Understanding the Impacts of Novel Coronavirus Outbreaks on People Who Use Drugs: A Systematic Review to Inform Practice and Drug Policy Responses to COVID-19
Abstract
:1. Introduction
Aims and Objectives
- What evidence exists regarding the impacts of any of the novel coronavirus outbreaks of the 21st Century, including COVID-19, on PWUD, drug-related deaths and other harms and what is the quality of evidence?
- How have services who provide support for PDU and policy makers responded to any of the 21st Century outbreaks, including COVID-19, and what is the quality of evidence supporting their responses?
- What are the gaps in evidence and what are the future research questions of importance in responding to any future outbreaks?
- What are the implications of past responses to coronavirus epidemics/pandemics to inform future service and policy responses?
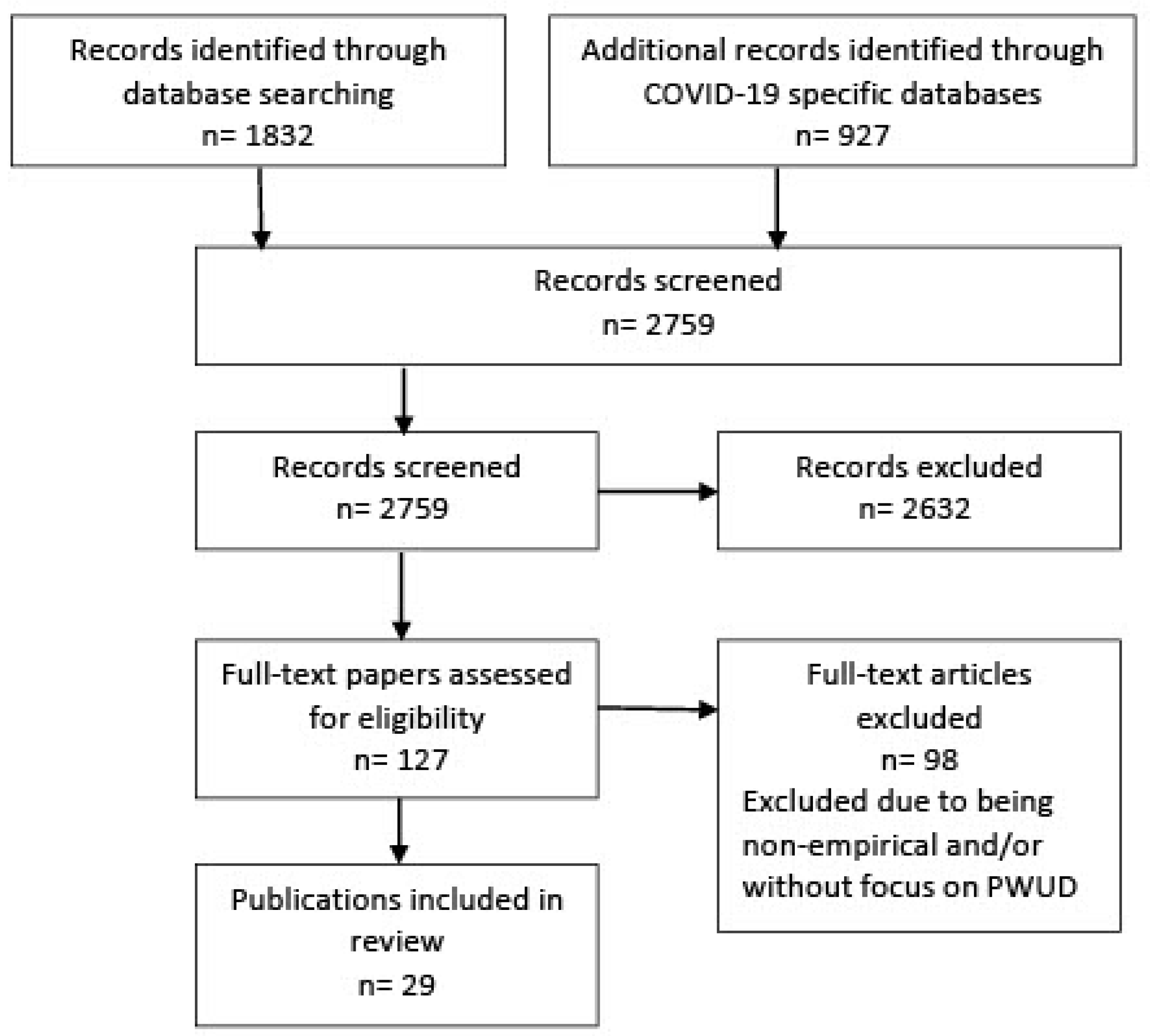
2. Materials and Methods
2.1. Search Strategy
- COVID-19 OR CORONAVIRUS OR 2019-ncov
- SARS-CoV-2
- SARS-CoV-1
- MERS
- SARS
- 1 OR 2 OR 3 OR 4 OR 5
- Problem Drug Users OR People who use drugs OR people who inject drugs
- 6 AND 7
- Limit 8 to English language; limit 8 to year range 2000–2020
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Reporting
2.4. Study Assessment/Quality Assessment
2.5. Additional Quality Assessment
2.5.1. Qualitative Studies
2.5.2. Quantitative Studies
2.5.3. Service Evaluation Studies
3. Results
3.1. Overview of Study Characteristics
- Treatment services/treatment/recovery (8 studies);
- Emergency medical services (5 studies);
- Low threshold services/shelter/homelessness (3 studies);
- People who use drugs/with diagnosis of SUD (7 studies);
- People with SUD and HIV (2 studies);
- Sexual minority CIS men (1 study);
- Prison (1 study).
3.2. Quality Assessment
3.2.1. Weight of Evidence: Methodological Quality, Methodological Relevance and Topic Relevance
3.2.2. The Additional Quality Assessment
3.3. Results Presented by Theme/Setting
3.3.1. Treatment/Recovery Services (Eight Studies)
3.3.2. Emergency Medical Services (EMS) (Five Studies)
3.3.3. Low Threshold Services/Shelter/Homeless (Three Studies)
3.3.4. People Who Use Drugs/with Diagnosis of Substance Use Disorder in Predominantly Community Settings
3.3.5. People with HIV and Substance Use Disorder
3.3.6. ‘Sexual Minority’ Men
3.3.7. Prison
4. Discussion
4.1. Psychological and Physical Wellbeing
4.2. Vulnerable Groups
4.3. Reduced Access to Treatment and Harm REDUCTION Services
4.4. Drug Related Deaths
4.5. Drug Use Patterns
4.6. Answering the Research Questions
4.6.1. Question 1. What Evidence Exists Regarding the Impacts of Any of the Novel Coronavirus Outbreaks of the 21st Century on Problem Drug Users, including COVID-19, Drug-Related Deaths and Other Harms; What Is the Quality of the Evidence?
4.6.2. Question 2. How Have Services Who Provide Support for PDU and Policy Makers Responded to Any of the 21st Century Outbreaks, including COVID-19 and What Is the Quality of the Evidence Supporting Their Responses?
4.6.3. Question 3. What Are the Gaps in Evidence and What Are the Future Research Questions of Importance in Responding to Any Future Outbreaks?
4.6.4. Question 4. What Are the Implications of Past Responses to Coronavirus Epidemics/Pandemics to Inform Future Service and Policy Responses and Specifically in Scotland?
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Drug Report 2020 (United Nations Publication, Sales No. E.20.XI.6). Available online: https://wdr.unodc.org/uploads/wdr2020/documents/WDR20_Booklet_2.pdf (accessed on 28 June 2021).
- National Institute for Health Care Excellence (NICE). Drug Use Disorders in Adults. 2012. Available online: https://www.nice.org.uk/guidance/qs23/resources/drug-use-disorders-in-adults-pdf-2098544097733 (accessed on 28 June 2021).
- Mathers, B.M.; Degenhardt, L.; Bucello, C.; Lemon, J.; Wiessing, L.; Hickman, M. Mortality among people who inject drugs: A systematic review and meta-analysis. Bull. World Health Organ. 2013, 91, 102–123. [Google Scholar] [CrossRef]
- Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid and Stimulant-Related Harms in Canada. Ottawa: Public Health Agency of Canada. March 2021. Available online: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/ (accessed on 28 June 2021).
- Lacobucci, G. Drug Deaths: Scottish minister vows to tackle “public health emergency”. BMJ 2019, 367, 16776. [Google Scholar] [CrossRef]
- National Records Scotland. Drug-Related Deaths in Scotland in 2019—Report. 2020. Available online: https://nrscotland.gov.uk/ (accessed on 8 February 2021).
- Center for Disease Control and Prevention. Available online: https://www.cdc.gov/drugoverdose/deaths/index.html (accessed on 30 March 2021).
- Imtiaz, S.; Shield, K.D.; Fischer, B.; Elton-Marshall, T.; Sornpaisarn, B.; Probst, C.; Rehm, J. Recent changes in trends of opioid overdose deaths in North America. Subst. Abuse Treat. Prev. Policy 2020, 15, 66. [Google Scholar] [CrossRef]
- Aldridge, R.W.; Story, A.; Hwang, S.W.; Nordentoft, M.; Luchenski, S.A.; Hartwell, G.; Tweed, E.J.; Lewer, D.; Katikireddi, S.V.; Hayward, A.C. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: A systematic review and meta-analysis. Lancet 2018, 391, 241–250. [Google Scholar] [CrossRef] [Green Version]
- Monnat, S.M. Factors Associated With County-Level Differences in U.S. Drug-Related Mortality Rates. Am. J. Prev. Med. 2018, 54, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics Deaths Related to Drug Poisonings in England and Wales 2019 Registrations. 2020. Available online: https://www.ons.gov.uk/ (accessed on 8 February 2021).
- Goldner, E.M.; Lusted, A.; Roerecke, M.; Rehm, J.; Fischer, B. Prevalence of Axis-1 psychiatric (with focus on depression and anxiety) disorder and symptomatology among non-medical prescription opioid users in substance use treatment: Systematic review and meta-analyses. Addict. Behav. 2014, 39, 520–553. [Google Scholar] [CrossRef] [PubMed]
- NIDA. Addiction and Health. 13 July 2020. Available online: https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/addiction-health (accessed on 24 February 2021).
- Thylstrup, B.; Clausen, T.; Hesse, M. Cardiovascular disease among people with drug use disorders. Int. J. Public Health 2015, 60, 659–668. [Google Scholar] [CrossRef] [Green Version]
- Bhargava, S.; Arora, R.R. Cocaine and cardiovascular complications. Am. J. Ther. 2011, 18, e95–e100. [Google Scholar] [CrossRef] [PubMed]
- Radke, J.B.; Owen, K.P.; Sutter, M.E.; Ford, J.B.; Albertson, T.E. The effects of opioids on the lung. Clin. Rev. Allergy Immunol. 2014, 46, 54–64. [Google Scholar] [CrossRef]
- Aveyard, P.; Gao, M.; Lindson, N.; Hartmann-Boyce, J.; Watkinson, P.; Young, D.; Coupland, C.A.; San Tan, P.; Clift, A.K.; Harrison, D.; et al. Association between pre-existing respiratory disease and its treatment, and severe COVID-19: A population cohort study. Lancet Respir. Med. 2021, 2213–2600. [Google Scholar] [CrossRef]
- Lohia, P.; Sreeram, K.; Nguyen, P.; Choudhary, A.; Khicher, S.; Yarandi, H.; Kapur, S.; Badr, M.S. Preexisting respiratory diseases and clinical outcomes in COVID-19: A multihospital cohort study on predominantly African American population. Respir. Res. 2021, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cevik, M.; Marcus, J.L.; Buckee, C.; Smith, T.C. SARS-CoV-2 transmission dynamics should inform policy. Clin. Infect. Dis. 2020, 73, S170–S176. [Google Scholar] [CrossRef]
- John Hopkins University. COVID-19 Dashboard. 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 8 February 2021).
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Altamimi, A.; Abu-Saris, R.; El-Metwally, A.; Alaifan, T.; Alamri, A. Demographic Variations of MERS-CoV Infection among Suspected and Confirmed Cases: An Epidemiological Analysis of Laboratory-Based Data from Riyadh Regional Laboratory. Biomed. Res. Int. 2020, 2020, 9629747. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef] [Green Version]
- National Records Scotland. Deaths Involving Coronavirus (COVID-19) in Scotland: Week 19 (4 May to 10 May 2020). Edinburgh: National Records of Scotland. 2020. Available online: https://www.nrscotland.gov.uk/files//statistics/covid19/covid-deaths-report-week-19.pdf (accessed on 3 June 2020).
- Singh, A.K.; Khunti, K. Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review. Diabetes Res. Clin. Pract. 2020, 165. [Google Scholar] [CrossRef]
- Sze, S.; Pan, D.; Nevill, C.R.; Gray, L.J.; Martin, C.M.; Nazareth, J.; Minhas, J.S.; Divall, P.; Khunti, K.; Abrams, K.R.; et al. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2021, 29, 100630. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE). COVID-19 Rapid Guideline: Managing COVID-19. Available online: https://www.nice.org.uk/guidance/NG191 (accessed on 28 June 2021).
- Grebely, J.; Cerdá, M.; Rhodes, T. COVID-19 and the health of people who use drugs: What is and what could be? Int. J. Drug Policy 2020, 83. [Google Scholar] [CrossRef]
- O’Carroll, A.; Duffin, T.; Collins, J. Harm reduction in the time of COVID-19: Case study of homelessness and drug use in Dublin, Ireland. Int. J. Drug Policy 2021, 87, 102966. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evidence for Policy and Practice Information and Co-Ordinating Centre. EPPI Centre Methods for Conducting Systematic Reviews (London, Social Science Research Unit, Institute of Education). 2010. Available online: https://eppi.ioe.ac.uk/cms/ (accessed on 8 February 2021).
- Critical Appraisal Skills Programme (CASP). Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 8 February 2021).
- Booth, A.; Hannes, K.; Harden, A.; Noyes, J.; Harris, J.; Tong, A. COREQ (Consolidated Criteria for Reporting Qualitative Studies). In Guidelines for Reporting Health Research: A User’s Manual; John Wiley & Sons Online: Hoboken, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Sandelowski, M.; Barroso, J. Classifying the Findings in Qualitative Studies. Qual. Health Res. 2003, 13, 905–923. [Google Scholar] [CrossRef]
- Dejong, C.J.; Verhagen, J.D.; Pols, R.; Verbrugge, C.G.; Baldacchino, A. Psychological impact of the acute COVID-19 period on patients with substance use disorders: We are all in this together. Basic Clin. Neurosci. 2020, 11, 207–216. [Google Scholar]
- Pandit, P.M.; Bhatia, G.; Sarkar, S. Treatment experience for opioid use disorder during COVID-19 in India: Learning from patients. J. Subst. Abus. Treat. 2020, 119. [Google Scholar] [CrossRef]
- Glober, N.; Mohler, G.; Huynh, P.; Arkins, T.; O’Donnell, D.; Carter, J.; Ray, B. Impact of COVID-19 Pandemic on Drug Overdoses in Indianapolis. J. Urban Health 2020, 97, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Welle-Strand, G.K.; Skurtveit, S.; Clasusen, T.; Sundal, C.; Gjersing, L. COVID-19 survey among people who use drugs in three cities in Norway. Drug Alcohol Depend. 2020, 217, 108302. [Google Scholar] [CrossRef] [PubMed]
- Slavova, S.; Rock, P.; Bush, H.M.; Quesinberry, D.; Walsh, S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020, 214, 108176. [Google Scholar] [CrossRef] [PubMed]
- Mariottini, C.; Ojanperä, I.; Kriikku, P. Increase in drugs-of-abuse findings in post-mortem toxicology due to COVID-19 restrictions—First observations in Finland. Drug Test. Anal. 2020. [Google Scholar] [CrossRef]
- Martinotti, G.; Alessi, M.C.; Di Natale, C.; Sociali, A.; Ceci, F.; Lucidi, L.; Picutti, E.; Di Carlo, F.; Corbo, M.; Vellante, F.; et al. Psychopathological Burden and Quality of Life in Substance Users During the COVID-19 Lockdown Period in Italy. Front. Psychiatry. 2020, 11. [Google Scholar] [CrossRef]
- Hochstatter, K.R.; Akhtar, W.Z.; Dietz, S.; Pe-Romashko, K.; Gustafson, D.H.; Shah, D.V.; Krechel, S.; Liebert, C.; Miller, R.; El-Bassel, N.; et al. Potential Influences of the COVID-19 Pandemic on Drug Use and HIV Care Among People Living with HIV and Substance Use Disorders: Experience from a Pilot mHealth Intervention. AIDS Behav. 2021, 25, 354–359. [Google Scholar] [CrossRef]
- Ochalek, T.A.; Cumpston, K.L.; Wills, B.K.; Gal, T.S.; Moeller, F.G. Nonfatal Opioid Overdoses at an Urban Emergency Department During the COVID-19 Pandemic. JAMA 2020, 324, 1673–1674. [Google Scholar] [CrossRef] [PubMed]
- Weiner, S.G.; Cash, R.E.; Hendricks, M.; El Ibrahim, S.; Baker, O.; Seethala, R.R.; Peters, G.; Goldberg, S.A. Ambulance Calls for Substace-Related Issues Before and After COVID-19. Prehospital Emerg. Care 2020. [Google Scholar] [CrossRef]
- Wang, Q.Q.; Kaelber, D.C.; Xu, R.; Volkow, N.D. COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States. Mol. Psychiatry 2021, 26, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Starks, T.J.; Jones, S.S.; Sauermilch, D.; Benedict, M.; Adebayo, T.; Cain, D.; Simpson, K.N. Evaluating the impact of COVID-19: A cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug Alcohol Depend. 2020, 216, 108260. [Google Scholar] [CrossRef]
- Whitfield, M.; Reed, H.; Webster, J.; Hope, V. The impact of COVID-19 restrictions on needle and syringe programme provision and coverage in England. Int. J. Drug Policy 2020, 83, 102851. [Google Scholar] [CrossRef]
- Bandara, S.; Kennedy-Hendricks, A.; Merritt, S.; Barry, C.L.; Saloner, B. Early Effects of COVID-19 on Programs Providing Medications for Opioid Use Disorder in Jails and Prisons. J. Addict. Med. 2020, 14, e257–e260. [Google Scholar] [CrossRef] [PubMed]
- Hawke, L.D.; Barbic, S.P.; Voineskos, A.; Szatmari, P.; Cleverley, K.; Hayes, E.; Relihan, J.; Daley, M.; Courtney, D.; Cheung, A.; et al. Impacts of COVID-19 on Youth Mental Health, Substance Use, and Well-being: A Rapid Survey of Clinical and Community Samples: Répercussions de la COVID-19 sur la santé mentale, l’utilisation de substances et le bien-être des adolescents: Un sondage rapide d’échantillons cliniques et communautaires. Can. J. Psychiatry 2020, 65, 701–709. [Google Scholar] [CrossRef]
- Peacock, A.; Price, O.; Dietze, P.; Bruno, R.; Salom, C.; Lenton, S.; Swanton, R.; Uporova, J.; Karlsson, A.; Chan, R.; et al. Impacts of COVID-19 and Associated Restrictions on People Who Use Illicit Stimulants in Australia: Findings from the Ecstasy and Related Drugs Reporting System 2020. Sydney: National Drug and Alcohol Research Centre. Available online: https://ndarc.med.unsw.edu.au/sites/default/files/ndarc/resources/COVID%20EDRS%20bulletin_National_20200917.pdf (accessed on 8 February 2021).
- Radfar, S.R.; De Jong, C.A.; Farhoudian, A.; Ebrahimi, M.; Rafei, P.; Vahidi, M.; Yunesian, M.; Kouimtsidis, C.; Arunogiri, S.; Massah, O.; et al. Reorganization of Substance Use Treatment and Harm Reduction Services During the COVID-19 Pandemic: A Global Survey. Front. Psychiatry 2021, 12, 639393. [Google Scholar] [CrossRef]
- Figgatt, M.C.; Salazar, Z.; Day, E.; Vincent, L.; Dasgupta, N. Take-home dosing experiences among persons receiving methadone maintenance treatment during COVID-19. J. Subst. Abuse Treat. 2021, 123, 108276. [Google Scholar] [CrossRef]
- Trujols, J.; Larrabeiti, A.; Sànchez, O.; Madrid, M.; De Andrés, S.; Duran-Sindreu, S. Increased flexibility in methadone take-home scheduling during the COVID-19 pandemic: Should this practice be incorporated into routine clinical care? J. Subst. Abuse Treat. 2020, 119, 108154. [Google Scholar] [CrossRef]
- Rodda, L.N.; West, K.L.; LeSaint, K.T. Opioid Overdose-Related Emergency Department Visits and Accidental Deaths during the COVID-19 Pandemic. J. Urban Health 2020, 97, 808–813. [Google Scholar] [CrossRef]
- Little, D.L.; Gaisser, M. Fewer Patients Started on Medications for Opioid Use Disorder during COVID-19. 2020. Available online: https://ehrn.org/articles/fewer-patients-started-on-medications-for-opioid-use-disorder-during-covid-19/ (accessed on 29 June 2020).
- Mellis, A.M.; Potenza, M.N.; Hulsey, J.N. COVID-19-related treatment service disruptions among people with single- and polysubstance use concerns. J. Subst. Abuse Treat. 2021, 121, 108180. [Google Scholar] [CrossRef] [PubMed]
- Rozanova, J.; Shenoi, S.; Zaviryukha, I.; Zeziulin, O.; Kiriazova, T.; Rich, K.; Mamedova, E.; Yariy, V. Social Support is Key to Retention in Care during Covid-19 Pandemic among Older People with HIV and Substance Use Disorders in Ukraine. Subst. Use Misuse 2020, 55, 1902–1904. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, J.J.; Mikre, M.; Whitley, P.; Dawson, E.; Huskey, A.; Lukowiak, A.; Giroir, B.P. Analysis of Drug Test Results Before and After the US Declaration of a National Emergency Concerning the COVID-19 Outbreak. JAMA 2020, 324, 1674–1677. [Google Scholar] [CrossRef]
- Nelson, E.; Dumbili, E.W.; Odeigah, O.W. Drug use treatment during COVID-19 pandemic: Community-based services in Nigeria. J. Subst. Use 2020. [Google Scholar] [CrossRef]
- Malczewski, A.; Kidawa, M.; Bevz, M. The impact of the COVID-19 epidemic on drug services, drug users and drug market in Poland -findings of the rapid situation assessment. Reitox Natl. Focal Point Natl. Bur. Drug Prev. Poland. 2020. [Google Scholar] [CrossRef]
- Martin, C.; Andrés, P.; Bullón, A.; Villegas, J.L.; de la Iglesia-Larrad, J.I.; Prieto, N.; Roncero, C. COVID pandemic as an opportunity for improving mental health treatments of the homeless people. Int. J. Soc. Psychiatry 2020. [Google Scholar] [CrossRef]
- Gamarel, K.E.; Reisner, S.L.; Laurenceau, J.-P.; Nemoto, T.; Operario, D. Gender minority stress, mental health and relationship quality: A dydadic investigation of transgender women and their cisgender male partners. J. Fam. Psychol. 2014, 28, 437–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castaldelli-Maia, J.M.; Marziali, M.E.; Lu, Z.; Martins, S.S. Investigating the effect of national government physical distancing measures on depression and anxiety during the COVID-19 pandemic through meta-analysis and meta-regression. Psychol. Med. 2021, 51, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Frank, P.; Iob, E.; Steptoe, A.; Fancourt, D. Trajectories of Depressive Symptoms among vulnerable groups in the UK during the COVID-19 pandemic. medRviv 2020. [Google Scholar] [CrossRef]
- Gayer˗Anderson, C.; Latham, R.; El Zerbi, C.V.; Strang, L.; Moxham Hall, V.; Knowles, G.; Marlow, S.; Avendano, M.; Manning, N.; Das-Munshi, J.; et al. Impacts of Social Isolation among Disadvantaged and Vulnerable Groups during Public Health Crises. Available online: https://esrc.ukri.org/files/news-events-and-publications/evidence-briefings/impacts-of-social-isolation-among-disadvantaged-and-vulnerable-groups-during-public-health-crises/ (accessed on 28 June 2021).
- British Medical Association BMA Position Statement on COVID-19 and Homelessness in England. 2020. Available online: https://www.bma.org.uk (accessed on 22 June 2021).
- Scottish Government COVID-19 Allocation Advice and Information for the Housing Sector. 2020. Available online: www.gov.scot (accessed on 28 June 2021).
- Parkes, T.; Carver, H.; Masterton, W.; Falzon, D.; Dumbrell, J.; Grant, S.; Wilson, I. ‘They already operated like it was a crisis, because it always has been a crisis’: A qualitative exploration of the response of one homeless service in Scotland to the COVID-19 pandemic. Harm Reduct. J. 2021, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Genberg, B.L.; Astemborski, J.; Piggott, D.A.; Woodson-Adu, T.; Kirk, G.D.; Mehta, S.H. The health and social consequences during the initial period of the COVID-19 pandemic among current and former people who inject drugs: A rapid phone survey in Baltimore, Maryland. Drug Alcohol Depend. 2021, 221, 108584. [Google Scholar] [CrossRef]
- Cyrus, E.; Clarke, R.; Hadley, D.; Bursac, Z.; Trepka, M.J.; Dévieux, J.G.; Bagci, U.; Furr-Holden, D.; Coudray, M.; Mariano, Y.; et al. The Impact of COVID-19 on African American Communities in the United States. Health Equity 2020, 4, 476–483. [Google Scholar] [CrossRef]
- Khanijahani, A. Racial, ethnic, and socioeconomic disparities in confirmed COVID-19 cases and deaths in the United States: A county-level analysis as of November 2020. Ethn. Health 2021, 26, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Malta, M.; Varatharajan, T.; Russell, C.; Pang, M.; Bonato, S.; Fischer, B. Opioid-related treatment, interventions, and outcomes among incarcerated persons: A systematic review. PLoS Med. 2019, 16, e1003002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marsden, J.; Stillwell, G.; Jones, H.; Cooper, A.; Eastwood, B.; Farrell, M.; Lowden, T.; Maddalena, N.; Metcalfe, C.; Shaw, J.; et al. Does exposure to opioid substitution treatment in prison reduce the risk of death after release? A national prospective observational study in England. Addiction 2017, 112, 1408–1418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Croxford, S.; Emanuel, E.; Ibitoye, A.; Njoroge, J.; Edmundson, C.; Bardsley, M.; Heinsbroek, E.; Hope, V.; Phipps, E. Preliminary indications of the burden of COVID-19 among people who inject drugs in England and Northern Ireland and the impact on access to health and harm reduction services. Public Health 2021, 192, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Lindqvist, K.; Wallmofeldt, C.; Holmén, E.; Hammarberg, A.; Kåberg, M. Health literacy and changes in pattern of drug use among participants at the Stockholm Needle Exchange Program during the COVID-19 pandemic. Harm Reduct. J. 2021, 18, 52. [Google Scholar] [CrossRef]
- Picchio, C.A.; Valencia, J.; Doran, J.; Swan, T.; Pastor, M.; Martró, E.; Colom, J.; Lazarus, J.V. The impact of the COVID-19 pandemic on harm reduction services in Spain. Harm Reduct. J. 2020, 17, 87. [Google Scholar] [CrossRef] [PubMed]
- Bardwell, G.; Small, W.; Lavalley, J.; McNeil, R.; Kerr, T. “People need them or else they’re going to take fentanyl and die”: A qualitative study examining the ‘problem’ of prescription opioid diversion during an overdose epidemic. Soc. Sci. Med. 2021, 279, 113986. [Google Scholar] [CrossRef]
- Bloor, R.N.; McAuley, R.; Smalldridge, N. Safe storage of methadone in the home—An audit of the effectiveness of safety information giving. Harm Reduct. J. 2005, 2, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horan, J.A.; Gooney, M.; van Hout, M.C. Safe storage of methadone in the home. An Irish audit of the effectiveness of information provision in pharmacies. Heroin Addict. Clin. Relat. Probl. 2016, 18, 31–40. [Google Scholar]
- Ali, F.; Russell, C.; Nafeh, F.; Rehm, J.; LeBlanc, S.; Elton-Marshall, T. Changes in substance supply and use characteristics among people who use drugs (PWUD) during the COVID-19 global pandemic: A national qualitative assessment in Canada. Int. J. Drug Policy 2021, 93, 103237. [Google Scholar] [CrossRef] [PubMed]
- Chimbar, L.; Moleta, Y. Naloxone Effectiveness: A Systematic Review. J. Addict. Nurs. 2018, 29, 167–171. [Google Scholar] [CrossRef] [PubMed]
- EMCDDA Trendspotter Briefing I Impact of COVID-19 on Patterns of Drug Use and Drug-Related Harms in Europe 2. Available online: https://wdr.unodc.org/wdr2020/field/WDR20_Booklet_3.pdf (accessed on 14 July 2020).
- UNODC—United Nations Office on Drugs and Crime. COVID-19 and the Drug Supply Chain: From Production and Trafficking to Use. 2020. Available online: https://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf (accessed on 27 July 2021).
- Been, F.; Emke, E.; Matias, J.; Baz-Lomba, J.A.; Boogaerts, T.; Castiglioni, S.; Campos-Mañas, M.; Celma, A.; Covaci, A.; de Voogt, P.; et al. Changes in drug use in European cities during early COVID-19 lockdowns—A snapshot from wastewater analysis. Environ. Int. 2021, 106540. [Google Scholar] [CrossRef]
| Inclusion | Exclusion |
|---|---|
| Studies reporting any impact on people who use drugs (PWUD) due to Severe Acute Respiratory Syndrome (SARS), Middle Eastern Respiratory Syndrome (MERS) or COVID-19 | |
| Studies reporting any service response to PWUD due to SARS, MERS or COVID-19 | |
| Qualitative, quantitative, mixed methods or review papers | Non empirical studies, i.e., commentaries, editorials, opinion pieces |
| Published in English | Published in language other than English |
| Published between 2000 and October 2020 | Studies published prior to 2000 |
| WoE 1 Components | Definition | Scoring Range |
|---|---|---|
| Methodological Quality | The trustworthiness of the results judged by the quality of the study within the accepted norms for undertaking a particular type of research design | 1 = excellent 2 = good 3 = satisfactory 4 = inadequate |
| Methodological Relevance | The appropriateness of the study design for addressing particular research questions | 1 = excellent 2 = good 3 = satisfactory 4 = inadequate |
| Topic Relevance | The appropriateness of focus of the study design for addressing their particular research questions | 1 = excellent 2 = good 3 = satisfactory 4 = inadequate |
| Study ID | Study Participants | Country | Setting | Setting Relevance | Method Quality | Method Relevance | Topic Relevance | Weight of Evidence |
|---|---|---|---|---|---|---|---|---|
| Qualitative studies | ||||||||
| DeJong 2020 [36] | Fifteen People with Substance Use Disorder (SUD) (11 under treatment and 4 in recovery) | Netherlands | Treatment and recovery | B | 2 | 1 | 1 | 2 |
| Pandit 2020 [37] | 4 male patients with SUD | India | Community; addiction treatment centre, outpatient service | C | 3 | 3 | 2 | 3 |
| Quantitative studies | ||||||||
| Glober 2020 [38] | Calls for service (CFS) (all/suspected accidental overdose (OD)/suspected OD with naloxone administration/fatal OD) | USA | Emergency Medical Services (EMS) Indianapolis | B | 2 | 2 | 1 | 2 |
| Welle-Strand 2020 [39] | 226 PWUD over 18 years. | Norway | User organisations near the open drug scenes and at low-threshold services | B | 3 | 1 | 1 | 2 |
| Slavova 2020 [40] | People brought to emergency services because of experiencing opioid overdose | USA | Emergency services for people who have an opioid overdose | C | 2 | 2 | 1 | 2 |
| Mariotinni 2020 [41] | All deaths occurring in Jan–Aug 2020 were included in which buprenorphine, amphetamines or THC-COOH were detected | Finland | Toxicology reports | C | 2 | 1 | 1 | 2 |
| Martinotti 2020 [42] | 153 addicted patients, both outpatients and residential inpatients | Italy | Disorder (DSM-5) currently in treatment as outpatients and/or in a residency program as inpatients recruited across Italy. Under lockdown | C | 3 | 2 | 1 | 2 |
| Hochstatter 2020 [43] | 64 People Living with HIV (PLWH) and Substance Use Disorders (SUD) (48 males, 15 females) | USA | Substance use and HIV care—Opioid Relapse Prevention and HIV Management | C | 3 | 2 | 1 | 2 |
| Ochalek 2020 [44] | Those presenting to emergency department with nonfatal unintentional overdose | USA | Emergency department | C | 3 | 3 | 1 | 2 |
| Weiner 2020 [45] | Those making ambulance calls for a substance misuse reason | USA | Ambulance | C | 1 | 1 | 2 | 2 |
| Wang 2020 [46] | 73,099,850 unique patients, including 7,510,380 patients with a diagnosis with SUD (substance use disorders) | USA | Population-level electronic health record (EHR) from 360 hospitals and 317,000 providers across 50 states in the US since 1999 | C | 2 | 3 | 2 | 2 |
| Starks 2020 [47] | 455 CiS male 18 years+ who use drugs: marijuana, cocaine, crack, crystal methamphetamine, GHB, and Ketamine | USA | Cis male LGBTQ+ community | C | 2 | 2 | 3 | 2 |
| Whitfield 2020 [48] | People attending the 105 (91%) of the 115 sites providing NSP services (community pharmacies and specialist service sites) | UK | NSP across Cheshire and Merseyside | A | 3 | 3 | 1 | 3 |
| Bandara 2020 [49] | Wardens, sheriffs, medical directors and other leadership from 19 prisons | USA | Prison | C | 3 | 2 | 1 | 3 |
| Hawke 2020 [50] | 622 youths aged 14 to 28 recruited across 4 existing participant cohorts | Canada | Based at Centre for Addiction and Mental Health, Toronto | B | 3 | 2 | 3 | 3 |
| Peacock 2020 [51] | People aged 18 or older who have used ecstasy and other illicit stimulants | Australia | Adults who have used ecstasy and other illicit stimulants | B | 3 | 3 | 3 | 3 |
| Seyed 2020 [52] | Unclear—aimed at substance use treatment and harm reduction services | Global | Substance use treatment and harm reduction services | B | 3 | 3 | 2 | 3 |
| Figgatt 2020 [53] | 104 persons receiving methadone from three clinics | USA | PWUD receiving from 3 methadone clinics | C | 3 | 3 | 1 | 3 |
| Trujols 2020 [54] | Take home medication schedule (weeks) pre and post COVID-19 for 102 patients | Spain | Methadone Clinic Barcelona | C | 3 | 3 | 2 | 3 |
| Rodda 2020 [55] | Opiate, opioid, heroin, and/or fentanyl related overdose admission to emergency room | USA | Emergency room | C | 3 | 3 | 2 | 3 |
| Little 2020 [56] | Patients receiving first-time prescriptions for Medications for Opioid Use Disorder (MOUD) | USA | Prescriptions for Medications for Opioid Use Disorder | C | 3 | 2 | 2 | 3 |
| Mellis 2021 [57] | 1148 PWUD and family | USA | Members of the Addictions Policy Forum | C | 3 | 4 | 2 | 3 |
| Rozanova 2020 [58] | 123 older people with HIV (males and females). 42% had co-occurring Substance Use Disorders. Plus some (unspecified numbers) telephone interviews with HIV and addiction service providers | Ukraine | Older people with HIV receiving treatment for HIV | C | 3 | 2 | 3 | 3 |
| Wainwright 2020 [59] | 75K + 75K (before and after COVID-19) Individuals (urine test results) with or at risk of SUD | USA | Nationwide lab urine results | C | 2 | 3 | 4 | 3 |
| Nelson 2020 [60] | 6 community drop in centres for PWUD | Nigeria | Community drop in centres for PWUD in Nigeria | C | 4 | 3 | 1 | 4 |
| Malczewski 2020 [61] | Those working in drug-related services including Drug enforcement service; Prevention institution; Harm reduction; Drug treatments | Poland | Drug treatment services in Poland | C | 4 | 3 | 3 | 4 |
| Program Evaluation | ||||||||
| Martin 2020 [62] | 27 homeless people residing in a municipal shelter | Spain | Homeless people in Salamanca city under lockdown in a municipal shelter | C | 3 | 3 | 2 | 3 |
| Components | Excellent | Good | Satisfactory | Inadequate |
|---|---|---|---|---|
| Methodological Quality | 0 | 8 | 17 | 2 |
| Methodological Relevance | 4 | 9 | 13 | 1 |
| Topic Relevance | 12 | 9 | 5 | 1 |
| Overall WoE 1 | 0 | 11 | 14 | 2 |
| Study | Method (Rating) | Participants | Setting (Context Rating) | Main Findings (Weight of Evidence—WoE) |
|---|---|---|---|---|
| Qualitative | ||||
| DeJong 2020 [36] | In-depth interview 2 Good | 15 People with Substance Use Disorder (SUD) Outpatient (8); Inpatient (3); Stable Recovery (4); 11 men and 4 women; mean age 37.2 years | SUD clinical inpatient and outpatient practice or non-clinical projects (B) Netherlands (South East) | COVID-19 has had a serious impact on thoughts, feelings, and behaviours. Thoughts were associated with a range of negative feelings and behaviours, such as stress, anger, avoidance, and isolation. Those still in treatment were fighting against the temptation to start using again; they felt emotionally isolated and sometimes patronised by healthcare workers. (WoE: 2 Good) |
| Pandit 2020 [37] | Case studies 3 Satisfactory | 4 males with SUD | SUD outpatient practice (C) India (no specific location) | Challenges for patients with opioid use disorders in this period, including increased risk of criminal charges due to increased policing, fear of contracting COVID-19 and transmitting it to family members, and stress due to occupational disruption and financial difficulties. Future policies should consider ways to enhance capability to provide medication-assisted treatment more easily to patients who have constrained resources, transport, skills, or willingness to quit. (WoE: 3 Satisfactory) |
| Quantitative | ||||
| Martinotti 2020 [42] | Questionnaire survey 3 Satisfactory | 153 people with diagnosis of SUD in treatment; mean age 39.8 years; 78% males | Outpatients and/or residency program inpatients (C) Italy (various regions) | The presence of a moderate psychopathological burden correlated to poor quality of life and low craving scores. More than half of the cohort reported reduced quality of life during COVID-19 lockdown, and the analysis showed a negative correlation between perceived quality of life and reported craving. (WoE: 2 Good) |
| Figgatt 2020 [53] | Questionnaire survey 3 Satisfactory | 104 persons receiving methadone from three clinics; aged 18 years and over; 56% of the sample were male; 90% of the sample classed as ‘non-Hispanic White’ | Methadone prescribing clinics (C) USA (North Carolina) | Before COVID-19, the clinic-level percent of participants receiving any amount of days’ supply of take-home doses at each clinic ranged from 56% to 82%, while it ranged from 78% to 100% since COVID-19. The clinic-level percent of participants receiving a take-homes days’ supply of a week or longer (i.e., ≥6 days) since COVID-19 ranged from 11% to 56%. Among 87 participants who received take-homes since COVID-19, only four reported selling their take-home doses. (WoE: 3 satisfactory) |
| Radfar 2020 [52] | Questionnaire survey 3 Satisfactory | 177 addiction medicine professionals from 77 countries | SUD treatment and harm reduction services (C) Global (77 countries) | Respondents from over 88% of countries reported that core medical and psychiatric care for SUDs had continued; however, only 56% of countries reported having had any business continuity plan, and 37.5% of countries reported shortages of methadone or buprenorphine supplies. Participants of 41% of countries reported partial discontinuation of harm-reduction services such as needle and syringe programs and condom distribution. In total, 57% of overdose prevention interventions and 81% of outreach services also having been negatively impacted. (WoE: 3 Satisfactory) |
| Malczewski 2020 [61] | Questionnaire survey 4 Inadequate | Provincial drug experts from 71 institutions | Primarily treatment services and harm reduction programmes (C) Poland (Nationwide) | The coronavirus epidemic has considerably affected the Polish drug services, especially in terms of ensuring the continuity of services at the adequate level. The operation of inpatient clinics (residentials treatment) and drop-in centres (harm reduction daily centre) has been limited the most. It is worth noting that substitution treatment has seen a higher demand for its services, which was the consequence of opioid users being deprived of income as a result of the epidemic. The lack of financial resources made drug users decide to enter opioid substitution treatment. (WoE: 4 Inadequate) |
| Whitfield 2020 [48] | Service provision monitoring 3 Satisfactory | People attending the 105 (91%) of the 115 sites providing NSP services | Needle and Syringe Programme provision (A) England (North West) | COVID-19 related restrictions resulted in the number of NSP clients decreasing by 36%, visits by 36%, and needles distributed by 29%. NSP coverage for those injecting psychoactive drugs halved, declining from 14 needles per-week during the 4 weeks to 15 March 2020 to 7 needles per-week by mid-April, and coverage has remained at this level since then. (WoE: 3 Satisfactory) |
| Trujols 2020 [54] | Before and after service evaluation 3 Satisfactory | 102 attendees of methadone clinic | Methadone Clinic (C) Spain (Barcelona) | Take home medication (number of days provided) overall increased significantly [t(101) = −7.759, p < 0.001, d = 0.7680] comparing preCOVID-19 (6–12 March) vs. postCOVID-19 (13 March–12 May). This increase did not lead to any detectable signs that patients might be misusing/diverting medication. (WoE: 3 Satisfactory) |
| Study | Method | Participants | Setting | Main Findings |
|---|---|---|---|---|
| Glober 2020 [38] | Analysis of data from emergency medical services (EMS) system and Coroner’s office pre and post stay at home order 2 Good | Calls to emergency medical services with suspected overdose or where naloxone was administered or death by overdose (actual number not reported); participants were predominately white (67 and 71% pre and post); 26 and 30% black (pre and post); the remainder described as ‘other’. The majority of participants were aged under 40 both pre and post. | Emergency medical services drug overdose and drug deaths (B) USA (Indiana) | Data regarding emergency medicine calls for service (CFS) and suspected accidental drug overdose deaths were analysed. Overdose CFS and EMS naloxone administration showed an increase with the social isolation of the Indiana stay-at-home order, but a continued increase after the stay-at-home order was terminated. Despite a mild 4% increase in all EMS CFS, overdose CFS increased 43% and CFS with naloxone administration increased 61% after the stay-at-home order. Deaths from drug overdoses increased by 47%. (WoE: 2 Good) |
| Ochalek 2020 [44] | Before and after comparison of electronic medical record data (early months of the pandemic compared to the previous year) 3 Satisfactory | 329 records of nonfatal, unintentional opioid-related opioid overdoses; the mean ages were 42.2 years and 44.0 years, 71 (70%) and 165 (73%) were male, 64 (63%) and 181 (80%) were Black, respectively. | Urban emergency department (C) USA (Virginia) | Number of unintentional opioid-related opioid overdoses increased (n =102 March–June 2019; n = 227 March June 2020). In March through June 2019 and March through June 2020, 55 (54%) and 127 (56%) patients received a naloxone prescription and 45 (44%) and 154 (68%) received treatment resources and/or a referral at discharge, respectively. However, only 4 (4%) and 14 (6%) of the 17 (17%) and 46 (20%) admitted patients received an addiction medicine consult, and 3 (3%) and 23 (10%) accessed treatment at the outpatient clinic after overdosing, respectively. (WoE: 2 Good) |
| Rodda 2020 [55] | Electronic medical record data before and after social distancing mandates were enacted 3 Satisfactory | 189 patients seen for opioid-related overdose. | 2 urban emergency departments (C) USA (San Francisco) | Emergency departments saw approximately 2.5 patients per day with opioid overdose, compared with 1.4 patients per day prior to this period. From 16 March to 18 April, there were 1.47 deaths per day, compared with 0.95 deaths per day prior to this period. During the first weeks of a COVID-19 pandemic, emergency room presentations and deaths related to opioid overdose may increase during an isolation period. (WoE: 3 Satisfactory) |
| Slavova 2020 [40] | Analysis of ambulance runs resulting in visits to Emergency Room before and after onset of COVID-19 pandemic 2 Good | Emergency response records of patients involved in ambulance runs for opioid overdose; no patient demographic data. | State Ambulance Reporting System (C) USA (Kentucky) | EMS runs in response to opioid overdoses have significantly increased since the COVID-19 crisis began. By comparing the period before the emergency declaration was made to the period after the declaration, EMS runs for opioid overdose have increased both in the rate of transportation to ED and, critically, in the number of those who were treated on the scene and refused transportation to ED. (WoE: 2 Good) |
| Weiner 2020 [45] | Retrospective cross-sectional analysis of evaluating average daily 9-1-1 ambulance calls for substance use-related issues compared with all other calls 2 Good | All 9-1-1 ambulance calls from February 15, 2020 to 15 May 2020; mean age 51.6 years (pre COVID-19) and 52.6 years post COVID-19); males were 49.8% of the pre sample and males and 52.8% of the post sample. | 9-1-1 ambulance calls (C) USA (Massachusetts) | Calls for substance-related reasons decreased by 16.4% compared with prior to the state-wide emergency. However, despite an initial decrease in calls, after the stay-at-home advisory calls for substance use began increasing by 0.7 (95% confidence interval (CI) 0.4–1.1) calls/day, while calls for other reasons did not significantly change (þ1.2 (95% CI −0.8 to 3.1) calls/day). Refusal of transport for substance-related calls increased from 5.0% before the state-wide emergency to 7.5% after the declaration (p < 0.001). (WoE: 2 Good) |
| Study | Method | Participants | Setting | Main Findings |
|---|---|---|---|---|
| Martin 2020 [62] | Programme evaluation with interview data 3 Satisfactory | 29 homeless people (a proportion of whom had substance misuse disorder or psychiatric disorder); 27 evaluated; 67% male; ‘average’ age 37 years; 33% had a SUD. | Hostel for confined homeless of the city council social services (C) Spain (Salamanca) | Due to the pandemic caused by COVID-19, social and healthcare circumstances relative to homeless population, which usually are complicated, could be even more difficult. However, due to the intervention and implementation of this new program in the City Hall resources made by the Psychiatry Service, the objectives of detecting, treating and referring patients to social and mental health care resources, turned the unfortunate situation of the pandemic into an opportunity for this population. (WoE: 3 Satisfactory) |
| Nelson 2020 [60] | Questionnaire survey collecting service level data 4 Inadequate | Managers of drop-in centres (n not reported). | Drop-in centres for PWUD operated by Non-Governmental Organizations (C) Nigeria (4 regions) | The lockdown limited the range and quality of services provided, and constrained uptake by PWUD. Service utilisation declined from 375 users in October 2019 to 198 in April, before reaching 321 in May. Female users were more affected by the disruption than men. Cannabis was the drug most commonly used by service users followed by opioids and alcohol. There were significant gaps in service provision, including limited face-to-face counselling and discontinuation of other services. (WoE: 4 Inadequate) |
| Welle-Strand 2020 [39] | Questionnaire survey 3 Satisfactory | 226 PWUD attending COVID-19 isolation units; mean age 43.1, 73% males. | Isolation units for COVID-19 positive PWUD (B) Norway (3 cities) | The main finding was that current or recent OMT experience (i.e., treatment engagement) was associated with improved knowledge of common COVID-19 symptoms and about available services. OMT may play an important role in COVID-19 prevention, as current and previous OMT patients were more likely to be aware of COVID-19 symptoms, as well as COVID-19 services available for PWUD. (WoE: 2 Good) |
| Study | Method | Participants | Setting | Main Findings |
|---|---|---|---|---|
| Hawke 2020 [50] | Questionnaire survey 3 Satisfactory | 622 participants aged 14–28; 62% female; 61% Caucasian | 4 existing participant cohorts based at the Centre for Addiction and Mental Health (CAMH) (C) Canada (Toronto, Ontario) | Reports of pre-pandemic mental health compared to intra-pandemic mental health show a statistically significant deterioration of mental health across clinical and community samples (p < 0.001), with greater deterioration in the community sample. A total of 68.4% of youth in the clinical sample and 39.9% in the community sample met screening criteria for an internalising disorder. Substance use declined in both clinical and community samples (p < 0.001), although 23.2% of youth in the clinical sample and 3.0% in the community sample met screening criteria for a substance use disorder. Participants across samples report substantial mental health service disruptions (48.7% and 10.8%) and unmet support needs (44.1% and 16.2%). (WoE: 3 Satisfactory) |
| Mellis 2020 [55] | Questionnaire survey 3 Satisfactory | 1,148 members of the APF network of patients, families and survivors; aged 18 years and over; 66% female, 88% Caucasian | Addiction Policy Forum (APF) fielded an uncompensated survey via email to their national (U.S.) network of patients, families, and survivors (C) USA (multiple states) | Individuals who reported a history of use of multiple substances were more likely to report that COVID-19 has affected their treatment and service access and were specifically more likely to report both use of telehealth services and difficulties accessing needed services. These findings suggest that individuals with a history of using multiple substances may be at greater risk for poor outcomes due to COVID-19, even in the face of expansion of telehealth service access. (WoE: 3 Satisfactory) |
| Peacock 2020 [51] | Questionnaire survey 3 Satisfactory | 389 people aged 18 or older who have used ecstasy and other illicit stimulants at least once monthly in the preceding six months Median age 23; 65% males | Participants recruited from the community via social media and/or peer referral (B) Australia (multiple states) | (Preliminary results). Most participants reported no change or a decrease in their drug use since COVID-19 restrictions compared to before March 2020, although changes in use varied by drug. Perceptions of drug availability were mostly that it remained stable. Participants reported negative impacts on mental health but did not report difficulties engaging with services for alcohol and drug-related reasons and had sought information about practices to reduce the risk of COVID-19 transmission while using drugs. (WoE: 3 Satisfactory) |
| Wainwright 2020 [59] | Cross sectional study of urine drug tests before and during COVID-19 declaration 2 Good | 150,000 patient specimens of urine sent for testing; aged 18 years and over; 47% male. No ethnicity information declared | Healthcare settings where practitioners have patients who are diagnosed with or at risk of substance misuse (C) USA (multiple states) | This study demonstrated that urine drug test positivity in a population diagnosed with or at risk of substance use disorders increased significantly for illicit cocaine, fentanyl, heroin, and methamphetamine from the 4 months before the COVID-19 emergency declaration to the 4 months after the COVID-19 declaration. (WoE: 3 Satisfactory) |
| Wang 2020 [46] | Retrospective case–control study of electronic health records 2 Good | 73,099,850 unique patients, of whom 12,030 had a diagnosis of COVID-19. 722,370 had been recently diagnosed with SUD; includes all age ranges; predominantly Caucasians | Electronic health records from 360 hospitals and 317,000 providers across 50 states in the US since 1999 (C) USA (50 states | Patients with a recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19 (adjusted odds ratio or AOR = 8.699 [8.411–8.997], P < 10−30). Compared to patients without SUD, patients with SUD had significantly higher prevalence of chronic kidney, liver, lung diseases, cardiovascular diseases, type 2 diabetes, obesity and cancer. Findings identify individuals with SUD, especially individuals with OUD and African Americans, as having increased risk for COVID-19 and its adverse outcomes, highlighting the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support. (WoE: 2 Good) |
| Little 2020 [54] | Predictive linear regression of Electronic Health Care population data 3 Satisfactory | Data are pooled from 16 healthcare organisations that span 11 states and cover 11.1 million patients | Receipt of prescription of medications for opioid use disorder (C) USA (12 states) | The number of patients receiving first-time prescriptions for Medications for Opioid Use Disorder (MOUD) decreased by over 30% in the spring of 2020 when compared to trends observed in EHR data from January 2017 to May 2020. This finding suggests that patients at risk for opioid use disorder (OUD) and overdose are increasingly vulnerable during the COVID-19 pandemic. (WoE: 3 Satisfactory) |
| Mariotinni 2020 [41] | Before and after lockdown analysis of post-mortem toxicology cases 2 Good | All post-mortem toxicology cases in Finland | Post-mortem where buprenorphine, amphetamine or cannabis was found (C) Finland | Immediately after government restrictions in March 2020, the numbers of buprenorphine, amphetamine and cannabis findings increased. The increase was most noticeable for amphetamine and was evident in all age groups. Findings indicate by association that there is an increased risk of drug-related harm (including death) in Finland. (WoE: 2 Good) |
| Study | Method | Participants | Setting | Main Findings |
|---|---|---|---|---|
| Hochstatter 2020 [43] | Questionnaire survey 6 weeks before national emergency compared to 6 weeks after 3 Satisfactory | 60 individuals with SUD and HIV; 75% male; 59% black or African American, 34% White, 2% mixed; 5% ‘other’ | Opioid relapse prevention and HIV management mobile-health Intervention (C) USA (Wisconsin) | During the pandemic, people who live with HIV and SUD increased illicit substance use and contact with other substance-using individuals and decreased their confidence to stay sober and attend recovery meetings. The proportion of people missing their HIV medications also increased, and confidence to attend HIV follow-up appointments decreased. (WoE: 2 Good) |
| Rozanova 2020 [58] | Questionnaire survey May 2020 3 Satisfactory | 123 older people (aged >50) with HIV and SUD; 47% women, also HIV and addiction treatment providers at frontlines and senior executive levels | Services providing treatment and care for older people with HIV and SUD (C) Ukraine (Kyiv) | While older people with SUD maintained HIV and SUD therapy throughout COVID-19 lockdown, social support is critical to avoiding treatment interruption. COVID-19 lockdown may disrupt MAT and ART among older people with HIV and SUD not only while being in place, but also during the reopening. After recent increases of support by clinicians, subsequent reduction of support may lead to people feeling even more isolated. (WoE: 3 Satisfactory) |
| Study | Method | Participants | Setting | Main Findings |
|---|---|---|---|---|
| Starks 2020 [47] | Matched cohort-controlled study with questionnaire survey compared respondents (surveyed May 6–17, 2020) and a matched sample selected from 65,707 respondents surveyed pre-COVID-19 2 Good | 455 adult sexual minority CIS males who use drugs; age range 18+; 47% ‘white’; 29% ‘black’; 14% Latino; 10% other; drugs mainly marijuana | Geosocial networking apps for gay, bi, trans, and queer people seeking sexual partners. The COVID-19 cohort responded to an advertisement that included an image of one or more adolescent or adult males. (C) USA (multiple states) | While the proportion of participants reporting marijuana and other illegal drug use as well as CAS with casual partners declined during COVID, the association between other illegal drug use and sexual risk behaviour was amplified. (WoE: 2 Good) |
| Study | Method | Participants | Setting | Main Findings |
|---|---|---|---|---|
| Bandara 2020 [49] | Questionnaire survey 3 Satisfactory | Wardens, sheriffs, medical directors, and other leadership (no demographic data) | 19 prisons (14 county jail systems and 5 state-level systems) that provide methadone and/or buprenorphine treatment for incarcerated populations (C) USA (multiple states) | Ten out of 16 systems reported downsizing their OAT programs. Seven of 16 systems made changes to medication dispensation processes. Half of systems report challenges implementing physical distancing (n¼8), and/or obtaining personal protective equipment (n¼8). In 13 out of 16 systems some OAT program participants were released early due to COVID-19 infection risk. (WoE: 3 Satisfactory) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Munro, A.; Booth, H.; Gray, N.M.; Love, J.; Mohan, A.R.M.; Tang, J.; MacGillivray, S. Understanding the Impacts of Novel Coronavirus Outbreaks on People Who Use Drugs: A Systematic Review to Inform Practice and Drug Policy Responses to COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 8470. https://doi.org/10.3390/ijerph18168470
Munro A, Booth H, Gray NM, Love J, Mohan ARM, Tang J, MacGillivray S. Understanding the Impacts of Novel Coronavirus Outbreaks on People Who Use Drugs: A Systematic Review to Inform Practice and Drug Policy Responses to COVID-19. International Journal of Environmental Research and Public Health. 2021; 18(16):8470. https://doi.org/10.3390/ijerph18168470
Chicago/Turabian StyleMunro, Alison, Hazel Booth, Nicola M. Gray, Joan Love, Andrea R. M. Mohan, Jason Tang, and Steve MacGillivray. 2021. "Understanding the Impacts of Novel Coronavirus Outbreaks on People Who Use Drugs: A Systematic Review to Inform Practice and Drug Policy Responses to COVID-19" International Journal of Environmental Research and Public Health 18, no. 16: 8470. https://doi.org/10.3390/ijerph18168470
APA StyleMunro, A., Booth, H., Gray, N. M., Love, J., Mohan, A. R. M., Tang, J., & MacGillivray, S. (2021). Understanding the Impacts of Novel Coronavirus Outbreaks on People Who Use Drugs: A Systematic Review to Inform Practice and Drug Policy Responses to COVID-19. International Journal of Environmental Research and Public Health, 18(16), 8470. https://doi.org/10.3390/ijerph18168470





