Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain
Abstract
:1. Introduction
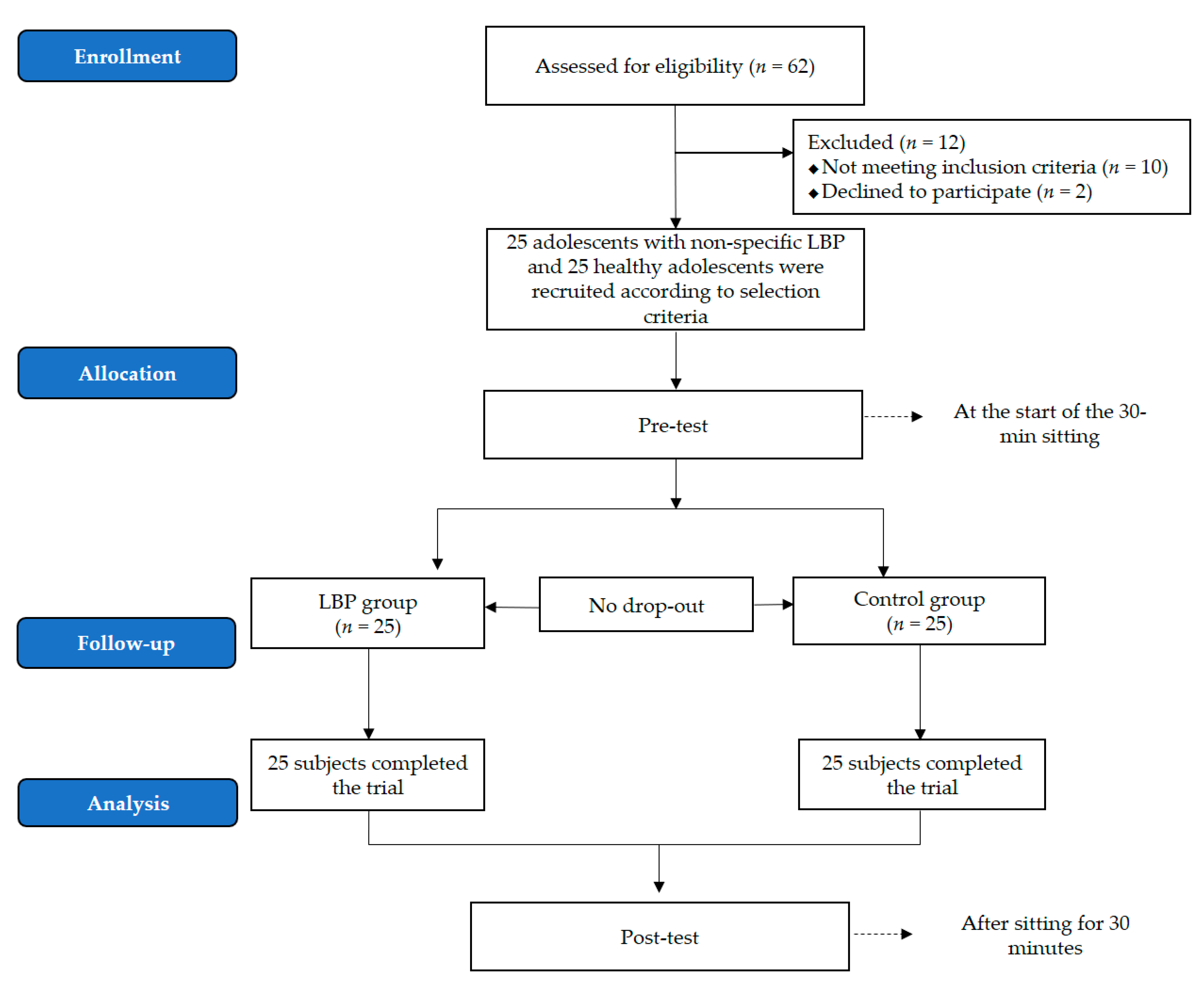
2. Subjects and Methods
2.1. Participants
2.2. Protocol
2.3. Outcome Measurements
2.4. Data Analysis
3. Results
3.1. General Characteristics of the Subjects
3.2. Comparison of Thoracolumbar Kyphosis
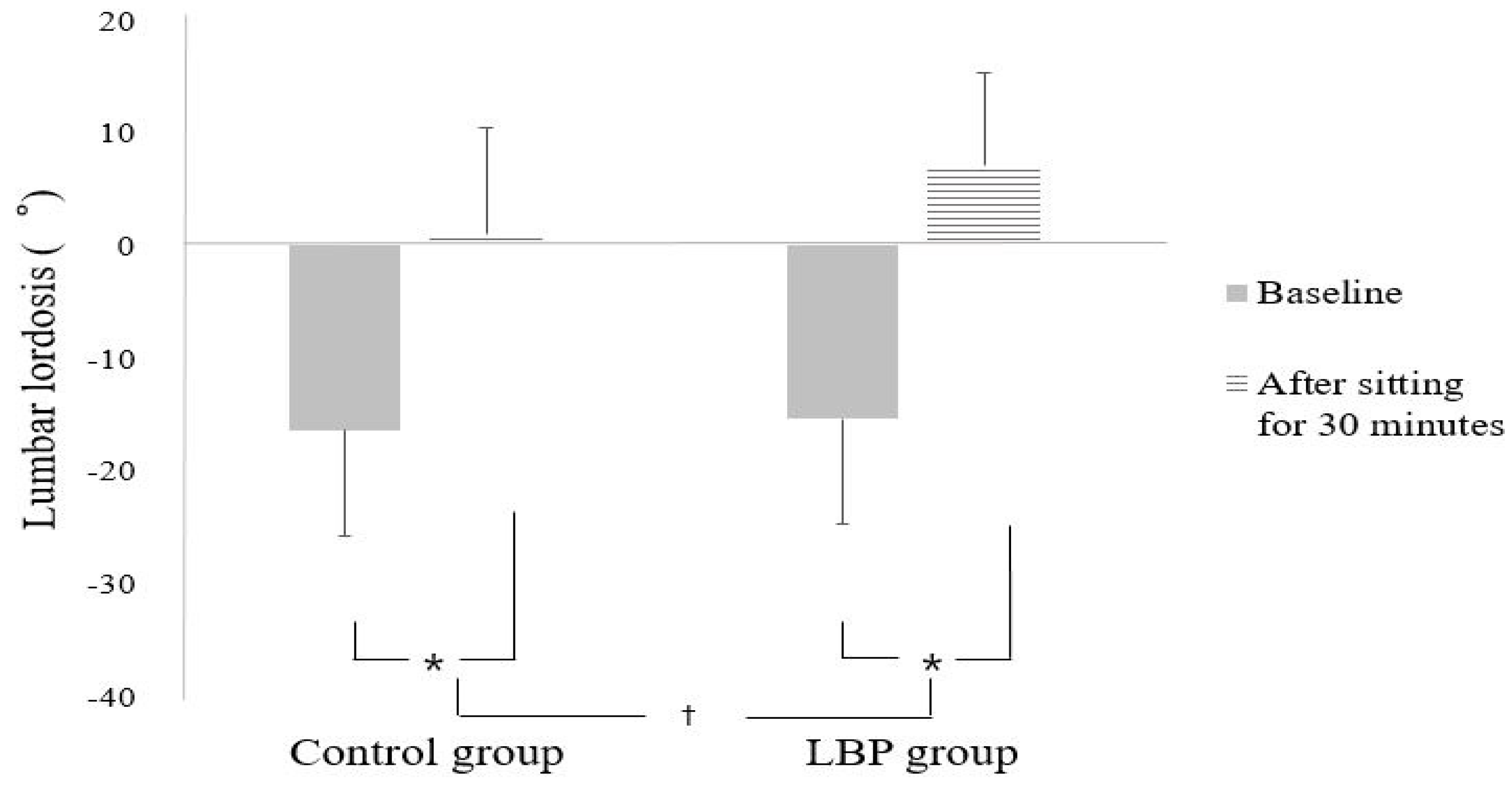
3.3. Comparison of Lumbar Lordosis
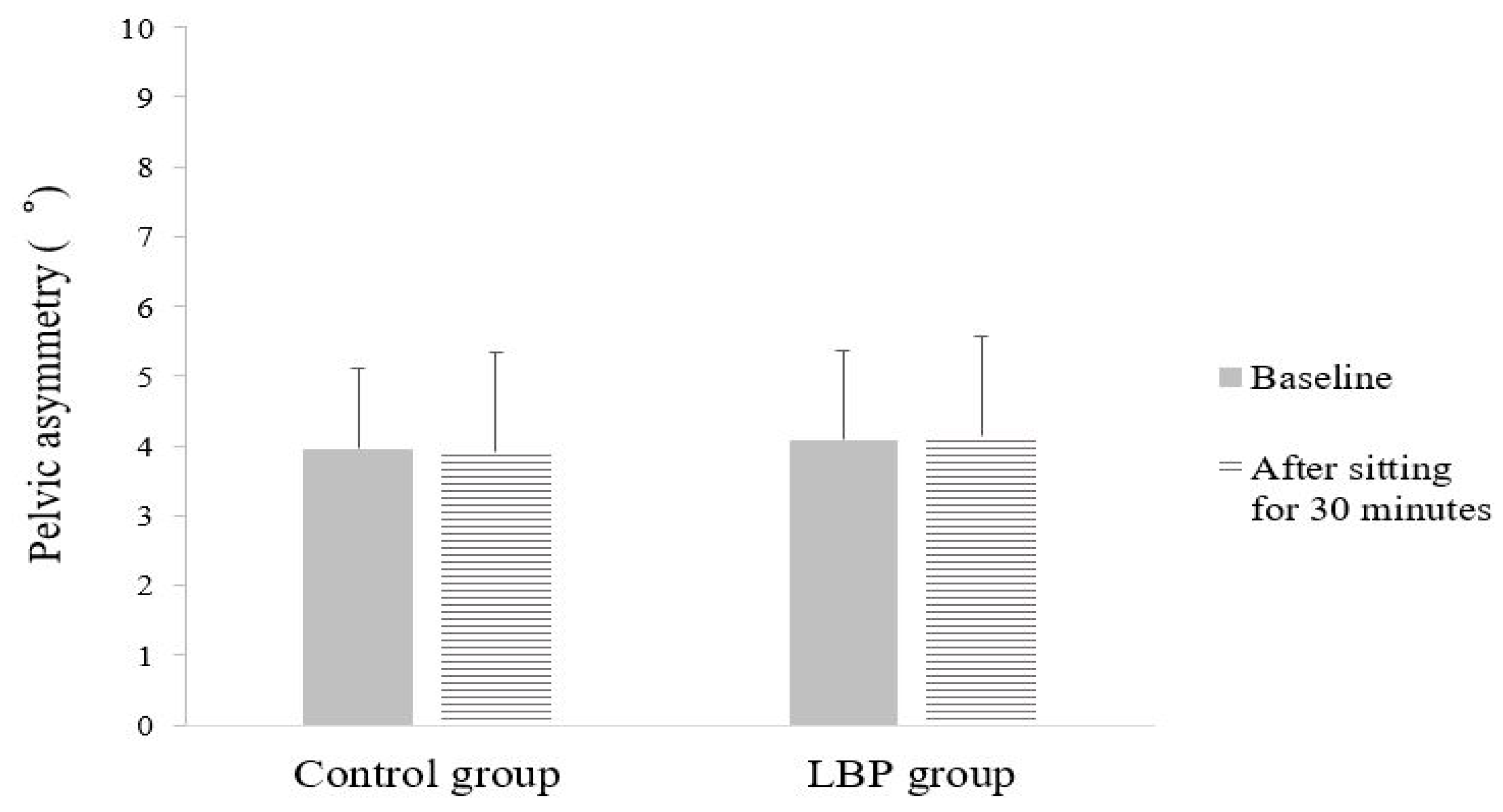
3.4. Comparison of Pelvic Asymmetry
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andrew, O. The History and Evolution of the Smartphone: 1992–2018. Available online: https://www.textrequest.com/blog/history-evolution-smartphone/ (accessed on 28 August 2018).
- Jonsson, P.; Johnson, P.W.; Hagberg, M.; Forsman, M. Thumb Joint Movement and Muscular Activity during Mobile Phone Texting-A Methodological Study. J. Electromyogr. Kinesiol. 2011, 21, 363–370. [Google Scholar] [CrossRef]
- Anderson, M.; Jiang, J. Teens, Social Media & Technology 2018; Pew Research Center: Washington, DC, USA, 2018; Available online: http://publicservicesalliance.org/wpcontent/uploads/2018/06/Teens-Social-Media-Technology-2018-PEW.pdf (accessed on 31 May 2018).
- Namwongsa, S.; Puntumetakul, R.; Neubert, M.S.; Boucaut, R. Effect of Neck Flexion Angles on Neck Muscle Activity among Smartphone Users with and without Neck Pain. Ergonomics 2019, 62, 1524–1533. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choi, Y.H.; Kim, J.G. Effects of the Cervical Flexion Angle during Smartphone Use on Muscle Fatigue and Pain in the Cervical Erector Spinae and Upper Trapezius in Normal Adults in Their 20s. J. Phys. Ther. Sci. 2017, 29, 921–923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betsch, M.; Kalbhen, K.; Michalik, R.; Schenker, H.; Gatz, M.; Quack, V.; Siebers, H.; Wild, M.; Migliorini, F. The Influence of Smartphone Use on Spinal Posture-A Laboratory Study. Gait Posture 2021, 85, 298–303. [Google Scholar] [CrossRef]
- Eitivipart, A.C.; Viriyarojanakul, S.; Redhad, L. Musculoskeletal Disorder and Pain Associated with Smartphone Use: A Systematic Review of Biomechanical Evidence. Hong Kong Physiother. J. 2018, 38, 77–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Win, A.M.; Yen, L.W.; Tan, K.H.; Lim, R.B.T.; Chia, K.S.; Mueller-Riemenschneider, F. Patterns of Physical Activity and Sedentary Behavior in a Representative Sample of a Multi-Ethnic South-East Asian Population: A Cross-Sectional Study. BMC Public Health 2015, 15, 318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parrish, A.M.; Trost, S.G.; Howard, S.J.; Batterham, M.; Cliff, D.; Salmon, J.; Okely, A. Evaluation of an Intervention to Reduce Adolescent Sitting Time during the School Day: The ‘Stadn Up for Health’ Randomized Controlled Trial. J. Sci. Med. Sport 2018, 21, 1244–1249. [Google Scholar] [CrossRef]
- Endo, K.; Suzuki, H.; Nishimura, H.; Tanaka, H.; Shishido, T.; Yamamoto, K. Sagittal Lumbar and Pelvic Alignment in the Standing and Sitting Positions. J. Orthop. Sci. 2012, 17, 682–686. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, D.E.; Soave, D.; Ross, K.; Callaghan, J.P. Lumbar Spine and Pelvic Posture between Standing and Sitting: A Radiologic Investigation Including Reliability and Repeatability of the Lumbar Lordosis Measure. J. Manip. Physiol. Ther. 2010, 33, 48–55. [Google Scholar] [CrossRef]
- Kerr, M.S.; Frank, J.W.; Shannon, H.S.; Norman, R.W.; Wells, R.P.; Neumann, W.P.; Bombardier, C.; Ontario Universities Back Pain Study Group. Biomechanical and Psychosocial Risk Factors for Low Back Pain at Work. Am. J. Public Health 2001, 91, 1069–1075. [Google Scholar]
- Neumann, D.A. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation; Mosby: St. Louis, MO, USA, 2002. [Google Scholar]
- Pynt, J.; Higgs, J.; Mackey, M. Historical Perspective Milestones in the Evolution of Lumbar Spinal Postural Health in Seating. Spine 2002, 27, 2180–2189. [Google Scholar] [CrossRef]
- Sondergaard, K.H.; Olesen, C.G.; Sondergaard, E.K.; de Zee, M.; Madeleine, P. The Variability and Complexity of Sitting Postural Control are Associated with Discomfort. J. Biomech. 2010, 43, 1997–2001. [Google Scholar] [CrossRef]
- Massaccesi, M.; Pagnotta, A.; Soccetti, A.; Masali, M.; Masiero, C.; Greco, F. Investigation of Work-Related Disorders in Truck Drivers using RULA Method. Appl. Ergon. 2003, 34, 303–307. [Google Scholar] [CrossRef]
- Dunn, K.M.; Hestbaek, L.; Cassidy, J.D. Low Back Pain across the Life Course. Best Pract. Res. Clin. Rheumatol. 2013, 27, 591–600. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.B.; Straker, L.M.; Smith, A.; Perry, M.; Kendall, G. Carer Experience of Back Pain is Associated with Adolescent Back Pain Experience even when Controlling for Other Carer and Family Factors. Clin. J. Pain 2008, 24, 226–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of Different Upright Sitting Postures on Spinal-Pelvic Curvature and Trunk Muscle Activation in a Pain-Free Population. Spine 2006, 31, E707–E712. [Google Scholar] [CrossRef]
- Wilke, H.J.; Neef, P.; Caimi, M.; Hoogland, T.; Claes, L.E. New In Vivo Measurements of Pressures in the Intervertebral Disc in Daily Life. Spine 1999, 24, 755–762. [Google Scholar] [CrossRef]
- Hey, H.W.D.; Wong, C.G.; Lau, E.T.; Tan, K.A.; Lau, L.L.; Liu, K.G.; Wong, H.K. Differences in Erect Sitting and Natural Sitting Spinal Alignment-Insights into a New Paradigm and Implications in Deformity Correction. Spine J. 2017, 17, 183–189. [Google Scholar] [CrossRef]
- Nimbarte, A.D.; Zreiqat, M.; Ning, X. Impact of Shoulder Position and Fatigue on the Flexion-Relaxation Response in Cervical Spine. Clin. Biomech. 2014, 29, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.M.; Gregory, D.E. The Use of Intermittent Trunk Flexion to Alleviate Low Back Pain during Prolonged Standing. J. Electromyogr. Kinesiol. 2016, 27, 46–51. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.B.; Mitchell, T.; Bulich, P.; Waller, R.; Holte, J. The Relationship between Posture and Back Muscle Endurance in Industrial Workers with Flexion-Related Low Back Pain. Man. Ther. 2006, 11, 264–271. [Google Scholar] [CrossRef]
- Womersley, L.; May, S. Sitting Posture of Subjects with Postural Backache. J. Manip. Physiol. Ther. 2006, 29, 213–218. [Google Scholar] [CrossRef]
- Viner, R.M.; Ozer, E.M.; Denny, S.; Marmot, M.; Resnick, M.; Fatusi, A.; Currie, C. Adolescence and the Social Determinants of Heal. Lancet 2012, 379, 1641–1652. [Google Scholar] [CrossRef]
- Jia, B.; Nussbaum, M.A. Influences of Continuous Sitting and Psychosocial Stress on Low Back Kinematics, Kinetics, Discomfort, and Localized Muscle Fatigue during Unsupported Sitting Activities. Ergonomics 2018, 61, 1671–1684. [Google Scholar] [CrossRef]
- Balagué, F.; Mannion, A.F.; Pellisé, F.; Cedraschi, C. Non-Specific Low Back Pain. Lancet 2012, 379, 482–491. [Google Scholar] [CrossRef] [Green Version]
- Fann, A.V. The Prevalence of Postural Asymmetry in People with and without Chronic Low Back Pain. Arch. Phys. Med. Rehabil. 2002, 83, 1736–1738. [Google Scholar] [CrossRef] [PubMed]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Different Ways to Balance the Spine in Sitting: Muscle Activity in Specific Postures Differs between Individuals with and without a History of Back Pain in Sitting. Clin. Biomech. 2018, 52, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Egan, D.A.; Cole, J.; Twomey, L. An Alternative Method for the Measurement of Pelvic Skeletal Asymmetry and the Association between Asymmetry and Back Pain. In Three Dimensional Analysis of Spinal Deformities; D’Amico, M., Merolli, A., Santambrogio, G., Eds.; IOS Press: Washington, DC, USA, 1995; pp. 171–177. [Google Scholar]
- Michaud, S.B.; Gard, S.A.; Childress, D.S. A Preliminary Investigation of Pelvic Obliquity Patterns during Gait in Persons with Transtibial and Transfemoral Amputation. J. Rehabil. Res. Dev. 2000, 37, 1–10. [Google Scholar] [PubMed]
- Shin, K.; Kim, D.; Jung, Y. Development of Korean Smart Phone Addiction Proneness Scale for Youth and Adults; Korean National Information Society Agency: Seoul, Korea, 2011. [Google Scholar]
- Xie, Y.; Szeto, G.; Dai, J. Prevalence and Risk Factors Associated with Musculoskeletal Complaints among Users of Mobile Handheld Devices: A Systematic Review. Appl. Ergon. 2017, 59, 132–142. [Google Scholar] [CrossRef]
- Johnseon, O.E.; Mbada, C.E.; Akosile, C.O.; Agbeja, O.A. Isometric Endurance of the Back Extensors in School-Aged Adolescents with and without Low Back Pain. J. Back Musculoskelet. Rehabil. 2009, 22, 205–211. [Google Scholar] [CrossRef]
- Waongenngarm, P.; Rajaratnam, B.S.; Janwantanakul, P. Internal Oblique and Transversus Abdominis Muscle Fatigue Induced by Slumped Sitting Posture after 1 Hour of Sitting in Office Workers. Saf. Health Work 2016, 7, 49–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, Y.; Kim, J.W.; Heo, J.H.; Jeon, H.M.; Choi, E.B.; Eom, G.M. The Effect of Sitting Posture on the Loads at Cervico-Thoracic and Lumbosacral Joints. Technol. Health Care 2018, 26, 409–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, E.S.; Ko, C.W.; Suh, S.W.; Kumar, S.; Kang, I.K.; Yang, J.H. The Effect of Age on Sagittal Plane Profile of the Lumbar Spine According to Standing, Supine, and Various Sitting Positions. J. Orthop. Surg. 2014, 9, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Dankaerts, W.; O’Sullivan, P.; Burnett, A.; Straker, L. Differences in Sitting Postures are Associated with Nonspecific Chronic Low Back Pain Disorders when Patients are Subclassified. Spine 2006, 31, 698–704. [Google Scholar] [CrossRef] [Green Version]
- O’Sullivan, P.B.; Burnett, A.; Floyd, A.N.; Gadsdon, K.; Logiudice, J.; Miller, D.; Quirke, H. Lumbar Repositioning Deficit in a Specific Low Back Pain Population. Spine 2003, 28, 1074–1079. [Google Scholar] [CrossRef]
- Dankaerts, W.; O’Sullivan, P.; Burnett, A.; Straker, L. Altered Patterns of Superficial Trunk Muscle Activation During Sitting in NonspecificChronic Low Back Pain Patients. Spine 2006, 31, 2017–2023. [Google Scholar] [CrossRef] [Green Version]
- Shirazi-Adl, A.; Drouin, G. Load-Bearing Role of Facets in a Lumbar Segment under Sagittal Plane Loadings. J. Biomech. 1987, 20, 601–613. [Google Scholar] [CrossRef]
- Al-Eisa, E.; Egan, D.A.; Wassersug, R. Fluctuating Asymmetry and Low Back Pain. Evol. Hum. Behav. 2004, 25, 31–37. [Google Scholar] [CrossRef]
- Knutson, G.A. Incidence of Foot Rotation, Pelvic Crest Unleveling, and Supine Leg Length Alignment Asymmetry and Their Relationship to Self-Reported Back Pain. J. Manip. Physiol. Ther. 2002, 25, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Eisa, E.; Egan, D.; Deluzio, K.; Wassersug, R. Effects of Pelvic Asymmetry and Low Back Pain on Trunk Kinematics during Sitting: A Comparison with Standing. Spine 2006, 31, 135–143. [Google Scholar] [CrossRef]
- Snijders, C.J.; Slaqter, A.H.; van Strik, R.; Vleeming, A.; Stoeckart, R.; Stam, H.J. Why Leg Crossing? The Influence of Common Postures on Abdominal Muscle Activity. Spine 1995, 20, 1989–1993. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.S.; An, D.H. Differences in Lumbar and Pelvic Angles and Gluteal Pressure in Different Sitting Postures. J. Phys. Ther. Sci. 2015, 27, 1333–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubousset, J. Pelvic Obliquity: A Review. Orthopedics 1991, 14, 479–481. [Google Scholar] [CrossRef] [PubMed]

| Variables | LBP Group (n = 25) | Control Group (n = 25) | p |
|---|---|---|---|
| Sex (male/female) | 15/10 | 17/8 | 0.771 b |
| Age (years) a | 17.96 ± 0.73 | 18.00 ± 0.65 | 0.839 c |
| Height (cm) a | 171.68 ± 5.93 | 172.52 ± 8.43 | 0.685 c |
| Weight (kg) a | 67.36 ± 14.12 | 69.04 ± 11.02 | 0.641 c |
| VAS (score) a,d | 4.12 ± 0.83 | - | |
| Postures that make symptoms worse (lumbar flexion/extension) | 22/3 | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
In, T.-s.; Jung, J.-h.; Jung, K.-s.; Cho, H.-y. Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain. Int. J. Environ. Res. Public Health 2021, 18, 8369. https://doi.org/10.3390/ijerph18168369
In T-s, Jung J-h, Jung K-s, Cho H-y. Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain. International Journal of Environmental Research and Public Health. 2021; 18(16):8369. https://doi.org/10.3390/ijerph18168369
Chicago/Turabian StyleIn, Tae-sung, Jin-hwa Jung, Kyoung-sim Jung, and Hwi-young Cho. 2021. "Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain" International Journal of Environmental Research and Public Health 18, no. 16: 8369. https://doi.org/10.3390/ijerph18168369
APA StyleIn, T.-s., Jung, J.-h., Jung, K.-s., & Cho, H.-y. (2021). Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain. International Journal of Environmental Research and Public Health, 18(16), 8369. https://doi.org/10.3390/ijerph18168369








