A Social-Ecological Approach to Identify Facilitators and Barriers of Home Modifications
Abstract
1. Introduction
1.1. Home Modifications and Aging-in-Place
1.2. Social-Ecological Model
2. Methods
2.1. Compliance with Ethical Standards
2.2. Design
2.3. Setting
2.4. Participant Recruitment
2.4.1. Residents
Inclusion and Exclusion Criteria
2.4.2. Professionals
Inclusion and Exclusion Criteria
2.5. Protocol
2.6. Data Management
2.7. Data Analysis
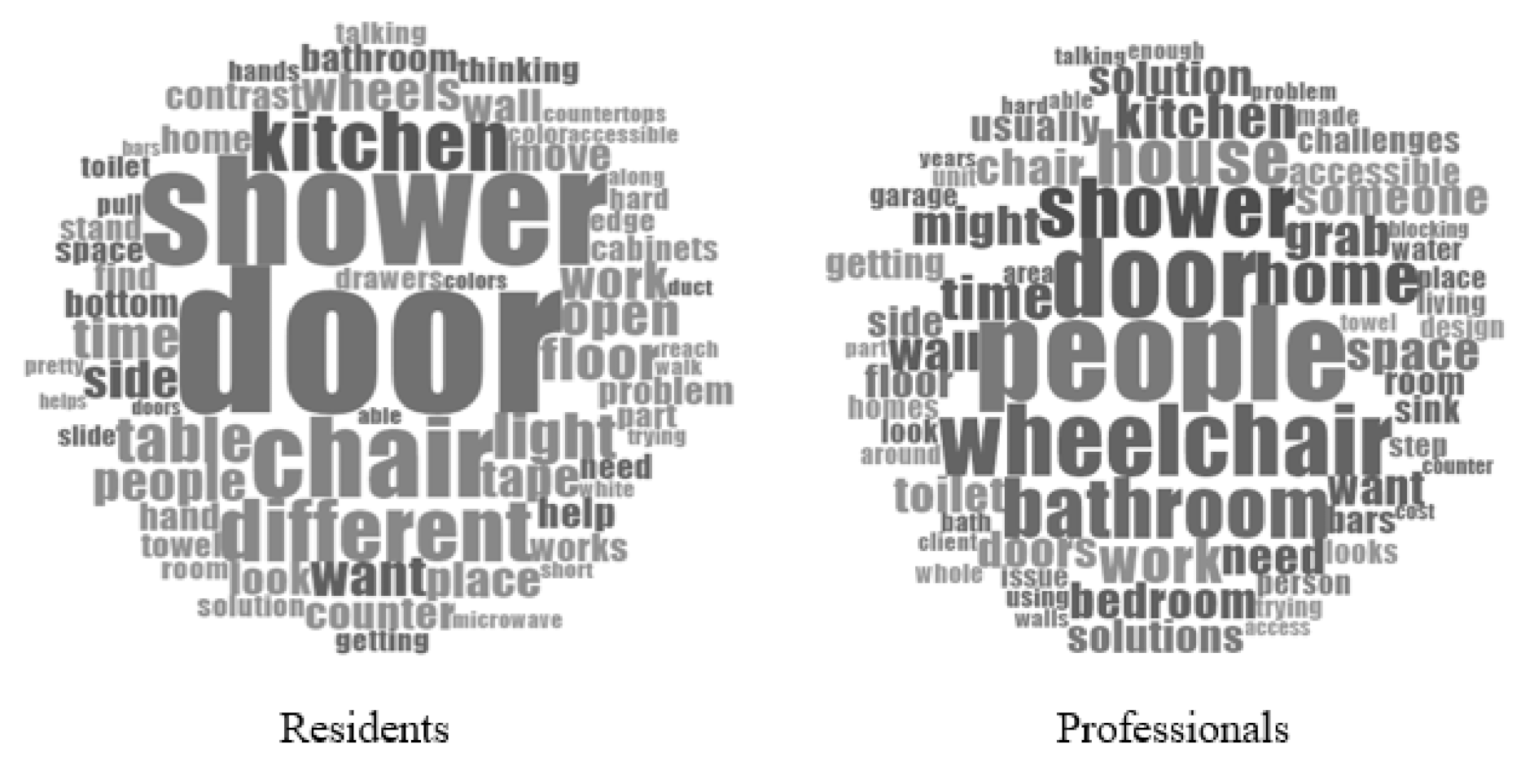
3. Results
3.1. Participant Characteristics
3.2. Individual
3.2.1. Needs and Preferences
“… To really not just evaluate the space but how they move and operate within that space and which areas they spend the most time in or what they do the most in those areas. And then time for decision making and talking together about what they would consider doable, or they would even consider, you know…in this menu of options you have, which part of the menu are you agreeable to even consider?”
3.2.2. Affordability
“I … remember like how big the plate is, and I try to go as back as far as I can before I set it down, and then I … use like my sense of touch as a gauge to kind of maneuver it.”
“Even from then [1990s] to now this stuff that was really, really cost-prohibitive and expensive … [but] these ideas we are coming up with they might be cost-prohibitive now but next week they won’t be. Somebody, some entrepreneur will come up and say, ‘okay, this need, I can make a bunch of money if I do this … and so I’ll get a quarter, I’ll sell millions of them.’”
3.3. Relationship
3.3.1. Resident and Family/Caregivers
3.3.2. Resident and Professional
3.3.3. Professional and Professional
3.4. Community
3.4.1. Community Resources
3.4.2. Neighbors
“[Home modifications] may even have a local government blessing. You can do this in certain neighborhoods, but the neighbors themselves don’t want it ‘cause they think it’s gonna take down the value of their property to do that.”
3.5. Societal
3.5.1. Laws
3.5.2. Social Norms
“Is there a cheaper way to do it just do it from the get-go? Make the homes universal design or at least … a bedroom and a bathroom on the first floor that you can… that has the three-foot door to make it accessible.”
“I was just thinking that almost all solutions are usually based on some short-term thought process … we just need to accommodate somebody for six months, a year, two years … it would be wonderful if houses came a little better prepared for a longer-term solution instead of having to be modified for a short-term solution, but I don’t know how you get there.”
4. Discussion
4.1. Individual Level
4.2. Relationship Level
4.3. Community Level
4.4. Societal Level
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Healthy Places Terminology. Available online: https://www.cdc.gov/healthyplaces/terminology.htm (accessed on 9 June 2021).
- Harrell, R.; Lynott, J.; Guzman, S.; Lampkin, C. What Is Livable? Community Preferences of Older Adults. Available online: http://www.aarp.org/ppi (accessed on 9 June 2021).
- Lee, S.-J.; Parrott, K.R.; Giddings, V.L.; Robinson, S.R.; Brown, G. The Influence of Home Modifications on Aging in Place for North Carolina Low-Income Elderly Homeowners. J. Fam. Consum. Sci. 2018, 109, 26–32. [Google Scholar] [CrossRef]
- World Health Organization. Good Health Adds Life to Years: Global Brief for World Health Day. 2012. Available online: http://www.who.int/world_health_day/2012 (accessed on 9 June 2021).
- Bo’sher, L.; Chan, S.; Ellen, I.G.; Karfunkel, B.; Liao, H. Accessibility of America’s Housing Stock: Analysis of the 2011 American Housing Survey (AHS). SSRN Electron. J. 2015. [Google Scholar] [CrossRef]
- Aplin, T.; de Jonge, D.; Gustafsson, L. Understanding the dimensions of home that impact on home modification decision making. Aust. Occup. Ther. J. 2013, 60, 101–109. [Google Scholar] [CrossRef]
- Struckmeyer, L.R.; Campbell, N.; Ellison, C.; Ahrentzen, S.; Classen, S. Home modifications and repurposing: Perspectives on the accessibility, affordability, and attractiveness. Disabil. Rehabil. 2021, 1–10. [Google Scholar] [CrossRef]
- Dye, C.; Willoughby, D.; Aybar-Damali, B.; Grady, C.; Oran, R.; Knudson, A. Improving Chronic Disease Self-Management by Older Home Health Patients through Community Health Coaching. Int. J. Environ. Res. Public Health 2018, 15, 660. [Google Scholar] [CrossRef] [PubMed]
- Barstow, B.A.; Bennett, D.K.; Vogtle, L.K. Perspectives on Home Safety: Do Home Safety Assessments Address the Concerns of Clients With Vision Loss? Am. J. Occup. Ther. 2011, 65, 635–642. [Google Scholar] [CrossRef]
- Keall, M.D.; Pierse, N.; Howden-Chapman, P.; Cunningham, C.; Cunningham, M.; Guria, J.; Baker, M.G. Home modifications to reduce injuries from falls in the Home Injury Prevention Intervention (HIPI) study: A cluster-randomised controlled trial. Lancet 2015, 385, 231–238. [Google Scholar] [CrossRef]
- Stark, S.; Landsbaum, A.; Palmer, J.; Somerville, E.K.; Morris, J.C. Client-centered home modifications improve daily activity performance of older adults. Can. J. Occup. Ther. 2009, 76, 235–245. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2857667/ (accessed on 9 June 2021). [CrossRef]
- Carnemolla, P.; Bridge, C. Housing Design and Community Care: How Home Modifications Reduce Care Needs of Older People and People with Disability. Int. J. Environ. Res. Public Health 2019, 16, 1951. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Nahemow, L. Ecology and the aging process. In The Psychology of Adult Development and Aging; Eisdorfer, C., Lawton, M.P., Eds.; American Psychological Association: Washington, DC, USA, 1973; pp. 154–196. [Google Scholar]
- Marquardt, G.; Johnston, D.; Black, B.S.; Morrison, A.; Rosenblatt, A.; Lyketsos, C.G.; Samus, Q.M. A Descriptive Study of Home Modifications for People with Dementia and Barriers to Implementation. J. Hous. Elder. 2011, 25, 258–273. [Google Scholar] [CrossRef]
- Wiseman, J.M.; Stamper, D.S.; Sheridan, E.; Caterino, J.M.; Quatman-Yates, C.C.; Quatman, C.E. Barriers to the Initiation of Home Modifications for Older Adults for Fall Prevention. Geriatr. Orthop. Surg. Rehabil. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Benefield, L.E.; Holtzclaw, B. Aging in Place. Nurs. Clin. N. Am. 2014, 49, 123–131. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. The Social-Ecological Model: A Framework for Prevention. Available online: https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html (accessed on 9 June 2021).
- Sallis, J.F.; Owen, N.; Fisher, E. Ecological models of health behavior. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass/Wiley: Hoboken, NJ, USA, 2015; pp. 43–64. ISBN 978-1-118-62900-0. [Google Scholar]
- Rebuilding Together. Rebuilding Together. Available online: https://rebuildingtogether.org/ (accessed on 9 June 2021).
- Project Re-Envision. Available online: https://pre.dcp.ufl.edu/ (accessed on 9 June 2021).
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice, 4th ed.; Sage Publications: St. Paul, MN, USA, 2014; pp. 244–326. ISBN 978-1412972123. [Google Scholar]
- Helle, T.; Iwarsson, S.; Brandt, Å. Validation of Housing Standards Addressing Accessibility. J. Appl. Gerontol. 2014, 33, 848–869. [Google Scholar] [CrossRef]
- Pettersson, C.; Brandt, Å.; Lexell, E.M.; Iwarsson, S. Autonomy and Housing Accessibility Among Powered Mobility Device Users. Am. J. Occup. Ther. 2015, 69, 6905290030. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pettersson, C.; Iwarsson, S.; Brandt, Å.; Norin, L.; Lexell, E.M. Men’s and women’s perspectives on using a powered mobility device: Benefits and societal challenges. Scand. J. Occup. Ther. 2014, 21, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, B.D.; Ma, E.A.M. Family, Know Thyself: A Workbook-Based Intergenerational Intervention to Improve Parent Care Coordination. Clin. Gerontol. 2009, 32, 147–163. [Google Scholar] [CrossRef]
- Kaup, M. Life-Span Housing for Aging in Place: Addressing the Home as an Integrated Part of the Solution to Long-Term Care in America. Sr. House Care J. 2009, 17, 101–113. [Google Scholar]
- Chee, Y.K.; Gitlin, L.N.; Dennis, M.P.; Hauck, W.W. Predictors of adherence to a skill-building intervention in dementia caregivers. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2007, 62, 673–678. [Google Scholar] [CrossRef]
- Nguyen, A.T.; Somerville, E.K.; Espín-Tello, S.M.; Keglovits, M.; Stark, S.L. A Mobile App Directory of Occupational Therapists Who Provide Home Modifications: Development and Preliminary Usability Evaluation. JMIR Rehabil. Assist. Technol. 2020, 7, e14465. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Simplican, S.C.; Leader, G.; Kosciulek, J.; Leahy, M. Defining social inclusion of people with intellectual and developmental disabilities: An ecological model of social networks and community participation. Res. Dev. Disabil. 2015, 38, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Marek, K.D.; Stetzer, F.; Adams, S.J.; Popejoy, L.L.; Rantz, M. Aging in Place Versus Nursing Home Care: Comparison of Costs to Medicare and Medicaid. Res. Gerontol. Nurs. 2012, 5, 123–129. [Google Scholar] [CrossRef] [PubMed]
- National Council on Independent Living. Visitability: Basic Access to Homes. Available online: https://visitability.org (accessed on 30 July 2021).
- National Council on Independent Living. NCIL Testimony to Congress in Support of the Inclusive Home Design Act. Available online: https://visitability.org/policy-strategies/ncil-testimony-to-congress-in-support-of-the-inclusive-home-design-act/ (accessed on 30 July 2021).
- Bridge, C.; Carnemolla, P.; Maalsen, S.; O’Neil, S.; Zmudzki, F. DIY Home Modifications: What information is required at point-of-sale? Final. Rep. 2016. [Google Scholar] [CrossRef]
| Ecological Level | Factors | Residents’ Counts | Professionals’ Counts |
|---|---|---|---|
| Individual | Needs & Preferences | 44 | 39 |
| Affordability | 4 | 11 | |
| Relationship | Resident & Family/Caregiver | 10 | 3 |
| Resident & Professional | 4 | 5 | |
| Professional & Professional | 0 | 4 | |
| Community | Community Resources | 11 | 14 |
| Neighbors | 0 | 2 | |
| Societal | Laws | 0 | 7 |
| Social Norms | 1 | 10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ellison, C.; Struckmeyer, L.; Kazem-Zadeh, M.; Campbell, N.; Ahrentzen, S.; Classen, S. A Social-Ecological Approach to Identify Facilitators and Barriers of Home Modifications. Int. J. Environ. Res. Public Health 2021, 18, 8720. https://doi.org/10.3390/ijerph18168720
Ellison C, Struckmeyer L, Kazem-Zadeh M, Campbell N, Ahrentzen S, Classen S. A Social-Ecological Approach to Identify Facilitators and Barriers of Home Modifications. International Journal of Environmental Research and Public Health. 2021; 18(16):8720. https://doi.org/10.3390/ijerph18168720
Chicago/Turabian StyleEllison, Carlyn, Linda Struckmeyer, Mahshad Kazem-Zadeh, Nichole Campbell, Sherry Ahrentzen, and Sherrilene Classen. 2021. "A Social-Ecological Approach to Identify Facilitators and Barriers of Home Modifications" International Journal of Environmental Research and Public Health 18, no. 16: 8720. https://doi.org/10.3390/ijerph18168720
APA StyleEllison, C., Struckmeyer, L., Kazem-Zadeh, M., Campbell, N., Ahrentzen, S., & Classen, S. (2021). A Social-Ecological Approach to Identify Facilitators and Barriers of Home Modifications. International Journal of Environmental Research and Public Health, 18(16), 8720. https://doi.org/10.3390/ijerph18168720






