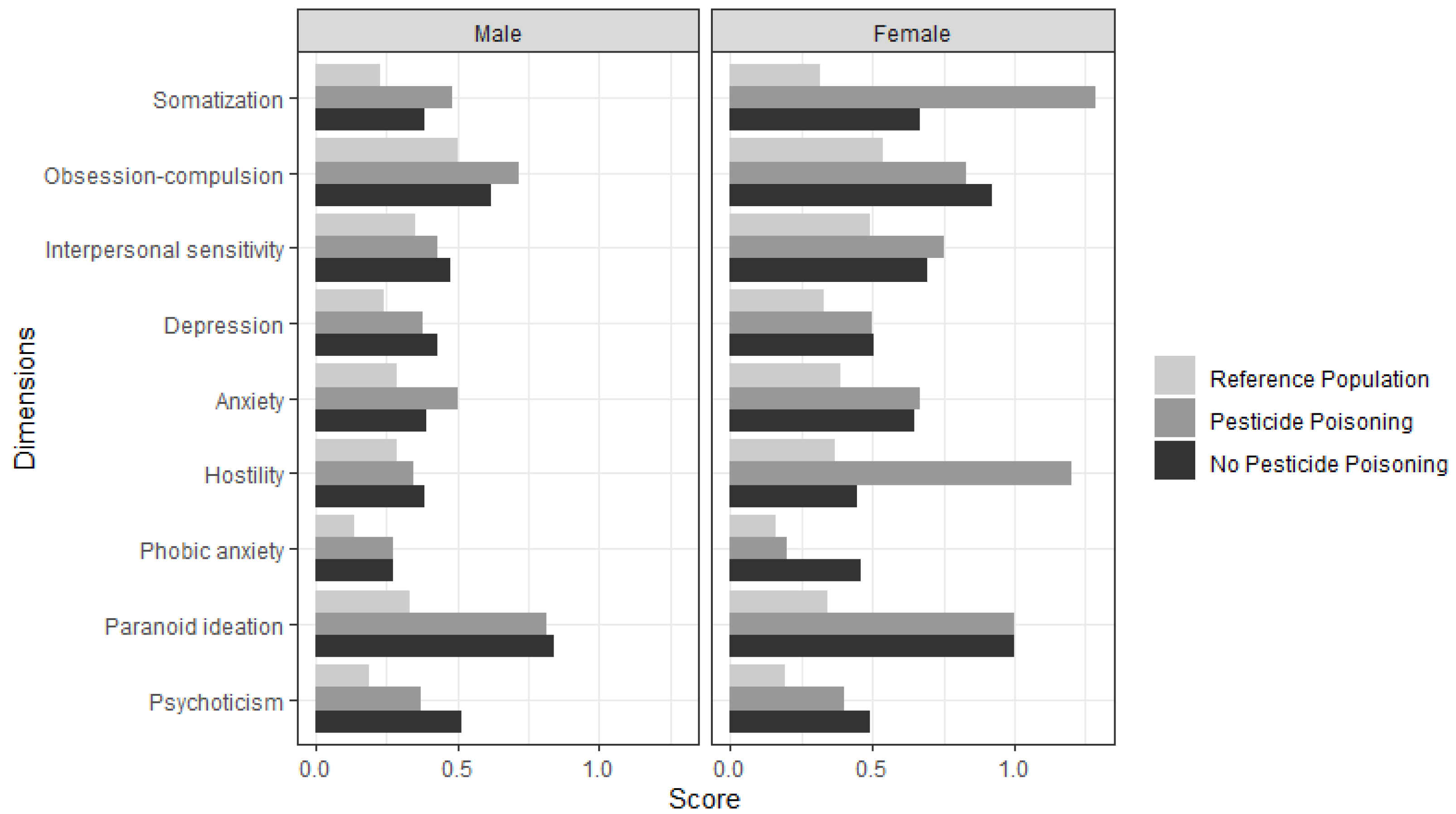
3.4. Psychological Distress Symptoms During the Month Prior to Interview
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Symptom | Farmers who Never Experienced APP (n = 257) | Farmers who Experienced at Least One APP (n = 43) | Difference in Frequency |
|---|---|---|---|
| Dizziness | 0.64 | 1.26 | 0.61 |
| Tense, anxious or nervous | 1.43 | 1.86 | 0.43 |
| Nausea | 0.75 | 0.53 | −0.22 |
| Vomiting | 0.22 | 0.26 | 0.04 |
| Diarrhea | 0.25 | 0.35 | 0.1 |
| Tired or low energy | 1.69 | 2.23 | 0.54 |
| More than normal sweating/perspiration | 0.84 | 0.88 | 0.04 |
| More than normal salivation | 0.28 | 0.30 | 0.02 |
| Difficulty seeing at night | 0.38 | 0.70 | 0.32 |
| Distracted, forgetful, or confused | 1.31 | 1.79 | 0.48 |
| Paleness | 0.24 | 0.21 | −0.03 |
| Headache | 1.48 | 1.72 | 0.24 |
| Earache | 0.21 | 0.26 | 0.05 |
| Loss of appetite | 0.67 | 0.65 | −0.02 |
| Accelerated heartrate | 0.30 | 0.67 | 0.37 |
| Difficulty with balance | 0.33 | 0.42 | 0.09 |
| Blurred or double vision | 0.55 | 0.70 | 0.15 |
| Difficulty concentrating | 1.04 | 1.47 | 0.43 |
| Numbness or tingling in hands or feet | 0.89 | 1.81 | 0.93 * |
| Felt fearful | 0.55 | 0.42 | −0.13 |
| Fainting | 0.04 | 0.14 | 0.1 |
| More irritable or angry than normal | 0.88 | 1.49 | 0.61 |
| Stomach pain | 0.65 | 0.58 | −0.07 |
| Shaking hands | 0.43 | 0.95 | 0.52 |
| Insomnia | 0.93 | 1.56 | 0.63 |
| Difficulty talking | 0.13 | 0.16 | 0.03 |
| Weakness in arms or legs | 0.67 | 1.09 | 0.42 |
| Changes in ability to smell and taste | 0.19 | 0.33 | 0.14 |
| Unsteady walking | 0.30 | 0.63 | 0.33 |
| Depressed, indifferent, or withdrawn | 0.74 | 0.81 | 0.07 |
| Spasms or involuntary movements | 0.33 | 0.44 | 0.11 |
References
- Sharma, A.; Kumar, V.; Shahzad, B.; Tanveer, M.; Sidhu, G.P.S.; Handa, N.; Kohli, S.K.; Yadav, P.; Bali, A.S.; Parihar, R.D.; et al. Worldwide pesticide usage and its impacts on ecosystem. Sn Appl. Sci. 2019, 1, 1446. [Google Scholar] [CrossRef] [Green Version]
- Thundiyil, J.G.; Stober, J.; Besbelli, N.; Pronczuk, J. Acute pesticide poisoning: A proposed classification tool. Bull. World Health Organ. 2008, 86, 205–209. [Google Scholar] [CrossRef]
- Ohlander, J.; Fuhrimann, S.; Basinas, I.; Cherrie, J.W.; Galea, K.S.; Povey, A.C.; van Tongeren, M.; Harding, A.-H.; Jones, K.; Vermeulen, R.; et al. Systematic review of methods used to assess exposure to pesticides in occupational epidemiology studies, 1993–2017. Occup. Environ. Med. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuhrimann, S.; Staudacher, P.; Lindh, C.; van Wendel de Joode, B.; Mora, A.M.; Winkler, M.S.; Kromhout, H. Variability and predictors of weekly pesticide exposure in applicators from organic, sustainable and conventional smallholder farms in Costa Rica. Occup. Environ. Med. 2020, 77, 40–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staudacher, P.; Fuhrimann, S.; Farnham, A.; Mora, A.M.; Atuhaire, A.; Niwagaba, C.; Stamm, C.; Eggen, R.I.L.; Winkler, M.S. Comparative Analysis of Pesticide Use Determinants Among Smallholder Farmers From Costa Rica and Uganda. Environ. Health Insights 2020, 14, 1178630220972417. [Google Scholar] [CrossRef] [PubMed]
- Corriols, M.; Marin, J.; Berroteran, J.; Lozano, L.M.; Lundberg, I. Incidence of acute pesticide poisonings in Nicaragua: A public health concern. Occup. Environ. Med. 2009, 66, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Wesseling, C.; Corriols, M.; Bravo, V. Acute pesticide poisoning and pesticide registration in Central America. Toxicol. Appl. Pharmacol. 2005, 207, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Kesavachandran, C.N.; Fareed, M.; Pathak, M.K.; Bihari, V.; Mathur, N.; Srivastava, A.K. Adverse health effects of pesticides in agrarian populations of developing countries. Rev. Environ. Contam. Toxicol. 2009, 200, 33–52. [Google Scholar]
- Corriols, M.; Marin, J.; Berroteran, J.; Lozano, L.M.; Lundberg, I.; Thorn, A. The Nicaraguan Pesticide Poisoning Register: Constant underreporting. Int. J. Health Serv. 2008, 38, 773–787. [Google Scholar] [CrossRef]
- Engel, L.S.; Seixas, N.S.; Keifer, M.C.; Longstreth, W.T., Jr.; Checkoway, H. Validity study of self-reported pesticide exposure among orchardists. J. Expo. Anal. Environ. Epidemiol. 2001, 11, 359–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoppin, J.A.; Yucel, F.; Dosemeci, M.; Sandler, D.P. Accuracy of self-reported pesticide use duration information from licensed pesticide applicators in the Agricultural Health Study. J. Expo. Sci. Environ. Epidemiol. 2002, 12, 313–318. [Google Scholar] [CrossRef] [Green Version]
- Lekei, E.E.; Ngowi, A.V.; London, L. Farmers’ knowledge, practices and injuries associated with pesticide exposure in rural farming villages in Tanzania. BMC Public Health 2014, 14, 389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blair, A.; Tarone, R.; Sandler, D.; Lynch, C.F.; Rowland, A.; Wintersteen, W.; Steen, W.C.; Samanic, C.; Dosemeci, M.; Alavanja, M.C. Reliability of reporting on life-style and agricultural factors by a sample of participants in the Agricultural Health Study from Iowa. Epidemiology 2002, 13, 94–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nigatu, A.W.; Bråtveit, M.; Moen, B.E. Self-reported acute pesticide intoxications in Ethiopia. BMC Public Health 2016, 16, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negatu, B.; Vermeulen, R.; Mekonnen, Y.; Kromhout, H. Neurobehavioural symptoms and acute pesticide poisoning: A cross-sectional study among male pesticide applicators selected from three commercial farming systems in Ethiopia. Occup. Environ. Med. 2018, 75, 283–289. [Google Scholar] [CrossRef] [PubMed]
- London, L.; Nell, V.; Thompson, M.L.; Myers, J.E. Effects of long-term organophosphate exposures on neurological symptoms, vibration sense and tremor among South African farm workers. Scand. J. Work. Environ. Health 1998, 24, 18–29. [Google Scholar] [CrossRef] [Green Version]
- Wesseling, C.; Keifer, M.; Ahlbom, A.; McConnell, R.; Moon, J.-D.; Rosenstock, L.; Hogstedt, C. Long-term Neurobehavioral Effects of Mild Poisonings with Organophosphate and n-Methyl Carbamate Pesticides among Banana Workers. Int. J. Occup. Environ. Health 2002, 8, 27–34. [Google Scholar] [CrossRef]
- Kim, J.Y.; Park, S.J.; Kim, S.K.; Kim, C.S.; Kim, T.H.; Min, S.H.; Oh, S.S.; Koh, S.B. Pesticide exposure and cognitive decline in a rural South Korean population. PLoS ONE 2019, 14, e0213738. [Google Scholar]
- Stallones, L.; Beseler, C.L. Assessing the connection between organophosphate pesticide poisoning and mental health: A comparison of neuropsychological symptoms from clinical observations, animal models and epidemiological studies. Cortex 2016, 74, 405–416. [Google Scholar] [CrossRef]
- Beseler, C.L.; Stallones, L.; Hoppin, J.A.; Alavanja, M.C.; Blair, A.; Keefe, T.; Kamel, F. Depression and pesticide exposures among private pesticide applicators enrolled in the Agricultural Health Study. Environ. Health Perspect. 2008, 116, 1713–1719. [Google Scholar] [CrossRef] [Green Version]
- Beseler, C.L.; Stallones, L. A cohort study of pesticide poisoning and depression in Colorado farm residents. Ann. Epidemiol. 2008, 18, 768–774. [Google Scholar] [CrossRef]
- Wesseling, C.; van Wendel de Joode, B.; Keifer, M.; London, L.; Mergler, D.; Stallones, L. Symptoms of psychological distress and suicidal ideation among banana workers with a history of poisoning by organophosphate or n-methyl carbamate pesticides. Occup. Environ. Med. 2010, 67, 778–784. [Google Scholar] [CrossRef] [Green Version]
- Beard, J.D.; Hoppin, J.A.; Richards, M.; Alavanja, M.C.; Blair, A.; Sandler, D.P.; Kamel, F. Pesticide exposure and self-reported incident depression among wives in the Agricultural Health Study. Environ. Res. 2013, 126, 31–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beard, J.D.; Umbach, D.M.; Hoppin, J.A.; Richards, M.; Alavanja, M.C.; Blair, A.; Sandler, D.P.; Kamel, F. Pesticide exposure and depression among male private pesticide applicators in the agricultural health study. Environ. Health Perspect. 2014, 122, 984–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curl, C.L.; Spivak, M.; Phinney, R.; Montrose, L. Synthetic Pesticides and Health in Vulnerable Populations: Agricultural Workers. Curr. Environ. Health Rep. 2020, 7, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wu, M.; Yao, H.; Yang, Y.; Cui, M.; Tu, Z.; Stallones, L.; Xiang, H. Pesticide poisoning and neurobehavioral function among farm workers in Jiangsu, People’s Republic of China. Cortex 2016, 74, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.M.; Harrison, V. Organophosphates II. Neurobehavioural Problems Following Low-Level Exposure: Methodological Considerations for Future Research. In A Handbook of Environmental Toxicology: Human Disorders and Ecotoxicology; CAB International: Wallingford, UK, 2020. [Google Scholar]
- Muñoz-Quezada, M.T.; Lucero, B.A.; Iglesias, V.P.; Muñoz, M.P.; Cornejo, C.A.; Achu, E.; Baumert, B.; Hanchey, A.; Concha, C.; Brito, A.; et al. Chronic exposure to organophosphate (OP) pesticides and neuropsychological functioning in farm workers: A review. Int. J. Occup. Environ. Health 2016, 22, 68–79. [Google Scholar] [CrossRef] [Green Version]
- Fuhrimann, S.; Winkler, M.S.; Staudacher, P.; Weiss, F.T.; Stamm, C.; Eggen, R.I.; Lindh, C.H.; Menezes-Filho, J.A.; Baker, J.M.; Ramirez-Munoz, F.; et al. Exposure to Pesticides and Health Effects on Farm Owners and Workers From Conventional and Organic Agricultural Farms in Costa Rica: Protocol for a Cross-Sectional Study. JMIR Res. Protoc. 2019, 8, e10914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winkler, M.S.; Atuhaire, A.; Fuhrimann, S.; Mora, A.M.; Niwagaba, C.; Oltramare, C.; Ramírez, F.; Ruepert, C.; Staudacher, P.; Weiss, F.; et al. Environmental Exposures, Health Effects and Institutional Determinants of Pesticide use in Two Tropical Settings. (working paper), Geneva. 31 March 2019. Available online: https://snis.ch/wp-content/uploads/2020/01/2014_Winkler_Working-Paper.pdf (accessed on 24 August 2021).
- Wesseling, C.; Aragon, A.; Rojas, M.; Blanco, L.; Lopez, L.; Soto, A.; Funez, A.; Ruepert, C.; Miranda, J.; Lopez, I. Efectos del Clorpirifos en la Salud de Trabajadores Bananeros de la Lima, Honduras; SALTRA, IRET-UNA, CISTA, UNAN-Leon: Heredia, Costa Rica, 2006. [Google Scholar]
- Rodezno, R.A.; Lundberg, I.; Escalona, E. Development of a questionnaire in Spanish on neurotoxic symptoms. Am. J. Ind. Med. 1995, 28, 505–520. [Google Scholar] [CrossRef]
- Derogatis, L.R. Brief Symptoms Inventory (BSI): Administration, Scoring and Procedures Manual 3rd edn. NCS Pearson, Inc.: Minneapolis, MN, USA, 1993. Available online: https://hazards.colorado.edu/nhcdata/chernobyl/ChData/ScalesInstruments/Scales%20and%20Indices/Scale%20Construction%20Instructions/BSI.pdf (accessed on 24 August 2021).
- Coelho, V.L.; Strauss, M.E.; Jenkins, J.H. Expression of symptomatic distress by Puerto Rican and Euro-American patients with depression and schizophrenia. J. Nerv. Ment. Dis. 1998, 186, 477–483. [Google Scholar] [CrossRef]
- Hemmings, M.; Reimann, J.O.; Madrigal, D.; Velasquez, R.J. Predictors of scores on the Brief Symptom Inventory for ethnically diverse female clients. Psychol. Rep. 1998, 83, 800–802. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2013; Available online: https://www.r-project.org/index.html (accessed on 24 August 2021).
- WHO. The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2009; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Kim, J.; Ko, Y.; Lee, W.J. Depressive symptoms and severity of acute occupational pesticide poisoning among male farmers. Occup. Environ. Med. 2013, 70, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Stevens, R.C.; MacCoss, M.J.; Goodlett, D.R.; Scherl, A.; Richter, R.J.; Suzuki, S.M.; Furlong, C.E. Identification and characterization of biomarkers of organophosphorus exposures in humans. Adv. Exp. Med. Biol. 2010, 660, 61–71. [Google Scholar]
- Fuhrimann, S.; Farnham, A.; Staudacher, P.; Atuhaire, A.; Manfioletti, T.; Niwagaba, C.B.; Namirembe, S.; Mugweri, J.; Winkler, M.S.; Portengen, L.; et al. Exposure to multiple pesticides and neurobehavioral outcomes among smallholder farmers in Uganda. Environ. Int. 2021, 152, 106477. [Google Scholar]
| Characteristics | Farmers Who Never Experienced APP (n = 257) | Farmers Who Experienced at Least One APP (n = 43) |
|---|---|---|
| Age (years) | 31.0 (24.0–46.0) | 50.0 (38.5–53.5) |
| Sex | ||
| Male | 231 (89.9) | 42 (97.7) |
| Female | 26 (10.1) | 1 (2.3) |
| Marital status | ||
| Married or living as married | 150 (58.4) | 33 (76.7) |
| Single | 99 (38.5) | 7 (16.3) |
| Separated/divorced/widowed | 8 (3.1) | 3 (7.0) |
| Job position | ||
| Farm owner | 86 (33.5) | 27 (62.8) |
| Farmworker | 171 (66.5) | 16 (37.2) |
| Country of birth | ||
| Costa Rica | 145 (56.4) | 32 (74.4) |
| Nicaragua | 112 (43.6) | 11 (25.6) |
| Education (years) | 6.0 (5.0–8.0) | 6.0 (6.0–6.0) |
| Smoking habits | ||
| Never | 129 (50.2) | 21 (48.8) |
| Former | 70 (27.3) | 17 (39.5) |
| Current | 58 (22.6) | 5 (11.6) |
| Number of drinks per week | 0.0 (0.0–4.0) | 0 (0.0–0.0) |
| Time applying pesticides (years) | 14.0 (7.0–28.0) | 34.0 (23.5–38.5) |
| Applicator of synthetic pesticides at time of interview | ||
| No | 68 (26.5) | 12 (27.9) |
| Yes | 189 (73.5) | 31 (72.1) |
| Household income (colones) | 320,000 (260,000–500,000) | 320,000 (228,000–600,000) |
| Household size | 4.0 (3.0–5.0) | 4.0 (2.5–5.0) |
| Training in safe practices for pesticide use | 98 (45.4) | 25 (65.8) |
| No | 118 (45.9) | 13 (30.2) |
| Yes | 98 (45.4) | 25 (65.8) |
| Pesticide use at time of interview | ||
| Time spent using pesticides (hours/week) | 8.0 (4.0–13.0) | 8.0 (4.0–21.0) |
| Used extremely or highly toxic pesticides in the last week (WHO classification Ia or Ib) | ||
| No | 200 (77.8) | 37 (86.0) |
| Yes | 34 (14.5) | 4 (9.8) |
| Symptom (Outcome) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Fainting | 4.99 (1.38, 17.40) | 7.48 (1.83, 30.74) |
| Shaking hands | 2.39 (1.17, 4.75) | 3.50 (1.60, 7.60) |
| Numbness or tingling in hands or feet | 3.30 (1.73, 6.27) | 3.23 (1.66, 6.32) |
| Insomnia | 2.44 (1.32, 4.47) | 2.53 (1.34, 4.79) |
| Accelerated heart rate | 2.38 (1.06, 5.09) | 2.42 (1.03, 5.47) |
| Dizziness | 2.59 (1.33, 5.01) | 2.38 (1.19, 4.72) |
| More irritable or angry than normal | 2.22 (1.19, 4.14) | 2.37 (1.23, 4.55) |
| Tired or low energy | 2.10 (1.14, 3.91) | 2.33 (1.23, 4.46) |
| Excessive salivation | 1.21 (0.39, 3.14) | 2.27 (0.67, 6.79) |
| Changes in ability to smell and taste | 1.86 (0.64, 4.71) | 2.23 (0.73, 6.17) |
| Difficulty concentrating | 1.91 (1.02, 3.53) | 2.01 (1.05, 3.85) |
| Excessive sweating/perspiration | 1.90 (0.85, 3.99) | 1.89 (0.82, 4.11) |
| Headache | 1.52 (0.83, 2.78) | 1.88 (0.99, 3.55) |
| Distracted, forgetful, or confused | 2.05 (1.11, 3.82) | 1.87 (0.99, 3.54) |
| Vomiting | 1.18 (0.42, 2.88) | 1.74 (0.58, 4.61) |
| Difficulty seeing at night | 1.97 (0.85, 4.26) | 1.67 (0.70, 3.75) |
| Unsteady walking | 1.93 (0.77, 4.43) | 1.59 (0.62, 3.73) |
| Tense, anxious or nervous | 1.90 (1.04, 3.48) | 1.57 (0.84, 2.94) |
| Nausea | 1.74 (0.81, 3.56) | 1.55 (0.70, 3.28) |
| Difficulty talking | 1.20 (0.27, 3.87) | 1.49 (0.32, 5.31) |
| Paleness | 1.11 (0.36, 2.85) | 1.41 (0.44, 3.90) |
| Loss of hunger/appetite | 1.10 (0.50, 2.25) | 1.40 (0.62, 3.00) |
| Weakness in arms and legs | 1.68 (0.84, 3.25) | 1.38 (0.68, 2.74) |
| Earache | 1.18 (0.42, 2.87) | 1.33 (0.46, 3.42) |
| Diarrhea | 1.23 (0.52, 2.66) | 1.12 (0.46, 2.49) |
| Abdominal or stomach pain | 0.97 (0.46, 1.94) | 1.11 (0.51, 2.32) |
| Blurred or double vision | 1.46 (0.70, 2.90) | 1.02 (0.47, 2.09) |
| Difficulty maintaining equilibrium | 1.22 (0.43, 2.97) | 0.99 (0.34, 2.47) |
| Felt scared/fear | 0.85 (0.38, 1.76) | 0.88 (0.38, 1.87) |
| Depressed, indifferent, or withdrawn | 0.99 (0.49, 1.93) | 0.87 (0.42, 1.72) |
| BSI Dimensions | Never Experienced APP (n = 257) | Experienced at Least One APP during Their Lifetime (n = 43) | Experienced at Least One APP during the Last 10 Years (n = 10) | Farmers from a 2010 Costa Rican Study Who had Experienced one APP 1–3 Years Previously (n = 43) [22] |
|---|---|---|---|---|
| Somatization | 0.29 (0.0, 0.57) | 0.29 (0.07, 0.64) | 0.36 (0.07, 1.11) | 0.86 (0.08, 1.65) |
| Obsession-compulsion | 0.50 (0.0, 1.0) | 0.50 (0.17, 1.0) | 0.75 (0.17, 1.46) | 0.83 (0.17, 1.50) |
| Interpersonal sensitivity | 0.25 (0.0, 0.75) | 0.25 (0.0, 0.75) | 0.25 (0.06, 0.94) | 0.50 (0.0, 1.0) |
| Depression | 0.17 (0.0, 0.67) | 0.17 (0.0, 0.5) | 0.50 (0.50, 0.67) | 0.33 (0.0, 1.0) |
| Anxiety | 0.17 (0.0, 0.67) | 0.33 (0.0, 0.75) | 0.58 (0.08, 1.17) | 0.40 (0.0, 1.0) |
| Hostility | 0.20 (0.0, 0.4) | 0.20 (0.0, 0.4) | 0.60 (0.20, 1.15) | 0.40 (0.0, 0.80) |
| Phobic anxiety | 0.0 (0.0, 0.4) | 0.0 (0.0, 0.4) | 0.40 (0.20, 0.90) | 0.40 (0.0, 1.0) |
| Paranoid ideation | 0.80 (0.2, 1.2) | 0.80 (0.2, 1.2) | 1.00 (0.85, 1.40) | 0.0 (0.0, 0.8) |
| Psychoticism | 0.20 (0.0, 0.8) | 0.20 (0.0, 0.6) | 0.60 (0.40, 1.25) | 0.25 (0.0, 0.75) |
| Global Severity Index (GSI) | 0.34 (0.11, 0.75) | 0.38 (0.18, 0.62) | 0.59 (0.42, 0.97) | 0.71 (0.28, 1.15) |
| BSI Dimensions | Never Experienced APP (n = 257) | Experienced at least One APP during Their Lifetime (n = 43) | Experienced at least One APP during the Last 10 Years (n = 10) | |||
|---|---|---|---|---|---|---|
| Prevalence n (%) | OR (95% CI) | Prevalence n (%) | OR (95% CI) | Prevalence n (%) | OR (95% CI) | |
| Somatization | 78 (30.4) | 1.0 | 12 (27.9) | 1.08 (0.49, 2.26) | 4 (40.0) | 1.57 (0.38, 5.88) |
| Obsession-compulsion | 61 (23.7) | 1.0 | 9 (20.9) | 1.05 (0.44, 2.33) | 3 (30.0) | 1.38 (0.29, 5.22) |
| Interpersonal sensitivity | 53 (20.6) | 1.0 | 10 (23.3) | 1.57 (0.67, 3.53) | 3 (30.0) | 1.80 (0.37, 7.03) |
| Depression | 57 (22.2) | 1.0 | 7 (16.3) | 0.82 (0.31, 1.92) | 2 (20.0) | 0.91 (0.13, 3.94) |
| Anxiety | 50 (19.5) | 1.0 | 11 (25.6) | 1.47 (0.65, 3.17) | 3 (30.0) | 2.0 (0.41, 7.65) |
| Hostility | 50 (19.5) | 1.0 | 7 (16.3) | 1.25 (0.46, 3.06) | 5 (50.0) | 4.51 (1.16, 17.70) |
| Phobic anxiety | 55 (21.4) | 1.0 | 8 (18.6) | 1.10 (0.44, 2.53) | 4 (40.0) | 2.55 (0.62, 9.52) |
| Paranoid ideation | 101 (39.3) | 1.0 | 19 (44.2) | 1.55 (0.77, 3.11) | 7 (70.0) | 3.76 (0.99, 18.18) * |
| Psychoticism | 77 (30.0) | 1.0 | 9 (20.9) | 0.87 (0.36, 1.92) | 5 (50.0) | 2.48 (0.65, 9.45) |
| Global Severity Index (GSI) | 81 (31.5) | 1.0 | 11 (25.6) | 0.91 (0.41, 1.92) | 5 (50.0) | 2.16 (0.57, 8.24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farnham, A.; Fuhrimann, S.; Staudacher, P.; Quirós-Lépiz, M.; Hyland, C.; Winkler, M.S.; Mora, A.M. Long-Term Neurological and Psychological Distress Symptoms among Smallholder Farmers in Costa Rica with a History of Acute Pesticide Poisoning. Int. J. Environ. Res. Public Health 2021, 18, 9021. https://doi.org/10.3390/ijerph18179021
Farnham A, Fuhrimann S, Staudacher P, Quirós-Lépiz M, Hyland C, Winkler MS, Mora AM. Long-Term Neurological and Psychological Distress Symptoms among Smallholder Farmers in Costa Rica with a History of Acute Pesticide Poisoning. International Journal of Environmental Research and Public Health. 2021; 18(17):9021. https://doi.org/10.3390/ijerph18179021
Chicago/Turabian StyleFarnham, Andrea, Samuel Fuhrimann, Philipp Staudacher, Marcela Quirós-Lépiz, Carly Hyland, Mirko S. Winkler, and Ana M. Mora. 2021. "Long-Term Neurological and Psychological Distress Symptoms among Smallholder Farmers in Costa Rica with a History of Acute Pesticide Poisoning" International Journal of Environmental Research and Public Health 18, no. 17: 9021. https://doi.org/10.3390/ijerph18179021
APA StyleFarnham, A., Fuhrimann, S., Staudacher, P., Quirós-Lépiz, M., Hyland, C., Winkler, M. S., & Mora, A. M. (2021). Long-Term Neurological and Psychological Distress Symptoms among Smallholder Farmers in Costa Rica with a History of Acute Pesticide Poisoning. International Journal of Environmental Research and Public Health, 18(17), 9021. https://doi.org/10.3390/ijerph18179021






