COVID-19 Stressors on Migrant Workers in Vietnam: Cumulative Risk Consideration
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Setting
2.3. Sample Size and Sampling
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Approval
3. Results
3.1. The Individual
3.2. Workplace
3.3. The Environment
3.4. The Community
4. Discussion
4.1. The Individual
4.2. Workplace
4.3. The Environment
4.4. The Community
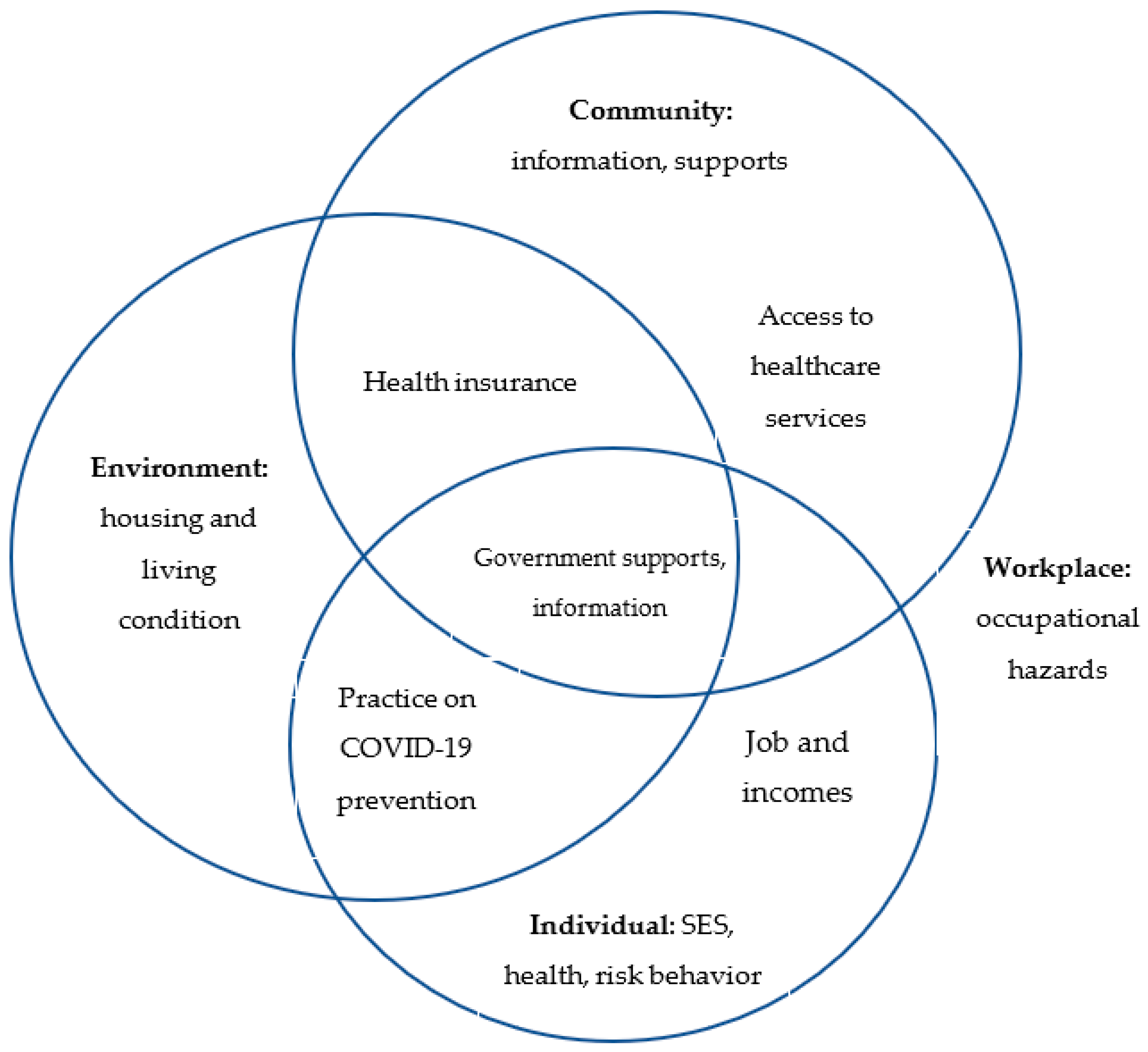
4.5. Framework
4.6. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Douglas, M.; Katikireddi, S.V.; Taulbut, M.; McKee, M.; McCartney, G. Mitigating the wider health effects of covid-19 pandemic response. BMJ 2020, 369, m1557. [Google Scholar] [CrossRef]
- Wilkinson, A. Local response in health emergencies: Key considerations for addressing the COVID-19 pandemic in informal urban settlements. Environ. Urban. 2020, 32, 503–522. [Google Scholar] [CrossRef]
- International Organization for Migration. World Migration Report 2020; International Organization for Migration: Grand-Saconnex, Switzerland, 2020. [Google Scholar]
- Bhopal, R. Covid-19: Undocumented migrants are probably at greatest risk. BMJ 2020, 369, m1673. [Google Scholar] [CrossRef]
- WHO. Risk Communication and Community Engagement (RCCE) Considerations: Ebola Response in the Democratic Republic of the Congo; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- International Labour Organization (ILO). ILO Global Estimates on Migrant Workers: Results and Methodology, 2nd ed.; International Labour Office: Geneva, Switzerland, 2018. [Google Scholar]
- Kluge, H.H.P.; Jakab, Z.; Bartovic, J.; D’Anna, V.; Severoni, S. Refugee and migrant health in the COVID-19 response. Lancet 2020, 395, 1237–1238. [Google Scholar] [CrossRef]
- World Health Organization. WHO Community Engagement Framework for Quality, People-Centred and Resilient Health Services; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- WHO. WPRO, Interim Guidance. Role of Community Engagement in Situations of Extensive Community Transmission of COVID-19; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Corburn, J.; Vlahov, D.; Mberu, B.; Riley, L.; Caiaffa, W.T.; Rashid, S.F.; Ko, A.; Patel, S.; Jukur, S.; Martínez-Herrera, E. Slum Health: Arresting COVID-19 and Improving Well-Being in Urban Informal Settlements. J. Urban Health 2020, 97, 348–357. [Google Scholar] [CrossRef] [Green Version]
- Ha, B.T.T.; La Quang, N.; Mirzoev, T.; Tai, N.T.; Thai, P.Q.; Dinh, P.C. Combating the COVID-19 Epidemic: Experiences from Vietnam. International. J. Environ. Res. Public Health 2020, 17, 3125. [Google Scholar] [CrossRef] [PubMed]
- Vu, L.T.H.; Nguyen, N.T.K.; Tran, H.T.D.; Muhajarine, N. mHealth information for migrants: An e-health intervention for internal migrants in Vietnam. Reprod. Health 2016, 13, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anh, L.T.K.; Vu, L.H.; Bonfoh, B.; Schelling, E. An analysis of interprovincial migration in Vietnam from 1989 to 2009. Glob. Health Action 2012, 5, 1–12. [Google Scholar] [PubMed] [Green Version]
- Long, G.T. Social Protection for Migrants in Vietnam: Practice and Policy Issues; UNESCAP Vietnam: Hanoi, Vietnam, 2013. [Google Scholar]
- General Statistics Office and UNFPA. The 2015 National Internal Migration Survey: Major Findings; Vietnam News Agency Publishing House: Hanoi, Vietnam, 2016.
- Van Kham, T.; Van Quyet, P. Access to social services: How poor migrants experience their life in contemporary Vietnamese urban areas. J. Soc. Sci. Humanit. 2015, 3, 277–290. [Google Scholar]
- Pham, L.T.L.; Vu, L.H.; Schelling, E. Health services for reproductive tract infections among female migrant workers in industrial zones in Ha Noi, Vietnam: An in-depth assessment. Reprod. Health 2012, 9, 1–11. [Google Scholar]
- Tran, B.X.; Vo, T.; Dang, A.K.; Nguyen, Q.N.; Vu, G.T.; Vu, L.G.; Do, K.N.; Latkin, C.A.; Ho, C.S.; Ho, R. Characterizing Unsafe Sexual Behavior among Factory Workers in the Context of Rapid Industrialization in Northern Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 5085. [Google Scholar] [CrossRef] [Green Version]
- Tran, B.X.; Vu, G.T.; Latkin, C.A.; Pham, H.Q.; Phan, H.T.; Le, H.T.; Ho, R.C. Characterize health and economic vulnerabilities of workers to control the emergence of COVID-19 in an industrial zone in Vietnam. Saf. Sci. 2020, 129, 104811. [Google Scholar] [CrossRef]
- Thanh, N.T.; LeBailly, P.; Dien, N.T. Migrant Workers for the Development of Industrial Zones in Bac Ninh Province, Vietnam. Asian Soc. Sci. 2018, 14, 115–123. [Google Scholar] [CrossRef]
- Vietnam Ministry of Health. COVID-19 Timeline [Dòng thời gian COVID-19]. 2021. Available online: https://ncov.moh.gov.vn/dong-thoi-gian (accessed on 13 April 2021).
- Fox, M.A.; Spicer, K.; Chosewood, L.C.; Susi, P.; Johns, D.O.; Dotson, G.S. Implications of applying cumulative risk assessment to the workplace. Environ. Int. 2018, 115, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Alahmad, B.; Kurdi, H.; Colonna, K.; Gasana, J.; Agnew, J.; A Fox, M. COVID-19 stressors on migrant workers in Kuwait: Cumulative risk considerations. BMJ Glob. Health 2020, 5, e002995. [Google Scholar] [CrossRef] [PubMed]
- UNFPA. Ethnic groups in Vietnam: An analysis of key indicators from the 2009 Vietnam Population and Housing Census; UNFPA Vietnam: Hanoi, Vietnam, 2020. [Google Scholar]
- Vietnam Ministry of Health. Information Website about the Pandemic of COVID-19. 2020. Available online: https://ncov.moh.gov.vn/ (accessed on 5 June 2020).
- Watson, M.F.; Bacigalupe, G.; Daneshpour, M.; Han, W.; Parra-Cardona, R. COVID-19 Interconnectedness: Health Inequity, the Climate Crisis, and Collective Trauma. Fam. Process. 2020, 59, 832–846. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Huong, L.T.; Hinh, N.D.; Nguyen, L.H.; Le, B.N.; Nong, V.M.; Thuc, V.T.M.; Tho, T.D.; Latkin, C.; Zhang, M.W.; et al. A study on the influence of internet addiction and online interpersonal influences on health-related quality of life in young Vietnamese. BMC Public Health 2017, 17, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.; Hu, Z.; Alias, H.; Wong, L.P. Knowledge, Attitudes, Impact, and Anxiety Regarding COVID-19 Infection Among the Public in China. Front. Public Health 2020, 8, 236. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.T.; Rahman, Z.; Emerson, M.R.; Nguyen, M.H.; Zabin, L.S. Cigarette Smoking and Drinking Behavior of Migrant Adolescents and Young Adults in Hanoi, Vietnam. J. Adolesc. Health 2012, 50, S61–S67. [Google Scholar] [CrossRef] [Green Version]
- Tran, B.X.; Vu, G.T.; Pham, K.T.H.; Vuong, Q.-H.; Ho, M.-T.; Vuong, T.-T.; Nguyen, H.-K.T.; Nguyen, C.T.; Latkin, C.A.; Ho, C.S.; et al. Depressive Symptoms among Industrial Workers in Vietnam and Correlated Factors: A Multi-Site Survey. Int. J. Environ. Res. Public Health 2019, 16, 1642. [Google Scholar] [CrossRef] [Green Version]
- International Organization for Migration. Vietnam. 2020. Available online: https://www.iom.int/countries/viet-nam (accessed on 11 December 2020).
- International Labour Organization (ILO). COVID-19 in Vietnam: The Unprecedented Dual Crisis. 2020. Available online: https://www.ilo.org/hanoi/Informationresources/Publicinformation/comments-and-analysis/WCMS_741641/lang--en/index.htm (accessed on 28 April 2020).
- International Labor Organization. Global Wage Report 2020–2021: Wages and Minimum Wages in the Time of COVID-19; International Labor Office: Geneva, Switzerland, 2020. [Google Scholar]
- Dang, H.-A.; Giang, L.T. Turning Vietnam’s COVID-19 Success into Economic Recovery: A Job-Focused Analysis of Individual Assessments on Their Finance and the Economy; IZA DP No13315. 2020; IZA Institute of Labor Economics: Bonn, Germany, 2020. [Google Scholar]
- Institute for Policy and Strategies for Agriculture and Rural Development. Rapid Assessment on the Impacts of COVID-19 on Rural Livelihoods in Vietnam; UNICEF Vietnam: Hanoi, Vietnam, 2020.
- UNICEF. Rapid Assessment on the Routine Services of Health, Nutrition and WASH at Commune Level; UNICEF Vietnam: Hanoi, Vietnam, 2020. [Google Scholar]
- UNICEF. Rapid Assessment of Social and Economic Impacts of COVID-19 on Children and Families in Vietnam; UNICEF Vietnam: Hanoi, Vietnam, 2020.
- UNICEF. The Impact of COVID-19 on Migrants and their Families; UNICEF: New York, NY, USA, 2020.
- International Labor Organization. COVID-19 and the Labour Market in Vietnam; ILO Country Offfice for Vietnam: Hanoi, Vietnam, 2020. [Google Scholar]
- Greenaway, C.; Hargreaves, S.; Barkati, S.; Coyle, C.M.; Gobbi, F.; Veizis, A.; Douglas, P. COVID-19: Exposing and addressing health disparities among ethnic minorities and migrants. J. Travel Med. 2020, 27. [Google Scholar] [CrossRef] [PubMed]
- Do, T.T.T.; Le, M.D.; Van Nguyen, T.; Tran, B.X.; Le, H.T.; Nguyen, H.D.; Nguyen, L.H.; Nguyen, C.T.; Tran, T.D.; Latkin, C.A.; et al. Receptiveness and preferences of health- related smartphone applications among Vietnamese youth and young adults. BMC Public Health 2018, 18, 764. [Google Scholar] [CrossRef] [PubMed]
- Van Nhu, H.; Tuyet-Hanh, T.T.; Van, N.T.A.; Linh, T.N.Q.; Tien, T.Q. Knowledge, Attitudes, and Practices of the Vietnamese as Key Factors in Controlling COVID-19. J. Community Health 2020, 45, 1263–1269. [Google Scholar] [CrossRef] [PubMed]
- Government of Vietnam, Decree 15/2020/NĐ-CP: Administrative Sanction in Areas of Telecommunication, Information Technology and e-Communication 2020. Available online: https://www.mard.gov.vn/Pages/nghi-dinh-so-15-2020-nd-cp-ngay-3-2-2020-cua-chinh-phu-ve-viec-quy-dinh-xu-phat-vi-pham-hanh-chinh-trong--.aspx (accessed on 5 June 2021).
| Variable | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Sex | 0.015 | |||
| Males | 64 (29.2%) | 91 (40.3%) | 155 (34.8%) | |
| Females | 155 (70.8%) | 135 (59.7%) | 290 (65.2%) | |
| Age groups | 0.20 | |||
| 18–24 | 62 (28.3%) | 78 (34.5%) | 140 (31.5%) | |
| 25–29 | 76 (34.7%) | 81 (35.8%) | 157 (35.3%) | |
| 30–34 | 57 (26.0%) | 41 (18.1%) | 98 (22.0%) | |
| 35–40 | 17 (7.8%) | 22 (9.7%) | 39 (8.8%) | |
| 41–50 | 7 (3.2%) | 4 (1.8%) | 11 (2.5%) | |
| Education levels | <0.001 | |||
| Secondary-school | 25 (11.4%) | 19 (8.4%) | 44 (9.9%) | |
| High-school | 139 (63.5%) | 84 (37.2%) | 223 (50.1%) | |
| Vocational | 2 (0.9%) | 15 (6.6%) | 17 (3.8%) | |
| College | 24 (11.0%) | 43 (19.0%) | 67 (15.1%) | |
| University and higher | 29 (13.2%) | 65 (28.8%) | 94 (21.1%) | |
| Religion | 0.25 | |||
| Buddhism | 18 (8.2%) | 10 (4.4%) | 28 (6.3%) | |
| Catholicism | 9 (4.1%) | 5 (2.2%) | 14 (3.1%) | |
| Christianity | 3 (1.4%) | 1 (0.4%) | 4 (0.9%) | |
| Non-religious | 188 (85.8%) | 209 (92.5%) | 397 (89.2%) | |
| Other | 1 (0.5%) | 1 (0.4%) | 2 (0.4%) | |
| Ethnicity | <0.001 | |||
| Dao | 0 (0.0%) | 9 (4.0%) | 9 (2.0%) | |
| Kinh | 195 (89.0%) | 139 (61.5%) | 334 (75.1%) | |
| Muong | 22 (10.0%) | 14 (6.2%) | 36 (8.1%) | |
| Nung | 0 (0.0%) | 19 (8.4%) | 19 (4.3%) | |
| Other | 1 (0.5%) | 12 (5.3%) | 13 (2.9%) | |
| Tay | 1 (0.5%) | 33 (14.6%) | 34 (7.6%) | |
| Marital status | <0.001 | |||
| Divorced | 5 (2.3%) | 5 (2.2%) | 10 (2.2%) | |
| Married | 143 (65.3%) | 106 (46.9%) | 249 (56.0%) | |
| Single | 71 (32.4%) | 115 (50.9%) | 186 (41.8%) | |
| Employment contract | 0.015 | |||
| No | 0 (0.0%) | 2 (0.9%) | 2 (0.4%) | |
| Yes | 219 (100.0%) | 224 (99.1%) | 443 (99.6%) |
| Variable | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Avoid crowded places | 217 (99.1%) | 222 (98.2%) | 0.43 | 439 (98.7%) |
| Frequently wash hands | 214 (97.7%) | 222 (98.2%) | 0.70 | 436 (98.0%) |
| Wear face mask in the public places | 216 (98.6%) | 224 (99.1%) | 0.63 | 440 (98.9%) |
| Avoid contacting people with illness | 210 (95.9%) | 214 (94.7%) | 0.55 | 424 (95.3%) |
| Report to health center when having symptoms (fever, cough) | 206 (94.1%) | 192 (85.0%) | 0.002 | 398 (89.4%) |
| Keep minimum of 2 m when talking | 208 (95.0%) | 211 (93.4%) | 0.47 | 419 (94.2%) |
| Self-report by apps (Bluezone) | 201 (91.8%) | 206 (91.2%) | 0.81 | 407 (91.5%) |
| Correct practice | 192 (87.7%) | 169 (74.8%) | <0.001 | 361 (81.1%) |
| Variable | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Exposure to Occupational Hazard | ||||
| Exposed to high temperature | 4 (1.8%) | 9 (4.0%) | 0.18 | 13 (2.9%) |
| Exposed to dust * | 3 (1.4%) | 19 (8.4%) | <0.001 | 22 (4.9%) |
| Exposed to noise * | 37 (16.9%) | 93 (41.2%) | <0.001 | 130 (29.2%) |
| Exposed to poor light | 3 (1.4%) | 3 (1.3%) | 0.97 | 6 (1.3%) |
| Exposed to humid | 2 (0.9%) | 4 (1.8%) | 0.43 | 6 (1.3%) |
| Exposed to chemical * | 6 (2.7%) | 18 (8.0%) | 0.015 | 24 (5.4%) |
| Health status | 0.30 | |||
| Fair | 47 (21.5%) | 58 (25.7%) | 105 (23.6%) | |
| Good | 172 (78.5%) | 168 (74.3%) | 340 (76.4%) | |
| Having chronic disease | 4 (1.8%) | 6 (2.7%) | 0.56 | 10 (2.2%) |
| Having acute disease | 9 (4.1%) | 15 (6.6%) | 0.24 | 24 (5.4%) |
| Having problem in mobility | 4 (1.8%) | 8 (3.5%) | 0.26 | 12 (2.7%) |
| Having problem in self-care | 4 (1.8%) | 3 (1.3%) | 0.67 | 7 (1.6%) |
| Health risk behaviour | ||||
| Smoking * | 8 (3.7%) | 38 (16.8%) | <0.001 | 46 (10.3%) |
| Drinking * | 23 (10.5%) | 91 (40.3%) | <0.001 | 114 (25.6%) |
| Playing online games * | 33 (15.1%) | 70 (31.0%) | <0.001 | 103 (23.1%) |
| Variables | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Residence area * | <0.001 | |||
| <12 | 23 (10.5%) | 49 (21.7%) | 72 (16.2%) | |
| 12–24 | 50 (22.8%) | 75 (33.2%) | 125 (28.1%) | |
| 25-36 | 98 (44.7%) | 44 (19.5%) | 142 (31.9%) | |
| >36 | 48 (21.9%) | 58 (25.7%) | 106 (23.8%) | |
| Living with family * | 206 (94.1%) | 152 (67.3%) | <0.001 | 358 (80.4%) |
| Living with friends * | 32 (14.6%) | 61 (27.0%) | 0.001 | 93 (20.9%) |
| Having clean water * | 219 (100.0%) | 221 (97.8%) | 0.027 | 440 (98.9%) |
| Having toilets and sanitation * | 219 (100.0%) | 226 (100.0%) | 445 (100.0%) | |
| Access to internet at home * | 215 (98.2%) | 207 (91.6%) | 0.002 | 422 (94.8%) |
| Variables | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Employment status | ||||
| Before COVID-19 * | <0.001 | |||
| Full-time employment | 211 (96.3%) | 190 (84.1%) | 401 (90.1%) | |
| Temporarily layoffs | 2 (0.9%) | 23 (10.2%) | 25 (5.6%) | |
| Unemployment | 6 (2.7%) | 13 (5.8%) | 19 (4.3%) | |
| 1 January–23 July | 0.23 | |||
| Full time employment | 196 (89.5%) | 190 (84.1%) | 386 (86.7%) | |
| Temporarily layoffs | 14 (6.4%) | 23 (10.2%) | 37 (8.3%) | |
| Unemployment | 9 (4.1%) | 13 (5.8%) | 22 (4.9%) | |
| 23 July–11 October | 0.11 | |||
| Full time employment | 214 (97.7%) | 215 (95.1%) | 429 (96.4%) | |
| Temporarily layoffs | 1 (0.5%) | 7 (3.1%) | 8 (1.8%) | |
| Unemployment | 4 (1.8%) | 4 (1.8%) | 8 (1.8%) | |
| Income (million VND) (Mean/SD) | ||||
| Before COVID-19 * | 5.7 (1.8) | 7.9 (4.4) | <0.001 | 6.8 (3.6) |
| 1 January–23 July * | 5.3 (1.7) | 7.9 (4.4) | <0.001 | 6.6 (3.6) |
| 23 July–11 October * | 5.6 (1.5) | 8.5 (4.0) | <0.001 | 7.1 (3.3) |
| Economic responsibility | ||||
| Worker only * | 128 (58.4%) | 187 (82.7%) | <0.001 | 315 (70.8%) |
| Family remittances | 158 (72.1%) | 157 (69.5%) | 0.53 | 315 (70.8%) |
| Other duties | 60 (27.4%) | 69 (30.5%) | 0.47 | 129 (29.0%) |
| Variables | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Healthcare facilities | ||||
| Having health insurance | 218 (99.5%) | 225 (99.6%) | 0.98 | 443 (99.6%) |
| Hospital * | 99 (45.2%) | 179 (79.2%) | <0.001 | 278 (62.5%) |
| Healthcare unit in company * | 154 (70.3%) | 112 (49.6%) | <0.001 | 266 (59.8%) |
| Commune health center * | 62 (28.3%) | 121 (53.5%) | <0.001 | 183 (41.1%) |
| Time available | ||||
| All the time * | 203 (92.7%) | 185 (81.9%) | <0.001 | 388 (87.2%) |
| Working time * | 13 (5.9%) | 26 (11.5%) | 0.038 | 39 (8.8%) |
| Variables | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| Updated information on COVID-19 | ||||
| Number of COVID-19 new cases * | 215 (98.2%) | 212 (93.8%) | 0.019 | 427 (96.0%) |
| Number of deaths due to COVID-19 * | 215 (98.2%) | 210 (92.9%) | 0.007 | 425 (95.5%) |
| COVID-19 prevention | 215 (98.2%) | 219 (96.9%) | 0.39 | 434 (97.5%) |
| Source of information on COVID-19 | ||||
| Television * | 210 (95.9%) | 183 (81.0%) | <0.001 | 393 (88.3%) |
| Radio * | 120 (54.8%) | 76 (33.6%) | <0.001 | 196 (44.0%) |
| Internet * | 210 (95.9%) | 198 (87.6%) | 0.002 | 408 (91.7%) |
| Mobile phone message | 206 (94.1%) | 191 (84.5%) | 0.062 | 397 (89.2%) |
| Leaflets * | 47 (21.5%) | 34 (15.0%) | 0.001 | 81 (18.2%) |
| Sources of Supports | Phuc Son- Ninh Binh | Que Vo- Bac Ninh | p | Total |
|---|---|---|---|---|
| n = 219 | n = 226 | n = 445 | ||
| PPE | ||||
| Company * | 95 (43.4%) | 146 (64.6%) | <0.001 | 241 (54.2%) |
| Dormitory landlords * | 11 (5.0%) | 32 (14.2%) | 0.001 | 43 (9.7%) |
| Community agencies | 47 (21.5%) | 64 (28.3%) | 0.095 | 111 (24.9%) |
| Healthcare facilities * | 55 (25.1%) | 79 (35.0%) | 0.024 | 134 (30.1%) |
| Family/Friends | 38 (17.4%) | 46 (20.4%) | 0.42 | 84 (18.9%) |
| Food | ||||
| Company * | 77 (35.2%) | 109 (48.2%) | 0.005 | 186 (41.8%) |
| Dormitory landlords * | 12 (5.5%) | 32 (14.2%) | 0.002 | 44 (9.9%) |
| Community agencies * | 47 (21.5%) | 69 (30.5%) | 0.029 | 116 (26.1%) |
| Healthcare facilities | 43 (19.6%) | 51 (22.6%) | 0.45 | 94 (21.1%) |
| Family/Friends * | 53 (24.2%) | 78 (34.5%) | 0.017 | 131 (29.4%) |
| Subsides for housing | ||||
| Company | 82 (37.4%) | 84 (37.2%) | 0.95 | 166 (37.3%) |
| Dormitory landlords * | 20 (9.1%) | 53 (23.5%) | <0.001 | 73 (16.4%) |
| Community agencies | 38 (17.4%) | 54 (23.9%) | 0.088 | 92 (20.7%) |
| Healthcare facilities | 35 (16.0%) | 38 (16.8%) | 0.81 | 73 (16.4%) |
| Family/Friends | 49 (22.4%) | 63 (27.9%) | 0.18 | 112 (25.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bui, H.T.T.; Duong, D.M.; Pham, T.Q.; Mirzoev, T.; Bui, A.T.M.; La, Q.N. COVID-19 Stressors on Migrant Workers in Vietnam: Cumulative Risk Consideration. Int. J. Environ. Res. Public Health 2021, 18, 8757. https://doi.org/10.3390/ijerph18168757
Bui HTT, Duong DM, Pham TQ, Mirzoev T, Bui ATM, La QN. COVID-19 Stressors on Migrant Workers in Vietnam: Cumulative Risk Consideration. International Journal of Environmental Research and Public Health. 2021; 18(16):8757. https://doi.org/10.3390/ijerph18168757
Chicago/Turabian StyleBui, Ha Thi Thu, Duc Minh Duong, Thanh Quoc Pham, Tolib Mirzoev, Anh Thi My Bui, and Quang Ngoc La. 2021. "COVID-19 Stressors on Migrant Workers in Vietnam: Cumulative Risk Consideration" International Journal of Environmental Research and Public Health 18, no. 16: 8757. https://doi.org/10.3390/ijerph18168757
APA StyleBui, H. T. T., Duong, D. M., Pham, T. Q., Mirzoev, T., Bui, A. T. M., & La, Q. N. (2021). COVID-19 Stressors on Migrant Workers in Vietnam: Cumulative Risk Consideration. International Journal of Environmental Research and Public Health, 18(16), 8757. https://doi.org/10.3390/ijerph18168757






