Using Autoregressive Integrated Moving Average (ARIMA) Modelling to Forecast Symptom Complexity in an Ambulatory Oncology Clinic: Harnessing Predictive Analytics and Patient-Reported Outcomes
Abstract
:1. Introduction
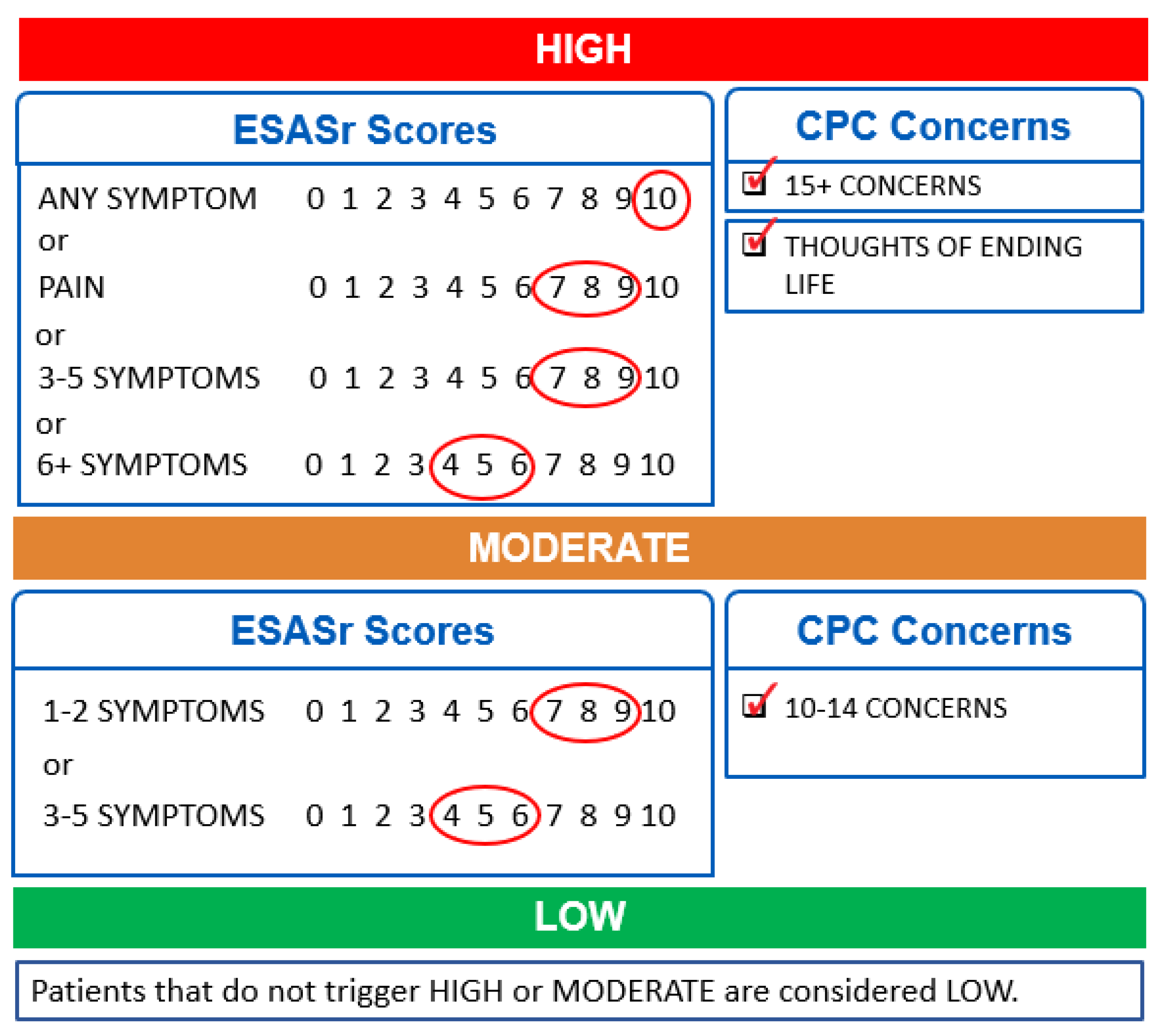
1.1. Symptom Complexity Algorithm
1.2. Scheduling Clinic Time and Allocating Staff
1.3. Purpose of the Study
2. Materials and Methods
2.1. Study Setting and Design
2.2. Ethics Approval
2.3. Data Analysis
2.4. Data Structure and Model Fit
2.5. Forecasting and Forecast Accuracy
3. Results
3.1. Sample Characteristics
3.2. Forecasting and Forecast Accuracy
4. Discussion
4.1. Forecasting Symptom Complexity to Improve Clinical Processes
4.2. Forecasting Symptom Complexity to Influence Innovative System Level Models of Care
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bates, D.W.; Saria, S.; Ohno-Machado, L.; Shah, A.; Escobar, G. Big data in health care: Using analytics to identify and manage high-risk and high-cost patients. Health Aff. 2014, 33, 1123–1131. [Google Scholar] [CrossRef] [Green Version]
- NEJM Catalyst. Healthcare Big Data and the Promise of Value-Based Care. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0290 (accessed on 23 February 2021).
- Edwards, J. What Is Predictive Analytics? Transforming Data into Future Insights. Available online: https://www.cio.com/article/3273114/what-is-predictive-analytics-transforming-data-into-future-insights.html (accessed on 11 May 2021).
- Simpson, K.D.; Melvin, S.; Fletcher, S. Expanding Patient Access to Cancer Care Services: Key Findings from a National Survey Show a Range of New Initiatives. Available online: https://www.accc-cancer.org/docs/documents/oncology-issues/articles/nd20/nd20-expanding-patient-access-to-cancer-care-services.pdf?sfvrsn=79f090c5_5 (accessed on 11 May 2021).
- Parikh, R.B.; Gdowski, A.; Patt, D.A.; Hertler, A.; Mermel, C.; Bekelman, J.E. Using Big Data and Predictive Analytics to Determine Patient Risk in Oncology. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, e53–e58. [Google Scholar] [CrossRef]
- Walter, F.M.; Rubin, G.; Bankhead, C.; Morris, H.C.; Hall, N.; Mills, K.; Dobson, C.; Rintoul, R.C.; Hamilton, W.; Emery, J. Symptoms and other factors associated with time to diagnosis and stage of lung cancer: A prospective cohort study. BJC 2015, 112, S6–S13. [Google Scholar] [CrossRef] [Green Version]
- Badana, A.N.S.; Marino, V.R.; Templeman, M.E.; McMillan, S.C.; Tofthagen, C.S.; Small, B.J.; Haley, W.E. Understanding the roles of patient symptoms and subjective appraisals in well-being among breast cancer patients. SCC 2019, 27, 4245–4252. [Google Scholar] [CrossRef]
- Snyder, C.; Brundage, M.; Rivera, Y.M.; Wu, A.W. A PRO-cision medicine methods toolkit to address the challenges of personalizing cancer care using patient-reported outcomes. Med. Care 2019, 57, S1–S7. [Google Scholar] [CrossRef] [PubMed]
- Matzka, M.; Kock-Hodi, S.; Jahn, P.; Mayer, H. Relationship among symptom clusters, quality of life, and treatment-specific optimism in patients with cancer. SCC 2018, 26, 2685–2693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omran, S.; Mcmillan, S. Symptom severity, anxiety, depression, self-efficacy and quality of life in patients with cancer. APJCP 2018, 19, 365–374. [Google Scholar] [PubMed]
- Montgomery, N.; Howell, D.; Ismail, Z.; Bartlett, S.J.; Brundage, M.; Bryant-Lukosius, D.; Krzyanowska, M.; Moody, L.; Snyder, C.; Barbera, L. Selecting, implementing and evaluating patient-reported outcome measures for routine clinical use in cancer: The Cancer Care Ontario approach. J. Patient Rep. Outcomes 2020, 4, 101:1–101:9. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Butow, P.; Dhillon, H.; Sandaresan, P. A review of the barriers to using patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) in routine cancer care. J. Med. Radiat. Sci. 2020, 68, 186–195. [Google Scholar] [CrossRef]
- Government of Alberta. Population Statistics. Available online: https://www.alberta.ca/population-statistics.aspx (accessed on 11 May 2021).
- Cancer Care Alberta. The 2021 Report on Cancer Statistics in Alberta. Available online: https://public.tableau.com/profile/cancercontrol.ab#!/vizhome/The2021ReportonCancerStatisticsinAlberta/Highlights (accessed on 11 May 2021).
- Cuthbert, C.A.; Watson, L.; Boyne, D.J.; Hemmelgarn, B.R.; Cheung, W.Y. Patient-reported outcomes in Alberta: Rational, scope, and design of a database initiative. Curr. Oncol. 2019, 26, e503–e509. [Google Scholar] [CrossRef] [Green Version]
- Canadian Partnership against Cancer. 2012 Cancer System Performance Report. Available online: https://www.systemperformance.ca/report/performance-report-2/ (accessed on 23 February 2021).
- Manojlovich, M.; Sidani, S. Nurse dose: What’s in a concept? RINAH 2008, 31, 310–319. [Google Scholar] [CrossRef]
- Manojlovich, M.; Sidani, S.; Covell, C.L.; Antonakos, C.L. Nurse dose: Linking staffing variables to adverse patient outcomes. Nurs. Res. 2011, 60, 214–220. [Google Scholar] [CrossRef]
- Rashwan, W. An Integrated Framework for Staffing and Shift Scheduling in Hospitals. Available online: https://arrow.tudublin.ie/busdoc/25 (accessed on 23 February 2021).
- Brundage, M.D.; Wu, A.W.; Rivera, Y.M.; Snyder, C. Promoting effective use of patient-reported outcomes in clinical practice: Themes from a “Methods Tool kit” paper series. JCE 2020, 122, 153–159. [Google Scholar] [CrossRef]
- Watson, L.; Qi, S.; DeIure, A.; Photitai, E.; Chmielewski, L.; Smith, L. Validating a patient-reported outcomes-derived algorithm for classifying symptom complexity levels among patients with cancer. JNCCN 2020, 18, 1518–1525. [Google Scholar] [CrossRef]
- Canadian Agency for Drugs and Technologies in Health (CADTH). Health Interventions in Ambulatory Cancer Care Centres. Available online: https://www.cadth.ca/node/89096 (accessed on 6 April 2021).
- Araujo, S.N.M.; Araujo Luz, M.H.B.; da Silva, G.R.F.; Andrade, E.M.L.R.; Nunes, L.C.C.; Moura, R.O. Cancer patients with oral mucositis: Challenges for nursing care. RLAE 2015, 23, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Alberta Innovates. A Project Ethics Community Consensus Initiative (ARECCI). Available online: https://albertainnovates.ca/programs/arecci (accessed on 20 January 2021).
- Pidduck, W.; Wan, B.A.; Zhang, L.; Chow, S.; Yee, C.; Chan, S.; Drost, L.; Sousa, P.; Lewis, D.; Lam, H.; et al. Seasonal fluctuations in psychological distress amongst women diagnosed with early breast cancer receiving radiotherapy. Pyscho-Oncol. 2019, 28, 2091–2097. [Google Scholar] [CrossRef] [PubMed]
- Basnet, S.; Merikanto, I.; Lahti, T.; Männistö, S.; Laatikainen, T.; Vartiainen, E.; Partonen, T. Seasonal variations in mood and behavior associate with common chronic diseases and symptoms in a population-based study. Psychiatry Res. 2016, 238, 181–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Earnest, A.; Evans, S.M.; Sampurno, F.; Millar, J. Forecasting annual incidence and mortality rate for prostate cancer in Australia until 2022 using autoregressive integrated moving average (ARIMA) models. BMJ Open 2019, 9, e031331:1–e031331:7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, L. Time series analysis and prediction on cancer incidence rates. JMD 2017, 2, 7030:1–7030:10. [Google Scholar] [CrossRef]
- Zheng, Y.-L.; Zhang, L.-P.; Zhang, X.-L.; Wang, K.; Zheng, Y.-J. Forecast model analysis for the morbidity of tuberculosis in Xinjiang, China. PLoS ONE 2015, 10, e0116832:1–e0116832:13. [Google Scholar] [CrossRef]
- Liu, Q.; Liu, X.; Jiang, B.; Yang, W. Forecasting incidence of hemorrhagic fever with renal syndrome in China using ARMIA model. BMC Infect. Dis. 2011, 11, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Heng, B.H.; Seow, Y.T.; Seow, E. Forecasting daily attendances at an emergency department to aid resource planning. BMC Emerg. Med. 2009, 9, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, B.; Turkcan, A.; Ceyhan, M.E.; Stuart, K. Improvement of chemotherapy patient flow and scheduling in an outpatient oncology clinic. IJPR 2015, 53, 7177–7190. [Google Scholar] [CrossRef]
- Karstens-Smith, B. A Timeline of COVID-19 in Alberta. Global News. Available online: https://globalnews.ca/news/7538547/covid-19-alberta-health-timeline/ (accessed on 3 August 2021).
- Watson, L.; Qi, S.; DeIure, A.; Link, C.; Photitai, E.; Chmielewski, L.; Hildebrand, A.; Ruether, D.; Rawson, K. Virtual cancer care during the COVID-19 pandemic in Alberta: Evidence from a mixed methods evaluation and key learnings. JCO OP 2021. [Google Scholar] [CrossRef]
- Jones, J.M.; Saeed, H.; Katz, M.S.; Lustberg, M.B.; Forster, V.J.; Nekhlyudov, L. Readdressing the needs of cancer survivors during COVID-19: A path forward. JNCI 2021. [Google Scholar] [CrossRef]
- Duffield, C.; Roche, M.; Thomas, E. Methods of measuring nursing workload in Australia. Collegian 2006, 13, 16–22. [Google Scholar] [CrossRef]
- Biddy, R.; Griffin, C.; Johnson, N.; Larocque, G.; Messersmith, H.; Moody, L.; Shamji, H.; Stevens, C.; Zwaal, C.; Singh, S. Person-Centred Care Guidelines Expert Panel. Cancer Care Ontario: Person-Centred Care Guideline. Available online: https://www.cancercareontario.ca/en/content/person-centred-care-guideline (accessed on 23 February 2021).
- Entwistle, V.A.; Watt, I.S. Treating patients as persons: A capabilities approach to support delivery of person-centered care. AJOB 2013, 13, 29–39. [Google Scholar] [CrossRef] [Green Version]
- Fitch, M.I.; Coronado, A.C.; Schippke, J.C.; Chadder, J.; Green, E. Exploring the perspectives of patients about their care experience: Identifying what patients perceive are important qualities in cancer care. SCC 2020, 28, 2299–2309. [Google Scholar] [CrossRef]
- Curigliano, G.; Cardoso, M.J.; Poortmans, P.; Gentilini, O.; Pravettoni, G.; Mazzocco, K.; Housami, N.; Pagani, O.; Senkus, E.; Cardoso, F. Recommendations for triage, prioritization and treatment of breast cancer patients during the COIVD-19 pandemic. Breast 2020, 52, 8–16. [Google Scholar] [CrossRef]
- Friedman, C.; Rubin, J.; Brown, J.; Buntin, M.; Corn, M.; Etheredge, L.; Gunter, C.; Musen, M.; Platt, R.; Stead, W.; et al. Toward a science of learning systems: A research agenda for the high-functioning Learning Health System. JAMIA 2015, 22, 43–50. [Google Scholar] [CrossRef] [Green Version]


| Model | Normalized BIC | Ljung-Box Q (18) | Ljung-Box p | MAE | RMSE |
|---|---|---|---|---|---|
| ARIMA (0, 0, 1) | −4.72 | 19.66 | 0.292 | 0.040 | 0.056 |
| ARIMA (0, 1, 0) | −3.57 | 26.65 | 0.086 | 0.067 | 0.104 |
| ARIMA (1, 1, 0) | −3.82 | 12.66 | 0.759 | 0.057 | 0.089 |
| ARIMA (0, 1, 1) | −3.97 | 19.98 | 0.275 | 0.052 | 0.080 |
| ARIMA (1, 1, 1) | −3.92 | 17.58 | 0.349 | 0.050 | 0.076 |
| Clinic Visit Date | Age (M) | Sex (% Male) | TG * (% NET/END) | TG * (%GU) | % Low | % Moderate | % High |
|---|---|---|---|---|---|---|---|
| 07-Aug-2019 | 66.6 | 82.6 | 17.4 | 56.5 | 69.6 | 13.0 | 17.4 |
| 14-Aug-2019 | 69.6 | 88.9 | 22.2 | 44.4 | 55.6 | 33.3 | 11.1 |
| 21-Aug-2019 | 63.7 | 70.0 | 10.0 | 70.0 | 70.0 | 20.0 | 10.0 |
| 28-Aug-2019 | 61.9 | 100.0 | 0.0 | 77.8 | 55.6 | 22.2 | 22.2 |
| 04-Sep-2019 | 63.7 | 72.7 | 13.6 | 50.0 | 45.0 | 25.0 | 30.0 |
| 11-Sep-2019 | 69.0 | 71.4 | 19.0 | 52.4 | 66.7 | 23.8 | 9.5 |
| 18-Sep-2019 | 66.7 | 81.3 | 0.0 | 81.3 | 56.3 | 25.0 | 18.8 |
| 25-Sep-2019 | 67.9 | 92.8 | 14.3 | 35.7 | 57.1 | 28.6 | 14.3 |
| 02-Oct-2019 | 61.8 | 64.7 | 23.5 | 35.3 | 47.1 | 29.4 | 23.5 |
| 09-Oct-2019 | 67.4 | 77.8 | 0.0 | 83.3 | 55.6 | 27.8 | 16.7 |
| 16-Oct-2019 | 67.8 | 83.3 | 33.3 | 41.7 | 75.0 | 16.7 | 8.3 |
| 23-Oct-2019 | 67.7 | 69.2 | 0.0 | 38.5 | 76.9 | 15.4 | 7.7 |
| 30-Oct-2019 | 69.6 | 68.4 | 15.8 | 57.9 | 47.4 | 36.8 | 15.8 |
| 06-Nov-2019 | 66.8 | 84.2 | 5.3 | 73.7 | 84.2 | 5.3 | 10.5 |
| 13-Nov-2019 | 67.5 | 82.4 | 29.4 | 52.9 | 52.9 | 35.3 | 11.8 |
| 20-Nov-2019 | 71.7 | 75.0 | 6.3 | 62.5 | 68.8 | 12.5 | 18.8 |
| 27-Nov-2019 | 73.2 | 42.9 | 14.3 | 42.9 | 71.4 | 28.6 | 0.0 |
| 04-Dec-2019 | 64.2 | 86.4 | 13.6 | 59.1 | 68.2 | 9.1 | 22.7 |
| 11-Dec-2019 | 71.3 | 85.7 | 28.6 | 64.3 | 71.4 | 21.4 | 7.1 |
| 18-Dec-2019 | 66.8 | 70.0 | 5.0 | 60.0 | 70.0 | 20.0 | 10.0 |
| 08-Jan-2020 | 67.9 | 85.0 | 20.0 | 75.0 | 60.0 | 30.0 | 10.0 |
| 15-Jan-2020 | 64.9 | 75.0 | 6.3 | 50.0 | 62.5 | 25.0 | 12.5 |
| 22-Jan-2020 | 68.2 | 50.0 | 20.0 | 40.0 | 45.0 | 30.0 | 25.0 |
| 29-Jan-2020 | 67.5 | 75.0 | 5.0 | 55.0 | 70.0 | 20.0 | 10.0 |
| Clinic Visit Date | Forecasts | Actual Observations | Absolute Error |
|---|---|---|---|
| 05-Feb-2020 | 14.6% | 19.0% | 4.4% |
| 12-Feb-2020 | 20.9% | 25.0% | 4.1% |
| 19-Feb-2020 | 7.3% | 13.3% | 6.0% |
| 26-Feb-2020 | 24.3% | 12.5% | 11.8% |
| 04-Mar-2020 | 14.5% | 23.5% | 9.0% |
| 11-Mar-2020 | 14.2% | 9.1% | 5.1% |
| 18-Mar-2020 | 20.0% | 25.0% | 5.0% |
| 25-Mar-2020 | 26.7% | 28.6% | 1.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watson, L.; Qi, S.; DeIure, A.; Link, C.; Chmielewski, L.; Hildebrand, A.; Rawson, K.; Ruether, D. Using Autoregressive Integrated Moving Average (ARIMA) Modelling to Forecast Symptom Complexity in an Ambulatory Oncology Clinic: Harnessing Predictive Analytics and Patient-Reported Outcomes. Int. J. Environ. Res. Public Health 2021, 18, 8365. https://doi.org/10.3390/ijerph18168365
Watson L, Qi S, DeIure A, Link C, Chmielewski L, Hildebrand A, Rawson K, Ruether D. Using Autoregressive Integrated Moving Average (ARIMA) Modelling to Forecast Symptom Complexity in an Ambulatory Oncology Clinic: Harnessing Predictive Analytics and Patient-Reported Outcomes. International Journal of Environmental Research and Public Health. 2021; 18(16):8365. https://doi.org/10.3390/ijerph18168365
Chicago/Turabian StyleWatson, Linda, Siwei Qi, Andrea DeIure, Claire Link, Lindsi Chmielewski, April Hildebrand, Krista Rawson, and Dean Ruether. 2021. "Using Autoregressive Integrated Moving Average (ARIMA) Modelling to Forecast Symptom Complexity in an Ambulatory Oncology Clinic: Harnessing Predictive Analytics and Patient-Reported Outcomes" International Journal of Environmental Research and Public Health 18, no. 16: 8365. https://doi.org/10.3390/ijerph18168365
APA StyleWatson, L., Qi, S., DeIure, A., Link, C., Chmielewski, L., Hildebrand, A., Rawson, K., & Ruether, D. (2021). Using Autoregressive Integrated Moving Average (ARIMA) Modelling to Forecast Symptom Complexity in an Ambulatory Oncology Clinic: Harnessing Predictive Analytics and Patient-Reported Outcomes. International Journal of Environmental Research and Public Health, 18(16), 8365. https://doi.org/10.3390/ijerph18168365








