Abstract
There is growing interest in the ways natural environments influence the development and progression of long-term health conditions. Vegetation and water bodies, also known as green and blue spaces, have the potential to affect health and behaviour through the provision of aesthetic spaces for relaxation, socialisation and physical activity. While research has previously assessed how green and blue spaces affect mental and physical wellbeing, little is known about the relationship between these exposures and health outcomes over time. This systematic review summarised the published evidence from longitudinal observational studies on the relationship between exposure to green and blue space with mental and physical health in adults. Included health outcomes were common mental health conditions, severe mental health conditions and noncommunicable diseases (NCDs). An online bibliographic search of six databases was completed in July 2020. After title, abstract and full-text screening, 44 eligible studies were included in the analysis. Depression, diabetes and obesity were the health conditions most frequently studied in longitudinal relationships. The majority of exposures included indicators of green space availability and urban green space accessibility. Few studies addressed the relationship between blue space and health. The narrative synthesis pointed towards mixed evidence of a protective relationship between exposure to green space and health. There was high heterogeneity in exposure measures and adjustment for confounding between studies. Future policy and research should seek a standardised approach towards measuring green and blue space exposures and employ theoretical grounds for confounder adjustment.
1. Introduction
It is well established that noncommunicable diseases (NCDs) are the largest contributors to the global burden of disease []. NCDs are medical conditions that are non-infectious and non-transmittable from person to person, and in 2017 they accounted for 73% of all global deaths []. Cardiovascular disease (CVD), diabetes, cancer and chronic lung disease are the most prevalent NCDs [] but they often tend to co-occur with common and severe mental health conditions such as depression, schizophrenia and bipolar disorder []. The relationship between physical and mental health is bidirectional and characterised by complex interactions [,]. Poor mental health increases the risk of developing NCDs due to engagement in unhealthy behaviours and low help seeking [,]. Having a long-term physical health condition, on the other hand, puts people at greater risk of depression and anxiety due to reduced quality of life, treatment side effects and disability [,]. Physical activity, diet, alcohol consumption and smoking play an important role in moderating this relationship but also independently affect the risk of developing both mental and physical health conditions []. While these modifiable risk factors are key drivers of NCDs, environmental exposures have also emerged as important determinants of health []. Noise and air pollution are now proven contributors to the global burden of disease and there is currently growing interest in studying the pathways between the natural environment and the development and progression of long-term health conditions. [,]. Green and blue spaces are areas of varying size that have been colonised by plants and/or fresh or saltwater. They make up a large proportion of the natural environment and can be both naturally occurring or existing as a result of human intervention [,]. Overall, the effects of green and blue spaces on health can be summarised by three major biopsychosocial pathways: reduction in harm (capturing and limiting air pollution, noise and heat); restoring capabilities (restoring attention and reducing stress); and building capacities (improving physical activity and social cohesion) [,,,,,].
There is now ample evidence about the relationship between exposure to different types of green and blue spaces and health. Cross-sectional research found greater exposure to an amount of green space and a blue space aesthetic (view from the window) to increase the odds of having good self-perceived general health [,]. A study on morbidity in primary care also deduced that, in general, having 10% more green space than average in the surrounding environment is associated with a lower risk of having mental and physical morbidity []. This relationship was stronger when green space was captured in a 1 km circular buffer than in a 3 km buffer []. Small reductions in CVD events, and the risk of all-cause and respiratory mortality were also observed with an increasing amount of greenness by cohort studies and meta-analysis [,,]. Moreover, the size of urban green spaces affects the odds of having multimorbidity, as those with CVD and/or diabetes living near a park with a relatively small area had 3.1 times higher odds of having depression compared to those who lived near a park with a big area []. These relationships also vary by sociodemographic characteristics. Some studies have shown that the health benefits of green spaces are greater for those of low socioeconomic status (SES), nonwhite ethnicity and male sex [,,].
Several systematic reviews of epidemiological studies have summarised the relationships between green and blue spaces and health [,,,,,,]. While greater exposure to green space was associated with better mental and physical wellbeing [], better general self-perceived health [], reduced risk of all-cause mortality [], reduced risk of CVD mortality, diabetes and preterm birth []; no relationship was observed for mental ill-health [], cognitive functioning [], urbanisation-related health conditions [] and long-term physical health conditions []. Plausible explanations for this included poor study quality, study type or heterogeneity in exposure measurements [,,]. Earlier systematic reviews studying the relationship between exposure to green space and physical long-term health conditions also found the literature to be saturated with cross-sectional studies that cannot prove causality [,,].
It is apparent that a broad range of health and wellbeing outcomes have been studied in systematic reviews on green and blue space. However, the effect of the natural environment on the development of highly prevalent long-term mental and physical health conditions over time is still uncertain. This systematic review addresses several gaps in the literature. First, it captures only longitudinal observational data to study the relationship between exposures to green and blue spaces with long-term mental and physical health conditions. Longitudinal, observational studies are important in deducing causality and informing public health interventions []. Government bodies, such as Public Health England [], have called for a need to improve quality, engagement and access to green spaces to promote good health, acknowledging there is high variation in the ways environmental exposures and types of health outcomes are used in research. Including both green and blue space exposure further addresses the methodological approaches in exposure measurements and aids the understanding of underlying mechanisms in the relationship. Thirdly, our systematic review aims to examine the relationship between exposure to green and blue spaces with the development and progression of multimorbidity. While prior systematic reviews have attempted to ascertain the relationship between the natural environment and single long-term conditions [,], little is known about the natural environment’s role in the development of multiple chronic conditions within an individual. Multimorbidity is a growing concern among aging populations because it reduces individuals’ quality of life, increases the risk of disability and puts financial strain on health systems []. Fourthly, the inclusion of both mental and physical health outcomes offers opportunities to identify differences in the direction and strength of associations between different outcomes.
This review, therefore, aims to:
- 1.
- Assess whether a significant relationship between exposures and outcomes exists.
- 2.
- Identify the type of environmental exposures, type of health conditions and behaviours studied together in longitudinal relationships.
- 3.
- Determine whether multimorbidity as a concept is studied in relation to different green/blue space exposures.
2. Materials and Methods
The Preferred Reporting Items for Systematic reviews and Meta-Analyses for Protocols (PRISMA-P) statement was used as guidance in protocol preparation and review reporting []. A protocol was registered via the International Prospective Register of Systematic Reviews (PROSPERO), identification number: CRD42020175965.
2.1. Selection Criteria
Studies published in academic journals in English were included. No date restrictions were applied. Only studies of a longitudinal, observational design with a population of male and/or female adults (mean population age: 18 years or older) were included. Populations with pre-existing health conditions and populations without pre-existing health conditions at baseline were included. Any study measuring green and/or blue space exposure that fits the broadly accepted definition of an area of naturally growing outdoor vegetation and/or water body was included. Studies that used objective (e.g., remote sensing) and/or subjective (self-reports) measures of green and blue spaces were eligible for inclusion. The primary outcome was mental and/or physical health. Mental health conditions included those which are classified by the National Institute for Health and Care Excellence NICE [,] as common (depression, generalised anxiety disorder (GAD), panic disorder, phobias, social anxiety disorder, obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD)) and severe mental health disorders (bipolar disorder, psychosis and schizophrenia). As defined by the Centre for Diseases Control, physical health included NCDs with a duration of one year or more that “require ongoing medical attention or limit activities of daily living or both” []. Secondary outcomes related to health were also included: health-related behaviours (physical activity, diet, smoking, alcohol consumption), physical functioning, frailty and health-related quality of life (QoL). Eligible outcomes were included if they were reported via structured clinical interviews or by validated self-reported instruments.
The search strategy was compiled in consultation with an information specialist from the University of York Centre for Reviews and Dissemination. A search strategy striving for high sensitivity was run on 17 July 2020 in six online databases: Embase, GreenFILE, MEDLINE, PsycINFO, Scopus, Science Citation Index (see Supplementary Material S1). Search terms for longitudinal study design, green and blue space exposures, and mental and physical health were included and combined with appropriate Boolean operators.
2.2. Data Extraction
Retrieved records were imported into Rayyan, a web-based application commonly used as a screening aid. Rayyan is a validated tool for systematic review screening that allows for flexibility in setting screening standards [,]. After duplicates were identified and removed, study titles and abstracts were screened against the inclusion and exclusion criteria by one reviewer (MG). Following this, the full text of each potentially eligible study was screened by one reviewer (MG). Reference lists of studies were also screened for potentially eligible records. Uncertainty about the inclusion of a study at all stages of the screening process was resolved through consensus meetings with a second reviewer or an attempt to contact the authors for clarification. Relevant data from selected studies were extracted into Microsoft Excel using a prespecified data extraction form adapted from Cochrane [,] by the reviewers to suit longitudinal observational studies (see Supplementary Material S2). Data extraction was executed by one reviewer (MG) and accompanied by consensus meetings with a second reviewer to resolve uncertainties.
2.3. Quality Appraisal
The Newcastle–Ottawa Scale (NOS) was used for risk of bias assessment. It is endorsed by the Cochrane as a suitable tool for observational cohort and case-control studies [,] with established validity and interrater reliability []. NOS consists of three domains that assess the quality of the cohort study. These include selection of the study based on the representativeness of cohort and exposure measures; comparability based on the design or analysis; and outcome assessment, including loss and adequacy of follow-up. A star was awarded if a study met the criteria specified by NOS’ developers (See Supplementary Material S3) [,]. The overall rating of the study was based on the sum of the stars across all domains. Good quality was awarded if a study scored 3 or 4 stars on the selection domain and 1 or 2 stars on the comparability domain and 2 or 3 stars on the outcome domain. Fair quality was awarded if a study scored 2 stars on the selection domain and 1 or 2 stars on the comparability domain and 2 or 3 stars on the outcome domain. Poor quality was awarded to those studies that scored 0 or 1 star on the selection domain or 0 stars on the comparability domain or 0 or 1 star on the outcome domain (See Supplementary Material S3 for more information) []. This tool allowed for selection and information bias to be assessed, particularly, sampling bias, differential loss to follow-up and confounding. One reviewer (MG) conducted the quality appraisal.
3. Results
3.1. Overview
The PRISMA-P flowchart in Figure 1 shows the process of identification, screening and inclusion of studies. The search yielded 24,176 studies after removal of duplicates (Figure 1). Of these, 23,941 were excluded during the title and abstract screening stage, leaving 233 studies for full-text assessment. One hundred and eighty-nine full-text records were excluded during that stage, leaving 44 studies for the qualitative narrative synthesis. Just under half (n = 90, 47.6%) of the excluded studies in the full-text screening stage did not include a green or blue space exposure, while another 38 (20.1%) studies did not have an observational longitudinal study design. A further 37 (19.6%) studies were excluded based on outcome, which either did not fit the definition of an NCD (n = 22), measured mortality (n = 3), did not use a validated instrument (n = 4), examined acute and/or infectious diseases (n = 7), or did not include a health condition (n = 1). Six studies were excluded because of the population type (all children) and 13 because of the publication type (one dissertation and twelve conference papers). Two records were also excluded because they were duplicates (See Supplementary Material S4).
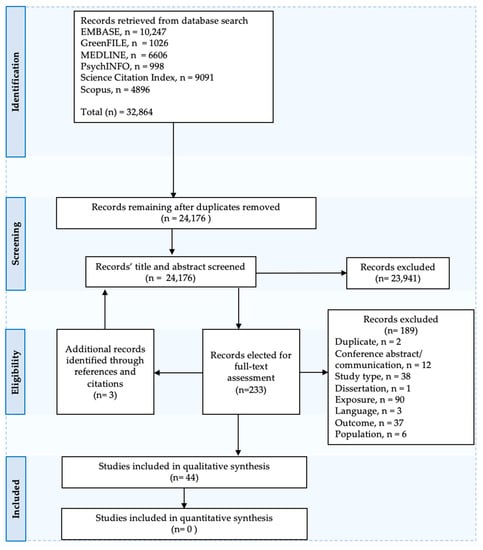
Figure 1.
PRISMA-P Flowchart.
Forty-four independent studies were included in the narrative synthesis [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. The majority (n = 42) were published between 2010 and 2020 and based in high-income countries (n = 35) (Table 1). Nine studies were based in middle- and low-income countries. Study populations mainly comprised of adults aged 35 years or older (n = 31) (Table 1). Seven studies included populations of all age groups and another six included young adults (18–35 years). Most studies included both men and women participants (n = 35). Six studies included only female participants [,,,,,] and one study included only male participants [] (Table 1). Almost all studies (n = 42, 95%) included predominantly healthy populations at baseline. Two studies included people with pre-existing health conditions, of which both were diabetes [,].

Table 1.
Summary of study characteristics, results and quality appraisal.
3.2. Quality Assessment
The methodological quality of more than half of all the included studies was rated as good (n = 24, 54.5%). Around one third (n = 14, 31.8%) of the studies scored poor and the rest (n = 6, 13.65%) scored fair on the overall NOS rating. Most studies scored high on the comparability domain of the scale, which assessed bias due to confounding. In general studies scored low on the selection and outcome domains (see Supplementary Material S5).
3.3. Exposures and Outcomes
Figure 2a,b provides an overview of the type and frequency of exposures and primary outcomes of the studies. Some studies used multiple indicators of green and blue space exposures and assessed more than one relevant outcome (see Table 1 for more information). There was high variation in exposure indicators, but a large proportion measured green space availability. The Normalised Difference Vegetation Index (NDVI) was the most frequently used indicator of green space availability, followed by percent green space. Almost all accessibility indicators measured either distance or presence of an urban park. One study measured green space usage [], while only four studies measured exposure to blue space [,,,].
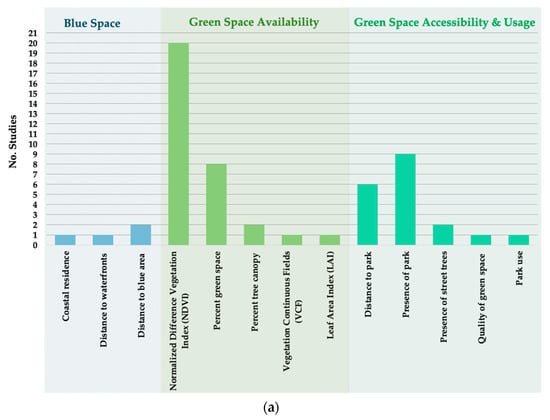
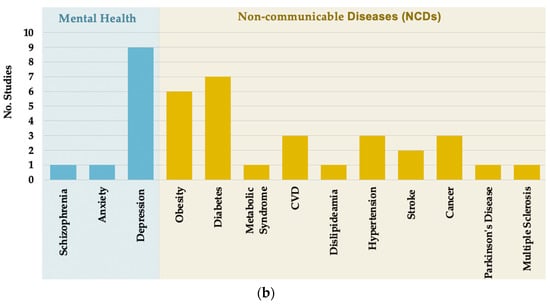
Figure 2.
Frequency and type of selected studies by: (a) exposure; (b) primary outcome.
Studies examined a wide range of mental and physical health outcomes. Depression was the most frequently studied (n = 9) mental health outcome. One study examined anxiety and another schizophrenia. Ten different types of NCDs were identified, of which diabetes (n = 7), obesity (n = 6), CVD (n = 3), hypertension (n = 3), cancer (n = 3) and stroke (n = 2) were most frequently studied (Figure 2b).
3.4. Relationship between Exposure to Green and Blue Space and Mental and Physical Health
Table 1 presents a summary of the effect estimates for the relationship between green and blue spaces with all relevant outcomes of this review. Overall, there was mixed evidence of a relationship between exposures and outcomes. Nine studies examined whether green space affects the risk of developing depression [,,,,,,,,] but six of those did not find a statistically significant association (n = 6) (Table 1) [,,,,,]. Out of those with a significant relationship, two studies found a small reduction [,], while one study found a small increase in the risk of depression with a greater availability of green space []. One study [] found a high reduction in the risk of developing schizophrenia in those exposed to the highest quintile of NDVI compared with those exposed to the lowest quintile (HR (95% CI): 0.37 (0.25, 0.55)).
There was also mixed evidence of a relationship between exposure to green and blue space and the development of NCDs. Four studies found the risk of developing diabetes was reduced with greater exposure to an amount of green space [,,,]. The rest (n = 3) found no statistically significant relationship [,,]. All studies about CVD showed a significant reduction in the risk of having CVD events with a greater exposure to green space [,,]. On the other hand, only two out of six studies on the development of obesity found a statistically significant relationship [,]. A small reduction in the risk of developing cancer was also observed with a greater exposure to green space in one out of three studies [].
Evidence across the retrieved studies suggests there is only a partial temporal relationship between exposure to green spaces and mental and physical health. CVD and diabetes were the conditions with strongest evidence of a protective relationship with green space. There was some evidence that the type of green space influences the relationship with health []. Astell-Burt and Feng [] found exposure to a greater percent of tree canopy, but not a greater percent of total green space (tree canopy and grass cover), moderately decreased the risk of developing CVD, diabetes and hypertension. While some studies found exposure spatial scales (e.g., size of distance buffers) attenuated the relationship [,], in sensitivity analyses most studies found no change in effect estimates when analyses were repeated using different buffer sizes (see Supplementary Material S6). Confounding variables also varied among studies, but all adjusted for sociodemographic characteristics. Some studies additionally adjusted for environmental variables, such as season, noise, air pollution and humidity [,,,,,] and health behaviours, like physical activity [,,,,,,,]. No differences in relationships were observed between studies that adjusted only for sociodemographic variables and those that additionally adjusted for environmental and behavioural factors.
3.5. Relationship between Green Space and Physical Activity
Physical activity was the most frequently studied outcome in this review (n = 13). Over half of the studies (n = 7) measured physical activity by type, such as walking, jogging, cycling. The rest measured total physical activity over the course of a prespecified time period (Table 1). Only five studies found a significant association between green space exposure and physical activity [,,,,]. There was some variation in adjustment for confounding variables between studies, but most adjusted for sociodemographic and neighbourhood contextual variables. Over half of the studies (n = 7) additionally adjusted for health status, including BMI, physical functioning and chronic diseases [,,,,,,]. However, no patterns between confounding and statistically significant findings could be identified. While one study found differences in results between exposure buffer sizes [], in sensitivity analyses, two studies found that the effect estimates did not change when green space was measured at different spatial scales (using different buffer sizes) [,].
3.6. Multimorbidity
This review found negligible evidence in the published literature of a longitudinal relationship between multimorbidity and green and/or blue space. One study examined how green space exposure affects the development of depression in adults with diabetes at baseline [] and found no significant association between higher NDVI values and incident depression at the 5-year follow-up. Two studies additionally observed a general trend of improvement in frailty status with increasing greenness [,]. Despite being a concept closely related to multimorbidity, the studies on frailty did not conceptualise or measure multimorbidity.
4. Discussion
4.1. Relationship between the Natural Environment and Health
This systematic review showed there is currently minimal evidence of a consistent, significant longitudinal relationship between exposure to green and blue space and mental and physical health. Where statistically significant relationships existed, the associations were quite weak. Highest reductions in the risk of developing long-term health conditions with greater exposure to green space was observed for diabetes, CVD, stroke and schizophrenia. While prior systematic reviews and observational studies have shown there to be some significant cross-sectional associations between depression, diabetes and obesity [,,,,], this systematic review concludes the relationship does not generally hold longitudinally. Due to the recent nature of the research, the reasons behind this are not entirely clear. One potential explanation could be the methodological design of longitudinal studies and the measurement of environmental exposures. First, the heterogeneity of green space exposure measures is well documented in the academic literature [,,]. This is also supported by studies in our systematic review. A range of data sources, including remote sensed imagery from land use maps, regional government databases and self-reported information, is commonly used to ascertain green space exposure in the neighbourhood []. Such data sources are often incomplete and provide a varying degree of accuracy, which increases the difficulty of sourcing enough data to measure green space both at baseline and follow-up. Very often, green space exposures in longitudinal studies are measured only at one point in time with the assumption that the presence of vegetation doesn’t change drastically over time [,,,,,,,,,,,,,,,,,,,,,]. However, urban areas undergoing regeneration or expansion may experience drastic changes in the amount and availability of greenery []. While cross-sectional studies only measure green space at a single point in time, longitudinal studies require multiple and complex exposure measurements. The unavailability of data to assess these changes in exposure over time could be a reason for the lack of longitudinal relationships.
Another potential explanation for the differences in results between cross-sectional and longitudinal studies could be the duration of follow-up of longitudinal studies. The dosage and duration of green space exposures required to influence health is still not entirely understood. However, there is some evidence that environmental factors in childhood and even from preconception and birth can shape the health of a person decades later []. Sensitive periods during human development are discrete time points at which certain environmental stimuli must be encountered for mental and physical development to occur []. The need to incorporate a life-course approach when studying the effects of green spaces on health has been previously highlighted, but its feasibility requires extensive utilisation and interpolation of historical data from varying sources []. While positive associations between green space and health observed in cross-sectional studies may be caused by sample size or sampling bias, the lack of relationship at a longitudinal level may be due to the low duration of follow-up. More research, therefore, is required to understand whether exposure to green space during sensitive periods of human development affects health later in life. This would better inform the duration of follow-up and study design of future longitudinal research.
It should be noted that our systematic review examined a broad range of mental and physical health outcomes, which yielded different strengths of associations. A finding that stood out was the relationship between exposure to green space and schizophrenia []. Chang et al. [] found the risk of developing schizophrenia to be reduced by 63% (HR (95% CI): 0.37 (0.25, 0.55)) in those exposed to the highest quintile NVDI compared to those exposed to the lowest. This is consistent with prior research on the relationship between green space and schizophrenia []. The reasoning behind these findings is not entirely clear but it is known that the risk of schizophrenia is often influenced by environmental exposures such as air pollution and urbanicity []. Biological mechanisms that affect brain development is a potential explanation for the increased risk of developing schizophrenia with greater exposure to air pollution []. As green spaces have the ability to reduce and capture air pollution, it is plausible that they counteract the negative effects of hazardous environmental factors.
Confounding could be a potential contributor to differences in results between studies included in this systematic review. Variation in confounding between studies was observed, but most adjusted for sociodemographic variables, such as age, sex and socioeconomic position. Although some studies additionally adjusted for physical activity, air quality and noise, no differences in relationships could be observed between minimally adjusted studies and those adjusting for additional environmental and behavioural variables. The review deduced there is currently no consensus on appropriate confounder adjustment, but it should be acknowledged that additional contextual factors like the built environment and clinical characteristics can also have an impact on the relationship. For example, studies have shown that neighbourhoods with high crime, deprivation, social disorganisation, a high retail density and land-use mix, can increase the risk of depression [,]. It is also hypothesised that further consideration of childcare duties and types of work might play an important role in the ways people utilise and interact with their environment []. We found that studies in this systematic review generally lacked adjustment for such variables, possibly due to a lack of such data in health cohorts.
Apart from confounding, differences in results could be due to exposure measurements. This review found a broad range of exposure indicators were used to conceptualise green space. The NDVI, percent green space and distance to park were the most frequently used, however, there was high heterogeneity between studies on the choice of spatial scale and exposure classes. Buffer sizes, time-of-year NDVI measurements and other green space exposure data sources varied, making meaningful comparisons between studies difficult and a potential reason for the differences in results. These findings have been previously flagged in prior systematic reviews [,,]. Where studies examined the type of green space, they mainly included urban parks. For most, this was measured as either the distance from the residential address or presence within a distance buffer. These are common measures of green space accessibility [] but have some limitations. First, such spatial measures fail to capture specific characteristics and features of urban parks. Some research, for example, indicates that physical activity is higher in parks with paved trails [], and visits to green spaces are more likely to occur if they have certain attributes, like trees, toilets, gym facilities, and the presence of lakes, ponds and trees [,]. Only one study included in this systematic review conducted a comparative analysis between exposure to trees and the total amount of vegetation in the neighbourhood []. They found the risk of CVD, diabetes and hypertension were all reduced with greater exposure to percent tree canopy cover, but not with greater exposure to percent total green space []. Greater exposure to street trees has been previously shown to reduce the odds of having hypertension [] and poor mental health []. While other studies of this review compared effect estimates using different buffer sizes (and found negligible differences), this finding suggests that it is the type and location of green spaces rather than the spatial scale that affects health. However, further comparative research is needed to establish this.
4.2. Strengths and Limitations
To the best of our knowledge, this is the first systematic review to summarise the published longitudinal literature on the relationship between green and blue spaces and chronic health. This is important for informing intervention design and policy decision making. According to the Medical Research Council’s framework for evaluating complex interventions [], appropriate methods need to be employed to first identify existing evidence and use it to guide theory development that is critical to intervention design. This systematic review contributed to the identification and synthesis of existing evidence and could help bridge the gap between empirical research and the development of programme theory about the role of green space in the maintenance of mental and physical health. Including both mental and physical health outcomes as well as related health states and behaviours additionally allowed for a comprehensive analysis and summary of the effects of the natural environment on highly prevalent NCDs and mental health problems. It also enabled comparisons of the strength and direction of associations. The choice to include both green and blue spaces as exposures, on the other hand, better informed of current research gaps in the published literature on the relationships between water bodies and health. Lastly, we summarised the limited evidence of longitudinal relationships between green and blue spaces and multimorbidity. While prior systematic reviews have assessed the effects of green spaces on health, they have not considered how these exposures may influence the development of multiple chronic conditions within an individual [,,,,,,]. This systematic review, therefore, flags additional research gaps in the study of multimorbidity development in relation to the natural environment.
There are a number of limitations. First, heterogeneity in study exposures and populations prevented us from conducting a quantitative synthesis analysis. While a narrative synthesis enabled a summary of results and associations, a meta-analysis may improve generalisability of the results by producing a pooled effect estimate and identifying sources of heterogeneity and bias []. Second, the Newcastle–Ottawa Scale is not as robust and as comprehensive a measure as ROBINS-I which is widely regarded as offering gold standard assessments of risk of bias of nonrandomised intervention studies []. The exposure domain on the Newcastle–Ottawa Scale might not be optimal for assessing information bias because it only classifies the quality of a study as good if the exposure is measured through objective measures. In the context of our review, objective measurements of green space are typically made by professional assessments or satellite imagery. However, self-reported exposures of natural environments are important in assessing the ways people interact with these spaces and may not necessarily introduce recall bias like clinical exposures []. Additionally, the Newcastle–Ottawa Scale includes domains that are critical to assessing key parameters of methodological quality of longitudinal cohort studies and in this sense functioned as a pragmatic solution for this review.
4.3. Review Implications
Despite the qualitative analysis of this review showing little relationship of exposure to green and blue space with health, this systematic review aided the identification of some key research gaps. First, there is a lack of framework to study the type and components of green and blue spaces on health. Longitudinal research has typically used an average estimation of green space availability or accessibility, and this is loosely based on European Environment Agency [] and Natural England’s [] recommendations of having an accessible green area of at least 2 ha no more than 300 m or within a 15-min walk from the residential address. Future research, however, should adopt a more holistic approach whereby different characteristics, dosage of exposure and specific person–environment interactions are studied in relation to health. This could improve the understanding of the different pathways between green space exposure and health, and lead to the design and implementation of evidence-based public health interventions.
Second, there is a need for more research into the relationship between blue space and health, as only four longitudinal studies were identified [,,,]. Prior academic literature has conceptualised the relationship between blue space and health to be driven by socio-environmental factors similar to those for green space []. Unlike green space, health policy recommendations for accessibility or availability of blue space are limited and primarily focused on coastal zones []. Government bodies and environmental agencies, therefore, should seek to develop more robust guidelines based on empirical research.
Finally, this review identified a lack of research into the ways green and blue spaces affect the development of multiple chronic conditions within an individual, also known as multimorbidity. The management of multimorbidity usually requires complex clinical interventions that have a negative impact on quality of life and put strain on healthcare systems [,,]. Green and blue spaces can influence behavioural change and promote good health through socio-ecological pathways and so the natural environment could play an important role in reducing the multimorbidity burden by preventing the onset or slowing the progression of several chronic conditions.
5. Conclusions
This systematic review showed there to be mixed evidence of a longitudinal relationship between green and blue spaces and mental and physical health, with just over half of all analyses indicating a nonsignificant relationship between exposures and health outcomes. The majority of published longitudinal observational studies assess exposure to green space through indicators of availability or urban green space accessibility. Few studies assess the effects of blue spaces on health. There was high heterogeneity between studies in exposure measures and confounding. This could be explained by a lack of existing framework and uniform guidelines on studying the effects of the natural environment on health. Future longitudinal research should incorporate a more holistic approach towards conceptualising green and blue space that moves beyond the amount or distance and towards capturing types and characteristics. This could greatly aid the understanding of causal pathways and improve intervention design.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18179010/s1, Supplementary Material S1: Search Strategy, Supplementary Material S2: Data extraction form adapted from Cochrane, Supplemental Material S3: NOS scale manual for cohort studies, Supplemental Material S4: Summary of excluded studies during full-text screening, Supplementary Material S5: Table of studies’ NOS rating, Supplementary Material S6: Summary of studies’ sensitivity analyses.
Author Contributions
Conceptualisation, M.G., P.C., J.C., S.G.; methodology, M.G., P.C., J.C., S.G.; software, M.G.; validation, M.G., P.C., J.C., S.G.; formal analysis, M.G.; investigation, M.G.; resources, M.G., P.C., J.C., S.G.; data curation, M.G.; writing—original draft preparation, M.G.; writing—review and editing, P.C., J.C.; visualisation, M.G.; supervision, P.C., J.C., S.G.; project administration, M.G., P.C., J.C., S.G.; funding acquisition, P.C., S.G. All authors have read and agreed to the published version of the manuscript.
Funding
The research was funded by the NIHR Applied Research Collaboration Yorkshire and Humber https://www.arc-yh.nihr.ac.uk/. The views expressed are those of the author(s), and not necessarily those of the NIHR or the Department of Health and Social Care.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. All data used in the production of this review are included in the published studies.
Acknowledgments
We would like to thank Cath Wright from the Centre for Reviews and Dissemination at the University of York for her help and advice with designing and conducting the search strategy of the systematic review.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Coates, M.M.; Kintu, A.; Gupta, N.; Wroe, E.B.; Adler, A.J.; Kwan, G.F.; Park, P.H.; Rajbhandari, R.; Byrne, A.L.; Casey, D.C.; et al. Burden of non-communicable diseases from infectious causes in 2017: A modelling study. Lancet Glob. Health 2020, 8, e1489–e1498. [Google Scholar] [CrossRef]
- Kim, H.C.; Oh, S.M. Noncommunicable diseases: Current status of major modifiable risk factors in Korea. J. Prev. Med. Public Health 2013, 46, 165. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Benjet, C.; Gureje, O.; Lund, C.; Scott, K.M.; Poznyak, V.; van Ommeren, M. Integrating mental health with other non-communicable diseases. BMJ 2019, 28, 364. [Google Scholar] [CrossRef] [Green Version]
- Prince, M.; Patel, V.; Saxena, S.; Maj, M.; Maselko, J.; Phillips, M.R.; Rahman, A. No health without mental health. Lancet 2007, 370, 859–877. [Google Scholar] [CrossRef]
- Steinmo, S.; Hagger-Johnson, G.; Shahab, L. Bidirectional association between mental health and physical activity in older adults: Whitehall II prospective cohort study. Prev. Med. 2014, 66, 74–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, B.E.; Edmondson, D.; Kronish, I.M. State of the art review: Depression, stress, anxiety, and cardiovascular disease. Am. J. Hypertens. 2015, 28, 1295–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caruso, R.; GiuliaNanni, M.; Riba, M.B.; Sabato, S.; Grassi, L. Depressive spectrum disorders in cancer: Diagnostic issues and intervention. A critical review. Curr. Psychiatry Rep. 2017, 19, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Patel, V.; Chatterji, S. Integrating mental health in care for noncommunicable diseases: An imperative for person-centered care. Health Aff. 2015, 34, 1498–1505. [Google Scholar] [CrossRef] [Green Version]
- Saxena, S.; Maj, M. Physical health of people with severe mental disorders: Leave no one behind. World Psychiatry 2017, 16, 1. [Google Scholar] [CrossRef] [Green Version]
- Prüss-Ustün, A.; van Deventer, E.; Mudu, P.; Campbell-Lendrum, D.; Vickers, C.; Ivanov, I.; Forastiere, F.; Gumy, S.; Dora, C.; Adair-Rohani, H.; et al. Environmental risks and non-communicable diseases. BMJ 2019, 364, l265. [Google Scholar] [CrossRef] [Green Version]
- Brulle, R.J.; Pellow, D.N. Environmental justice: Human health and environmental inequalities. Annu. Rev. Public Health 2006, 27, 103–124. [Google Scholar] [CrossRef] [Green Version]
- McDougall, C.W.; Quilliam, R.S.; Hanley, N.; Oliver, D.M. Freshwater blue space and population health: An emerging research agenda. Sci. Total Environ. 2020, 737, 140196. [Google Scholar] [CrossRef] [PubMed]
- Alcock, I.; White, M.P.; Lovell, R.; Higgins, S.L.; Osborne, N.J.; Husk, K.; Wheeler, B.W. What accounts for ‘England's green and pleasant land’? A panel data analysis of mental health and land cover types in rural England. Landsc. Urban Plan. 2015, 142, 38–46. [Google Scholar] [CrossRef] [Green Version]
- Wolch, J.R.; Byrne, J.; Newell, J.P. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough’. Landsc. Urban Plan. 2014, 125, 234–244. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.C.; Maheswaran, R. The health benefits of urban green spaces: A review of the evidence. J. Public Health 2011, 33, 212–222. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.J.; Khreis, H.; Triguero-Mas, M.; Gascon, M.; Dadvand, P. Fifty shades of green. Epidemiology 2017, 28, 63–71. [Google Scholar] [CrossRef]
- Maas, J.; Van Dillen, S.M.; Verheij, R.A.; Groenewegen, P.P. Social contacts as a possible mechanism behind the relation between green space and health. Health Place 2009, 15, 586–595. [Google Scholar] [CrossRef] [Green Version]
- Van den Berg, M.M.; van Poppel, M.; van Kamp, I.; Ruijsbroek, A.; Triguero-Mas, M.; Gidlow, C.; Nieuwenhuijsen, M.J.; Gražulevičiene, R.; van Mechelen, W.; Kruize, H.; et al. Do physical activity, social cohesion, and loneliness mediate the association between time spent visiting green space and mental health? Environ. Behav. 2019, 51, 144–166. [Google Scholar] [CrossRef]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; De Vries, S.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.J.; et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef] [PubMed]
- de Vries, S.; Verheij, R.A.; Groenewegen, P.P.; Spreeuwenberg, P. Natural environments—healthy environments? An exploratory analysis of the relationship between greenspace and health. Environ. Plan. A 2003, 35, 1717–1731. [Google Scholar] [CrossRef] [Green Version]
- Garrett, J.; White, M.P.; Huang, J.; Ng, S.; Hui, Z.; Leung, C.; Tse, S.; Fung, F.; Elliott, L.R.; Depledge, M.H.; et al. The association between blue space exposure, health and wellbeing in Hong Kong. Health Place 2019, 55, 100–110. [Google Scholar] [CrossRef]
- Maas, J.; Verheij, R.A.; de Vries, S.; Spreeuwenberg, P.; Schellevis, F.G.; Groenewegen, P.P. Morbidity is related to a green living environment. J. Epidemiol. Community Health 2009, 63, 967–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villeneuve, P.J.; Jerrett, M.; Su, J.G.; Burnett, R.T.; Chen, H.; Wheeler, A.J.; Goldberg, M.S. A cohort study relating urban green space with mortality in Ontario, Canada. Environ. Res. 2012, 115, 51–58. [Google Scholar] [CrossRef]
- Rojas-Rueda, D.; Nieuwenhuijsen, M.J.; Gascon, M.; Perez-Leon, D.; Mudu, P. Green spaces and mortality: A systematic review and meta-analysis of cohort studies. Lancet Planet. Health 2019, 3, e469–e477. [Google Scholar] [CrossRef] [Green Version]
- Seo, S.; Choi, S.; Kim, K.; Kim, S.M.; Park, S.M. Association between urban green space and the risk of cardiovascular disease: A longitudinal study in seven Korean metropolitan areas. Environ. Int. 2019, 125, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, D.; Safraj, S.; Tayyab, M.; Shivashankar, R.; Patel, S.A.; Narayanan, G.; Ajay, V.S.; Ali, M.K.; Narayan, K.V.; Tandon, N.; et al. Park availability and major depression in individuals with chronic conditions: Is there an association in urban India? Health Place 2017, 47, 54–62. [Google Scholar] [CrossRef]
- Roe, J.; Aspinall, P.A.; Ward Thompson, C. Understanding relationships between health, ethnicity, place and the role of urban green space in deprived urban communities. Int. J. Environ. Res. Public Health 2016, 13, 681. [Google Scholar] [CrossRef] [Green Version]
- Richardson, E.A.; Mitchell, R. Gender differences in relationships between urban green space and health in the United Kingdom. Soc. Sci. Med. 2010, 71, 568–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gascon, M.; Triguero-Mas, M.; Martínez, D.; Dadvand, P.; Forns, J.; Plasència, A.; Nieuwenhuijsen, M.J. Mental health benefits of long-term exposure to residential green and blue spaces: A systematic review. Int. J. Environ. Res. Public Health 2015, 12, 4354–4379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gascon, M.; Zijlema, W.; Vert, C.; White, M.P.; Nieuwenhuijsen, M.J. Outdoor blue spaces, human health and well-being: A systematic review of quantitative studies. Int. J. Hyg. Environ. Health 2017, 220, 1207–1221. [Google Scholar] [CrossRef]
- Van den Berg, M.; Wendel-Vos, W.; Van Poppel, M.; Kemper, H.; van Mechelen, W.; Maas, J. Health benefits of green spaces in the living environment: A systematic review of epidemiological studies. Urban For. Urban Green. 2015, 14, 806–816. [Google Scholar] [CrossRef]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef] [PubMed]
- de Keijzer, C.; Gascon, M.; Nieuwenhuijsen, M.J.; Dadvand, P. Long-term green space exposure and cognition across the life course: A systematic review. Curr. Environ. Health Rep. 2016, 3, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Kabisch, N.; van den Bosch, M.; Lafortezza, R. The health benefits of nature-based solutions to urbanization challenges for children and the elderly–A systematic review. Environ. Res. 2017, 159, 362–373. [Google Scholar] [CrossRef] [PubMed]
- Di Nardo, F.; Saulle, R.; La Torre, G. Green areas and health outcomes: A systematic review of the scientific literature. Ital. J. Public Health 2010, 7, 402–413. [Google Scholar]
- Caruana, E.J.; Roman, M.; Hernández-Sánchez, J.; Solli, P. Longitudinal studies. J. Thoracic Dis. 2015, 7, E537. [Google Scholar]
- Public Health England. Local Action on Health Inequalities: Improving Access to Green Spaces; Health Equity Briefing 8: Sep. 2014; Public Health England: London, UK, 2014. [Google Scholar]
- Pearson-Stuttard, J.; Ezzati, M.; Gregg, E.W. Multimorbidity—a defining challenge for health systems. Lancet Public Health 2019, 4, e599–e600. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols [PRISMA-P] 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute for Health and Care Excellence. Getting Help and Support for Common Mental Health Problems; National Institute for Health and Care Excellence: London, UK, 2011. [Google Scholar]
- National Institute for Health and Care Excellence. NICEimpact Mental Health; National Institute for Health and Care Excellence: London, UK, 2018. [Google Scholar]
- Center for Disease Control and Prevention. 2021. Available online: https://www.cdc.gov/globalhealth/healthprotection/ncd/index.html (accessed on 23 May 2021).
- Kellermeyer, L.; Harnke, B.; Knight, S. Covidence and rayyan. J. Med Libr. Assoc. JMLA 2018, 106, 580. [Google Scholar] [CrossRef] [Green Version]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Bero, L.; Rennie, D. The Cochrane Collaboration: Preparing, maintaining, and disseminating systematic reviews of the effects of health care. JAMA 1995, 274, 1935–1938. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Peterson, J.; Welch, V.; Losos, M.; Tugwell, P.J. The Newcastle-Ottawa Scale [NOS] for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2011. [Google Scholar]
- Lo, C.K.; Mertz, D.; Loeb, M. Newcastle-Ottawa Scale: Comparing reviewers’ to authors’ assessments. BMC Med. Res. Methodol. 2014, 14, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banay, R.F.; James, P.; Hart, J.E.; Kubzansky, L.D.; Spiegelman, D.; Okereke, O.I.; Spengler, J.D.; Laden, F. Greenness and depression incidence among older women. Environ. Health Perspect. 2019, 127, 027001. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Niño, J.A.; Bonilla-Tinoco, L.J.; Manrique-Espinoza, B.S.; Salinas-Rodríguez, A.; Santos-Luna, R.; Román-Pérez, S.; Morales-Carmona, E.; Duncan, D.T. Neighborhood features and depression in Mexican older adults: A longitudinal analysis based on the study on global AGEing and adult health [SAGE], waves 1 and 2 [2009–2014]. PLoS ONE 2019, 14, e0219540. [Google Scholar] [CrossRef] [Green Version]
- Gariepy, G.; Thombs, B.D.; Kestens, Y.; Kaufman, J.S.; Blair, A.; Schmitz, N. The neighbourhood built environment and trajectories of depression symptom episodes in adults: A latent class growth analysis. PLoS ONE 2015, 10, e0133603. [Google Scholar] [CrossRef] [PubMed]
- Gariepy, G.; Kaufman, J.S.; Blair, A.; Kestens, Y.; Schmitz, N. Place and health in diabetes: The neighbourhood environment and risk of depression in adults with Type 2 diabetes. Diabet. Med. 2015, 32, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Melis, G.; Gelormino, E.; Marra, G.; Ferracin, E.; Costa, G. The effects of the urban built environment on mental health: A cohort study in a large northern Italian city. Int. J. Environ. Res. Public Health 2015, 12, 14898–14915. [Google Scholar] [CrossRef]
- Picavet, H.S.; Milder, I.; Kruize, H.; de Vries, S.; Hermans, T.; Wendel-Vos, W. Greener living environment healthier people?: Exploring green space, physical activity and health in the Doetinchem Cohort Study. Prev. Med. 2016, 89, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Tomita, A.; Vandormael, A.M.; Cuadros, D.; Di Minin, E.; Heikinheimo, V.; Tanser, F.; Slotow, R.; Burns, J.K. Green environment and incident depression in South Africa: A geospatial analysis and mental health implications in a resource-limited setting. Lancet Planet. Health 2017, 1, e152–e162. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X. Association of urban green space with mental health and general health among adults in Australia. JAMA Netw. Open 2019, 2, e198209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pun, V.C.; Manjourides, J.; Suh, H.H. Association of neighborhood greenness with self-perceived stress, depression and anxiety symptoms in older US adults. Environ. Health 2018, 17, 1. [Google Scholar] [CrossRef] [Green Version]
- Chang, H.T.; Wu, C.D.; Pan, W.C.; Lung, S.C.; Su, H.J. Association between surrounding greenness and schizophrenia: A taiwanese cohort study. Int. J. Environ. Res. Public Health 2019, 16, 1415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalton, A.M.; Jones, A.P. Residential neighbourhood greenspace is associated with reduced risk of cardiovascular disease: A prospective cohort study. PLoS ONE 2020, 15, e0226524. [Google Scholar] [CrossRef] [Green Version]
- Tamosiunas, A.; Grazuleviciene, R.; Luksiene, D.; Dedele, A.; Reklaitiene, R.; Baceviciene, M.; Vencloviene, J.; Bernotiene, G.; Radisauskas, R.; Malinauskiene, V.; et al. Accessibility and use of urban green spaces, and cardiovascular health: Findings from a Kaunas cohort study. Environ. Health 2014, 13, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, C.; Sbihi, H.; Tamburic, L.; Brauer, M.; Frank, L.D.; Davies, H.W. Association of long-term exposure to transportation noise and traffic-related air pollution with the incidence of diabetes: A prospective cohort study. Environ. Health Perspect. 2017, 125, 087025. [Google Scholar] [CrossRef] [Green Version]
- Renzi, M.; Cerza, F.; Gariazzo, C.; Agabiti, N.; Cascini, S.; Di Domenicantonio, R.; Davoli, M.; Forastiere, F.; Cesaroni, G. Air pollution and occurrence of type 2 diabetes in a large cohort study. Environ. Int. 2018, 112, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Dalton, A.M.; Jones, A.P.; Sharp, S.J.; Cooper, A.J.; Griffin, S.; Wareham, N.J. Residential neighbourhood greenspace is associated with reduced risk of incident diabetes in older people: A prospective cohort study. BMC Public Health 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Liao, J.; Chen, X.; Xu, S.; Li, Y.; Zhang, B.; Cao, Z.; Zhang, Y.; Liang, S.; Hu, K.; Xia, W. Effect of residential exposure to green space on maternal blood glucose levels, impaired glucose tolerance, and gestational diabetes mellitus. Environ. Res. 2019, 176, 108526. [Google Scholar] [CrossRef] [PubMed]
- Hobbs, M.; Griffiths, C.; Green, M.A.; Christensen, A.; McKenna, J. Examining longitudinal associations between the recreational physical activity environment, change in body mass index, and obesity by age in 8864 Yorkshire Health Study participants. Soc. Sci. Med. 2019, 227, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Persson, Å.; Pyko, A.; Lind, T.; Bellander, T.; Östenson, C.G.; Pershagen, G.; Eriksson, C.; Lõhmus, M. Urban residential greenness and adiposity: A cohort study in Stockholm County. Environ. Int. 2018, 121, 832–841. [Google Scholar] [CrossRef] [PubMed]
- Halonen, J.I.; Kivimäki, M.; Pentti, J.; Stenholm, S.; Kawachi, I.; Subramanian, S.V.; Vahtera, J. Green and blue areas as predictors of overweight and obesity in an 8-year follow-up study. Obesity 2014, 22, 1910–1917. [Google Scholar] [CrossRef]
- Lee, J.J.; Hwang, S.J.; Mutalik, K.; Corey, D.; Joyce, R.; Block, J.P.; Fox, C.S.; Powell-Wiley, T.M. Association of built environment characteristics with adiposity and glycaemic measures. Obes. Sci. Pract. 2017, 3, 333–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Astell-Burt, T.; Feng, X. Urban green space, tree canopy and prevention of cardiometabolic diseases: A multilevel longitudinal study of 46 786 Australians. Int. J. Epidemiol. 2020, 49, 926–933. [Google Scholar] [CrossRef] [Green Version]
- Paquet, C.; Coffee, N.T.; Haren, M.T.; Howard, N.J.; Adams, R.J.; Taylor, A.W.; Daniel, M. Food environment, walkability, and public open spaces are associated with incident development of cardio-metabolic risk factors in a biomedical cohort. Health Place 2014, 28, 173–176. [Google Scholar] [CrossRef]
- de Keijzer, C.; Basagana, X.; Tonne, C.; Valentin, A.; Alonso, J.; Antó, J.M.; Nieuwenhuijsen, M.J.; Kivimäki, M.; Singh-Manoux, A.; Sunyer, J.; et al. Long-term exposure to greenspace and metabolic syndrome: A Whitehall II study. Environ. Pollut. 2019, 255, 113231. [Google Scholar] [CrossRef]
- Datzmann, T.; Markevych, I.; Trautmann, F.; Heinrich, J.; Schmitt, J.; Tesch, F. Outdoor air pollution, green space, and cancer incidence in Saxony: A semi-individual cohort study. BMC Public Health 2018, 18, 1–10. [Google Scholar] [CrossRef]
- Conroy, S.M.; Clarke, C.A.; Yang, J.; Shariff-Marco, S.; Shvetsov, Y.B.; Park, S.Y.; Albright, C.L.; Hertz, A.; Monroe, K.R.; Kolonel, L.N.; et al. Contextual Impact of Neighborhood Obesogenic Factors on Postmenopausal Breast Cancer: The Multiethnic Cohort. Cancer Epidemiol. Biomark. Prev. 2017, 26, 480–489. [Google Scholar] [CrossRef] [Green Version]
- Haraldsdottir, A.; Steingrimsdottir, L.; Valdimarsdottir, U.A.; Aspelund, T.; Tryggvadottir, L.; Harris, T.B.; Launer, L.J.; Mucci, L.A.; Giovannucci, E.L.; Adami, H.O.; et al. Early life residence, fish consumption, and risk of breast cancer. Cancer Epidemiol. Prev. Biomark. 2017, 26, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Orioli, R.; Antonucci, C.; Scortichini, M.; Cerza, F.; Marando, F.; Ancona, C.; Manes, F.; Davoli, M.; Michelozzi, P.; Forastiere, F.; et al. Exposure to residential greenness as a predictor of cause-specific mortality and stroke incidence in the Rome longitudinal study. Environ. Health Perspect. 2019, 127, 027002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, L.A.; Hystad, P.; Burnett, R.T.; Kwong, J.C.; Crouse, D.L.; van Donkelaar, A.; Tu, K.; Lavigne, E.; Copes, R.; Martin, R.V.; et al. Urban green space and the risks of dementia and stroke. Environ. Res. 2020, 186, 109520. [Google Scholar] [CrossRef]
- Yuchi, W.; Sbihi, H.; Davies, H.; Tamburic, L.; Brauer, M. Road proximity, air pollution, noise, green space and neurologic disease incidence: A population-based cohort study. Environ. Health 2020, 19, 8. [Google Scholar] [CrossRef] [Green Version]
- de Keijzer, C.; Tonne, C.; Sabia, S.; Basagaña, X.; Valentín, A.; Singh-Manoux, A.; Antó, J.M.; Alonso, J.; Nieuwenhuijsen, M.J.; Sunyer, J.; et al. Green and blue spaces and physical functioning in older adults: Longitudinal analyses of the Whitehall II study. Environ. Int. 2019, 122, 346–356. [Google Scholar] [CrossRef]
- Yu, R.; Wang, D.; Leung, J.; Lau, K.; Kwok, T.; Woo, J. Is neighborhood green space associated with less frailty? Evidence from the Mr. and Ms. Os [Hong Kong] study. J. Am. Med. Dir. Assoc. 2018, 19, 528–534. [Google Scholar] [CrossRef]
- Zhu, A.; Yan, L.; Wu, C.; Ji, J.S. Residential greenness and frailty among older adults: A longitudinal cohort in China. J. Am. Med. Dir. Assoc. 2020, 21, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.; Mazumdar, S.; Ding, D.; Morgan, G.; Comino, E.J.; Bauman, A.; Jalaludin, B. Neighbourhood greenspace and physical activity and sedentary behaviour among older adults with a recent diagnosis of type 2 diabetes: A prospective analysis. BMJ Open 2019, 9, e028947. [Google Scholar] [CrossRef]
- Cleland, V.J.; Timperio, A.; Crawford, D. Are perceptions of the physical and social environment associated with mothers' walking for leisure and for transport? A longitudinal study. Prev. Med. 2008, 47, 188–193. [Google Scholar] [CrossRef]
- Coogan, P.F.; White, L.F.; Adler, T.J.; Hathaway, K.M.; Palmer, J.R.; Rosenberg, L. Prospective study of urban form and physical activity in the Black Women's Health Study. Am. J. Epidemiol. 2009, 170, 1105–1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalton, A.M.; Wareham, N.; Griffin, S.; Jones, A.P. Neighbourhood greenspace is associated with a slower decline in physical activity in older adults: A prospective cohort study. SSM-Popul. Health 2016, 2, 683–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faerstein, E.; da Silveira, I.H.; Boclin, K.D.; Curioni, C.C.; de Castro, I.R.; Junger, W.L. Associations of neighborhood socioeconomic, natural and built environmental characteristics with a 13-year trajectory of non-work physical activity among civil servants in Rio de Janeiro, Brazil: The Pro-Saude Study. Health Place 2018, 53, 110–116. [Google Scholar] [CrossRef]
- Hogendorf, M.; Groeniger, J.O.; Noordzij, J.M.; Beenackers, M.A.; van Lenthe, F.J. Longitudinal effects of urban green space on walking and cycling: A fixed effects analysis. Health Place 2020, 61, 102264. [Google Scholar] [CrossRef]
- Josey, M.J.; Moore, S. The influence of social networks and the built environment on physical inactivity: A longitudinal study of urban-dwelling adults. Health Place 2018, 54, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.S.; Chan, F.Y.; Leung, J.; Yu, B.; Lu, Z.H.; Woo, J.; Kwok, T.; Lau, K.K. Longitudinal Association of Built Environment Pattern with Physical Activity in a Community-Based Cohort of Elderly Hong Kong Chinese: A Latent Profile Analysis. Int. J. Environ. Res. Public Health 2020, 17, 4275. [Google Scholar] [CrossRef] [PubMed]
- Michael, Y.L.; Perdue, L.A.; Orwoll, E.S.; Stefanick, M.L.; Marshall, L.M. Osteoporotic Fractures in Men Study Group. Physical activity resources and changes in walking in a cohort of older men. Am. J. Public Health 2010, 100, 654–660. [Google Scholar] [CrossRef]
- Sugiyama, T.; Shibata, A.; Koohsari, M.J.; Tanamas, S.K.; Oka, K.; Salmon, J.; Dunstan, D.W.; Owen, N. Neighborhood environmental attributes and adults' maintenance of regular walking. Med. Sci. Sports Exerc. 2015, 47, 1204–1210. [Google Scholar] [CrossRef] [Green Version]
- Yang, L.; Griffin, S.; Khaw, K.T.; Wareham, N.; Panter, J. Longitudinal associations between built environment characteristics and changes in active commuting. BMC Public Health 2017, 17, 1–8. [Google Scholar]
- Meyer, K.A.; Boone-Heinonen, J.; Duffey, K.J.; Rodriguez, D.A.; Kiefe, C.I.; Lewis, C.E.; Gordon-Larsen, P. Combined measure of neighborhood food and physical activity environments and weight-related outcomes: The CARDIA study. Health Place 2015, 33, 9–18. [Google Scholar] [CrossRef] [Green Version]
- De la Fuente, F.; Saldías, M.A.; Cubillos, C.; Mery, G.; Carvajal, D.; Bowen, M.; Bertoglia, M.P. Green Space Exposure Association with Type 2 Diabetes Mellitus, Physical Activity, and Obesity: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 97. [Google Scholar] [CrossRef] [PubMed]
- Lachowycz, K.; Jones, A.P. Greenspace and obesity: A systematic review of the evidence. Obes. Rev. 2011, 12, e183–e189. [Google Scholar] [CrossRef] [PubMed]
- Müller, G.; Harhoff, R.; Rahe, C.; Berger, K. Inner-city green space and its association with body mass index and prevalent type 2 diabetes: A cross-sectional study in an urban German city. BMJ Open 2018, 8, e019062. [Google Scholar] [CrossRef] [Green Version]
- Feng, J.; Glass, T.A.; Curriero, F.C.; Stewart, W.F.; Schwartz, B.S. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place 2010, 16, 175–190. [Google Scholar] [CrossRef]
- Zhou, Y.; von Lengerke, T.; Dreier, M. Comparing different data sources by examining the associations between surrounding greenspace and children's weight status. Int. J. Health Geogr. 2021, 20, 1–3. [Google Scholar] [CrossRef]
- Xiao, Y.; Zhang, Y.; Sun, Y.; Tao, P.; Kuang, X. Does green space really matter for residents' obesity? A new perspective from Baidu Street View. Front. Public Health 2020, 8, 332. [Google Scholar] [CrossRef] [PubMed]
- Darkwah, R.M.; Cobbinah, P.B. Stewardship of urban greenery in an era of global urbanisation. Int. J. Environ. Ecol. Geol. Geophys. Eng. 2014, 8, 671–674. [Google Scholar]
- Jones, N.L.; Gilman, S.E.; Cheng, T.L.; Drury, S.S.; Hill, C.V.; Geronimus, A.T. Life course approaches to the causes of health disparities. Am. J. Public Health 2019, 109, S48–S55. [Google Scholar] [CrossRef] [PubMed]
- Zeanah, C.H.; Gunnar, M.R.; McCall, R.B.; Kreppner, J.M.; Fox, N.A., VI. Sensitive periods. Monogr. Soc. Res. Child Dev. 2011, 76, 147–162. [Google Scholar] [CrossRef] [Green Version]
- Pearce, J.; Shortt, N.; Rind, E.; Mitchell, R. Life course, green space and health: Incorporating place into life course epidemiology. Int. J. Environ. Res. Public Health 2016, 13, 331. [Google Scholar] [CrossRef]
- Engemann, K.; Pedersen, C.B.; Arge, L.; Tsirogiannis, C.; Mortensen, P.B.; Svenning, J.C. Childhood exposure to green space–a novel risk-decreasing mechanism for schizophrenia? Schizophr. Res. 2018, 199, 142–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newbury, J.B.; Arseneault, L.; Beevers, S.; Kitwiroon, N.; Roberts, S.; Pariante, C.M.; Kelly, F.J.; Fisher, H.L. Association of air pollution exposure with psychotic experiences during adolescence. JAMA Psychiatry 2019, 76, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Ahern, J.; Rudenstine, S.; Wallace, Z.; Vlahov, D. Urban built environment and depression: A multilevel analysis. J. Epidemiol. Community Health 2005, 59, 822–827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saarloos, D.; Alfonso, H.; Giles-Corti, B.; Middleton, N.; Almeida, O.P. The built environment and depression in later life: The health in men study. Am. J. Geriatr. Psychiatry 2011, 19, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Prince, S.A.; Kristjansson, E.A.; Russell, K.; Billette, J.M.; Sawada, M.; Ali, A.; Tremblay, M.S.; Prud’Homme, D. A multilevel analysis of neighbourhood built and social environments and adult self-reported physical activity and body mass index in Ottawa, Canada. Int. J. Environ. Res. Public Health 2011, 8, 3953–3978. [Google Scholar] [CrossRef] [PubMed]
- de Keijzer, C.; Bauwelinck, M.; Dadvand, P. Long-term exposure to residential greenspace and healthy ageing: A systematic review. Curr. Environ. Health Rep. 2020, 7, 65–88. [Google Scholar] [CrossRef] [PubMed]
- Vanaken, G.J.; Danckaerts, M. Impact of green space exposure on children’s and adolescents’ mental health: A systematic review. Int. J. Environ. Res. Public Health 2018, 15, 2668. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. Urban Green Spaces and Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Kaczynski, A.T.; Potwarka, L.R.; Saelens, B.E. Association of park size, distance, and features with physical activity in neighborhood parks. Am. J. Public Health 2008, 98, 1451–1456. [Google Scholar] [CrossRef] [PubMed]
- Grilli, G.; Mohan, G.; Curtis, J. Public park attributes, park visits, and associated health status. Landsc. Urban Plan. 2020, 199, 103814. [Google Scholar] [CrossRef]
- Costigan, S.A.; Veitch, J.; Crawford, D.; Carver, A.; Timperio, A. A cross-sectional investigation of the importance of park features for promoting regular physical activity in parks. Int. J. Environ. Res. Public Health 2017, 14, 1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreira, T.C.; Polizel, J.L.; Santos, I.D.; Silva Filho, D.F.; Bensenor, I.; Lotufo, P.A.; Mauad, T. Green spaces, land cover, street trees and hypertension in the megacity of São Paulo. Int. J. Environ. Res. Public Health 2020, 17, 725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Tan, P.Y. Associations between urban green spaces and health are dependent on the analytical scale and how urban green spaces are measured. Int. J. Environ. Res. Public Health 2019, 16, 578. [Google Scholar] [CrossRef] [Green Version]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ioannidis, J.P.; Lau, J. Pooling research results: Benefits and limitations of meta-analysis. Jt. Comm. J. Qual. Improv. 1999, 25, 462–469. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leslie, E.; Sugiyama, T.; Ierodiaconou, D.; Kremer, P. Perceived and objectively measured greenness of neighbourhoods: Are they measuring the same thing? Landsc. Urban Plan. 2010, 95, 28–33. [Google Scholar] [CrossRef]
- Kabisch, N.; Strohbach, M.; Haase, D.; Kronenberg, J. Urban green space availability in European cities. Ecol. Indic. 2016, 70, 586–596. [Google Scholar] [CrossRef]
- Lovell, R. Links between Natural Environments and Physical Activity: Evidence Briefing; Natural England: Exeter, UK, 2016. [Google Scholar]
- Grellier, J.; White, M.P.; Albin, M.; Bell, S.; Elliott, L.R.; Gascón, M.; Gualdi, S.; Mancini, L.; Nieuwenhuijsen, M.J.; Sarigiannis, D.A.; et al. BlueHealth: A study programme protocol for mapping and quantifying the potential benefits to public health and well-being from Europe’s blue spaces. BMJ Open 2017, 7, e016188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elliott, L.R.; White, M.P.; Grellier, J.; Rees, S.E.; Waters, R.D.; Fleming, L.E. Recreational visits to marine and coastal environments in England: Where, what, who, why, and when? Mar. Policy 2018, 97, 305–314. [Google Scholar] [CrossRef] [Green Version]
- Head, A.; Fleming, K.; Kypridemos, C.; Pearson-Stuttard, J.; O’Flaherty, M. Multimorbidity: The case for prevention. J. Epidemiol. Community Health 2021, 75, 242–244. [Google Scholar] [CrossRef] [PubMed]
- Pati, S.; Swain, S.; Knottnerus, J.A.; Metsemakers, J.F.; van den Akker, M. Health related quality of life in multimorbidity: A primary-care based study from Odisha, India. Health Qual. Life Outcomes 2019, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lenzi, J.; Avaldi, V.M.; Rucci, P.; Pieri, G.; Fantini, M.P. Burden of multimorbidity in relation to age, gender and immigrant status: A cross-sectional study based on administrative data. BMJ Open 2016, 6, e012812. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).