Systematic Review of the Relationships between 24-Hour Movement Behaviours and Health Indicators in School-Aged Children from Arab-Speaking Countries
Abstract
1. Introduction
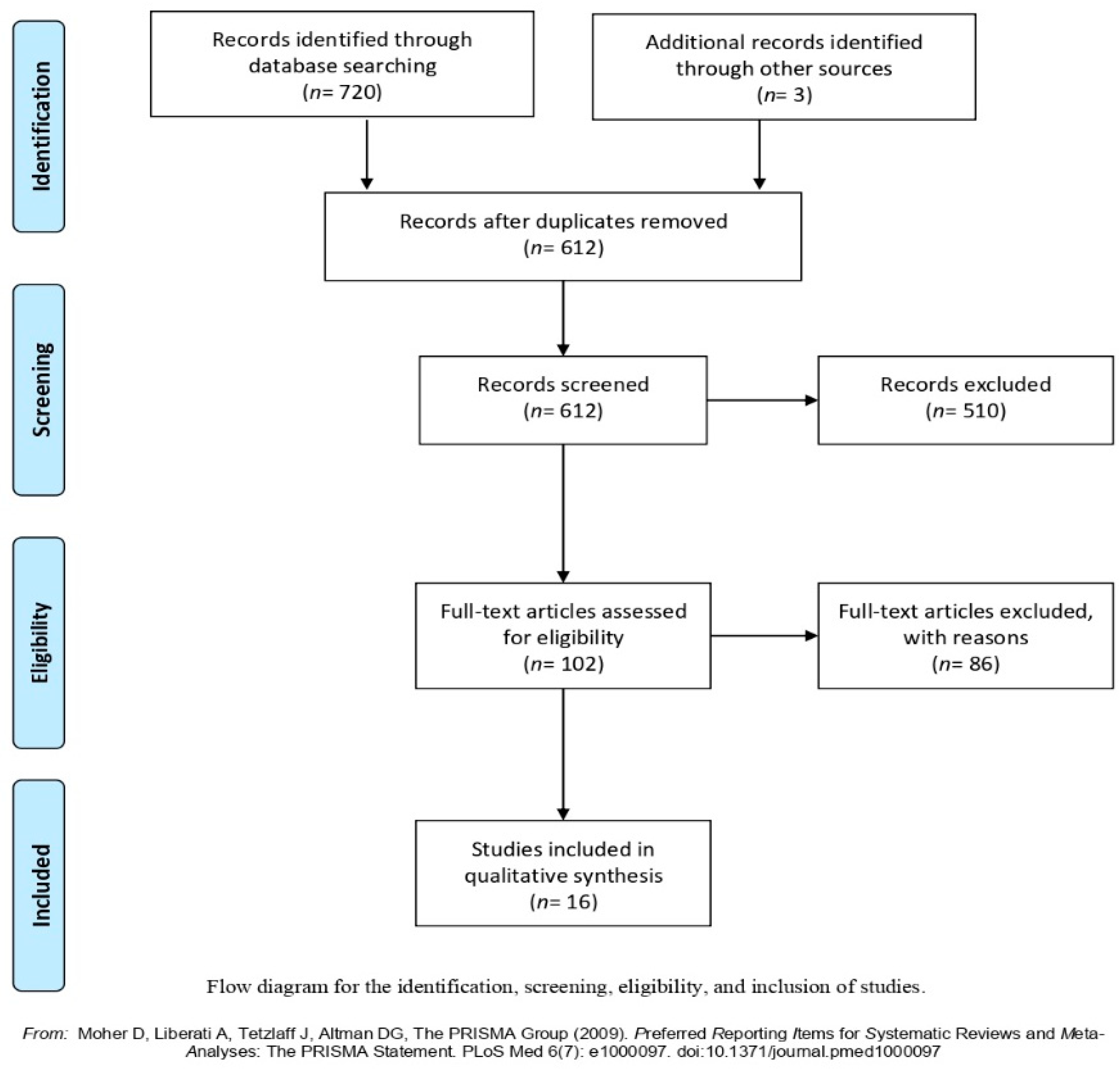
2. Methods
2.1. Eligibility Criteria
Sleep: “a naturally recurring state of body and mind characterized by altered consciousness, relatively inhibited sensory activity, inhibition of nearly all voluntary muscles and reduced interactions with surroundings”.[13]
SB: “any waking behaviour characterized by an energy expenditure ≤1.5 metabolic equivalents (METs), while in a sitting, reclining or lying posture”.[14]
PA: “any bodily movement produced by skeletal muscles that results in energy expenditure above the resting metabolic rate”.[15]
2.2. Search Strategy
2.3. Data Extraction
2.4. Quality Assessment
| Literature Reference and Country | Study Design | Sample Size (% Female), Mean Age or Age Range (Years) | Type of Behaviour | Exposure and Assessment Instrument | Outcomes | Statistical Analysis & Confounders (If Reported) | Main Results |
|---|---|---|---|---|---|---|---|
| AlHazzaa et al., (2019) Saudi Arabia [17] | Cross-sectional | 1033 (51.1% female); mean age = 9.2 ± 1.7 | Sleep | Sleep: Parent-proxy reported average sleep duration per night (<9 h vs. ≥9 h). | Adiposity: body weight (kg) and BMI. | Logistic regression analysis. Confounders: body weight, age and gender. | No significant association between sleep duration and overweight or obesity status (aOR = 1.00; 95% CI 0.71 t0 1.64; p = 0.717). |
| Al-Hazzaa, (2007) Saudi Arabia [18] | Cross-sectional | 296 (100% male); mean age = 10.3 ± 1.3 | PA | PA: Pedometer measured steps taken/day. | Adiposity: BMI, skinfold measurements (triceps and subscapular, body fat %, FMI and FFMI. | Pearson’s correlation. Confounders: age, gender, daily pedometer counts and total energy expenditure. | Significant negative associations between step counts/day and body fat % (r = −0.207; p = 0.006), BMI (r = −0.198; p = 0.007), FMI (r = −0.214; p = 0.004), but not with FFMI (r = −0.089; p = 0.231). |
| Hassan and Al-Kharusy, (2000) Oman [19] | Pilot study | 109 (100% male); mean age = 9.68 ± 0.92 | PA and SB | PA: Leisure time sport activities personal activity score (hours/week) assessed with 1.6–km run/walk. SB: Parent-proxy reported duration of TV watching and/or playing video or computer games. | Fitness: cardiorespiratory endurance. Adiposity: Log sum of 5 skinfold measurements (triceps, subscapular, suprailiac, abdominal and thigh). | Pearson correlation coefficients. | Personal activity score has a strong negative correlation with the time to complete the 1.6 km run/walk and the sum of skinfolds (r = −0.40, −0.42; p = 0.001). No significant associations between TV watching hours and fitness or fatness (p = n.r). |
| Hadhood et al., (2016) Egypt [20] | Cross-sectional | 711 (54.5% female); mean age = 10.36 ± 1.9 | PA | PA: Parent-proxy reported weekly practice of physical exercise. | Adiposity: BMI and body weight. | Chi square test. | No significant association between physical exercise and overweight and/or obesity (p = 0.19). |
| Badawi et al., (2013) Egypt [21] | Cross-sectional | 852 (50.2% female); mean age = 9.5 ± 1.8 | PA and SB | PA: Parent-proxy reported practice of sports, and transportation to school. SB: Parent-proxy reported time spent watching TV. | Adiposity: BMI and body weight. | t-test, ANOVA test. | Significant association between low PA and BMI (p = < 0.001). Significant association between SB and BMI (p = < 0.001). |
| Al-Lahham et al., (2019) Palestine [22] | Cross-sectional | 1320 (48% female); mean age = 9.5 ± 1.5 | PA and SB | PA: Parent-proxy reported daily PA (min), mode of transport to school. SB: Parent-proxy reported screen time (min). | Adiposity: BMI and body weight. | Chi square test. Confounders: transporting means to school, total screen time, total PA time and age. | Significant association between levels of PA (transportation means only) and BMI (p = 0.031). Screen time had no significant effect on BMI, however, it had a borderline effect (p = 0.069). |
| Jemaa et al., (2018) Tunisia [23] | Cross-sectional | 40 (47.5% female); mean age = 9.34 ± 0.94 | PA and SB | PA and SB: Accelerometer measures (LPA, MPA, VPA, MVPA); Subjective measures (mean PA Questionnaire for Older Children (PAQ-C) score and intensity classification). | Adiposity: % fat mass. | Pearson Correlation coefficient. | The average MVPA showed a negative significant correlation with body fat % (r = −0.343, p = 0.030). The score of PA determined by PAQ-C was not significantly correlated with the body fat % (r = −0.227, p = 0.158). |
| Lafta and Kadhim, (2005) Iraq [24] | Case control | 2084 (male and female); 7–13 (age range) | SB | SB: Parent proxy reported watching TV (>3 h/day) via questionnaire. | Adiposity: BMI-defined overweight/obese. | Chi-square test. Confounders: age, birth rank, type of feeding during infancy, dietary pattern, pattern of PA and working after school time. | Watching TV (> 3 h/day) was a significant factor for overweight in 7–9 year males ( = 19.69, 95% CI 1.79 to 4.97; p < 0.001). |
| Alam (2008) Saudi Arabia [25] | Cross-sectional | 1072 (100% female); 8–12 (age range) | SB | SB: Parent proxy reported duration of TV watching via questionnaire. | Adiposity: BMI and body weight. | Chi square test. | Watching TV (>2 h/day) was significantly higher among obese students ( = 12.98, p = 0.011). |
| Arora et al., (2018) Qatar [26] | Cross-sectional | 264 (62.1% female); mean age = 9.0 ± 1.2 | Sleep and SB | Sleep: weekday sleep duration. SB: SB time assessed with wrist Actigraphy/Technology Use Questionnaire. | Adiposity: BMI z-score, waist circumference, neck circumference, body fat % and fat mass. | Multiple linear regression. Confounders: objective estimate of sedentariness, dietary habits, age, sex, ethnicity and total technology use. | Significant associations between sleep duration and sleep insufficiency (<8 h) and all indicators of obesity (p < 0.001) except for neck circumference. Waist circumference (cm) yielded the largest effect: β = −4.99, p < 0.001 (average sleep duration) and β = 6.49, p < 0.001 (<8 h). Sleep duration variation (night-to-night sleep duration variability) was not significantly associated with any outcome. Poor sleep efficiency was positively associated with body fat percentage (β = 2.20, p = 0.028). |
| Al-Kutbe et al., (2017) Saudi Arabia [27] | Cross-sectional | 266 (100% female); 8–11 (age range) | PA and SB | PA and SB: Number of steps taken/day with accelerometer (WGT3X-BTActigraph). | Adiposity: body weight (kg). | Multiple linear regression. Confounders: daily energy intake, daily total energy expenditure, body weight, age and family income. | No association between the number of steps or the time spent in MVPA and body weight (Beta = 0.034; p = 0.575, 0.368). |
| Al-Hazzaa and Alrasheedi, (2007) Saudi Arabia [28] | Cross-sectional | 224 (51.3% female); mean age = 5.19 ± 0.85 | PA and SB | PA: Pedometer measured steps taken/day. SB: Parent proxy reported duration of TV watching/day via questionnaire. | Adiposity: BMI, skinfold measurements (triceps, subscapular (sum and ratio), FM %, FFM %, FMI and FFMI. | One-way ANOVA and post hoc test (Scheffe). Confounders: body size for FMI and FFMI only. | No significant differences between obese and non-obese children in steps counts/day (p = 0.109). No significant difference between active and inactive preschool children in any of the measured anthropometric and body composition variables (body weight (p = 0.644), BMI (p = 0.961), triceps skinfold (p = 0.975), subscapular skinfold (p = 0.738), sum of 2 skinfolds (p = 0.854), subscapular/triceps ratio (p = 0.219), fat % (p = 0.985), fat mass (p = 0.664), fat free mass (p = 0.744), FMI (p = 0.850), FFMI (p = 0.896). Obese children spent significantly more time watching TV (197.5 ± 89.3 min/day) than their non-obese peers (150.0 ± 60.9 min/day) (p = 0.001). |
| Alqaderi et al., (2016) Kuwait [29] | Longitudinal study | 8317 in 1st phase and 6316 in 2nd phase (61.4% female); 8–11 at visit 1, 10–12 at follow up (age range) | Sleep | Sleep: Lifestyle habits interview reported daily sleep hours, TV and video game use. | Adiposity: Waist circumference. | Multilevel longitudinal linear regression model. Confounders: age and gender. | Short sleep duration was significantly associated with increased waist circumference (beta = −0.11; 95%CI 0.14 to 0.17; p = < 0.05). |
| Al-Ghamdi, (2013) Saudi Arabia [30] | Case control | 397 (49.3% female); mean age = 11.4 (SD: n.r.) | PA and SB | PA and SB: questionnaire (interview) reported watching TV (>3 h/day) and daily exercise. | Adiposity: BMI. | Chi-square test. Confounders: TV, VG time/day, age, daily exercise/day. | Watching TV (>3 h/day), especially over the weekend, was significantly associated with childhood obesity ( = 4.136, p = 0.042). No significant associations between the rate of exercising at school, home and outdoors and obesity ( = 1.248, 1.032, 2.604; p = 0.870, 0.905, 0.626). |
| Yousef et al., (2013) UAE [31] | Cross-sectional | 197 (34% female); mean age = 8.7 ± 2.1 | SB | SB: Parent proxy reported watching TV (>2 h/day). | Behavioral problems. | Chi square test, logistic regression. Confounders: birth order and number of siblings. | Watching TV/video game > 2 h/day was associated with withdrawn behavior (OR = 0.275; 95% CI 0.106 to 0.712; p = 0.008), attention problem (OR = 0.480; 95% CI 0.241 to 0.956; p = 0.037), externalizing problems (OR = 0.393; 95% CI 0.201 to 0.771; p = 0.007) and Child Behavior Checklist total score (OR = 0.441; 95% CI 0.229 to 0.848; p = 0.014). |
| Zayed and Kilani, (2014) Oman [32] | Cross-sectional | 165 (100% female); 10–13 (age range) | PA | PA: number of occurrences and the duration of the practice of PA per week assessed with PA interview questionnaire. | Depression and low self-esteem. | One-way ANOVA and post hoc test (Scheffe). | Regular PA was significantly associated with improved self-esteem; differences were seen between those who never exercised and those who exercised regularly (mean square = 358.257; F = 4.787; p = 0.10). |
3. Results
3.1. Measurement of Movement Behaviours
3.2. Health Indicators
3.2.1. Adiposity
3.2.2. Behavioural Problems
3.2.3. Depression and Low Self-Esteem
3.2.4. Fitness
4. Discussion
4.1. Areas for Future Research
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A. Supplementary Information
References
- Tremblay, M.S.; Colley, R.C.; Saunders, T.; Healy, G.; Owen, N. Physiological and health implications of a sedentary lifestyle. Appl. Physiol. Nutr. Metab. 2010, 35, 725–740. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Carson, V.; Gray, C.E.; Tremblay, M.S. Importance of All Movement Behaviors in a 24 Hour Period for Overall Health. Int. J. Environ. Res. Public Health 2014, 11, 12575–12581. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Carson, V.; Chaput, J.-P.; Gorber, S.C.; Dinh, T.; Duggan, M.; Faulkner, G.; Gray, C.E.; Gruber, R.; Janson, K.; et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl. Physiol. Nutr. Metab. 2016, 41, S311–S327. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.; Pate, R.R.; Gorber, S.C.; Kho, M.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.; Okely, A.; Gorber, S.C.; et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Gray, C.; Poitras, V.J.; Carson, V.; Gruber, R.; Olds, T.; Weiss, S.K.; Gorber, S.C.; Kho, M.; Sampson, M.; et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S266–S282. [Google Scholar] [CrossRef] [PubMed]
- Saunders, T.J.; Gray, C.; Poitras, V.J.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.; Olds, T.; Gorber, S.C.; Kho, M.; Sampson, M.; et al. Combinations of physical activity, sedentary behaviour and sleep: Relationships with health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S283–S293. [Google Scholar] [CrossRef] [PubMed]
- Okely, A.; Ghersi, D.; Loughran, S.; Cliff, D.; Shilton, T.; Jones, R. Australian 24-hour movement guidelines for children (5–12 years) and young people (13–17 years): An integration of physical activity, sedentary behaviour. Canberra: Aust. Gov. 2019. [Google Scholar] [CrossRef]
- Child labour in Arab States (IPEC). International Programme on the Elimination of Child Labour (IPEC). Available online: https://www.ilo.org/ipec/Regionsandcountries/arab-states/lang--en/index.htm (accessed on 8 January 2020).
- Sharara, E.; Akik, C.; Ghattas, H.; Obermeyer, C.M. Physical inactivity, gender and culture in Arab countries: A systematic assessment of the literature. BMC Public Health 2018, 18, 639. [Google Scholar] [CrossRef]
- Farrag, N.S.; Cheskin, L.J.; Farag, M.K. A systematic review of childhood obesity in the Middle East and North Africa (MENA) region: Prevalence and risk factors meta-analysis. Adv. Pediatr. Res. 2017, 4, 8. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Chaput, J.; Saunders, T.; Carson, V. Interactions between sleep, movement and other non-movement behaviours in the pathogenesis of childhood obesity. Obes. Rev. 2017, 18, 7–14. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; On Behalf of Sbrn Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; Debeer, H. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiology 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Alhussain, M.; Alhowikan, A.M.; Obeid, O.A. Insufficient Sleep Duration and Its Association with Breakfast Intake, Overweight/Obesity, Socio-Demographics and Selected Lifestyle Behaviors among Saudi School Children. Nat. Sci. Sleep 2019, 11, 253–263. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M. Pedometer-determined physical activity among obese and non-obese 8- to 12-year-old Saudi schoolboys. J. Physiol. Anthr. 2007, 26, 459–465. [Google Scholar] [CrossRef]
- Hassan, M.O.; Al-Kharusy, W. Physical fitness and fatness among Omani schoolboys: A pilot study. J. Sci. Res. Med Sci. 2000, 2, 37–41. [Google Scholar]
- Hadhood, S.E.S.A.; Ali, R.A.E.; Mohamed, M.M.; Mohammed, E.S. Prevalence and Correlates of Overweight and Obesity among School Children in Sohag, Egypt. Open J. Gastroenterol. 2017, 7, 75–88. [Google Scholar] [CrossRef][Green Version]
- Badawi, N.E.-S.; Barakat, A.A.; El Sherbini, S.A.; Fawzy, H.M. Prevalence of overweight and obesity in primary school children in Port Said city. Egypt. Pediatr. Assoc. Gaz. 2013, 61, 31–36. [Google Scholar] [CrossRef]
- Al-Lahham, S.; Jaradat, N.; Altamimi, M.; Anabtawi, O.; Irshid, A.; Alqub, M.; Dwikat, M.; Nafaa, F.; Badran, L.; Mohareb, R.; et al. Prevalence of underweight, overweight and obesity among Palestinian school-age children and the associated risk factors: A cross sectional study. BMC Pediatr. 2019, 19, 1–13. [Google Scholar] [CrossRef]
- Ben Jemaa, H.; Mankaï, A.; Mahjoub, F.; Kortobi, B.; Khlifi, S.; Draoui, J.; Minaoui, R.; Karmous, I.; Ben Hmad, H.; Ben Slama, F.; et al. Physical Activity Level Assessed by Accelerometer and PAQ-C in Tunisian Children. Ann. Nutr. Metab. 2018, 73, 234–240. [Google Scholar] [CrossRef]
- Lafta, R.K.; Kadhim, M.J. Childhood obesity in Iraq: Prevalence and possible risk factors. Ann. Saudi Med. 2005, 25, 389–393. [Google Scholar] [CrossRef]
- Alam, A.A. Obesity among female school children in North West Riyadh in relation to affluent lifestyle. Saudi Med. J. 2008, 29, 1139–1144. [Google Scholar]
- Arora, T.; Gad, H.; Omar, O.M.; Choudhury, S.; Chagoury, O.; Sheikh, J.; Taheri, S. The associations among objectively estimated sleep and obesity indicators in elementary schoolchildren. Sleep Med. 2018, 47, 25–31. [Google Scholar] [CrossRef]
- Al-Kutbe, R.; Payne, A.; De Looy, A.; Rees, G.A. A comparison of nutritional intake and daily physical activity of girls aged 8-11 years old in Makkah, Saudi Arabia according to weight status. BMC Public Health 2017, 17, 592. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; A Al-Rasheedi, A. Adiposity and physical activity levels among preschool children in Jeddah, Saudi Arabia. Saudi Med. J. 2007, 28, 766. [Google Scholar]
- Alqaderi, H.; Goodson, J.M.; Subramanian, S.V.; Tavares, M. Short Sleep Duration and Screen-Based Activities: A Longitudinal Multilevel Analysis. Am. J. Lifestyle Med. 2016, 12, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Al-Ghamdi, S.H. The association between watching television and obesity in children of school-age in Saudi Arabia. J. Fam. Community Med. 2013, 20, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Yousef, S.; Eapen, V.; Zoubeidi, T.; Mabrouk, A. Behavioral correlation with television watching and videogame playing among children in the United Arab Emirates. Int. J. Psychiatry Clin. Pr. 2014, 18, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Zayed, K.; Kilani, H. Physical activity is associated with depression and self-esteem levels among Omani female children. Can. J. Clin. Nutr. 2014, 2, 15–28. [Google Scholar]
- COVID-19 on the Arab Region An Opportunity to Build Back Better. 2020. Available online: https://unsdg.un.org/resources/policy-brief-impact-covid-19-arab-region-opportunity-build-back-better (accessed on 10 January 2021).
- Baskaran, A. UNESCO Science Report: Towards 2030. Inst. Econ. 2016, 8, 125–127. [Google Scholar]
- Carson, V.; Chaput, J.-P.; Janssen, I.; Tremblay, M.S. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Prev. Med. 2017, 95, 7–13. [Google Scholar] [CrossRef]
- Turrisi, T.B.; Bittel, K.M.; West, A.B.; Hojjatinia, S.; Hojjatinia, S.; Mama, S.K.; Lagoa, C.M.; Conroy, D.E. Seasons, weather, and device-measured movement behaviors: A scoping review from 2006 to 2020. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 1–26. [Google Scholar] [CrossRef]
- Elasha, B.O. Mapping of Climate Change Threats and Human Development Impacts in the Arab Region; UNDP Arab Development Report–Research Paper Series; UNDP Regiona Bureau for the Arab States: Amman, Jordan, 2010; Available online: https://www.arabstates.undp.org/content/rbas/en/home/library/huma_development/mapping-of-climate-change-threats-and-human-development-impacts-.html (accessed on 6 January 2021).
- Al-Mohannadi, A.; Moahhed, G. The effect of weather conditions on the seasonal variation of physical activity. Aspetar Sports Med. J. 2015, 4, 228–231. [Google Scholar]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity: A systematic review. Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef]
- Edwards, N.M.; Myer, G.D.; Kalkwarf, H.J.; Woo, J.; Khoury, P.R.; Hewett, T.E.; Daniels, S.R. Outdoor Temperature, Precipitation, and Wind Speed Affect Physical Activity Levels in Children: A Longitudinal Cohort Study. J. Phys. Act. Health 2015, 12, 1074–1081. [Google Scholar] [CrossRef]
- Quante, M.; Wang, R.; Weng, J.; Kaplan, E.R.; Rueschman, M.; Taveras, E.M.; Rifas-Shiman, S.L.; Gillman, M.W.; Redline, S. Seasonal and weather variation of sleep and physical activity in 12–14-year-old children. Behav. Sleep Med. 2019, 17, 398–410. [Google Scholar] [CrossRef]
| Study | 1. Selection Bias | 2. Attrition Bias | 3. Detection Bias | 4. Performance Bias | 5. Selective Reporting Bias | Score * | ROB Quality | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Clear Criteria for Those included and/or Excluded? | Was the Sample Randomly Selected? | Did an Adequate Proportion (At Least 70%) of Those Consenting to Participate in the Study Have Complete Data? (Incomplete Follow-Up; High Loss to Follow-Up; Missing Data) | Did the Study Report the Sources and Details of the Tool Used in the Study to Assess The Outcomes? | Was the Tool Used in the Study to Assess the Outcomes Reliable and/or Valid? | Did the Study Report the Sources and Details of the Measurement Tool Used in the Study for Movement Behaviours? | Were the Measurements of Movement Behaviours in This Study Reliable and/or Valid? | Did the Study Have Complete Data and/or Reports All Outcomes and Not Others Based on the Results? | |||
| Rating | Rating | Rating | Rating | Rating | Rating | Rating | Rating | |||
| Al-Hazzaa et al., 2019 [17] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6/8 | Low |
| Al-Hazzaa, 2007 [18] | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 5/8 | High |
| Hassan and Al-Kharusy, 2000 [19] | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 4/8 | High |
| Hadhood et al., 2016 [20] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6/8 | Low |
| Badawi et al., 2013 [21] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6/8 | Low |
| Al-Lahham et al., 2019 [22] | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 4/8 | High |
| Jemaa et al., 2018 [23] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 6/8 | Low |
| Lafta and Kadhim, 2005 [24] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 5/8 | High |
| Alam, 2008 [25] | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 4/8 | High |
| Arora et al., 2018 [26] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7/8 | Low |
| Al-Kutbe et al., 2017 [27] | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6/8 | Low |
| Al-Hazzaa and Alrasheedi, 2007 [28] | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7/8 | Low |
| Al-Qaderi et al., 2016 [29] | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 5/8 | High |
| Al-Ghamdi, 2013 [30] | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 5/8 | High |
| Yousef et al., 2013 [31] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8/8 | Low |
| Zayed and Kilani, 2014 [32] | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 5/8 | High |
| 11/16 | 8/16 | 11/16 | 15/16 | 13/16 | 10/16 | 6/16 | 15/16 | |||
| Study | Outcomes | Exposure: Favorable Associations | Exposure: Null Associations | Summary | ||||
|---|---|---|---|---|---|---|---|---|
| Adiposity | PA | SB | Sleep | PA | SB | Sleep | ||
| Al-Kutbe et al., 2017 | Body weight | ✓ | ✓ | 5/14 studies showed favorable associations between PA and adiposity outcomes. 4/14 studies showed null associations between PA and adiposity outcomes. 6/14 studies showed favorable associations between SB and adiposity outcomes. 3/14 studies showed null associations between SB and adiposity outcomes. 2/14 studies showed favorable associations between sleep and adiposity outcomes 1/14 studies showed null association between sleep and adiposity outcomes. | ||||
| AlHazzaa et al., 2019 | Body weight and BMI | ✓ | ||||||
| Jemaa et al., 2018 | % fat mass | ✓ | ✓ | |||||
| Hadhoodet al., 2016 | BMI and body weight | ✓ | ||||||
| Badawi et al., 2013 | BMI and body weight | ✓ | ✓ | |||||
| Al-Lahham et al., 2019 | BMI and body weight | ✓ | ✓ | |||||
| Al-Hazzaa, 2007 | BMI, skinfold measurements (triceps and subscapular, body fat %, FMI and FFMI.) | ✓ | ||||||
| Arora et al., 2018 | BMI z-score, waist circumference, neck circumference, body fat % and fat mass. | ✓ | ✓ | |||||
| Alam, 2008 | BMI and body weight | ✓ | ||||||
| Al-Hazzaa and Alrasheedi, 2007 | BMI, skinfold measurements (triceps, subscapular (sum and ratio), FM %, FFM %, FMI and FFMI.) | ✓ | ✓ | |||||
| Lafta and Kadhim, 2005 | BMI -defined overweight/obese. | ✓ | ||||||
| Al-Ghamdi, 2013 | BMI | ✓ | ✓ | |||||
| Alqaderi et al., 2016 | Waist circumference | ✓ | ||||||
| Hassan and Al-Kharusy, 2000 | Log sum of 5 skinfold measurements (triceps, subscapular, suprailiac, abdominal and thigh). | ✓ | ||||||
| Yousef et al., 2013 | Behavioural problems | ✓ | 1/1 studies showed favorable association between SB and behavioural problems. | |||||
| Zayed and Kilani, 2014 | Depression and low self-esteem | ✓ | 1/1 studies showed favorable association between PA and depression and low self-esteem. | |||||
| Hassan and Al-Kharusy, 2000 | Fitness: cardiorespiratory endurance | ✓ | 1/1 studies showed null association between SB and fitness measures. | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, Y.A.; Sousa-Sá, E.; Chong, K.H.; Parrish, A.-M.; Okely, A.D. Systematic Review of the Relationships between 24-Hour Movement Behaviours and Health Indicators in School-Aged Children from Arab-Speaking Countries. Int. J. Environ. Res. Public Health 2021, 18, 8640. https://doi.org/10.3390/ijerph18168640
Alanazi YA, Sousa-Sá E, Chong KH, Parrish A-M, Okely AD. Systematic Review of the Relationships between 24-Hour Movement Behaviours and Health Indicators in School-Aged Children from Arab-Speaking Countries. International Journal of Environmental Research and Public Health. 2021; 18(16):8640. https://doi.org/10.3390/ijerph18168640
Chicago/Turabian StyleAlanazi, Yazeed A., Eduarda Sousa-Sá, Kar Hau Chong, Anne-Maree Parrish, and Anthony D. Okely. 2021. "Systematic Review of the Relationships between 24-Hour Movement Behaviours and Health Indicators in School-Aged Children from Arab-Speaking Countries" International Journal of Environmental Research and Public Health 18, no. 16: 8640. https://doi.org/10.3390/ijerph18168640
APA StyleAlanazi, Y. A., Sousa-Sá, E., Chong, K. H., Parrish, A.-M., & Okely, A. D. (2021). Systematic Review of the Relationships between 24-Hour Movement Behaviours and Health Indicators in School-Aged Children from Arab-Speaking Countries. International Journal of Environmental Research and Public Health, 18(16), 8640. https://doi.org/10.3390/ijerph18168640






_Okely.png)

