Exploring Treatment for Depression in Parkinson’s Patients: A Cross-Sectional Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
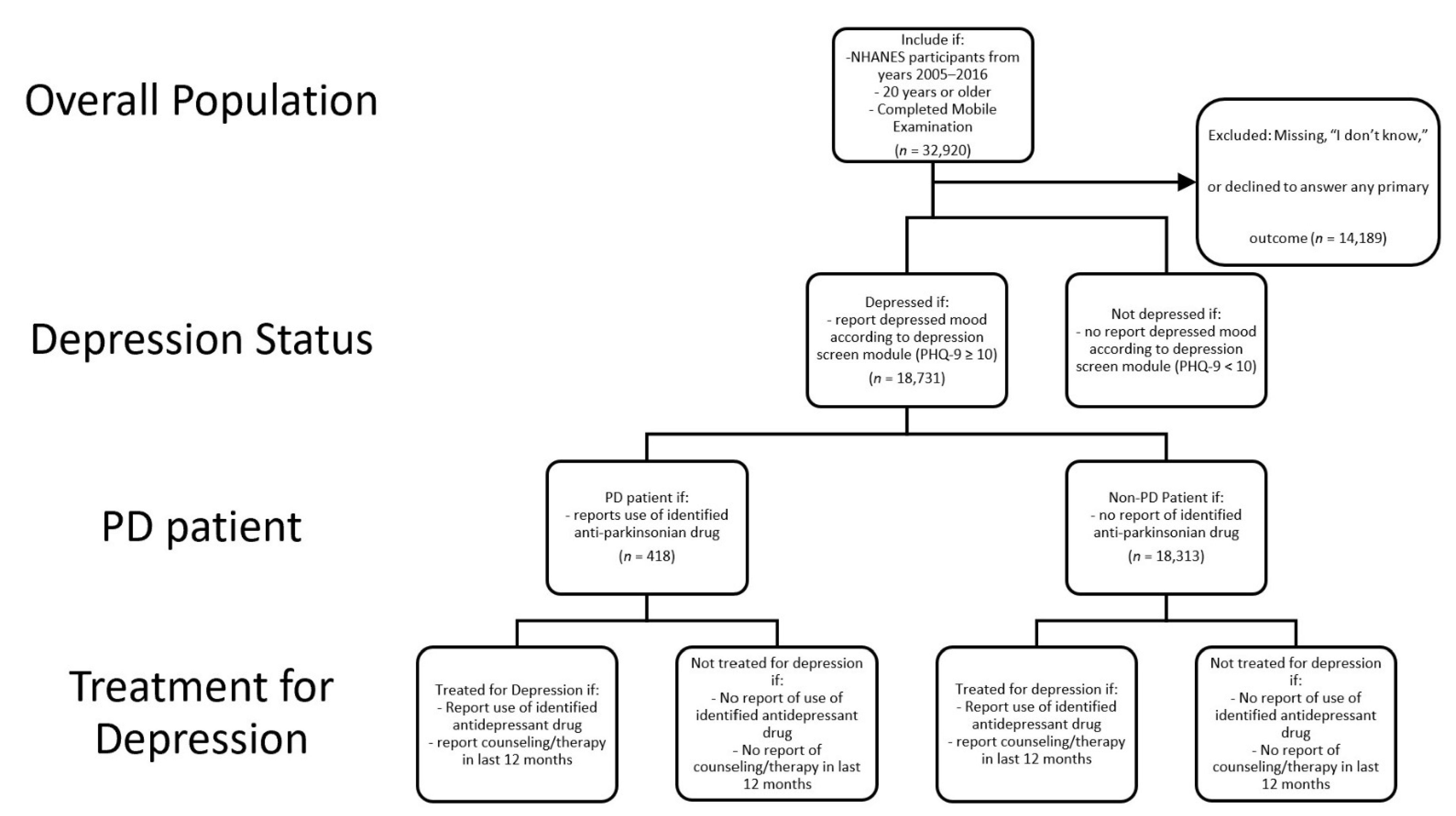
2.2. Study Design and Participant Sample
2.3. Measures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NHANES | National Health and Nutrition Examination Survey |
| PD | Parkinson’s Disease |
| PHQ-9 | Patient Health Questionnaire-9 |
| NCHS | National Center for Health Statistics |
| OR | Odds ratio |
References
- Marras, C.; Beck, J.C.; Bower, J.H.; Roberts, E.; Ritz, B.; Ross, G.W.; Abbott, R.D.; Savica, R.; Van Den Eeden, S.K.; Willis, A.W.; et al. Prevalence of Parkinson’s disease across North America. NPJ Parkinson’s Dis. 2018, 4, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeltere, L.; Kuzņecovs, V.; Erts, R. Depression and social phobia in essential tremor and Parkinson’s disease. Brain Behav. 2017, 7, e00781. [Google Scholar] [CrossRef]
- Bulloch, A.G.M.; Fiest, K.M.; Williams, J.V.A.; Lavorato, D.H.; Berzins, S.A.; Jetté, N.; Pringsheim, T.M.; Patten, S.B. Depression—A common disorder across a broad spectrum of neurological conditions: A cross-sectional nationally representative survey. Gen. Hosp. Psychiatry 2015, 37, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Reijnders, J.S.A.M.; Ehrt, U.; Weber, W.E.J.; Aarsland, D.; Leentjens, A.F.G. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov. Disord. 2008, 23, 183–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haasum, Y.; Fastbom, J.; Johnell, K. Use of antidepressants in Parkinson’s disease: A Swedish register-based study of over 1.5 million older people. Parkinsonism Relat. Disord. 2016, 27, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, S.; Vadiei, N.; Goldstone, L.; Alrabiah, Z.; Sherman, S.J. Patterns and Predictors of Depression Treatment among Older Adults with Parkinson’s Disease and Depression in Ambulatory Care Settings in the United States. Parkinson’s Dis. 2018, 2018. [Google Scholar] [CrossRef]
- Nagy, A.; Schrag, A. Neuropsychiatric aspects of parkinson’s disease. J. Neural Transm. 2019, 126, 889–896. [Google Scholar] [CrossRef]
- Van Uem, J.M.T.; Cerff, B.; Kampmeyer, M.; Prinzen, J.; Zuidema, M.; Hobert, M.A.; Gräber, S.; Berg, D.; Maetzler, W.; Liepelt-Scarfone, I. The association between objectively measured physical activity, depression, cognition, and health-related quality of life in Parkinson’s disease. Parkinsonism Relat. Disord. 2018, 48, 74–81. [Google Scholar] [CrossRef]
- Prisnie, J.C.; Sajobi, T.T.; Wang, M.; Patten, S.B.; Fiest, K.M.; Bulloch, A.G.M.; Pringsheim, T.; Wiebe, S.; Jette, N. Effects of depression and anxiety on quality of life in five common neurological disorders. Gen. Hosp. Psychiatry 2018, 52, 58–63. [Google Scholar] [CrossRef]
- Sagna, A.; Gallo, J.J.; Pontone, G.M. Systematic review of factors associated with depression and anxiety disorders among older adults with Parkinson’s disease. Parkinsonism Relat. Disord. 2014, 20, 708–715. [Google Scholar] [CrossRef] [Green Version]
- Antonini, A.; Tesei, S.; Zecchinelli, A.; Barone, P.; De Gaspari, D.; Canesi, M.; Sacilotto, G.; Meucci, N.; Mariani, C.; Pezzoli, G. Randomized study of sertraline and low-dose amitriptyline in patients with Parkinson’s disease and depression: Effect on quality of life. Mov. Disord. 2006, 21, 1119–1122. [Google Scholar] [CrossRef]
- Schrag, A.; Jahanshahi, M.; Quinn, N.P. What contributes to depression in Parkinson’s disease? Psychol. Med. 2001, 31, 65–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lachner, C.; Armstrong, M.J.; Gruber-Baldini, A.L.; Rezvani, Z.; Reich, S.G.; Fishman, P.S.; Salazar, R.; Shulman, L.M. Discordance Between Physician Assessment and Patient-Reported Depressive Symptoms in Parkinson Disease. J. Geriatr. Psychiatry Neurol. 2017, 30, 191–195. [Google Scholar] [CrossRef]
- Oehlberg, K.; Barg, F.K.; Brown, G.K.; Taraborelli, D.; Stern, M.B.; Weintraub, D. Attitudes regarding the etiology and treatment of depression in Parkinson’s disease: A qualitative study. J. Geriatr. Psychiatry Neurol. 2008, 21, 123–132. [Google Scholar] [CrossRef] [Green Version]
- Richard, I.H.; Kurlan, R. The under-recognition of depression in Parkinson’s disease. Neuropsychiatr. Dis. Treat 2006, 2, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.; Anderson, W.S.; Brandt, J.; Mari, Z.; Pontone, G.M. Neuropsychiatric Complications of Parkinson Disease Treatments: Importance of Multidisciplinary Care. Am. J. Geriatr. Psychiatry 2016, 24, 1171–1180. [Google Scholar] [CrossRef] [Green Version]
- McDonald, W.M.; Richard, I.H.; DeLong, M.R. Prevalence, etiology, and treatment of depression in Parkinson’s disease. Biol. Psychiatry 2003, 54, 363–375. [Google Scholar] [CrossRef]
- Althaus, A.; Arránz Becker, O.; Spottke, A.; Dengler, R.; Schneider, F.; Kloss, M.; Eggert, K.; Oertel, W.H.; Dillmann, U.; Herting, B.; et al. Frequency and treatment of depressive symptoms in a Parkinson’s disease registry. Parkinsonism Relat. Disord. 2008, 14, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Bega, D.; Wu, S.S.; Pei, Q.; Schmidt, P.N.; Simuni, T. Recognition and treatment of depressive symptoms in Parkinson’s disease: The NPF dataset. J. Parkinson’s Dis. 2014, 4, 639–643. [Google Scholar] [CrossRef] [Green Version]
- Menza, M.; Dobkin, R.D.; Marin, H.; Mark, M.H.; Gara, M.; Buyske, S.; Bienfait, K.; Dicke, A. The impact of treatment of depression on quality of life, disability and relapse in patients with Parkinson’s disease. Mov. Disord. 2009, 24, 1325–1332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Starkstein, S.E.; Brockman, S. Management of Depression in Parkinson’s Disease: A Systematic Review. Mov. Disord. Clin. Pr. 2017, 4, 470–477. [Google Scholar] [CrossRef] [Green Version]
- Goodarzi, Z.; Hanson, H.M.; Jette, N.; Patten, S.; Pringsheim, T.; Holroyd-Leduc, J. Barriers and Facilitators for Guidelines with Depression and Anxiety in Parkinson’s Disease or Dementia. Can. J. Aging 2018, 37, 185–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Hyattsville, MD, USA. Available online: https://wwwn.cdc.gov/nchs/nhanes/default.aspx (accessed on 12 July 2019).
- Wittayanukorn, S.; Qian, J.; Hansen, R.A. Prevalence of depressive symptoms and predictors of treatment among U.S. adults from 2005 to 2010. Gen. Hosp. Psychiatry 2014, 36, 330–336. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.S.; Oh, Y.; Rand, K.L.; Wu, W.; Cyders, M.A.; Kroenke, K.; Stewart, J.C. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in U.S. adults across sex, race/ethnicity, and education level: NHANES 2005–2016. Depress. Anxiety 2019, 36, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey (NHANES) MEC Interviewers Procedures Manual; US Department of Health and Human Services, Centers for Disease Control and Prevention: Hyatsville, MD, USA, 2016; pp. 5-1–5-3.
- Brody, D.J.; Pratt, L.A.; Hughes, J.P. Prevalence of Depression Among Adults Aged 20 and over: United States, 2013–2016; NCHS Data Brief, no. 303; National Center for Health Statistics: Hyatsville, MD, USA, 2018.
- Luo, Y.; Kataoka, Y.; Ostinelli, E.G.; Cipriani, A.; Furukawa, T.A. National Prescription Patterns of Antidepressants in the Treatment of Adults With Major Depression in the US Between 1996 and 2015: A Population Representative Survey Based Analysis. Front. Psychiatry 2020, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D.S.; Sarvet, A.L.; Meyers, J.L.; Saha, T.D.; Ruan, W.J.; Stohl, M.; Grant, B.F. Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA Psychiatry 2018, 75, 336–346. [Google Scholar] [CrossRef] [Green Version]
- Kohn, R.; Ali, A.A.; Puac-Polanco, V.; Figueroa, C.; Lopez-Soto, V.; Morgan, K.; Saldivia, S.; Vicente, B. Mental health in the Americas: An overview of the treatment gap. Rev. Panam. Salud. Publica 2018, 42, e165. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.F.; Wu, Y.; Sollinger, A.B.; Muthukattil, R.J.; Ferrara, J.M. Comparing No-Show Rates of Neurology Outpatients with and without Parkinson’s Disease: A Real-World Assessment of the Parkinsonian Personality Profile. J. Parkinsons Dis. 2020, 10, 347–350. [Google Scholar] [CrossRef]
- Weir, S.; Samnaliev, M.; Kuo, T.C.; Tierney, T.S.; Walleser Autiero, S.; Taylor, R.S.; Schrag, A. Short- and long-term cost and utilization of health care resources in Parkinson’s disease in the UK. Mov. Disord. 2018, 33, 974–981. [Google Scholar] [CrossRef] [Green Version]
- Katon, W.; Ciechanowski, P. Impact of major depression on chronic medical illness. J. Psychosomat. Res. 2002, 53, 859–863. [Google Scholar] [CrossRef]
- Richard, I.H.; LaDonna, K.A.; Hartman, R.; Podgorski, C.; Kurlan, R.; Group, S.-P.S. The patients’ perspective: Results of a survey assessing knowledge about and attitudes toward depression in PD. Neuropsychiatr. Dis. Treat. 2007, 3, 903–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, R.; Trivedi, R.; Gray, C.; Lorenz, K.A.; Zulman, D. Neurologist Strategies for Optimizing the Parkinson’s Disease Clinical Encounter. J. Geriatr. Psychiatry Neurol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Dobkin, R.D.; Rubino, J.T.; Friedman, J.; Allen, L.A.; Gara, M.A.; Menza, M. Barriers to mental health care utilization in Parkinson’s disease. J. Geriatr. Psychiatry Neurol. 2013, 26, 105–116. [Google Scholar] [CrossRef] [Green Version]
- Brandt-Christensen, M.; Kvist, K.; Nilsson, F.M.; Andersen, P.K.; Kessing, L.V. Use of antiparkinsonian drugs in Denmark: Results from a nationwide pharmacoepidemiological study. Mov. Disord. 2006, 21, 1221–1225. [Google Scholar] [CrossRef] [PubMed]

| Unweighted N | Weighted % | |
|---|---|---|
| Age | ||
| 20–39 | 3514 | 22.64 |
| 40–59 | 6015 | 39.23 |
| 60–79 | 7232 | 30.89 |
| 80+ | 1970 | 7.24 |
| Gender | ||
| Male | 8251 | 42.3 |
| Female | 10,480 | 57.7 |
| Ethnicity | ||
| Hispanic | 3772 | 8.74 |
| Non-Hispanic White | 9464 | 75.34 |
| Non-Hispanic Black | 4000 | 10.16 |
| Other Race | 1495 | 5.76 |
| Income | ||
| <45,000 | 7182 | 56.18 |
| ≥45,000 | 9517 | 43.82 |
| Missing | 2032 | |
| Economic Status | ||
| Above Poverty Line | 13,851 | 87.73 |
| In Poverty | 3365 | 12.27 |
| Missing | 1515 | |
| Education | ||
| Less than High School | 4801 | 15.94 |
| High School Graduate | 9652 | 54.05 |
| College Graduate | 4255 | 30.02 |
| Missing | 23 | |
| Marital Status | ||
| Married/Living with Partner | 11,009 | 63.92 |
| Not Married | 7712 | 36.08 |
| Missing | 10 | |
| Citizenship | ||
| U.S. citizen | 17,243 | 95.65 |
| Non-U.S. Citizen | 1472 | 4.35 |
| Missing | 16 |
| PD | No PD | p-Value | |||
|---|---|---|---|---|---|
| (n = 418, 2.22%) | (n = 18,313, 97.78%) | ||||
| Unweighted N | Weighted % | Unweighted N | Weighted % | ||
| PHQ-9 ≥ 10 | <0.0001 | ||||
| Yes | 108 | 26.46 | 1852 | 9.58 | |
| No | 260 | 73.54 | 14,748 | 90.42 | |
| Age | <0.0001 | ||||
| 20–39 | 54 | 15.75 | 3460 | 22.8 | |
| 40–59 | 153 | 43.7 | 5862 | 39.13 | |
| 60–79 | 129 | 26.04 | 7103 | 30.99 | |
| 80+ | 82 | 14.51 | 1888 | 7.08 | |
| Gender | 0.0207 | ||||
| Male | 170 | 34.9 | 8081 | 42.47 | |
| Female | 248 | 65.1 | 10,232 | 57.53 | |
| Ethnicity | 0.0077 | ||||
| Hispanic | 62 | 6.03 | 3710 | 8.8 | |
| Non-Hispanic White | 275 | 81.98 | 9189 | 75.19 | |
| Non-Hispanic Black | 60 | 7.8 | 3940 | 10.21 | |
| Other Race | 21 | 4.19 | 1474 | 5.8 | |
| Income | <0.0001 | ||||
| <45,000 | 105 | 41.19 | 7077 | 56.52 | |
| ≥45,000 | 260 | 58.81 | 9257 | 43.48 | |
| Missing | 53 | 1979 | |||
| Economic Status | <0.0001 | ||||
| Above Poverty Line | 271 | 79.05 | 13,580 | 87.92 | |
| In Poverty | 107 | 20.95 | 3258 | 12.08 | |
| Missing | 40 | 1475 | |||
| Education | 0.0004 | ||||
| Less than High School | 129 | 22.67 | 4672 | 15.79 | |
| High School Graduate | 219 | 56.61 | 9433 | 53.99 | |
| College Graduate | 69 | 20.73 | 4186 | 30.23 | |
| Missing | 1 | 22 | |||
| Marital Status | 0.001 | ||||
| Married/Living with Partner | 208 | 54.84 | 10,801 | 64.13 | |
| Not Married | 209 | 45.16 | 7503 | 35.87 | |
| Missing | 1 | 9 | |||
| Citizenship | 0.0017 | ||||
| U.S. citizen | 401 | 97.99 | 16,842 | 95.6 | |
| Non-U.S. Citizen | 17 | 2.01 | 1455 | 4.4 | |
| Missing | 0 | 16 | |||
| Overall | PD Status | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| (n = 108, 5.75%) | (n = 1852, 94.25%) | ||||||
| Unweighted N | Weighted % | Unweighted N | Weighted % | Unweighted N | Weighted % | ||
| Depression Management by Medication or Mental Health Encounter | <0.0001 | ||||||
| Yes | 977 | 54.97 | 87 | 85.12 | 890 | 53.13 | |
| No | 983 | 45.03 | 21 | 14.88 | 962 | 46.87 | |
| Depression Managed by Medication | 0.0002 | ||||||
| Yes | 723 | 42.51 | 63 | 62.42 | 660 | 41.3 | |
| No | 1237 | 57.49 | 45 | 37.58 | 1192 | 58.7 | |
| Limited Physical Function Due to Emotional Problem | 0.0052 | ||||||
| Yes | 163 | 9.18 | 17 | 15.9 | 146 | 8.77 | |
| No | 1738 | 90.82 | 86 | 84.1 | 1652 | 91.23 | |
| Missing | 59 | 5 | |||||
| Consulted Mental Health Provider in Last 12 months | <0.0001 | ||||||
| Yes | 599 | 32.51 | 68 | 67.71 | 531 | 30.36 | |
| No | 1360 | 67.49 | 40 | 32.29 | 1320 | 69.64 | |
| Missing | 1 | 0 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
DeMarco, E.C.; Al-Hammadi, N.; Hinyard, L. Exploring Treatment for Depression in Parkinson’s Patients: A Cross-Sectional Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8596. https://doi.org/10.3390/ijerph18168596
DeMarco EC, Al-Hammadi N, Hinyard L. Exploring Treatment for Depression in Parkinson’s Patients: A Cross-Sectional Analysis. International Journal of Environmental Research and Public Health. 2021; 18(16):8596. https://doi.org/10.3390/ijerph18168596
Chicago/Turabian StyleDeMarco, Elisabeth C., Noor Al-Hammadi, and Leslie Hinyard. 2021. "Exploring Treatment for Depression in Parkinson’s Patients: A Cross-Sectional Analysis" International Journal of Environmental Research and Public Health 18, no. 16: 8596. https://doi.org/10.3390/ijerph18168596
APA StyleDeMarco, E. C., Al-Hammadi, N., & Hinyard, L. (2021). Exploring Treatment for Depression in Parkinson’s Patients: A Cross-Sectional Analysis. International Journal of Environmental Research and Public Health, 18(16), 8596. https://doi.org/10.3390/ijerph18168596






