Dentist Related Factors Associated with Implementation of COVID-19 Protective Measures: A National Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics, Study Design, and Sample
2.2. Participants
2.3. Development and Validation of the Online Survey
2.4. Missing Data
2.5. Statistical Analysis
2.6. Confidentiality and Data Retention
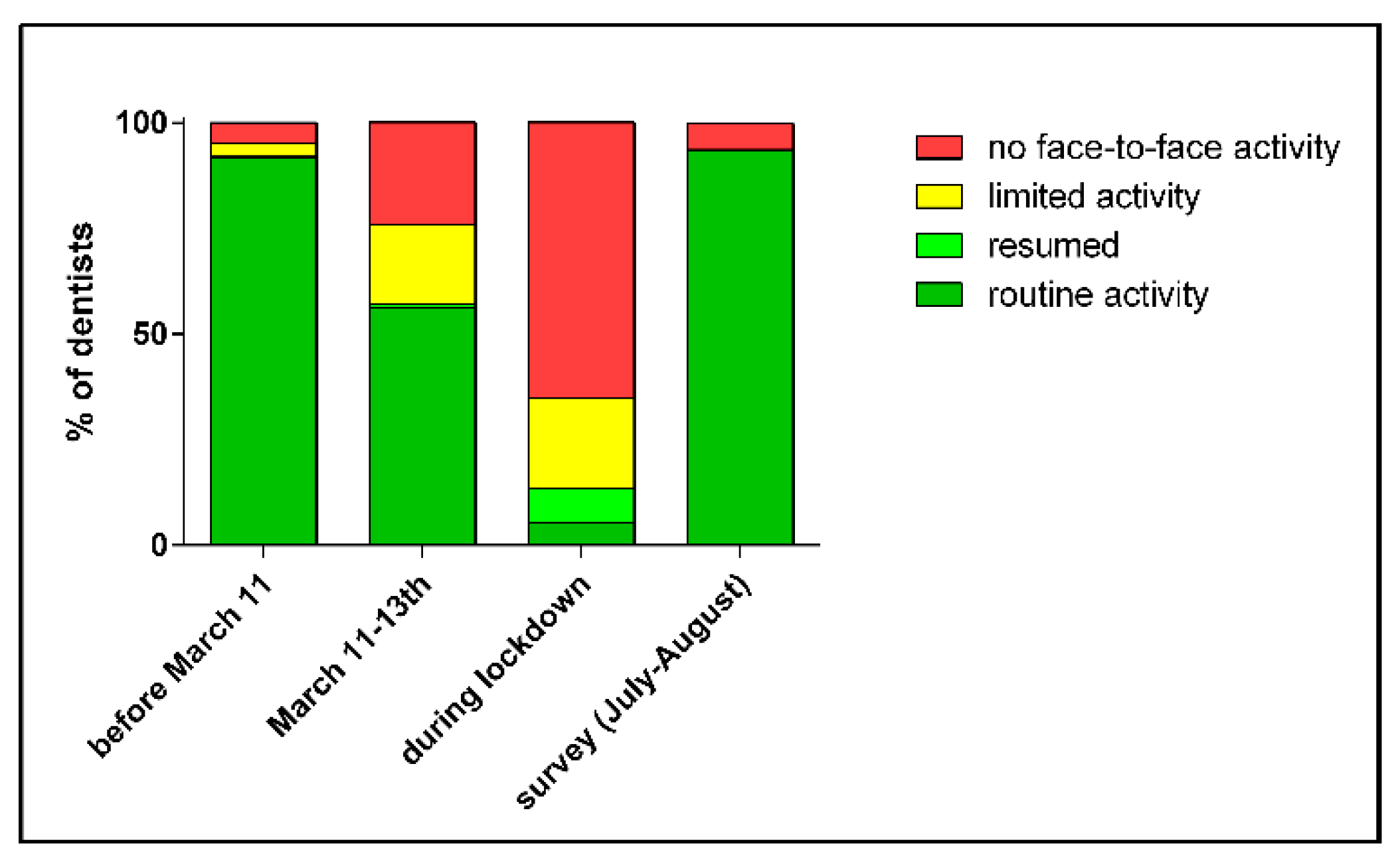
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation (WHO). WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. 2021. Available online: https://covid19.who.int/ (accessed on 17 June 2021).
- European Centre for Disease Prevention and Control. COVID-19. 2020. Available online: https://www.europa.eu (accessed on 17 June 2021).
- Centers for Disease Control and Prevention. SARS-CoV-2 Variant Classifications and Definitions. 2020. Available online: https://www.cdc.gov (accessed on 17 June 2021).
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCOV and controls in dental practice. Int. J. Oral. Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Gund, M.; Isack, J.; Hannig, M.; Thieme-Ruffing, S.; Gärtner, B.; Boros, G.; Rupf, S. Contamination of surgical mask during aerosol-producing dental treatments. Clin. Oral Investig. 2021, 25, 3173–3180. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banakar, M.; Lankarani, K.B.; Jafarpour, D.; Moayedi, S.; Banakar, M.H.; Mohammad Sadeghi, A. COVID-19 transmission risk and protective protocols in dentistry: A systematic review. BMC Oral Health 2020, 20, 275. [Google Scholar] [CrossRef] [PubMed]
- Buitrago-Garcia, D.; Egli-Gany, D.; Counotte, M.J.; Hossmann, S.; Imeri, H.; Ipekci, A.M.; Salanti, G.; Low, N. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med. 2020, 17, e1003346. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations during Severe Shortages. Interim Guidance. 2020. Available online: https://www.WHO-2019-nCov-IPC_PPE_use-2020.3-eng.pdf (accessed on 17 June 2021).
- Centers for Disease Control and Prevention. Guidance for Dental Settings|CDC. CDC’s Updated Guidance for Dental Settings Addresses Screening, Infection Control Protocols - CDA. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed on 17 June 2021).
- SCIENSANO. Maitrise des Infections à SARS-VOV-2 Pour la Pratique Dentaire. 2020. Available online: https://covid-19.sciensano.be/sites/default/files/Covid19/COVID19_procedure_dentists_FR.pdf (accessed on 17 June 2021).
- Cagetti, M.G.; Cairoli, J.L.; Senna, A.; Campus, G. COVID-19 Outbreak in North Italy: An Overview on Dentistry. A Questionnaire Survey. Int. J. Environ. Res. Public Health 2020, 17, 3835. [Google Scholar] [CrossRef]
- Shivalingesh, K.K.; Swati, S.; Sahil, T.; Divya, S.; Kaushikee, S.; Ahmed, J.H.; Alankrita, C.; Ruby, J.; Kuldeep, J.D. Assessing Knowledge, Attitudes and Practices of dental practitioners regarding the COVID-19 pandemic: A multinational study. Dent. Med. Probl. 2020, 57, 11–17. [Google Scholar]
- Estrich, C.G.; Mikkelsen, M.; Morrissey, R.; Geisinger, M.L.; Ioannidou, E.; Vujicic, M.; Araujo, M.W.A. Estimating COVID-19 prevalence and infection control practices among US dentists. J. Am. Dent. Assoc. 2020, 151, 815–824. [Google Scholar] [CrossRef]
- Campus, G.; Diaz-Betancourt, M.; Cagetti, M.G.; Giacaman, R.A.; Manton, D.J.; Douglas, G.A.V.; Carvalho, T.S.; Carvalho, J.C.; Vukovic, A.; COVIDental Collaboration Group. The COVID-19 pandemic and its global effects on dentistry. An international survey. J. Dent. 2021, 103749. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gotzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. STROBE Initiative, Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [Green Version]
- Direction générale Soins de Santé. Statistiques annuelles des Professionnels des Soins de Santé en Belgique 2019. Service Public Fédéral Santé Publique, Sécurité de la Chaîne Alimentaire et Environnement. 2019. Available online: http://www.health.belgium.be/fr/sante (accessed on 17 June 2011).
- Campus, G.; Diaz-Betancourt, M.; Cagetti, M.G.; Carvalho, J.C.; Carvalho, T.S.; Cortés-Martinicorena, J.F.; Deschner, J.; Douglas, G.V.A.; Giacaman, R.S.; Machiulskiene, V.; et al. Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey. Int. J. Environ. Res. Public Health 2020, 17, 5598. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Coronavirus Disease (COVID-19): How Is It Transmitted? Updated 30 April 2021. 2021. Available online: https://www.who.int/ (accessed on 17 June 2021).
- SCIENSANO. Incidence du COVID-19 Dans la Population Active par Secteur D’activité Professionnelle. Rapport Incidence du COVID-19 Dans la Population Active.pdf. 2021. Available online: https://www.sciensano.be/en (accessed on 17 June 2021).
- Wolf, T.G.; Zeyer, O.; Campus, G. COVID-19 in Switzerland and Liechtenstein: A Cross-Sectional Survey among Dentists’ Awareness, Protective Measures and Economic Effects. Int. J. Environ. Res. Public Health 2020, 17, 9051. [Google Scholar] [CrossRef]
- Persoon, L.F.; Volgenant, C.M.V.; van der Veen, M.H.; Opdam, N.J.M.; Manton, D.J.; Brues, J.J.M. Impact van het coronavirus op de praktijkvoering van de Nederlandse mondzorg. Ned. Tijdschr. Tandheelkd. 2021, 28, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Conway, D.I.; Culshaw, S.; Edwards, M.; Clark, C.; Watling, C.; Robertson, C.; Braid, R.; O’Keefe, E.; McGoldrick, N.; Burns, J.; et al. SARS-CoV-2 Positivity in Asymptomatic-Screened Dental Patients. J. Dent. Res. 2021, 100, 583–590. [Google Scholar] [CrossRef]
- Araujo, M.W.B.; Estrich, C.G.; Mikkelsen, M.; Morrissey, R.; Harrison, B.; Geisinger, M.L.; Ioannidou, E.; Vujicic, M. COVID-2019 among dentists in the United States: A 6-month longitudinal report of accumulative prevalence and incidence. J. Am. Dent. Assoc. 2021, 152, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Peditto, M.; Scapellato, S.; Marcianò, A.; Costa, P.; Oteri, G. Dentistry during the COVID-19 Epidemic: An Italian Workflow for the Management of Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 3325. [Google Scholar] [CrossRef] [PubMed]
- Jungo, S.; Moreau, N.; Mazevet, M.E.; Ejeil, A.-N.; Duplan, M.B.; Salmon, B.; Smail-Faugeron, V. Prevalence and risk indicators of first-wave COVID-19 among oral health-care workers: A French epidemiological survey. PLoS ONE 2021, 16, e0246586. [Google Scholar] [CrossRef]
- National Institute for Health and Disability Insurance (Belgium). Accueil—INAMI. 2021. Available online: https://www.fgov.be (accessed on 17 June 2021).
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. [Google Scholar] [CrossRef]
- Huang, Q.; Marzouk, T.; Cirligeanu, R.; Malmstrom, H.; Eliav, E.; Ren, Y.-F. Ventilation Assessment by Carbon Dioxide Levels in Dental Treatment Rooms. J. Dent. Res. 2021, 100, 810–816. [Google Scholar] [CrossRef]
- Holliday, R.; Allison, J.R.; Currie, C.C.; Edwards, D.C.; Bowes, C.; Pickering, K.; Reay, S.; Durham, J.; Lumb, J.; Rostami, N.; et al. Evaluating contaminated dental aerosol and splatter in an open plan clinic environment: Implications for the COVID-19 pandemic. J. Dent. 2021, 105, 103565. [Google Scholar] [CrossRef]
- Innes, N.; Johnson, I.G.; Al-Yaseen, W.; Harris, R.; Jones, R.; Kc, S.; McGregor, S.; Robertson, M.; Wade, W.G.; Gallagher, J.E. A systematic review of droplet and aerosol generation in dentistry. J. Dent. 2021, 105, 103556. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Ma, B.; Cheng, Y.; Bian, Z. Epidemiological Investigation of OHCWs with COVID-19. J. Dent. Res. 2020, 99, 1444–1452. [Google Scholar] [CrossRef]
- Sabino-Silva, R.; Jardim, A.C.G.; Siqueira, W.L. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin. Oral Investig. 2020, 24, 1619–1621. [Google Scholar] [CrossRef] [Green Version]
- Wu, K.Y.; Wu, D.T.; Nguyen, T.T.; Tran, D.S. COVID-19’s impact on private practice and academic dentistry in North America. Oral Dis. 2021, 27, 684–687. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, T.F.; Battineni, G.; Teja, K.V.; Marto, C.M.; Spagnuolo, G. A Review of Prolonged Post-COVID-19 Symptoms and Their Implications on Dental Management. Int. J. Environ. Res. Public Health 2021, 18, 5131. [Google Scholar] [CrossRef]
- Schwendicke, F.; Krois, J.; Gomez, J. Impact of SARS-CoV2 (Covid-19) on dental practices: Economic analysis. J. Dent. 2020, 99, 103387. [Google Scholar] [CrossRef] [PubMed]
- Dalewski, B.; Lukasz Palka, L.; Kiczmer, P.; Sobolewska, E. The Impact of SARS-CoV-2 Outbreak on the Polish Dental Community’s Standards of Care-A Six-Month Retrospective Survey-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 1281. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Wordley, V.; Thompson, W. How did COVID-19 impact on dental antibiotic prescribing across England? Br. Dent. J. 2020, 229, 601–604. [Google Scholar] [CrossRef] [PubMed]
- Palmer, N.O.A.; Seoudi, N. The effect of SARS-CoV-2 on the prescribing of antimicrobials and analgesics by NHS general dental practitioners in England. Br. Dent. J. 2021, 21, 1–6. [Google Scholar] [CrossRef]
- Leroy, R.; Bourgeois, J.; Verleye, L.; Declerck, D.; Depuydt, P.; Eloot, A.; Carvalho, J.C.; Teughels, W.; Cauwels, R.; Leprince, J.; et al. Guideline on the Prudent Prescription of Antibiotics in the Dental Office. Good Clinical Practice (GCP) Brussels: Belgian Health Care Knowledge Centre (KCE). 2020. KCE Reports 332. D/2020/10.273/23. Available online: https://kce.fgov.be/sites/default/files/atoms/files/KCE_332_Antibiotics_in_dental_office_Report_2.pdf (accessed on 17 June 2021).
- Leroy, R.; Bourgeois, J.; Verleye, L.; Carvalho, J.C.; Eloot, A.; Cauwels, R.; Declerck, D. Are systemic antibiotics indicated in children presenting with an odontogenic abscess in the primary dentition? A systematic review of the literature. Clin. Oral Investig. 2021, 25, 2537–2544. [Google Scholar] [CrossRef]
| Variables | Categories | Number (%) |
|---|---|---|
| Region (missing = 1) | Brussels | 205 (14.3%) |
| Flanders | 775 (54.0%) | |
| Wallonia | 455 (31.7%) | |
| Age group (years) | ≤34 | 207 (14.4%) |
| 35–44 | 154 (10.7%) | |
| 45–54 | 274 (19.1%) | |
| 55–64 | 516 (35.9%) | |
| ≥65 | 285 (19.8%) | |
| Gender | Female | 845 (58.8%) |
| Male | 591 (41.2%) | |
| Language spoken (missing = 1) | Dutch | 765 (53.3%) |
| French | 670 (46.7%) | |
| Professional activity (Missing = 34) | General dentist | 1322 (94.3%) |
| Orthodontist | 46 (3.3%) | |
| Periodontist | 29 (2.0%) | |
| Maxillofacial surgeon | 5 (0.4%) | |
| Practice type (missing = 34) | Private owner | 918 (65.5%) |
| Private coworker | 409 (29.2%) | |
| Hospital practice | 36 (2.5%) | |
| Other | 39 (2.8%) | |
| Reported infection rate * | Brussels | 55 (0.04%) |
| Flanders | 25 (0.02%) | |
| Wallonia | 46 (0.03%) | |
| Working status at the moment of the survey (missing = 54) | None | 61 (4.4%) |
| Yes, remote advice | 12 (0.9%) | |
| Yes, face to face | 1309 (94.7%) |
| Protective Measure | Number | % |
|---|---|---|
| Appointment organization | 537 | 49.5 |
| Waiting area organization | 422 | 38.9 |
| Surface cleansing | 934 | 86.2 |
| Hand hygiene procedures | 894 | 82.5 |
| Mouth rinse protocol | 809 | 74.6 |
| Aerosol control (mask, visor, gown, rubber dam, and limiting rotating instruments) | 401 | 33.5 |
| All measures | 86 | 7.9 |
| Variables | Dentists Having Experienced COVID-19 Infection | ||
|---|---|---|---|
| β | SE | p Value | |
| Age group 55–64 years | 0.149 | 0.286 | <0.0001 |
| Age > 65 years | 0.522 | 0.492 | 0.023 |
| Implementation of cleansing protocol | 0.030 | 0.310 | 0.003 |
| Variables | Dentists Having Experienced COVID-19 Infection | ||
|---|---|---|---|
| β | SE | p Value | |
| Dentists with high self-perceived risk of virus acquisition in the dental setting | 2.090 | 0.291 | 0.011 |
| Dentists with low concern of getting infected in the dental setting | 0.576 | 0.251 | 0.027 |
| Dentists with low confidence of being able to prevent transmission in the dental setting | 0.535 | 0.273 | 0.022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carvalho, J.C.; Declerck, D.; Jacquet, W.; Bottenberg, P. Dentist Related Factors Associated with Implementation of COVID-19 Protective Measures: A National Survey. Int. J. Environ. Res. Public Health 2021, 18, 8381. https://doi.org/10.3390/ijerph18168381
Carvalho JC, Declerck D, Jacquet W, Bottenberg P. Dentist Related Factors Associated with Implementation of COVID-19 Protective Measures: A National Survey. International Journal of Environmental Research and Public Health. 2021; 18(16):8381. https://doi.org/10.3390/ijerph18168381
Chicago/Turabian StyleCarvalho, Joana Christina, Dominique Declerck, Wolfgang Jacquet, and Peter Bottenberg. 2021. "Dentist Related Factors Associated with Implementation of COVID-19 Protective Measures: A National Survey" International Journal of Environmental Research and Public Health 18, no. 16: 8381. https://doi.org/10.3390/ijerph18168381
APA StyleCarvalho, J. C., Declerck, D., Jacquet, W., & Bottenberg, P. (2021). Dentist Related Factors Associated with Implementation of COVID-19 Protective Measures: A National Survey. International Journal of Environmental Research and Public Health, 18(16), 8381. https://doi.org/10.3390/ijerph18168381







