A Cross-Sectional Analysis of the Association between Domestic Cooking Energy Source Type and Respiratory Infections among Children Aged under Five Years: Evidence from Demographic and Household Surveys in 37 Low-Middle Income Countries
Abstract
:1. Introduction
2. Materials and Methods
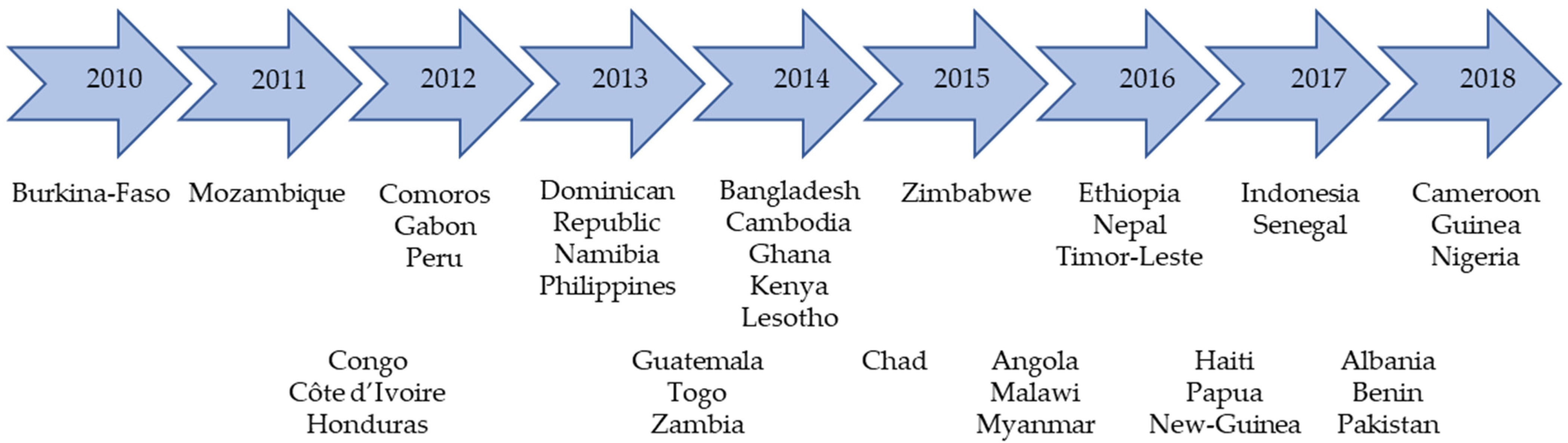
2.1. Setting and Study Design
2.2. Ethical Approval and Authorisation
2.3. Data Variables
2.3.1. Outcome/Dependent Variables
2.3.2. Exposure/Independent Variables
2.3.3. Child, Maternal and Paternal Characteristics
2.3.4. Household and Contextual Characteristics
2.4. Data Analysis
3. Results
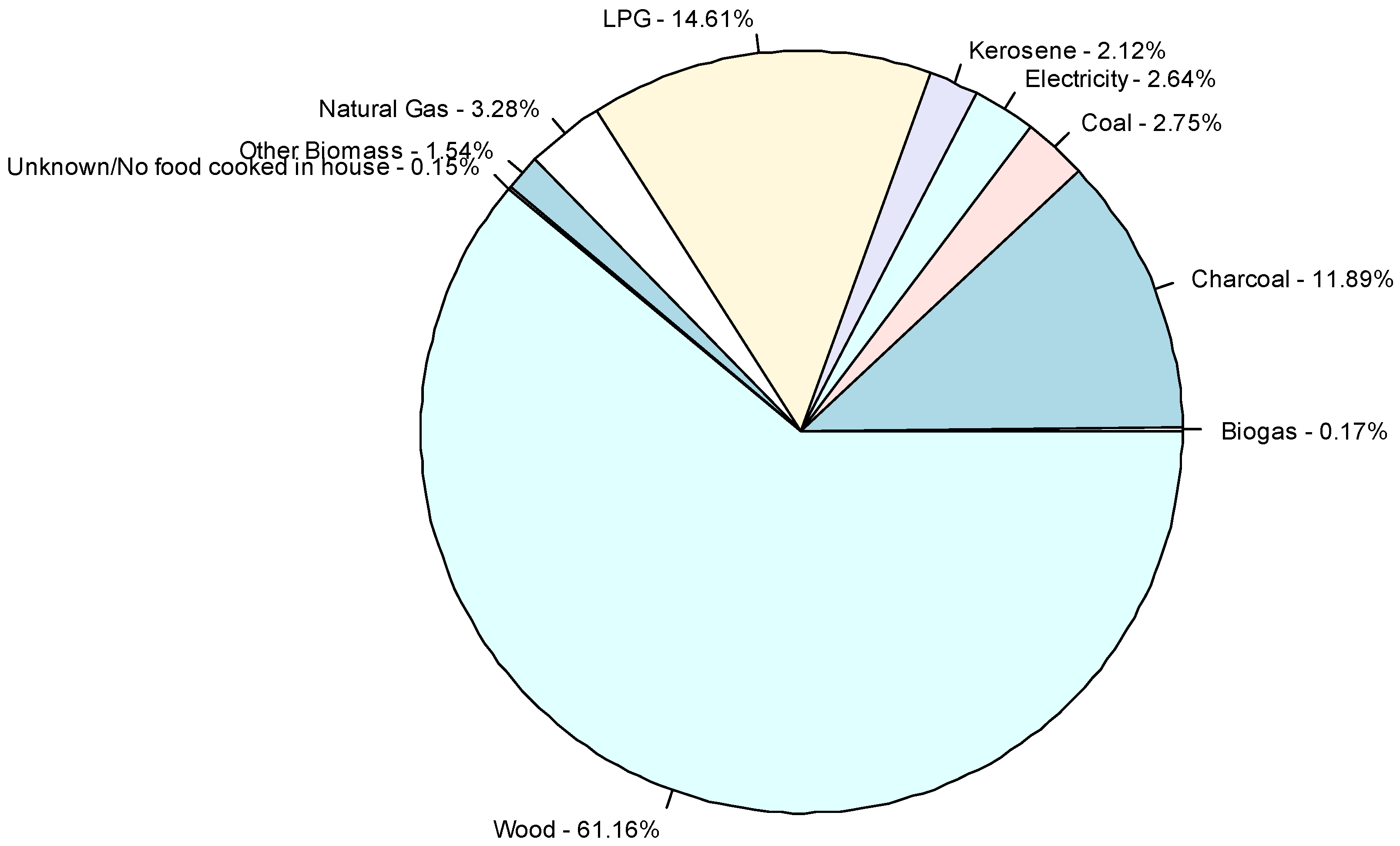
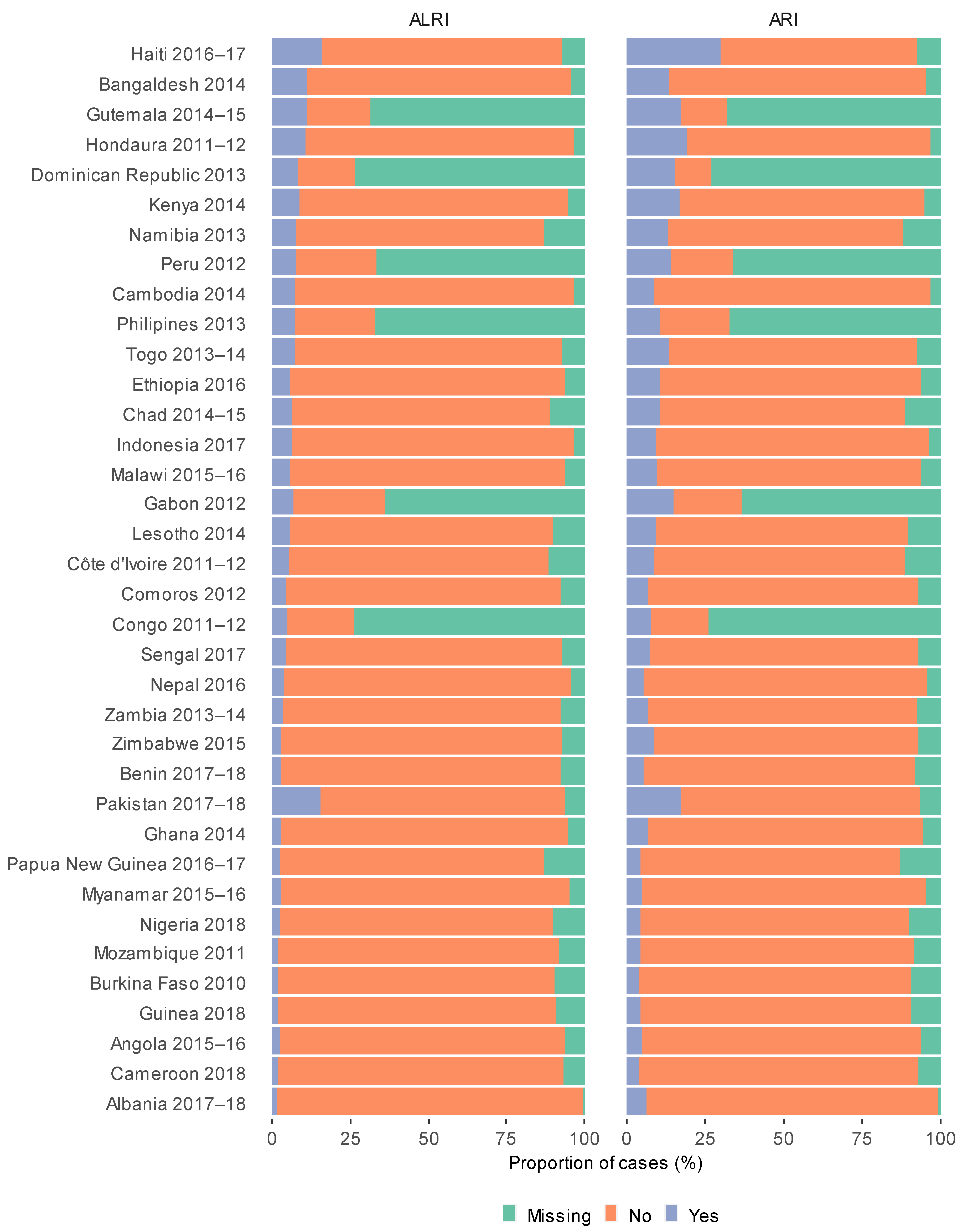
3.1. Descriptive Analysis
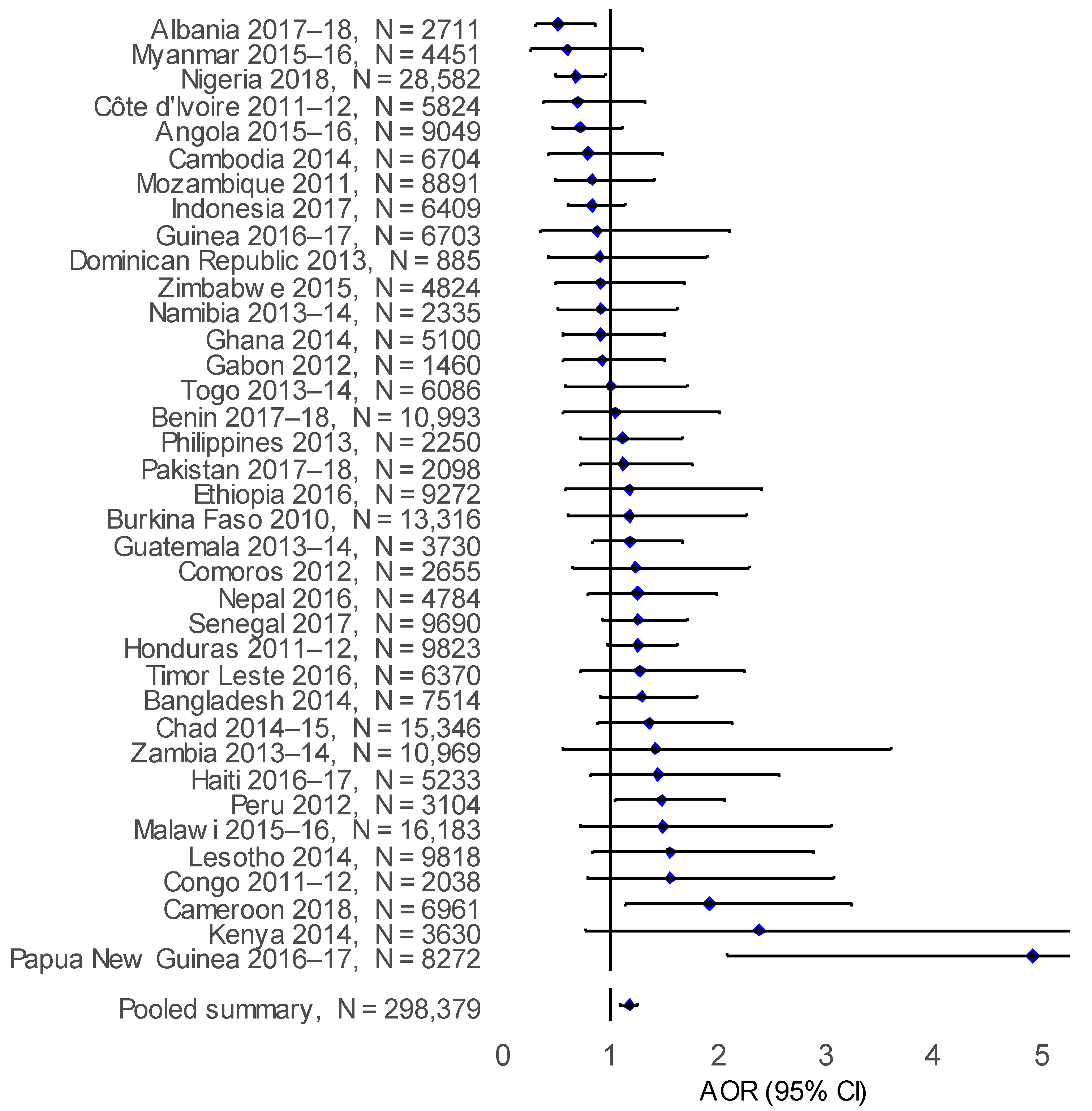
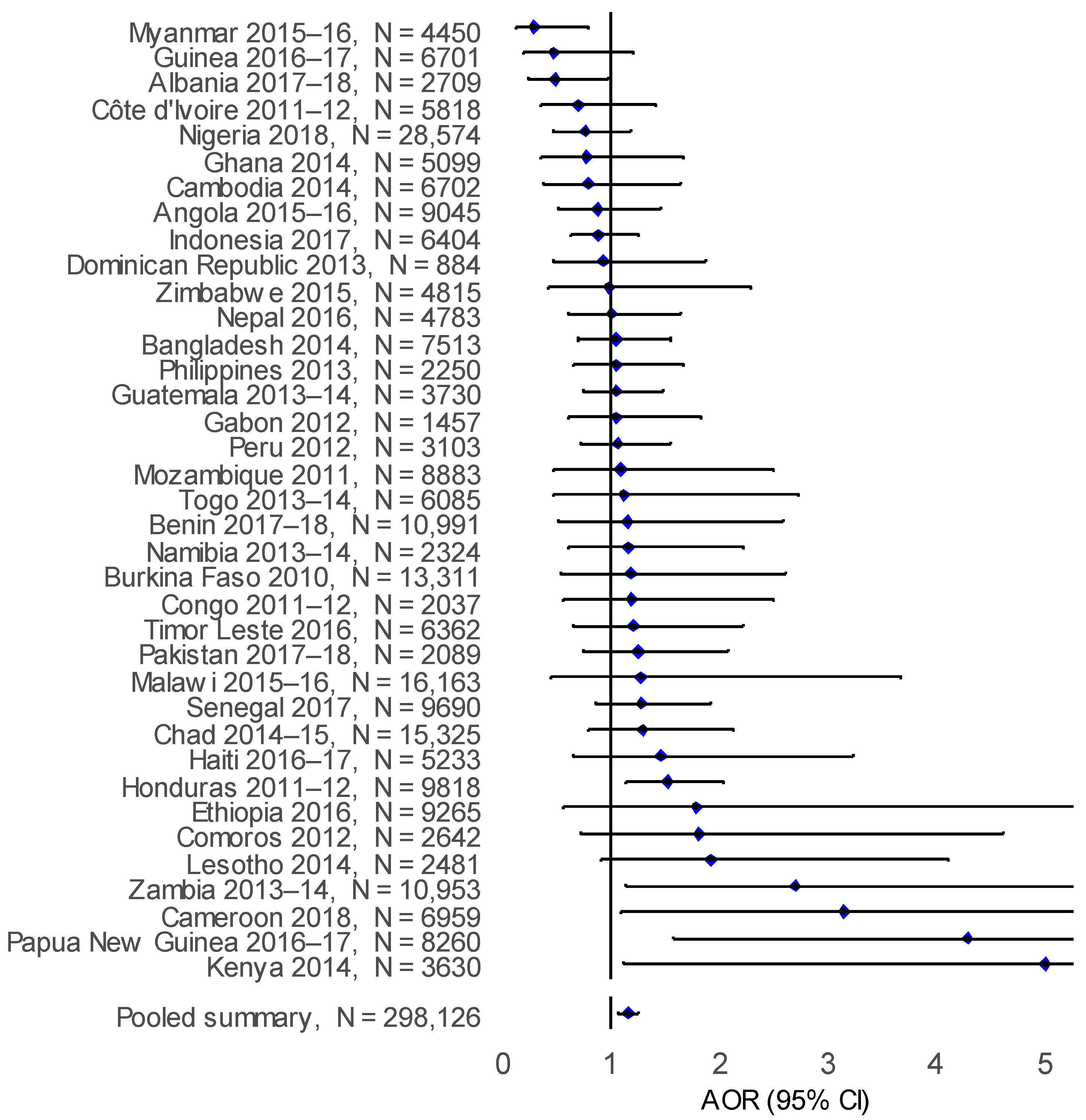
3.2. Risk of ARI and ALRI in Children under Five
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| ARI | ALRI | |||
|---|---|---|---|---|
| OR (95%CI) | p Value | OR (95%CI) | p Value | |
| Cooking energy source (Kerosene categorised as biomass energy source) | ||||
| Clean | Ref. | Ref. | ||
| Biomass | 0.85 (0.80–0.90) | <0.001 | 0.90 (0.85–0.96) | 0.001 |
| Cooking energy source (Kerosene categorised as clean energy source) | ||||
| Clean | Ref. | Ref. | ||
| Biomass | 0.89 (0.84–0.94) | <0.001 | 0.95 (0.89–1.00) | 0.067 |
| Child age (years) | ||||
| <1 | 0.92 (0.88–0.96) | <0.001 | 0.83 (0.79–0.87) | <0.001 |
| 1 | Ref. | Ref. | ||
| 2 | 0.85 (0.81–0.88) | <0.001 | 0.79 (0.75–0.83) | <0.001 |
| 3 | 0.73 (0.69–0.76) | <0.001 | 0.65 (0.61–0.68) | <0.001 |
| 4 | 0.62 (0.59–0.65) | <0.001 | 0.54 (0.51–0.57) | <0.001 |
| Sex of child | ||||
| Female | Ref. | Ref. | ||
| Male | 1.05 (1.02–1.08) | 0.001 | 1.06 (1.02–1.09) | 0.003 |
| Mode of delivery | ||||
| Vaginal | Ref. | Ref. | ||
| Caesarean | 1.66 (1.57–1.76) | <0.001 | 1.56 (1.46–1.67) | <0.001 |
| Breastfeeding status | ||||
| Ever breast fed | Ref. | Ref. | ||
| Never breast fed | 0.97 (0.87–1.07) | 0.528 | 1.56 (1.46–1.67) | <0.001 |
| Maternal age (Years) | ||||
| 15–24 | Ref. | Ref. | ||
| 25–35 | 0.83 (0.80–0.86) | <0.001 | 1.67 (1.58–1.77) | <0.001 |
| 36–49 | 0.78 (0.75–0.82) | <0.001 | 1.50 (1.41–1.60) | <0.001 |
| Maternal level of education | ||||
| No education | Ref. | Ref. | ||
| Primary | 1.77 (1.68–1.85) | <0.001 | 1.67 (1.58–1.77) | <0.001 |
| Secondary or Higher | 1.63 (1.54–1.72) | <0.001 | 1.50 (1.41–1.60) | <0.001 |
| Household wealth index | ||||
| Lowest | Ref. | Ref. | ||
| Low | 0.98 (0.93–1.03) | 0.403 | 0.94 (0.89–1.00) | 0.044 |
| Middle | 0.96 (0.90–1.01) | 0.131 | 0.91 (0.85–0.97) | 0.003 |
| High | 0.87 (0.82–0.93) | <0.00 | 0.80 (0.75–0.86) | <0.001 |
| Highest | 0.78 (0.73–0.84) | <0.001 | 0.70 (0.65–0.75) | <0.001 |
| Place of residence | ||||
| Rural | Ref. | Ref. | ||
| Urban | 1.05 (1.00–1.10) | 0.065 | 0.98 (0.93–1.04) | 0.526 |
| Household smoking | ||||
| No | Ref. | Ref. | ||
| Yes | 1.03 (0.99–1.08) | 0.132 | 1.15 (1.09–1.21) | <0.001 |
| Number of households members | ||||
| ≤6 | Ref. | Ref. | ||
| ≥6 | 0.88 (0.85–0.92) | <0.001 | 0.90 (0.86–0.94) | <0.001 |
| Cooking location | ||||
| Indoors | Ref. | Ref. | ||
| Outdoors | 0.77 (0.74–0.81) | <0.001 | 0.79 (0.75–0.83) | <0.001 |
| Paternal level of education | ||||
| No education | Ref. | Ref. | ||
| Primary | 1.84 (1.74–1.95 | <0.001 | 1.78 (1.67–1.90) | <0.001 |
| Secondary or Higher | 1.63 (1.54–1.73) | <0.001 | 1.55 (1.45–1.65) | <0.001 |
| Analysis (N) | ARI | ALRI | ||
|---|---|---|---|---|
| AOR (95%CI) | p Value | AOR (95%CI) | p Value | |
| Exploratory analyses | ||||
| Controlling for breastfeeding a (n = 255,588) | 1.14 (1.07–1.23) | <0.001 | 1.16 (1.07–1.26) | 0.001 |
| Controlling for household’s smoking b (n = 272,852) | 1.13 (1.06–1.22) | 0.001 | 1.13 (1.04–1.24) | 0.005 |
| Controlling for husband’s education c (n = 179,330) | 1.13 (1.06–1.22) | 0.001 | 1.13 (1.04–1.23) | 0.003 |
| ARI | ALRI | |||
|---|---|---|---|---|
| AOR (95%CI) | p Value | AOR (95%CI) | p Value | |
| N = 298,379 | N = 298,126 | |||
| Cooking energy source | ||||
| Clean | Ref. | Ref. | ||
| Biomass | 1.20 (1.12–1.27) | <0.001 | 1.19 (1.10–1.28) | <0.001 |
| Child age (years) | ||||
| <1 | 0.95 (0.91–0.99) | 0.024 | 0.86 (0.81–0.91) | <0.001 |
| 1 | Ref. | Ref. | ||
| 2 | 0.84 (0.81–0.88) | <0.001 | 0.79 (0.75–0.84) | <0.001 |
| 3 | 0.74 (0.71–0.78) | <0.001 | 0.66 (0.62–0.70) | <0.001 |
| 4 | 0.64 (0.61–0.67) | <0.001 | 0.56 (0.52–0.59) | <0.001 |
| Sex of child | ||||
| Female | Ref. | Ref. | ||
| Male | 0.74 (0.71–0.78) | <0.001 | 0.66 (0.62–0.70) | <0.001 |
| Mode of delivery | ||||
| Vaginal | Ref. | Ref. | ||
| Caesarean | 1.08 (1.01–1.14) | 0.018 | 1.02 (0.95–1.09) | 0.646 |
| Maternal age (Years) | ||||
| 15–24 | ||||
| 25–35 | 0.95 (0.92–0.99) | 0.011 | 0.99 (0.95–1.04) | 0.719 |
| 36–49 | 0.93 (0.89–0.98) | 0.009 | 0.98 (0.92–1.05) | 0.59 |
| Maternal level of education | ||||
| No education | Ref. | Ref. | ||
| Primary | 1.22 (1.16–1.29) | <0.001 | 1.18 (1.11–1.26) | <0.001 |
| Secondary or Higher | 1.14 (1.07–1.21) | <0.001 | 1.07 (0.99–1.15) | 0.088 |
| Household wealth index | ||||
| Lowest | Ref. | Ref. | ||
| Low | 0.99 (0.94–1.04) | 0.657 | 0.95 (0.90–1.01) | 0.101 |
| Middle | 0.98 (0.93–1.04) | 0.577 | 0.94 (0.88–1.00) | 0.05 |
| High | 0.93 (0.87–0.99) | 0.031 | 0.87 (0.80–0.94) | <0.001 |
| Highest | 0.88 (0.81–0.95) | 0.001 | 0.79 (0.72–0.87) | <0.001 |
| Place of residence | ||||
| Rural | Ref. | Ref. | ||
| Urban | 0.99 (0.94–1.04) | 0.617 | 1.02 (0.96–1.08) | 0.537 |
| Number of households members | ||||
| ≤6 | ||||
| ≥6 | 0.98 (0.95–1.02) | 0.341 | 0.98 (0.93–1.02) | 0.295 |
| Cooking location | ||||
| Indoors | Ref. | Ref. | ||
| Outdoors | 0.97 (0.93–1.01) | 0.165 | 0.98 (0.93–1.04) | 0.528 |
| Sub-analysis * | ||||
| Urban areas only (n = 101,444) | 1.18 (1.08–1.29) | <0.001 | 1.17 (1.05–1.30) | 0.003 |
| Rural areas only (n = 196,682) | 1.17 (1.06–1.29) | 0.002 | 1.15 (1.02–1.29) | 0.024 |
References
- Sanbata, H.; Asfaw, A.; Kumie, A. Association of biomass fuel use with acute respiratory infections among under- five children in a slum urban of Addis Ababa, Ethiopia. BMC Public Health 2014, 14, 1122. [Google Scholar] [CrossRef] [Green Version]
- Woolley, K.E.; Bagambe, T.; Singh, A.; Avis, W.R.; Kabera, T.; Weldetinsae, A.; Mariga, S.T.; Kirenga, B.; Pope, F.D.; Neil Thomas, G.; et al. Investigating the association between wood and charcoal domestic cooking, respiratory symptoms and acute respiratory infections among children aged under 5 years in uganda: A cross-sectional analysis of the 2016 demographic and health survey. Int. J. Environ. Res. Public Health 2020, 17, 3974. [Google Scholar] [CrossRef]
- International Energy Agency. Share of Population Relying on Different Cooking Fuels in Selected Countries, 2015—Charts—Data & Statistics—IEA. Available online: https://www.iea.org/data-and-statistics/charts/share-of-population-relying-on-different-cooking-fuels-in-selected-countries-2015 (accessed on 22 September 2020).
- Okello, G.; Devereux, G.; Semple, S. Women and girls in resource poor countries experience much greater exposure to household air pollutants than men: Results from Uganda and Ethiopia. Environ. Int. 2018, 119, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Admasie, A.; Kumie, A.; Worku, A. Children under five from houses of unclean fuel sources and poorly ventilated houses have higher odds of suffering from acute respiratory infection in Wolaita-Sodo, Southern Ethiopia: A case-control study. J. Environ. Public Health 2018, 2018, 9320603. [Google Scholar] [CrossRef]
- Smith, K.R.; Samet, J.M.; Romieu, I.; Bruce, N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax 2000, 55, 518–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toman, M.; Bluffstone, R. Challenges in Assessing the Costs of Household Cooking Energy in Lower-Income Countries; World Bank Group Policy Research Working Paper; World Bank Group: Washington, DC, USA, 2017; Volume 25. [Google Scholar] [CrossRef]
- Taylor, E.T.; Nakai, S. The levels of toxic air pollutants in kitchens with traditional stoves in rural Sierra Leone. J. Environ. Prot. 2012, 3, 1353–1363. [Google Scholar] [CrossRef] [Green Version]
- Romieu, I.; Samet, J.M.; Smith, K.R.; Bruce, N. Outdoor air pollution and acute respiratory infections among children in developing countries. J. Occup. Environ. Med. 2002, 44, 640–649. [Google Scholar] [CrossRef]
- Bruce, N.; Pope, D.; Rehfuess, E.; Balakrishnan, K.; Adair-Rohani, H.; Dora, C. WHO indoor air quality guidelines on household fuel combustion: Strategy implications of new evidence on interventions and exposure-risk functions. Atmos. Environ. 2015, 106, 451–457. [Google Scholar] [CrossRef]
- Da Costa, J.L.; Navarro, A.; Neves, J.B.; Martin, M. Household wood and charcoal smoke increases risk of otitis media in childhood in Maputo. Int. J. Epidemiol. 2004, 33, 573–578. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Air Pollution and Child Health. Available online: https://www.who.int/news/item/29-10-2018-more-than-90-of-the-worlds-children-breathe-toxic-air-every-day (accessed on 2 March 2021).
- Bickton, F.M.; Ndeketa, L.; Sibande, G.T.; Nkeramahame, J.; Payesa, C.; Milanzi, E.B. Household air pollution and under-five mortality in sub-Saharan Africa: An analysis of 14 demographic and health surveys. Environ. Health Prev. Med. 2020, 25, 67. [Google Scholar] [CrossRef] [PubMed]
- Venkata Ramana, P.; Michael, T.; Sumi, M.; Kammila, S. The State of the Global Clean and Improved Cooking Sector; Energy Sector Management Assistance Program Technical Paper No. 007/15; World Bank: Washington, DC, USA, 2015. [Google Scholar]
- Woolley, K.E.; Dickinson-Craig, E.; Bartington, S.E.; Oludotun, T.; Kirenga, B.; Mariga, S.T.; Kabera, T.; Coombe, A.; Pope, F.D.; Singh, A.; et al. Effectiveness of interventions to reduce household air pollution from solid biomass fuels and improve maternal and child health outcomes in low- and middle-income countries: A systematic review protocol. Syst. Rev. 2021, 10, 33. [Google Scholar] [CrossRef]
- Quinn, A.K.; Bruce, N.; Puzzolo, E.; Dickinson, K.; Sturke, R.; Jack, D.W.; Mehta, S.; Shankar, A.; Sherr, K.; Rosenthal, J.P. An analysis of efforts to scale up clean household energy for cooking around the world. Energy Sustain. Dev. 2018, 46, 1–10. [Google Scholar] [CrossRef]
- World Bank Clean and Improved Cooking in Sub-Saharan Africa: A Landscape Report Africa Renewable Energy Access Program (AFREA). Available online: https://openknowledge.worldbank.org/handle/10986/22521 (accessed on 1 March 2021).
- Wright, L.L.; Eaton, L.M.; Perlack, R.D.; Stokes, B.J. Woody biomass. In Comprehensive Renewable Energy; Elsevier: Boston, MA, USA, 2012; Volume 5, pp. 263–291. ISBN 9780080878737. [Google Scholar]
- Simkovich, S.M.; Williams, K.N.; Pollard, S.; Dowdy, D.; Sinharoy, S.; Clasen, T.F.; Puzzolo, E.; Checkley, W. A systematic review to evaluate the association between clean cooking technologies and time use in low- and middle-income countries. Int. J. Environ. Res. Public Health 2019, 16, 2277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goel, K.; Sarta, J.A.; Gagan, A.; Parul, G.; Vijay, K. A cross-sectional study on prevalence of acute respiratory infections ARI in under five children of Meerut District India. J. Community Med. Health Educ. 2013, 2, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Mondal, D.; Paul, P. Effects of indoor pollution on acute respiratory infections among under-five children in India: Evidence from a nationally representative population-based study. PLoS ONE 2020, 15, e0237611. [Google Scholar] [CrossRef]
- Naz, L.; Ghimire, U. Assessing the prevalence trend of childhood pneumonia associated with indoor air pollution in Pakistan. Environ. Sci. Pollut. Res. 2020, 27, 44540–44551. [Google Scholar] [CrossRef]
- Buchner, H.; Rehfuess, E.A. Cooking and season as risk factors for acute lower respiratory infections in African children: A cross-sectional multi-country analysis. PLoS ONE 2015, 10, e0128933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tekle, A.G.; Worku, A.; Berhane, Y. Factors associated with acute respiratory infection in children under the age of 5 years: Evidence from the 2011 Ethiopia Demographic and Health Survey. Pediatr. Health Med. Ther. 2015, 6, 9. [Google Scholar] [CrossRef] [Green Version]
- DHS. The DHS Program—DHS Methodology. Available online: https://dhsprogram.com/methodology/survey-types/DHS-Methodology.cfm (accessed on 30 June 2021).
- The Demographic and Health Surveys. The DHS Program—Available Datasets. Available online: https://dhsprogram.com/data/available-datasets.cfm (accessed on 28 February 2021).
- The Demographic and Health Surveys. The DHS Program: Protecting the Privacy of DHS Survey Respondents. Available online: https://dhsprogram.com/What-We-Do/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm (accessed on 5 March 2020).
- World Health Organization. WHO|RSV Surveillance Case Definitions. Available online: https://www.who.int/teams/global-influenza-programme/global-respiratory-syncytial-virus-surveillance/case-definitions (accessed on 6 July 2021).
- World Health Organization. Household Energy Use: DRAFT Catalogue of Cooking, Heating and Lighting Fuels and Technologies. Available online: https://mics.unicef.org/files?job=W1siZiIsIjIwMTcvMDIvMDMvMTYvMjcvMjUvNTk5L1BpY3RvcmlhbHNfV0hPX0hvdXNlaG9sZF9FbmVyZ3lfVXNlX0NhdGFsb2d1ZV9TZXB0ZW1iZXJfMjAxNl8ucGRmIl1d&sha=57b4a452fcc0ac88 (accessed on 30 June 2021).
- The Demographic and Health Surveys. The DHS Program—Research Topics—Wealth Index. Available online: https://dhsprogram.com/topics/wealth-index/index.cfm (accessed on 1 March 2021).
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Boston, MA, USA, 2020. [Google Scholar]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2019. [Google Scholar]
- International Energy Agency; International Renewable Energy Agency; United Nations; World Bank Group; World Health Organization. Access to clean fuels and technologies for cooking. In Tracking SDG7: The Energy Progress Report 2018; World Bank: Washington, DC, USA, 2018; pp. 40–55. [Google Scholar]
- Zhang, Y.; Li, Z. COVID-19′s Impact on the Transition to clean Cooking Fuels: Initial Findings from a Case Study in Rural Kenya. Available online: https://openknowledge.worldbank.org/handle/10986/35258 (accessed on 30 June 2021).
- Shupler, M.; Mwitari, J.; Gohole, A.; Anderson de Cuevas, R.; Puzzolo, E.; Čukić, I.; Nix, E.; Pope, D. COVID-19 impacts on household energy & food security in a Kenyan informal settlement: The need for integrated approaches to the SDGs. Renew. Sustain. Energy Rev. 2021, 144, 111018. [Google Scholar] [CrossRef]
- Von Schirnding, Y.; Bruce, N.; Smith, K.; Ballard-Tremeer, G.; Ezzati, M.; Lvovsky, K. Addressing the Impact of Household Energy and Indoor Air Pollution on the Health of the Poor: Implications for Policy Action; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Khalequzzaman, M.; Kamijima, M.; Sakai, K.; Ebara, T.; Hoque, B.A.; Nakajima, T. Indoor air pollution and health of children in biomass fuel-using households of Bangladesh: Comparison between urban and rural areas. Environ. Health Prev. Med. 2011, 16, 375–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiedinmyer, C.; Dickinson, K.; Piedrahita, R.; Kanyomse, E.; Coffey, E.; Hannigan, M.; Alirigia, R.; Oduro, A. Rural-urban differences in cooking practices and exposures in Northern Ghana. Environ. Res. Lett. 2017, 12, 065009. [Google Scholar] [CrossRef]
- Barnes, B.; Mathee, A.; Moiloa, K. Assessing child time—Activity patterns in relation to indoor cooking fires in developing countries: A methodological comparison. Int. J. Hyg. Environ. Health 2005, 208, 219–225. [Google Scholar] [CrossRef]
- Ezzati, M.; Kammen, D.M. Indoor air pollution from biomass combustion and acute respiratory infections in Kenya: An exposure-response study. Lancet 2001, 358, 619–624. [Google Scholar] [CrossRef]
- Pope, D.; Bruce, N.; Dherani, M.; Jagoe, K.; Rehfuess, E. Real-life effectiveness of ‘improved’ stoves and clean fuels in reducing PM2.5 and CO: Systematic review and meta-analysis. Environ. Int. 2017, 101, 7–18. [Google Scholar] [CrossRef]
- Weaver, A.M.; Gurley, E.S.; Crabtree-Ide, C.; Salje, H.; Yoo, E.H.; Mu, L.; Akter, N.; Ram, P.K. Air pollution dispersion from biomass stoves to neighboring homes in Mirpur, Dhaka, Bangladesh. BMC Public Health 2019, 19, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Smith, K.R.; Pillarisetti, A. Household air pollution from solid cookfuels and its effects on health. In Disease Control Priorities: Injury Prevention and Environmental Health, 3rd ed.; The World Bank: Washington, DC, USA, 2017; Volume 7, pp. 133–152. ISBN 9781464805226. [Google Scholar]
- Taylor, E.T.; Nakai, S. Prevalence of acute respiratory infections in women and children in western sierra leone due to smoke from wood and charcoal stoves. Int. J. Environ. Res. Public Health 2012, 9, 2252–2265. [Google Scholar] [CrossRef] [Green Version]
- Mishra, V.; Smith, K.R.; Retherford, R.D. Effects of cooking smoke and environmental tobacco smoke on acute respiratory infections in young Indian children. Popul. Environ. 2005, 26, 375–396. [Google Scholar] [CrossRef]
- Alemayehu, M.; Alemu, K.; Sharma, H.R.; Gizaw, Z.; Shibru, A. Household fuel use and acute respiratory infections in children under five years of age in Gondar city of Ethiopia. J. Environ. Earth Sci. 2014, 4, 77–85. [Google Scholar]
- Mishra, V. Indoor air pollution from biomass combustion and acute respiratory illness in preschool age children in Zimbabwe. Int. J. Epidemiol. 2003, 32, 847–853. [Google Scholar] [CrossRef] [Green Version]
- Enyew, H.D.; Mereta, S.T.; Hailu, A.B. Biomass fuel use and acute respiratory infection among children younger than 5 years in Ethiopia: A systematic review and meta-analysis. Public Health 2021, 193, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Dherani, M.; Pope, D.; Mascarenhas, M.; Smith, K.R.; Weber, M.; Bruce, N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: A systematic review and meta-analysis. Bull. World Health Organ. 2008, 86, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Odo, D.B.; Yang, I.A.; Knibbs, L.D. A systematic review and appraisal of epidemiological studies on household fuel use and its health effects using demographic and health surveys. Int. J. Environ. Res. Public Health 2021, 18, 1411. [Google Scholar] [CrossRef] [PubMed]
- Alam, A.; Tawale, N.; Patel, A.; Dibley, M.J.; Jadhao, S.; Raynes-Greenow, C. Household air pollution intervention implications: Findings from qualitative studies and a field trial of clean cookstoves in two rural villages in India. Int. J. Environ. Res. Public Health 2016, 13, 893. [Google Scholar] [CrossRef] [PubMed]
- Havens, D.; Wang, D.; Grigg, J.; Gordon, S.B.; Balmes, J.; Mortimer, K. The cooking and pneumonia study (CAPS) in Malawi: A cross-sectional assessment of carbon monoxide exposure and carboxyhemoglobin levels in children under 5 years old. Int. J. Environ. Res. Public Health 2018, 15, 1936. [Google Scholar] [CrossRef] [Green Version]
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K. bong H.; Mortimer, K.; Asante, K.P.; Balakrishnan, K.; Balmes, J.; et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef] [Green Version]
- Arnold, F.; Khan, S.M. Perspectives and implications of the Improving Coverage Measurement Core Group’s validation studies for household surveys. J. Glob. Health 2018, 8, 010606. [Google Scholar] [CrossRef]
- Croft, N.T.; Marshall, A.M.J.; Allen, C.K. Guide to DHS Statistics (Version 2); ICF International: Rockville, MD, USA, 2018. [Google Scholar]

| ARI N = 299,118 | ALRI N = 298,841 | |||||
|---|---|---|---|---|---|---|
| Explanatory Variables | Yes N = 32,438 (10.8%) | No N = 266,679 (89.2%) | p Value | Yes N = 19,426 (6.5%) | No N = 279,415 (93.5%) | p Value |
| Cooking energy source | 0.012 | 0.081 | ||||
| Clean | 6547 (20.2%) | 47,187 (17.7%) | 3770 (19.4%) | 49,921 (17.9%) | ||
| Biomass | 25,824 (79.8%) | 219,015 (82.3%) | 15,615 (80.6%) | 228,992 (82.1%) | ||
| Missing | 67 | 477 | 41 | 502 | ||
| Child age (years) | <0.001 | <0.001 | ||||
| <1 | 7572 (23.3%) | 55,614 (20.9%) | 4441 (22.9%) | 58,720 (21.0%) | ||
| 1 | 7873 (24.3%) | 53,320 (20.0%) | 5102 (26.3%) | 56,039 (20.1%) | ||
| 2 | 6476 (20.0%) | 51,828 (19.4%) | 3913 (20.1%) | 54,349 (19.5%) | ||
| 3 | 5682 (17.5%) | 53,057 (19.9%) | 3266 (16.8%) | 55,397 (19.8%) | ||
| 4 | 4835 (14.9%) | 52,860 (19.8%) | 2703 (13.9%) | 54,910 (19.7%) | ||
| Sex of child | <0.001 | <0.001 | ||||
| Male | 16,811 (51.8%) | 134,922 (50.6%) | 10,099 (52.0%) | 141,489 (50.6%) | ||
| Female | 15,627 (48.2%) | 131,757 (49.4%) | 9327 (48.0%) | 137,926 (49.4%) | ||
| Mode of delivery | <0.001 | <0.001 | ||||
| Vaginal | 28,437 (88.9%) | 244,809 (93.0%) | 17,000 (89.2%) | 255,981 (92.8%) | ||
| Caesarean | 3557 (11.1%) | 18,436 (7.0%) | 2065 (10.8%) | 19,917 (7.2%) | ||
| Missing | 444 | 3435 | 362 | 3517 | ||
| Breastfeeding status | <0.001 | <0.001 | ||||
| Ever breast fed | 25,602 (96.4%) | 219,737 (96.3%) | 15,390 (96.1%) | 229,736 (96.3%) | ||
| Never breast fed | 953 (3.6%) | 8461 (3.7%) | 620 (3.9%) | 8782 (3.7%) | ||
| Missing | 5883 | 38,481 | 3416 | 40,896 | ||
| Maternal age (Years) | <0.001 | <0.001 | ||||
| 15–24 | 10,545 (32.5%) | 75,517 (28.3%) | 6260 (32.2%) | 79,685 (28.5%) | ||
| 25–35 | 16,650 (51.3%) | 143,162 (53.7%) | 10,014 (51.5%) | 149,672 (53.6%) | ||
| 36–49 | 5244 (16.2%) | 48,001 (18.0%) | 3152 (16.2%) | 50,057 (17.9%) | ||
| Maternal level of education | <0.001 | <0.001 | ||||
| No education | 7686 (23.7%) | 92,024 (34.5%) | 4751 (24.5%) | 94,882 (34.0%) | ||
| Primary | 13,026 (40.2%) | 88,356 (33.1%) | 7825 (40.3%) | 93,467 (33.5%) | ||
| Secondary or Higher | 11,726 (36.1%) | 86,272 (32.4%) | 6851 (35.3%) | 91,038 (32.6%) | ||
| Missing | 0 | 29 | 0 | 29 | ||
| Household wealth index | <0.001 | <0.001 | ||||
| Lowest | 7902 (24.4%) | 60,168 (22.6%) | 4977 (25.6%) | 63,041 (22.6%) | ||
| Low | 7335 (22.6%) | 57,061 (21.4%) | 4446 (22.9%) | 59,886 (21.4%) | ||
| Middle | 6744 (20.8%) | 53,640 (20.1%) | 4029 (20.7%) | 56,295 (20.1%) | ||
| High | 5850 (18.0%) | 50,981 (19.1%) | 3391 (17.5%) | 53,379 (19.1%) | ||
| Highest | 4607 (14.2%) | 44,829 (16.8%) | 2582 (13.3%) | 46,814 (16.8%) | ||
| Place of residence | <0.001 | <0.001 | ||||
| Urban | 11,387 (35.1%) | 90,829 (34.1%) | 6565 (33.8%) | 95,551 (34.2%) | ||
| Rural | 21,051 (64.9%) | 175,850 (65.9%) | 12,861 (66.2%) | 183,864 (65.8%) | ||
| Household smoking | ||||||
| No | 18,370 (73.7%) | 182,328 (74.0%) | 10,514 (71.8%) | 189,978 (74.1%) | ||
| Yes | 6561 (26.3%) | 63,968 (26.0%) | 4135 (28.2%) | 66,340 (25.9%) | ||
| Missing | 7507 | 20,384 | 4777 | 23,098 | ||
| Number of households members | <0.001 | <0.001 | ||||
| ≤6 | 19,835 (61.2%) | 155,110 (58.2%) | 11,834 (60.9%) | 162,905 (58.3%) | ||
| ≥6 | 12,592 (38.8%) | 111,369 (41.8%) | 7586 (39.1%) | 116,305 (41.7%) | ||
| Missing | 11 | 201 | 6 | 205 | ||
| Cooking location | <0.001 | <0.001 | ||||
| Indoors | 24,520 (75.8%) | 188,269 (70.8%) | 14,657 (75.7%) | 197,942 (71.0%) | ||
| Outdoors | 7826 (24.2%) | 77,651 (29.2%) | 4702 (24.3%) | 80,690 (29.0%) | ||
| Missing | 92 | 759 | 67 | 783 | ||
| Paternal level of education | <0.001 | <0.001 | ||||
| No education | 5692 (20.4%) | 71,767 (30.7%) | 3505 (20.8%) | 73,897 (30.2%) | ||
| Primary | 10,201 (36.6%) | 69,809 (29.9%) | 6226 (37.0%) | 73,718 (30.1%) | ||
| Secondary or Higher | 11,946 (42.9%) | 92,192 (39.4%) | 7110 (42.2%) | 96,957 (39.6%) | ||
| Missing | 4599 | 32,911 | 2585 | 34,844 | ||
| ARI (N = 298,379) | ALRI (N = 298,126) | |||
|---|---|---|---|---|
| AOR (95%CI) | p Value | AOR (95%CI) | p Value | |
| Cooking energy source | ||||
| Clean | Ref. | Ref. | ||
| Biomass | 1.17 (1.09–1.25) | <0.001 | 1.16 (1.07–1.25) | <0.001 |
| Child age (years) | ||||
| <1 | 0.95 (0.91–0.99) | 0.024 | 0.86 (0.82–0.91) | <0.001 |
| 1 | Ref. | Ref. | ||
| 2 | 0.85 (0.81–0.88) | <0.001 | 0.79 (0.75–0.84) | <0.001 |
| 3 | 0.74 (0.71–0.78) | <0.001 | 0.66 (0.62–0.70) | <0.001 |
| 4 | 0.64 (0.61–0.67) | <0.001 | 0.56 (0.52–0.59) | <0.001 |
| Sex of child | ||||
| Female | Ref. | Ref. | ||
| Male | 1.05 (1.02–1.09) | 0.001 | 1.06 (1.02–1.10) | 0.002 |
| Mode of delivery | ||||
| Vaginal | Ref. | Ref. | ||
| Caesarean | 1.07 (1.01–1.14) | 0.02 | 1.02 (0.94–1.09) | 0.67 |
| Maternal age (Years) | ||||
| 15–24 | Ref. | Ref. | ||
| 25–35 | 0.95 (0.92–0.99) | 0.011 | 0.99 (0.95–1.04) | 0.703 |
| 36–49 | 0.93 (0.89–0.98) | 0.009 | 0.98 (0.92–1.05) | 0.585 |
| Maternal level of education | ||||
| No education | Ref. | Ref. | ||
| Primary | 1.22 (1.15–1.28) | <0.001 | 1.18 (1.11–1.26) | <0.001 |
| Secondary or Higher | 1.13 (1.07–1.20) | <0.001 | 1.06 (0.99–1.14) | 0.103 |
| Household wealth index | ||||
| Lowest | Ref. | Ref. | ||
| Low | 0.99 (0.94–1.04) | 0.624 | 0.95 (0.90–1.01) | 0.091 |
| Middle | 0.98 (0.93–1.04) | 0.509 | 0.93 (0.87–1.00) | 0.04 |
| High | 0.92 (0.87–0.99) | 0.018 | 0.86 (0.80–0.93) | <0.001 |
| Highest | 0.87 (0.80–0.94) | 0.001 | 0.78 (0.71–0.86) | <0.001 |
| Place of residence | ||||
| Rural | Ref. | Ref. | ||
| Urban | 0.98 (0.93–1.03) | 0.387 | 1.01 (0.95–1.07) | 0.755 |
| Number of households members | ||||
| ≤6 | Ref. | Ref. | ||
| ≥6 | 0.99 (0.95–1.02) | 0.440 | 0.98 (0.94–1.02) | 0.367 |
| Cooking location | ||||
| Indoors | Ref. | Ref. | ||
| Outdoors | 0.97 (0.93–1.02) | 0.223 | 0.99 (0.93–1.04) | 0.629 |
| Analysis (N) | ARI | ALRI | ||
|---|---|---|---|---|
| AOR (95%CI) | p Value | AOR (95%CI) | p Value | |
| Sub-analysis | ||||
| Urban areas only (n = 101,444) | 1.16 (1.06–1.28) | 0.001 | 1.14 (1.02–1.27) | 0.018 |
| Rural areas only (n = 196,682) | 1.14 (1.03–1.26) | 0.010 | 1.13 (1.00–1.27) | 0.051 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Janabi, Z.; Woolley, K.E.; Thomas, G.N.; Bartington, S.E. A Cross-Sectional Analysis of the Association between Domestic Cooking Energy Source Type and Respiratory Infections among Children Aged under Five Years: Evidence from Demographic and Household Surveys in 37 Low-Middle Income Countries. Int. J. Environ. Res. Public Health 2021, 18, 8516. https://doi.org/10.3390/ijerph18168516
Al-Janabi Z, Woolley KE, Thomas GN, Bartington SE. A Cross-Sectional Analysis of the Association between Domestic Cooking Energy Source Type and Respiratory Infections among Children Aged under Five Years: Evidence from Demographic and Household Surveys in 37 Low-Middle Income Countries. International Journal of Environmental Research and Public Health. 2021; 18(16):8516. https://doi.org/10.3390/ijerph18168516
Chicago/Turabian StyleAl-Janabi, Zubaidah, Katherine E. Woolley, G. Neil Thomas, and Suzanne E. Bartington. 2021. "A Cross-Sectional Analysis of the Association between Domestic Cooking Energy Source Type and Respiratory Infections among Children Aged under Five Years: Evidence from Demographic and Household Surveys in 37 Low-Middle Income Countries" International Journal of Environmental Research and Public Health 18, no. 16: 8516. https://doi.org/10.3390/ijerph18168516
APA StyleAl-Janabi, Z., Woolley, K. E., Thomas, G. N., & Bartington, S. E. (2021). A Cross-Sectional Analysis of the Association between Domestic Cooking Energy Source Type and Respiratory Infections among Children Aged under Five Years: Evidence from Demographic and Household Surveys in 37 Low-Middle Income Countries. International Journal of Environmental Research and Public Health, 18(16), 8516. https://doi.org/10.3390/ijerph18168516







