Measuring the Association of Self-Perceived Physical and Social Neighborhood Environment with Health of Chinese Rural Residents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
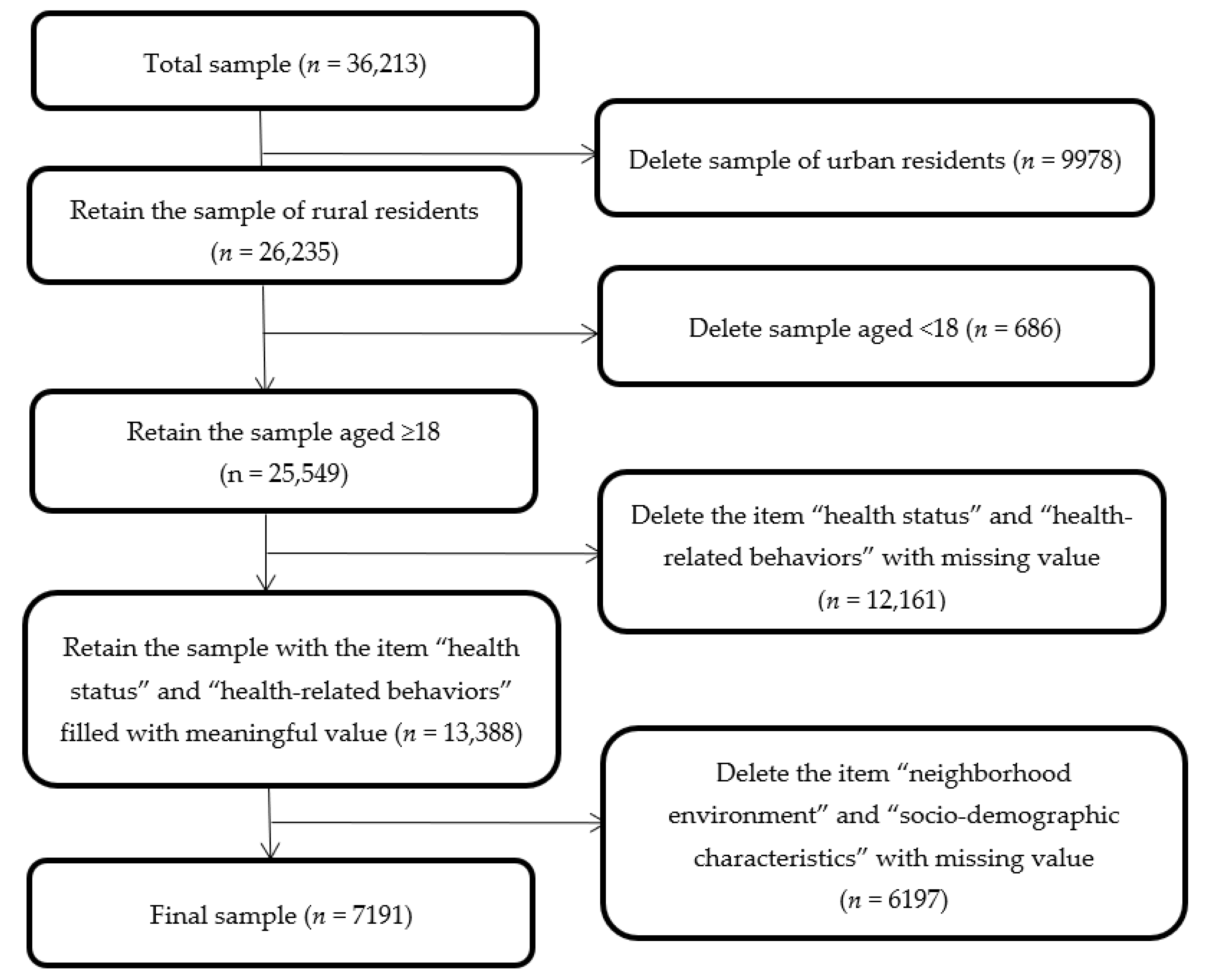
2.2. Study Population
2.3. Measures
2.3.1. Health Status
2.3.2. Health-Related Behaviors
2.3.3. Neighborhood Environment
2.3.4. Socio-Demographic Characteristics
2.4. Statistical Analyses
3. Results
3.1. Characteristics of Participants
3.2. Health Status of Participants
3.3. Health-Related Behaviors of Participants
3.4. Neighborhood Environment Status of Participants
3.5. The Associations of Self-Perceived Neighborhood Environment with Health Status
3.6. The Associations between Self-Perceived Neighborhood Environment and Health-Related Behaviors
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brug, J.; Lenthe, F.J.; Kremers, S.P.J. Revisiting Kurt Lewin: How to gain insight into environmental correlates of obesogenic behaviors. Am. J. Prev. Med. 2006, 31, 525–529. [Google Scholar] [CrossRef]
- Van den Berg, M.; Wendel-Vos, W.; van Poppel, M.; Kemper, H.; van Mechelen, W.; Maas, J. Health benefits of green spaces in the living environment: A systematic review of epidemiological studies. Urban For. Urban Green 2015, 14, 806–816. [Google Scholar] [CrossRef]
- Putrik, P.; de Vries, N.K.; Mujakovic, S.; van Amelsvoort, L.; Kant, I.; Kunst, A.E.; van Oers, H.; Jansen, M. Living environment matters: Relationships between neighborhood characteristics and health of the residents in a Dutch municipality. J. Commun. Health 2015, 40, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Yao, X.; Sun, B.; Zhong, Z.; Yin, C. The impact of rural built environment on obesity in China: An Empirical Study Based on BMI data of villagers. Shanghai Urban Plan. 2020, 154, 8–14. [Google Scholar]
- Zhang, Y.; Dai, G.; Mao, W.; Yang, D.; Qin, X. Multi factor analysis of the influence of community environment on depression of Chengdu residents. Chin. J. Soc. Med. 2011, 28, 23–26. [Google Scholar]
- Wu, N.; Dai, J.; Chen, Z.; Li, Z.; Qian, J.; Gao, J.; Wang, Z.; Fu, H. Relationship between living environment and subjective well being of residents in Dongtai City, Jiangsu Province. Environ. Occup. Med. 2018, 35, 729–734. [Google Scholar]
- Benjamin, A.; Gabriele, D.; Fanny, J. Effects of changes in living environment on physical health: A prospective German cohort study of non-movers. Eur. J. Public Health 2019, 29, 1147–1153. [Google Scholar]
- Naydenov, K.; Melikov, A.; Markov, D.; Stankov, P.; Bornehag, C.G.; Sundell, J. A comparison between occupants’ and inspectors’ reports on home dampness and their association with the health of children: The ALLHOME study. Build. Environ. 2007, 43, 1840–1849. [Google Scholar] [CrossRef]
- Qin, B.; Zhu, W.; Dong, H. The Influence of Neighborhood Environment and Transportation on Residents’ Mental Wellbeing: Based on Questionnaire of 16 Communities in Beijing. Urban Rural Plan. 2018, 3, 34–42. [Google Scholar]
- Xing, C. Home ownership, don’t forget to protect health-living environment and health. Furnit. Environ. 1997, 06, 17–18. [Google Scholar]
- Pulles, M.P.J.; Biesiot, W.; Stewart, R. Adverse effects of environmental noise on health: An interdisciplinary approach. Environ. Int. 1990, 16, 437–445. [Google Scholar] [CrossRef]
- Halonen, J.I.; Lanki, T.; Yli-Tuomi, T.; Turunen, A.W.; Pentti, J.; Kivimäki, M.; Vahtera, J. Associations of traffic noise with self-rated health and psychotropic medication use. Scand. J. Work. Environ. Health 2014, 40, 235–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seidler, A.; Hegewald, J.; Seidler, A.L. Association between aircraft, road and railway traffic noise and depression in a large case-control study based on secondary data. Environ. Res. 2017, 152, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Yang, B.; Liu, P.; Zhang, J.; Lu, Y. The longitudinal relationship between exposure to air pollution and depression in older adults. Int. J. Geriatr. Psych. 2020, 35, 610–616. [Google Scholar] [CrossRef]
- Zhou, Y.; Liu, J. Air Pollution and Mental Health of Older Adults in China. Sustainability 2020, 12, 950. [Google Scholar] [CrossRef] [Green Version]
- Sallis, J.F.; Philip, R.N.; Broyles, S.L.; Berry, C.C. Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psy. 1993, 12, 390–398. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Donovan, R.J. The relative influence of individual, social and physical environment determinants of physical activity. Soc. Sci. Med. 2002, 54, 1793–1812. [Google Scholar] [CrossRef]
- Gomez, J.E.; Johnson, B.A.; Selva, M.; Sallis, J.F. Violent crime and outdoor physical activity among inner-city youth. Prev. Med. 2004, 39, 876–881. [Google Scholar] [CrossRef]
- Kouvatsou, K.; Iliadou, M.; Kalatzi, P.; Sakellari, E.; Tziaferi, S. Depression Among Elderly Users of Open and Closed Care Facilities in a Rural Region of Greece: An Important Public Health Issue. Mater. Socio-Med. 2020, 32, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Dijst, M.; Faber, J.; Geertman, S.; Cui, C. Healthy urban living: Residential environment and health of older adults in Shanghai. Health Place 2017, 47, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; Liu, W. Physical Exercise, Social Interaction, Access to Care, and Community Service: Mediators in the Relationship Between Socioeconomic Status and Health Among Older Patients with Diabetes. Front. Public Health 2020, 8, 589742. [Google Scholar] [CrossRef]
- Madu, E.; Mezue, K.; Madu, K. Social determinants and cardiovascular care: A focus on vulnerable populations and the Jamaica experience. FASEB BioAdvances 2021, 3, 266–274. [Google Scholar] [CrossRef]
- Park, N.S.; Jang, Y.; Lee, B.S.; Chiriboga, D.A. Relationship between perceived neighborhood environment and depressive symptoms in older Korean Americans: Do chronic disease and functional disability modify it? Asian Am. J. Psychol. 2015, 6, 174–180. [Google Scholar] [CrossRef]
- Dawson, C.T.; Wu, W.; Fennie, K.P.; Ibañez, G.; Cano, M.Á.; Pettit, J.W.; Trepka, M.J. Perceived neighborhood social cohesion moderates the relationship between neighborhood structural disadvantage and adolescent depressive symptoms. Health Place 2019, 56, 88–98. [Google Scholar] [CrossRef]
- Yan, S.; Zheng, X. Promoting physical and mental health: The impact of community public space on social cohesion. Urban Stud. 2021, 28, 117–124. [Google Scholar]
- Manferdelli, G.; Torre, A.L.; Codella, R. Outdoor physical activity bears multiple benefits to health and society. J. Sport. Med. Phys. Fit. 2019, 59, 868–879. [Google Scholar] [CrossRef]
- Donley, A.M.; Nicholson, H.L. Comparing the Health of Relocated Public Housing Residents and Current Residents of a Historically Black Community: The Moderating Role of Social Cohesion. J. Black Stud. 2019, 50, 26–44. [Google Scholar] [CrossRef]
- Norbäck, D.; Zock, J.-P.; Plana, E.; Heinrich, J.; Svanes, C.; Sunyer, J.; Künzli, N.; Villani, S.; Olivieri, M.; Soon, A.; et al. Mould and dampness in dwelling places, and onset of asthma: The population-based cohort ECRHS. Occup. Environ. Med. 2013, 70, 325–331. [Google Scholar] [CrossRef] [Green Version]
- Saito, K.; Iwata, N.; Hosokawa, T.; Ohi, G. Housing factors and perceived health status among Japanese women living in aggregated dwelling units. Int. J. Health Serv. 1993, 23, 541–554. [Google Scholar] [CrossRef]
- Salehi, A.; Harris, N.; Sebar, B.; Coyne, E. The relationship between living environment, well-being and lifestyle behaviours in young women in Shiraz, Iran. Health Soc. Care Comm. 2017, 25, 275–284. [Google Scholar] [CrossRef] [Green Version]
- Schulz, A.J.; Mentz, G.; Lachance, L.; Zenk, S.N.; Johnson, J.; Stokes, C.; Mandell, R. Do observed or perceived characteristics of the neighborhood environment mediate associations between neighborhood poverty and cumulative biological risk? Health Place 2013, 24C, 147–156. [Google Scholar] [CrossRef] [Green Version]
- Ruijsbroek, A.; Mohnen, S.M.; Droomers, M.; Kruize, H.; Gidlow, C. Neighbourhood green space, social environment and mental health: An examination in four European cities. Int. J. Public Health 2017, 62, 657–667. [Google Scholar] [CrossRef] [Green Version]
- Tilt, B. The politics of industrial pollution in rural China. J. Peasant Stud. 2013, 40, 1147–1164. [Google Scholar] [CrossRef]
- Tan, Y.; Xu, H.; Zhang, X. Sustainable urbanization in China: A comprehensive literature review. Cities 2016, 55, 82–93. [Google Scholar] [CrossRef]
- Moreno, G.; Morales, L.S.; Fatima, N.; Tseng, C.H.; Isiordia, M.; Noguera, C.; Mangione, C.M. Neighborhood Perceptions and Health-Related Outcomes Among Latinos with Diabetes from a Rural Agricultural Community. J. Commun. Health 2014, 39, 1077–1084. [Google Scholar] [CrossRef] [Green Version]
- Luo, Y.; Zhang, L.; Pan, X. Neighborhood Environments and Cognitive Decline Among Middle-Aged and Older People in China. J. Gerontol. B-Psychol. 2019, 74, e60–e71. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Lu, D.; Kang, M. Social capital and the mental health of children in rural China withdifferent experiences of parental migration. Soc. Sci. Med. 2015, 132, 270–277. [Google Scholar] [CrossRef]
- Van, D.; Levecque, K.; Bracke, P. Measurement equivalence of the CES-D 8 in the general population in Belgium: A gender perspective. Arch. Public Health 2009, 67, 98–111. [Google Scholar]
- Coninck, D.D.; Matthijs, K.; Luyten, P. Depression in Belgian First-Year University Students: A Longitudinal Study of Self-Definition, Interpersonal Relatedness, Mentalizing, and Integration. J. Clin. Psychol. 2021, 77, 1715–1731. [Google Scholar] [CrossRef]
- Tavolacci, M.P.; Wouters, E.; Velde, S. The Impact of COVID-19 Lockdown on Health Behaviors among Students of a French University. Int. J. Environ. Res. Public Health 2021, 8, 4346. [Google Scholar] [CrossRef] [PubMed]
- Kathe, N.; Payakachat, N. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual. Life Res. 2009, 18, 727–735. [Google Scholar]
- Fleishman, J.A.; Zuvekas, S.H. Global self-rated mental health: Associations with other mental health measures and with role functioning. Med. Care 2007, 45, 602–609. [Google Scholar] [CrossRef]
- Xie, J.; Wu, E.Q.; Zheng, Z.-J.; Sullivan, P.W.; Zhan, L.; Labarthe, D.R. Patient-Reported health status in coronary heart disease in the united states: Age, sex, racial, and ethnic differences. Circulation 2008, 118, 491–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, A.Z.; Liu, G.G.; Christensen, D.B. Inappropriate medication use and health outcomes in the elderly. J. Am. Geriatr. Soc. 2004, 52, 1934–1939. [Google Scholar] [CrossRef]
- Park, S.; Chan, K.; Williams, E.C. Gain of employment and perceived health status among previously unemployed persons: Evidence from a longitudinal study in the United States. Public Health 2016, 133, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, B.W.; White, M.; Stahl-Timmins, W.; Depledge, M.H. Does living by the coast improve health and wellbeing. Health Place 2012, 18, 1198–1201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, H.; Qi, Y.; Chen, J.; Shao, S.; Lin, S. Incentive and coordination: Ecological fiscal transfers’ effects on eco-environmental quality. Environ. Impact. Asses. 2021, 87, 106518. [Google Scholar] [CrossRef]
- Guo, P. Current situation and Development Countermeasures of rural public sports facilities in Henan Province under Rural Revitalization. Agr. Econ. 2020, 3, 62–64. [Google Scholar]
- Cho, S.; Kim, S. Does a healthy lifestyle matter? A daily diary study of unhealthy eating at home and behavioral outcomes at work. J. Appl. Psych. 2021, 1–51. [Google Scholar] [CrossRef]
- Haynes, P.L.; Wolf, R.L.; Howe, G.W. Unemployed Individuals Reporting Hindrance Work Stress at Previous Job Have Increased Likelihood of Insomnia Disorder. Int. J. Behav. Med. 2021, 28, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Andersson, A.; Mrdby, A.C.; Holmgren, K. Associations between leisure activities and binge drinking in adults: Findings from a Swedish newly sick-listed sample. Work. (Read. Mass) 2014, 48, 143–153. [Google Scholar] [CrossRef]
- Laaksonen, M.; Talala, K.; Martelin, T.; Rahkonen, O.; Roos, E.; Helakorpi, S.; Laatikainen, T.; Prättälä, R. Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: A follow-up of 60 000 men and women over 23 years. Eur. J. Public Health 2008, 18, 38–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | Total Population n (%) | Variables | Total Population n (%) |
|---|---|---|---|
| DE | Household income, mean ± SD | 41,516.15 ± 46,411.37 | |
| Bad | 1085 (15.09) | Subjective Social Class | |
| Good | 6106 (84.91) | Low | 2135 (29.69) |
| PFC | Fair | 3356 (46.67) | |
| Bad | 957 (13.31) | High | 1700 (23.64) |
| Good | 6234 (86.69) | Depressive mood, mean ± SD | 5.32 ± 3.96 |
| PS | Self-rated health | ||
| Bad | 584 (8.12) | Unhealthy | 1119 (15.56) |
| Good | 6607 (91.88) | Fair | 1216 (16.91) |
| NR | Healthy | 4856 (67.53) | |
| Bad | 92 (1.28) | Chronic | |
| Good | 7099 (98.72) | No | 6060 (84.27) |
| Age groups in years | Yes | 1131 (15.73) | |
| <60 | 5743 (79.86) | Time sleeping weekday | |
| ≥60 | 1448 (20.14) | <9 h | 1376 (19.14) |
| Gender | ≥9 h | 5815 (80.86) | |
| Male | 3870 (53.82) | Physical exercise | |
| Female | 3321 (46.18) | No | 4818 (67.00) |
| Marital status | At least one time | 2373 (33.00) | |
| Unmarried | 520 (7.23) | Smoking frequencies | |
| Married | 6386 (88.81) | No | 4789 (66.60) |
| Divorce or bereavement | 285 (3.96) | Yes | 2402 (33.40) |
| Education level | Alcohol consumption | ||
| Middle school and below | 6267 (87.15) | No | 6021 (83.73) |
| High school/vocational school | 646 (8.98) | Yes | 1170 (16.27) |
| College and above | 278 (3.87) | BMI, mean ± SD | 23.28 ± 3.43 |
| Region | Underweight | 442 (6.15) | |
| Eastern | 2854 (39.69) | Normal | 3929 (54.64) |
| Central | 1533 (21.32) | Overweight | 2205 (30.66) |
| Western | 2803 (38.98) | Obesity | 615 (8.55) |
| Variables | Depressive Mood | Self-Rated Health | Chronic Disease | BMI | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | Coefficient | 95% CI | |
| DE (ref: bad) | 0.74 | 0.65–0.84 *** | 1.32 | 1.14–1.53 *** | 0.90 | 0.74–1.09 | 0.08 | −0.14–0.31 |
| PFC (ref: bad) | 0.81 | 0.71–0.92 ** | 1.30 | 1.11–1.51 *** | 0.79 | 0.65–0.96 * | −0.04 | −0.28–0.19 |
| PS (ref: bad) | 0.75 | 0.64–0.89 *** | 1.15 | 0.96–1.38 | 0.82 | 0.65–1.04 | −0.17 | −0.47–0.12 |
| NR (ref: bad) | 0.46 | 0.31–0.66 *** | 2.14 | 1.42–3.21 *** | 0.53 | 0.33–0.87 * | −1.07 | −1.76–−0.38 ** |
| Age (ref: <60) | 1.06 | 0.95–1.18 | 0.56 | 0.50–0.64 *** | 2.00 | 1.72–2.33 *** | −1.17 | −1.37–−0.96 *** |
| Gender (ref: male) | 1.52 | 1.40–1.65 *** | 0.65 | 0.59–0.72 *** | 1.40 | 1.23–1.60 *** | −0.25 | −0.41–−0.10 *** |
| Marital status (ref: unmarried) | ||||||||
| Married | 0.97 | 0.82–1.14 | 0.31 | 0.23–0.41 *** | 4.26 | 2.64–6.87 *** | 1.22 | 0.90–1.53 *** |
| Divorce or bereavement | 2.18 | 1.67–2.85 *** | 0.28 | 0.19–0.41 *** | 4.52 | 2.58–7.91 *** | 1.27 | 0.77–1.78 *** |
| Education level (ref: Middle school and below) | ||||||||
| High school/vocational school | 0.86 | 0.74–0.99b * | 1.43 | 1.18–1.75 *** | 0.94 | 0.73–1.21 | −0.20 | −0.47–0.07 |
| College and above | 0.72 | 0.58–0.89 ** | 1.31 | 0.94–1.84 | 0.98 | 0.63–1.52 | −0.24 | −0.67–0.17 |
| Region (ref: Eastern) | ||||||||
| Central | 1.03 | 0.93–1.15 | 1.00 | 0.87–1.14 | 1.34 | 1.13–1.60 *** | −0.32 | −0.52–−0.11 ** |
| Western | 1.69 | 1.54–1.85 *** | 0.81 | 0.72–0.91 *** | 1.50 | 1.29–1.75*** | −1.39 | −1.57–−1.22 *** |
| Social position (ref: low) | ||||||||
| Fair | 0.64 | 0.58–0.70 *** | 1.32 | 1.18–1.48 *** | 1.00 | 0.85–1.17 | 0.21 | 0.03–0.39 * |
| High | 0.64 | 0.57–0.72 *** | 1.45 | 1.26–1.66 *** | 1.16 | 0.97–1.38 | 0.34 | 0.12–0.55 ** |
| Household income | 0.88 | 0.85–0.91 *** | 1.12 | 1.08–1.16 *** | 0.99 | 0.95–1.04 | 0.09 | 0.03–0.15 ** |
| Variables | Time Sleeping Weekday | Physical Exercise | Smoking Frequencies | Alcohol | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| DE (ref: bad) | 1.09 | 0.91–1.30 | 0.93 | 0.79–1.08 | 0.95 | 0.79–1.15 | 1.20 | 0.97–1.47 |
| PFC (ref: bad) | 1.05 | 0.87–1.27 | 1.20 | 1.02–1.42 * | 0.95 | 0.78–1.15 | 0.81 | 0.65–1.01 |
| PS (ref: bad) | 1.00 | 0.80–1.26 | 1.05 | 0.86–1.28 | 0.93 | 0.72–1.18 | 0.96 | 0.73–1.27 |
| NR (ref: bad) | 0.98 | 0.57–1.68 | 1.54 | 0.93–2.53 | 1.24 | 0.70–2.20 | 1.01 | 0.52–1.94 |
| Age (ref: <60) | 0.77 | 0.67–0.90 *** | 1.32 | 1.16–1.51 *** | 0.94 | 0.81–1.10 | 0.98 | 0.83–1.16 |
| Gender (ref: male) | 1.01 | 0.90–1.15 | 1.04 | 0.94–1.15 | 0.01 | 0.01–0.02 *** | 23.26 | 17.87–30.26 *** |
| Marital status (ref: unmarried) | ||||||||
| Married | 0.72 | 0.54–0.95 * | 0.81 | 0.66–1.00 | 0.81 | 0.64–1.02 | 0.72 | 0.54–0.95 * |
| Divorce or bereavement | 0.53 | 0.36–0.79 ** | 0.73 | 0.53–1.02 | 0.78 | 0.52–1.15 | 0.82 | 0.52–1.30 |
| Education level (ref: Middle school and below) | ||||||||
| High school/vocational school | 1.18 | 0.94–1.47 | 1.60 | 1.35–1.90 *** | 0.78 | 0.64–0.95 * | 1.28 | 1.02–1.61 * |
| College and above | 1.59 | 1.08–2.34 * | 2.95 | 2.27–3.85 *** | 0.31 | 0.22–0.43 *** | 3.36 | 2.06–5.46 *** |
| Region (ref: Eastern) | ||||||||
| Central | 1.03 | 0.89–1.20 | 1.13 | 0.99–1.29 | 1.07 | 0.91–1.27 | 1.62 | 1.35–1.93 *** |
| Western | 1.65 | 1.44–1.90 *** | 0.82 | 0.73–0.92 *** | 1.12 | 0.97–1.28 | 2.48 | 2.11–2.91 *** |
| Social class (ref: low) | ||||||||
| Fair | 1.01 | 0.87–1.17 | 1.30 | 1.15–1.47 *** | 1.10 | 0.95–1.28 | 0.93 | 0.79–1.09 |
| High | 0.77 | 0.65–0.91 ** | 1.82 | 1.58–2.09 *** | 1.19 | 1.00–1.42 * | 0.79 | 0.65–0.96 * |
| Household income | 0.97 | 0.93–1.02 | 1.05 | 1.01–1.09 * | 0.96 | 0.92–1.01 | 0.94 | 0.88–0.99 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, P.; Wang, J.; Wang, X.; Nie, W.; Zhen, F. Measuring the Association of Self-Perceived Physical and Social Neighborhood Environment with Health of Chinese Rural Residents. Int. J. Environ. Res. Public Health 2021, 18, 8380. https://doi.org/10.3390/ijerph18168380
Liu P, Wang J, Wang X, Nie W, Zhen F. Measuring the Association of Self-Perceived Physical and Social Neighborhood Environment with Health of Chinese Rural Residents. International Journal of Environmental Research and Public Health. 2021; 18(16):8380. https://doi.org/10.3390/ijerph18168380
Chicago/Turabian StyleLiu, Pengcheng, Jing Wang, Xiaojie Wang, Wenjie Nie, and Fangfang Zhen. 2021. "Measuring the Association of Self-Perceived Physical and Social Neighborhood Environment with Health of Chinese Rural Residents" International Journal of Environmental Research and Public Health 18, no. 16: 8380. https://doi.org/10.3390/ijerph18168380
APA StyleLiu, P., Wang, J., Wang, X., Nie, W., & Zhen, F. (2021). Measuring the Association of Self-Perceived Physical and Social Neighborhood Environment with Health of Chinese Rural Residents. International Journal of Environmental Research and Public Health, 18(16), 8380. https://doi.org/10.3390/ijerph18168380





