Association between Body Mass Index and Outcomes in Patients with Return of Spontaneous Circulation after Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources and Literature Search Strategy
2.4. Study Selection
2.5. Data Collection Process and Data Items
2.6. Risk of Bias in Individual Studies
2.7. Statistical Analysis
3. Results
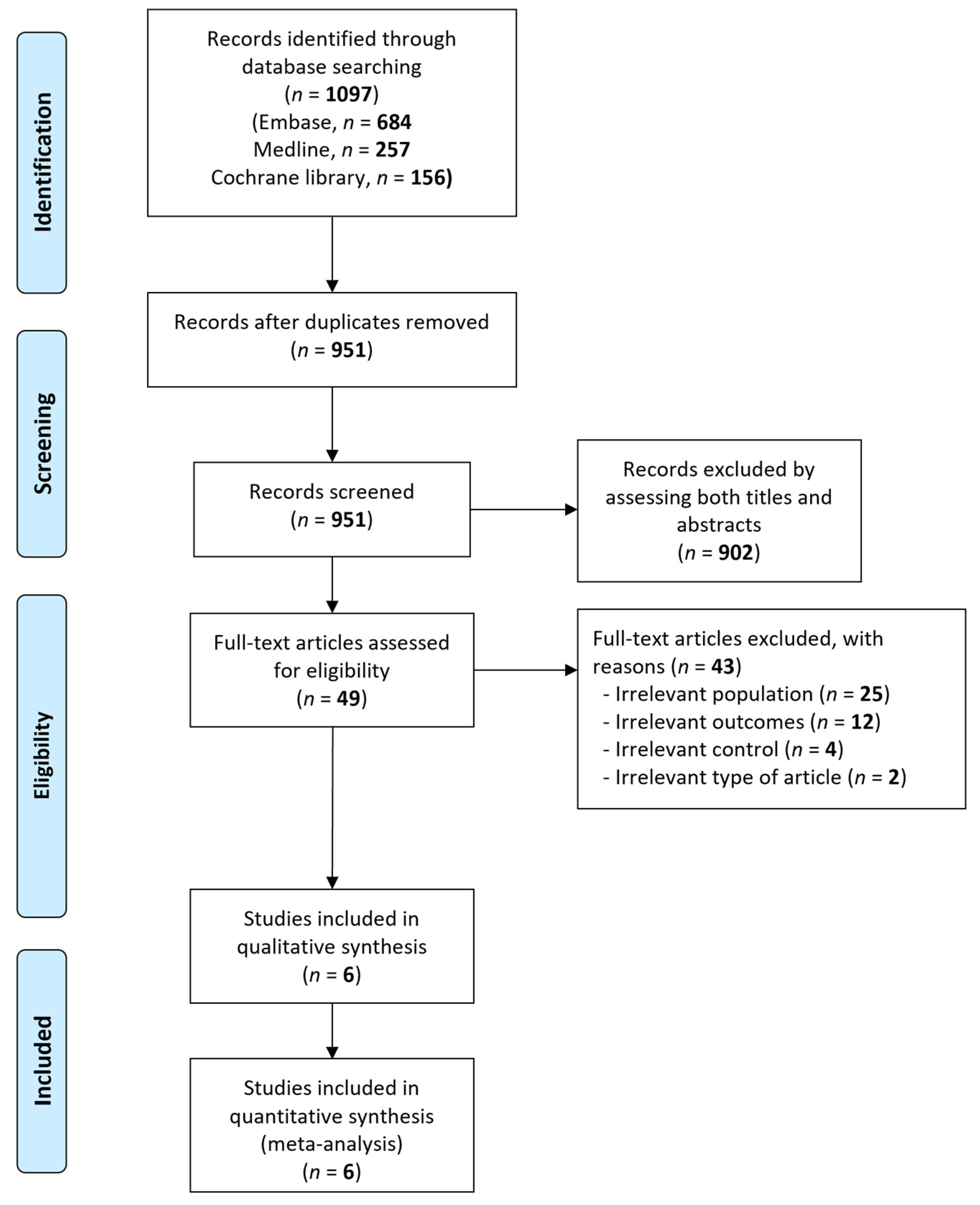
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Individual Studies
3.4. Results of Meta-Analyses
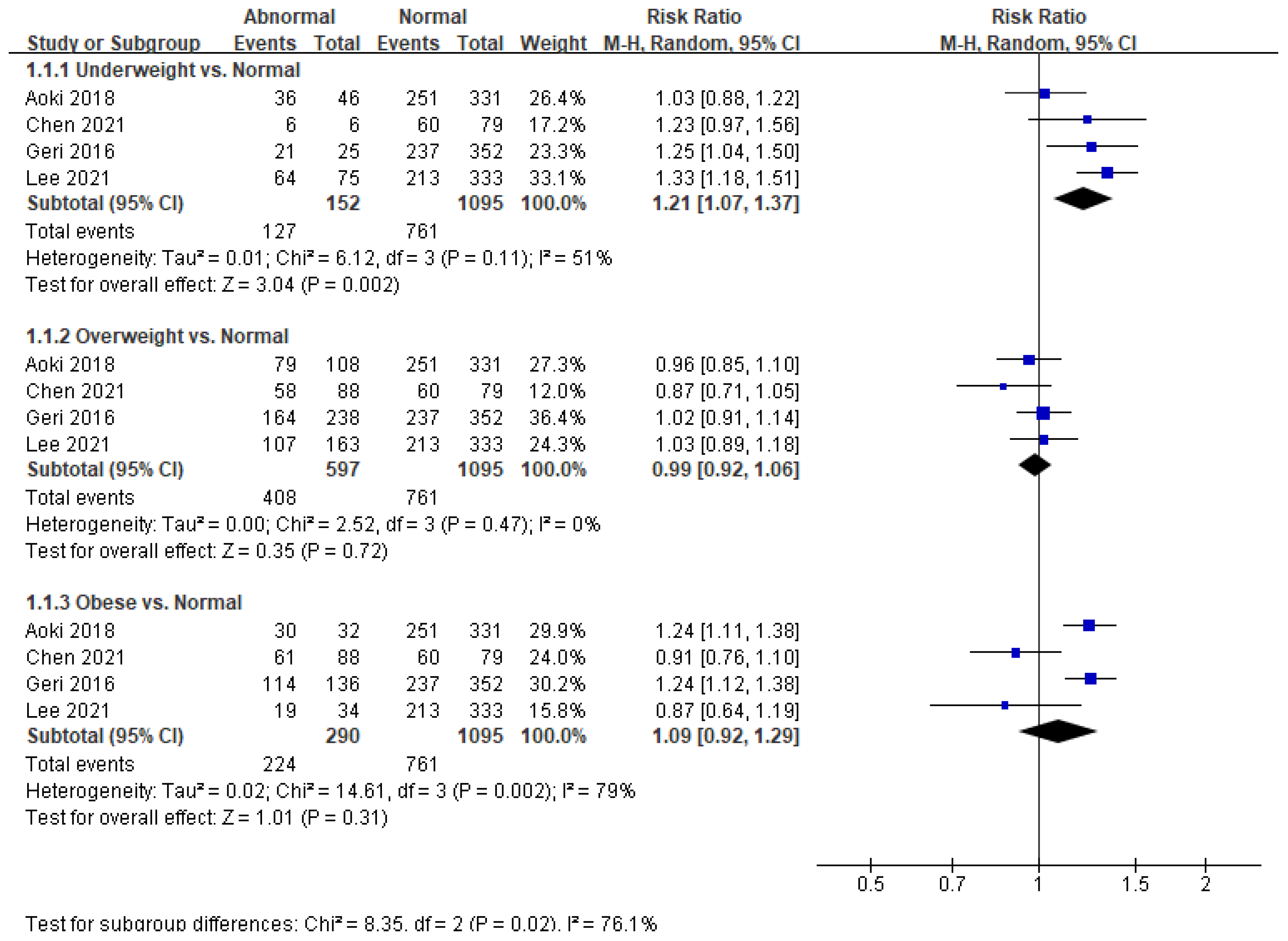
3.4.1. Association between BMI and Neurological Outcome in Patients with ROSC after OHCA
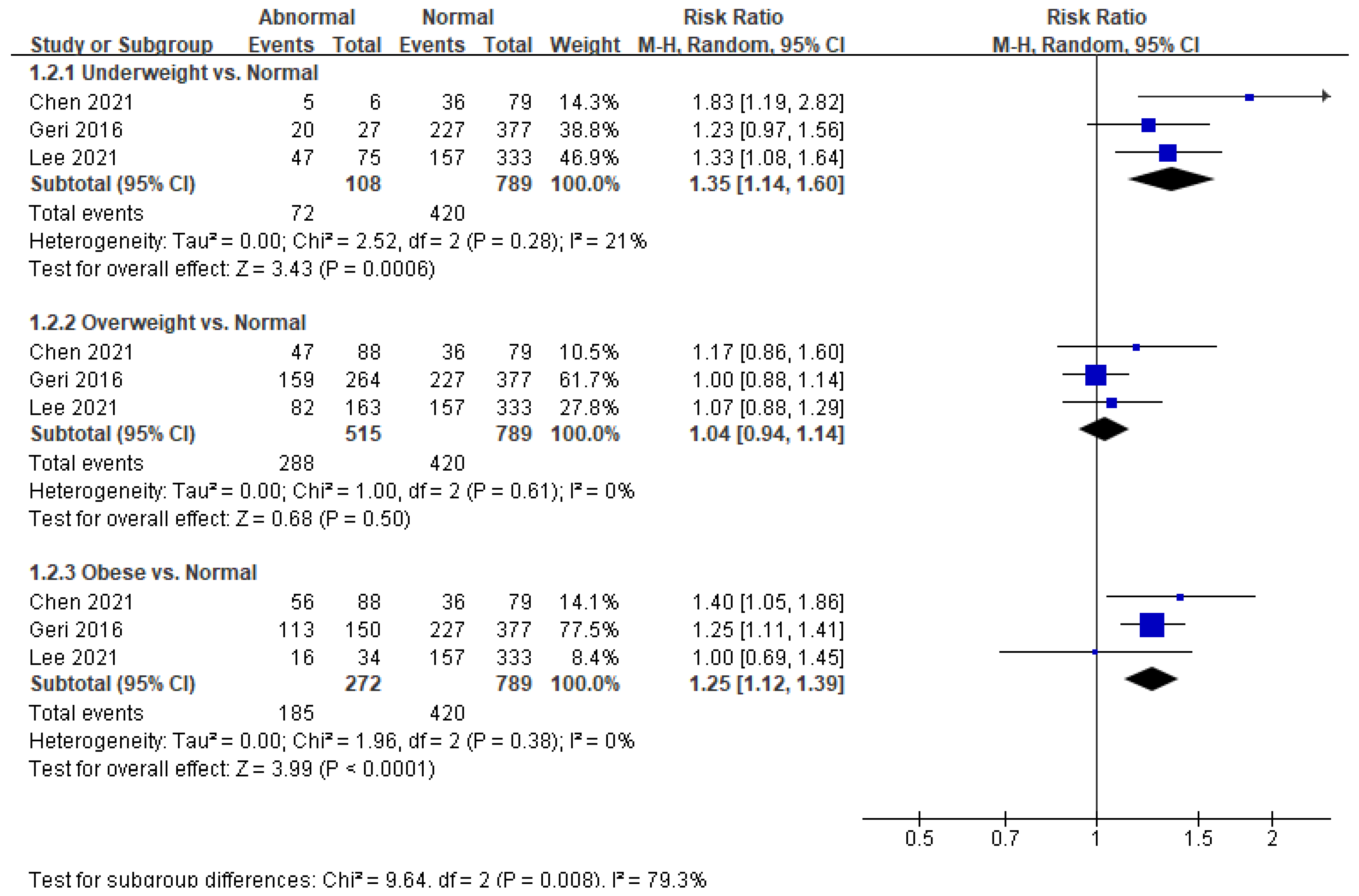
3.4.2. Association between BMI and in-Hospital Mortality in Patients with ROSC after OHCA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | body mass index |
| ROSC | return of spontaneous circulation |
| OHCA | out-of-hospital cardiac arrest |
| RR | risk ratio |
| IHCA | in-hospital cardiac arrest |
| PNO | poor neurological outcome |
| CPC | Cerebral Performance Category |
| CI | confidence interval |
| TTM | targeted temperature management |
References
- World Health Organization. WHO Key Facts-Obesity and Overweight. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 1 June 2021).
- Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity, and Obesity. Data, Trend and Maps [online]. Available online: https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html (accessed on 19 July 2021).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics-2020 update: A report from the american heart association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 american heart association scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism [internet]. Circulation 2006, 113, 898–918. [Google Scholar]
- Parker, B.K.; Manning, S.; Winters, M.E. The crashing obese patient. West. J. Emerg. Med. 2019, 20, 323–330. [Google Scholar] [CrossRef]
- Moon, T.S.; Fox, P.E.; Somasundaram, A.; Minhajuddin, A.; Gonzales, M.X.; Pak, T.J.; Ogunnaike, B. The influence of morbid obesity on difficult intubation and difficult mask ventilation. J. Anesth. 2019, 33, 96–102. [Google Scholar] [CrossRef]
- Lee, J.; Oh, J.; Lim, T.H.; Kang, H.; Park, J.H.; Song, S.Y.; Shin, G.H.; Song, Y. Comparison of optimal point on the sternum for chest compression between obese and normal weight individuals with respect to body mass index, using computer tomography: A retrospective study. Resuscitation 2018, 128, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; De Schutter, A.; Milani, R.V. Healthy obese versus unhealthy lean: The obesity paradox. Nat. Rev. Endocrinol. 2015, 11, 55–62. [Google Scholar] [CrossRef]
- Chalkias, A.; Xanthos, T. The obesity paradox in cardiac arrest patients. Int. J. Cardiol. 2014, 171, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Lee, J.H.; Han, S. Underweight: Another risk factor for cardiovascular disease? Medicine 2017, 96, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M.; Graubard, B.I.; Williamson, D.F.; Gail, M.H. Excess deaths associated with underweight, overweight, and obesity. J. Am. Med. Assoc. 2005, 293, 1861–1867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finkielman, J.D.; Gajic, O.; Afessa, B. Underweight is independently associated with mortality in post-operative and non-operative patients admitted to the intensive care unit: A retrospective study. BMC Emerg. Med. 2004, 4, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geri, G.; Savary, G.; Legriel, S.; Dumas, F.; Merceron, S.; Varenne, O.; Livarek, B.; Richard, O.; Mira, J.P.; Bedos, J.P.; et al. Influence of body mass index on the prognosis of patients successfully resuscitated from out-of-hospital cardiac arrest treated by therapeutic hypothermia. Resuscitation 2016, 109, 49–55. [Google Scholar] [CrossRef]
- Kakavas, S.; Georgiopoulos, G.; Oikonomou, D.; Karayiannis, D.; Masi, S.; Karlis, G.; Xanthos, T. The impact of body mass index on post resuscitation survival after cardiac arrest: A meta-analysis. Clin. Nutr ESPEN 2018, 24, 47–53. [Google Scholar] [CrossRef]
- Ma, Y.; Huang, L.; Zhang, L.; Yu, H.; Liu, B. Association between body mass index and clinical outcomes of patients after cardiac arrest and resuscitation: A meta-analysis. Am. J. Emerg. Med. 2018, 36, 1270–1279. [Google Scholar] [CrossRef]
- Høybye, M.; Stankovic, N.; Holmberg, M.; Christensen, H.C.; Granfeldt, A.; Andersen, L.W. In-hospital vs. out-of-hospital cardiac arrest: Patient characteristics and survival. Resuscitation 2021, 158, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Oh, J.; Kang, H.; Lim, T.H.; Ko, B.S.; Choi, H.J.; Park, S.M.; Jo, Y.H.; Lee, J.S.; Park, Y.S.; et al. Association between the body mass index and outcomes of patients resuscitated from out-of-hospital cardiac arrest: A prospective multicentre registry study. Scand. J. Trauma. Resusc. Emerg. Med. 2021, 29, 1–11. [Google Scholar] [CrossRef]
- Chen, C.T.; Lin, M.C.; Lee, Y.J.; Li, L.H.; Chen, Y.J.; Hou, P.C.; How, C.K. Association between body mass index and clinical outcomes in out-of-hospital cardiac arrest survivors treated with targeted temperature management. J. Chin. Med. Assoc. 2021, 84, 504–509. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. J. Am. Med. Assoc. 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Akram, D.S.; Astrup, A.V.; Atinmo, T.; Boissin, J.L.; Bray, G.A.; Carroll, K.K.; Chitson, P.; Chunming, C.; Dietz, W.H.; Hill, J.O.; et al. Obesity: Preventing and managing the global epidemic. World Heal. Organ. Tech. Rep. Ser. 2000, 894, 1–253. [Google Scholar]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials. 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, version 6.2; The Cochrane Collaboration: Cochrane, ON, USA, 2021; Available online: www.training.cochrane.org/handbook (accessed on 20 February 2021).
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Aoki, M.; Hagiwara, S.; Oshima, K.; Suzuki, M.; Sakurai, A.; Tahara, Y.; Nagao, K.; Yonemoto, N.; Yaguchi, A.; Morimura, N. Obesity was associated with worse neurological outcome among Japanese patients with out-of-hospital cardiac arrest. Intensive Care Med. 2018, 44, 665–666. [Google Scholar] [CrossRef] [PubMed]
- Galatianou, I.; Karlis, G.; Apostolopoulos, A.; Intas, G.; Chalari, E.; Gulati, A.; Iacovidou, N.; Chalkias, A.; Xanthos, T. Body mass index and outcome of out-of-hospital cardiac arrest patients not treated by targeted temperature management. Am. J. Emerg. Med. 2017, 35, 1247–1251. [Google Scholar] [CrossRef] [PubMed]
- Bunch, T.J.; White, R.D.; Lopez-Jimenez, F.; Thomas, R.J. Association of body weight with total mortality and with ICD shocks among survivors of ventricular fibrillation in out-of-hospital cardiac arrest. Resuscitation 2008, 77, 351–355. [Google Scholar] [CrossRef]
- Jung, Y.H.; Lee, B.K.; Lee, D.H.; Lee, S.M.; Cho, Y.S.; Jeung, K.W. The association of body mass index with outcomes and targeted temperature management practice in cardiac arrest survivors. Am. J. Emerg. Med. 2017, 35, 268–273. [Google Scholar] [CrossRef]
- Testori, C.; Sterz, F.; Losert, H.; Krizanac, D.; Haugk, M.; Uray, T.; Arrich, J.; Stratil, P.; Sodeck, G. Cardiac arrest survivors with moderate elevated body mass index may have a better neurological outcome: A cohort study. Resuscitation 2011, 82, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Leary, M.; Cinousis, M.J.; Mikkelsen, M.E.; Gaieski, D.F.; Abella, B.S.; Fuchs, B.D. The association of body mass index with time to target temperature and outcomes following post-arrest targeted temperature management. Resuscitation 2014, 85, 244–247. [Google Scholar] [CrossRef]
- Matinrazm, S.; Ladejobi, A.; Pasupula, D.K.; Javed, A.; Durrani, A.; Ahmad, S.; Munir, M.B.; Adelstein, E.; Jain, S.K.; Saba, S. Effect of body mass index on survival after sudden cardiac arrest. Clin. Cardiol. 2018, 41, 46–50. [Google Scholar] [CrossRef] [Green Version]
- Jain, R.; Nallamothu, B.K.; Chan, P.S. Body mass index and survival after in-hospital cardiac arrest. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 490–497. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.; Oh, J.; Lee, J.; Kang, H.; Lim, T.H.; Ko, B.S.; Cho, Y.; Song, S.Y. Retrospective study using computed tomography to compare sufficient chest compression depth for cardiopulmonary resuscitation in obese patients. J. Am. Heart Assoc. 2019, 8, 1–8. [Google Scholar] [CrossRef]
- Vanden Hoek, T.L.; Morrison, L.J.; Shuster, M.; Donnino, M.; Sinz, E.; Lavonas, E.J.; Jeejeebhoy, F.M.; Gabrielli, A. Part 12: Cardiac arrest in special situations 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010, 122 (Suppl. 3), S829–S861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hubert, H.B.; Feinleib, M.; McNamara, P.M.; Castelli, W.P. Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study. Circulation 1983, 67, 968–977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.-H.; Huang, C.-H.; Chang, W.-T.; Fu, C.-M.; Wang, H.-C.; Tsai, M.-S.; Yu, P.-H.; Wu, Y.W.; Ma, M.H.-M.; Chen, W.-J. Associations between body size and outcomes of adult in-hospital cardiac arrest: A retrospective cohort study. Resuscitation 2018, 130, 67–72. [Google Scholar] [CrossRef]
- Berrington de Gonzalez, A.; Hartge, P.; Cerhan, J.R.; Flint, A.J.; Hannan, L.; MacInnis, R.J.; Moore, S.C.; Tobias, G.S.; Anton-Culver, H.; Freeman, L.B.; et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 2010, 363, 2211–2219. [Google Scholar] [CrossRef] [Green Version]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Chae, M.K.; Lee, S.E.; Min, Y.G.; Park, E.J. Initial serum cholesterol level as a potential marker for post cardiac arrest patient outcomes. Resuscitation 2020, 146, 50–55. [Google Scholar] [CrossRef]
- Fernandes, L.A.; Braz, L.G.; Koga, F.A.; Kakuda, C.M.; Mõdolo, N.S.P.; De Carvalho, L.R.; Vianna, P.T.G.; Braz, J.R.C. Comparison of peri-operative core temperature in obese and non-obese patients. Anaesthesia 2012, 67, 1364–1369. [Google Scholar] [CrossRef]
- Geocadin, R.G.; Callaway, C.W.; Fink, E.L.; Golan, E.; Greer, D.M.; Ko, N.U.; Lang, E.; Licht, D.J.; Marino, B.S.; McNair, N.D.; et al. Standards for studies of neurological prognostication in comatose survivors of cardiac arrest: A scientific statement from the American heart association. Circulation 2019, 140, E517–E542. [Google Scholar] [CrossRef]


| Author. | Year | Country | Inclusion Period | Study Type | Sample Size | PNO, n (%) | Mortality, n (%) | BMI Classification | Time Point of Neurologic Outcome Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Aoki | 2018 | Japan | 2012 | mPOS | 517 | 36/46 (78.3) 251/331 (75.8) 79/108 (73.2) 30/32 (93.8) | NR | Underweight (<18.5) Normal (18.5–24.9) Overweight (25.0–29.9) Obese (≥30.0) | 1 month |
| Bunch | 2007 | USA | 1990–2006 | mPOS | 213 | 37/68 (54.4) 42/78 (53.9) 35/67 (52.2) | 37/68 (54.4) 42/78 (53.9) 35/67 (52.2) | Low to normal weight (<25) Overweight (25–30) Obese (>30) | at hospital discharge |
| Chen | 2021 | USA | 2011–2018 | mROS | 261 | 6/6 (100) 60/79 (75.9) 58/88 (65.9) 61/88 (69.3) | 5/6 (83.3) 36/79 (45.6) 47/88 (53.4) 56/88 (63.6) | Underweight (<18.5) Normal (18.5–24.9) Overweight (25.0–29.9) Obese (≥30.0) | at hospital discharge |
| Galatianou | 2017 | Greece | 2014 | sPOS | 13 | 0/1 (0.0) 5/12 (41.7) | 0/1 (0.0) 5/12 (41.7) | Normal (<25) Elevated BMI (≥25) | at ICU discharge |
| Geri | 2016 | France | 2005–2012 | mPOS | 818 | 21/25 (84.0) 237/352 (67.3) 164/238 (68.9) 114/136 (83.8) | 20/27 (74.1) 227/377 (60.2) 159/264 (60.2) 113/150 (75.3) | Underweight (<18.5) Normal (18.5–25) Overweight (25–30) Obese (>30) | at ICU discharge |
| Lee | 2021 | Korea | 2015–2018 | mPOS | 605 | 64/75 (85.3) 213/333 (64.0) 107/163 (65.6) 19/34 (55.9) | 47/75 (62.7) 157/333 (47.1) 82/163 (50.3) 16/34 (47.1) | Underweight (<18.5) Normal (18.5–25) Overweight (25–30) Obese (≥30) | at hospital discharge |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; Shin, H.; Oh, J.; Lim, T.-H.; Kang, B.-S.; Kang, H.; Choi, H.-J.; Kim, C.; Park, J.-H. Association between Body Mass Index and Outcomes in Patients with Return of Spontaneous Circulation after Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8389. https://doi.org/10.3390/ijerph18168389
Lee H, Shin H, Oh J, Lim T-H, Kang B-S, Kang H, Choi H-J, Kim C, Park J-H. Association between Body Mass Index and Outcomes in Patients with Return of Spontaneous Circulation after Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(16):8389. https://doi.org/10.3390/ijerph18168389
Chicago/Turabian StyleLee, Heekyung, Hyungoo Shin, Jaehoon Oh, Tae-Ho Lim, Bo-Seung Kang, Hyunggoo Kang, Hyuk-Joong Choi, Changsun Kim, and Jung-Hwan Park. 2021. "Association between Body Mass Index and Outcomes in Patients with Return of Spontaneous Circulation after Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 16: 8389. https://doi.org/10.3390/ijerph18168389
APA StyleLee, H., Shin, H., Oh, J., Lim, T.-H., Kang, B.-S., Kang, H., Choi, H.-J., Kim, C., & Park, J.-H. (2021). Association between Body Mass Index and Outcomes in Patients with Return of Spontaneous Circulation after Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(16), 8389. https://doi.org/10.3390/ijerph18168389







