Study on the Formation Mechanism of Medical and Health Organization Staff’s Emergency Preparedness Behavioral Intention: From the Perspective of Psychological Capital
Abstract
1. Introduction
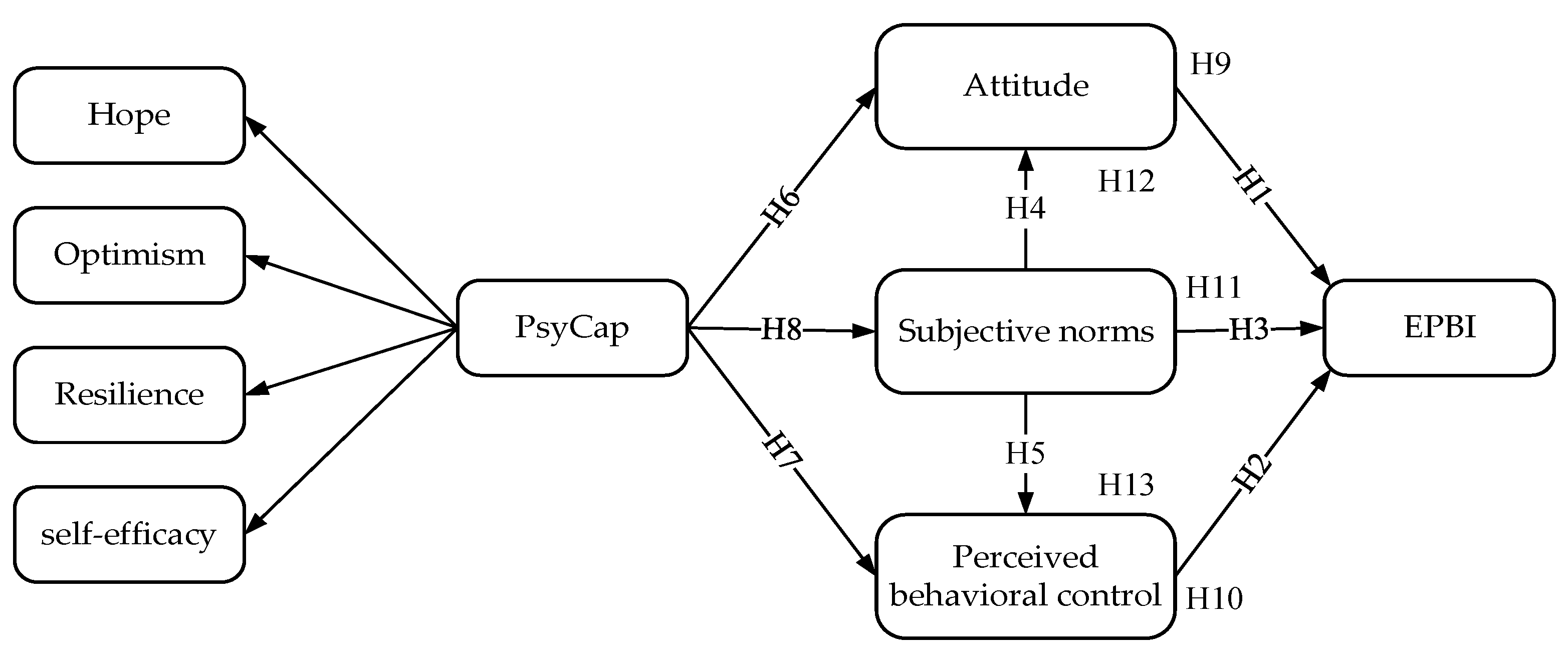
2. Research Hypotheses and Theoretical Model
2.1. TPB and EPBI
2.2. PsyCap and TPB
2.3. The Intermediary Role of Attitude, Perceived Behavioral Control, and Subjective Norms
3. Methods
3.1. Study Design
3.2. Measures
3.3. Study Participants
3.4. Data Analysis
4. Results
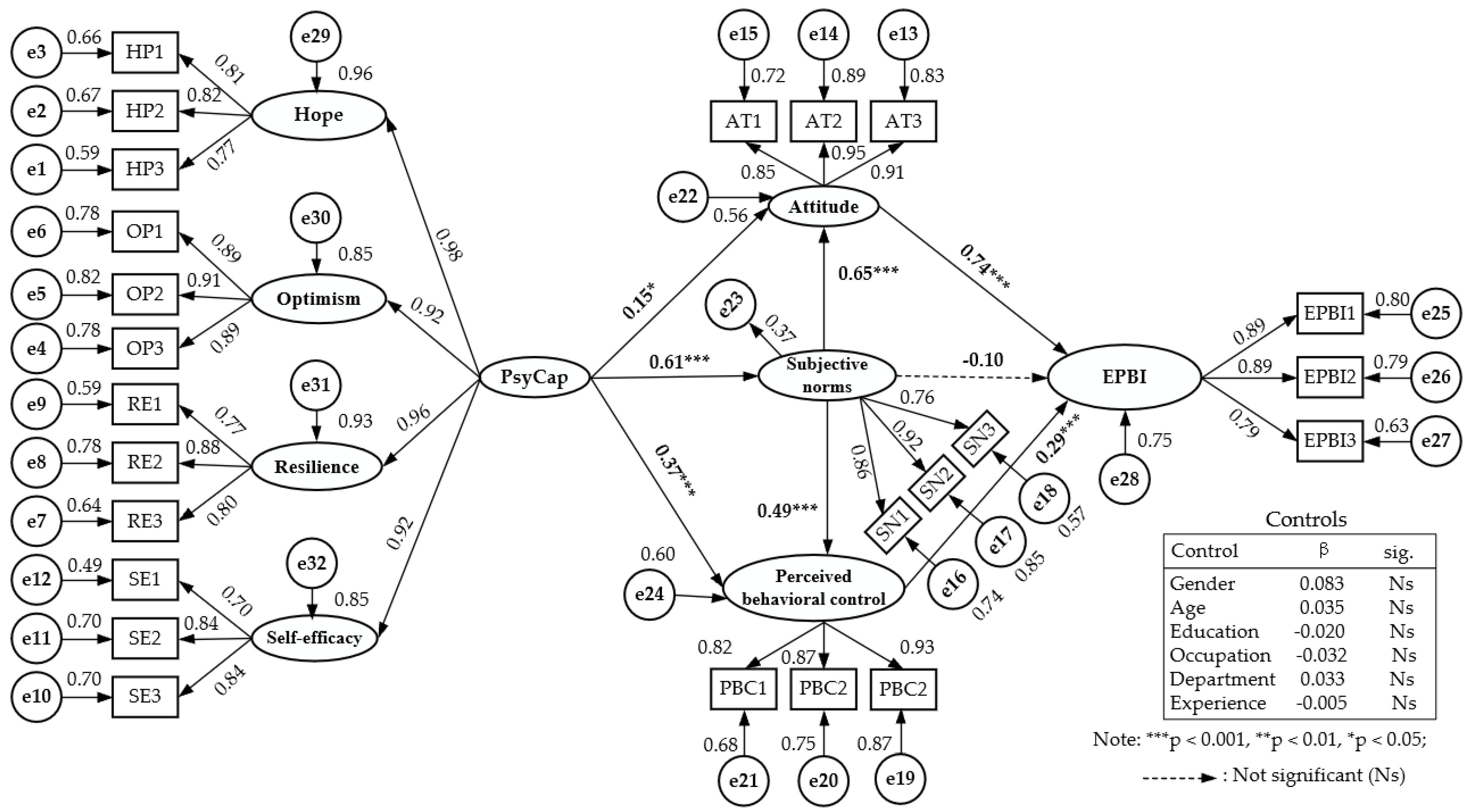
4.1. Reliability and Validity Testing
4.2. Model Fitting
4.3. Hypotheses Testing
5. Conclusions and Suggestions
5.1. Theoretical Contribution
5.2. Practical Significance
- (1)
- Cultivate crisis awareness and improve the psychological risk reserve of MHO staff.
- (2)
- Strengthen the training of emergency knowledge to make MHO staff fully aware of the significance and value of EP.
- (3)
- Conduct emergency practice drills to enhance the confidence of MHO staff in dealing with unexpected accidents.
- (4)
- Establish emergency logistics support work to ensure MHO workers’ health and life safety, etc.
- (1)
- Involve MHO staff in the process of preparing emergency preparedness and response plans.
- (2)
- Make realistic and optimistic expectations to counteract the pessimism of MHO staff about emergency preparedness.
- (3)
- Reinforce the transferable value of emergency preparation behavior in the career development of MHO staff.
- (4)
- Provide positive feedback to MHO staff who are actively involved in emergency preparedness, etc.
5.3. Limitations and Prospect
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Pu, C.Y.; Liu, Z.; Pan, X.J.; Addai, B. The impact of natural disasters on China’s macro economy. Environ. Sci. Pollut. Res. 2020, 27, 43987–43998. [Google Scholar] [CrossRef]
- Xiao, W.; Xu, J.F.; Lv, X.J. Establishing a georeferenced spatio-temporal database for Chinese coal mining accidents between 2000 and 2015. Geomat. Nat. Hazards Risk 2019, 10, 242–270. [Google Scholar] [CrossRef]
- Zha, D.J. Non-Traditional Security and China-US Relations. Asian Perspect. 2021, 45, 75–81. [Google Scholar]
- Si, R.S.; Lu, Q.; Aziz, N. Impact of COVID-19 on peoples’ willingness to consume wild animals: Empirical insights from China. One Health 2021, 12, 100240. [Google Scholar] [CrossRef]
- Wu, Q.; Han, J.W.; Lei, C.Q.; Ding, W.; Li, B.; Zhang, L. The challenges and countermeasures in emergency management after the establishment of the ministry of emergency management of China: A case study. Int. J. Disaster Risk Reduct. 2021, 55, 102075. [Google Scholar] [CrossRef]
- Cao, Y.L.; Shan, J.; Gong, Z.Z.; Kuang, J.Q.; Gao, Y. Status and Challenges of Public Health Emergency Management in China Related to COVID-19. Front. Public Health 2020, 8, 250. [Google Scholar] [CrossRef]
- Kong, F.; Sun, S. Understanding and Strengthening the Emergency Management and Comprehensive Disaster Reduction in China’s Rural Areas: Lessons from Coping with the COVID-19 Epidemic. Sustainability 2021, 13, 3642. [Google Scholar] [CrossRef]
- Luo, H.S.; Qian, H.W. Research on the basic theory and practice of emergency management in China in the new development stage. China Emerg. Manag. 2021, 4, 18–29. [Google Scholar]
- Day, A.; Staniszewska, S.; Bullock, I. Planning for Chaos: Developing the Concept of Emergency Preparedness through the Experience of the Paramedic. J. Emerg. Nurs. 2021, 47, 487–502. [Google Scholar] [CrossRef]
- Zhao, M.M.; Liu, B.H.; Wang, L.; Wu, Q.H.; Kang, Z.; Hao, Y.H.; Amporfro, D.; Gao, L.J. A Cross-Sectional Study on China’s Public Health Emergency Personnel’s Field Coping-Capacity: Need, Influencing Factors, and Improvement Options. Disaster Med. Public Health Prep. 2020, 14, 192–200. [Google Scholar] [CrossRef]
- Chen, C.L.; Tang, J.S.; Lai, M.K.; Hung, C.H. Factors influencing medical staff’s intentions to implement family-witnessed cardiopulmonary resuscitation: A cross-sectional, multihospital survey. Eur. J. Cardiovasc. Nursing. 2017, 16, 492–501. [Google Scholar] [CrossRef]
- Rottger, S.; Maier, J.; Krex-Brinkmann, L.; Kowalski, J.T.; Krick, A.; Felfe, J.; Stein, M. Social cognitive aspects of the participation in workplace health promotion as revealed by the theory of planned behavior. Prev. Med. 2017, 105, 104–108. [Google Scholar] [CrossRef]
- Rich, A.; Medisauskaite, A.; Potts, H.W.W.; Griffin, A. A theory-based study of doctors’ intentions to engage in professional behaviours. BMC Med. Educ. 2020, 20, 44. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Dholakia, U.M.; Mookerjee, A. Individual and Group Bases of Social Influence in Online Environments. Media Psychol. 2006, 8, 95–126. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behaviour: Reactions and reflections. Psychol. Health 2011, 26, 1113–1127. [Google Scholar] [CrossRef]
- Malik, N.; Dhar, R.L. Authentic leadership and its impact on extra role behaviour of nurses: The mediating role of psychological capital and the moderating role of autonomy. Pers. Rev. 2017, 46, 277–296. [Google Scholar] [CrossRef]
- Luthans, F.; Luthans, K.W.; Luthans, B.C. Positive psychological capital: Beyond human and social capital. Bus. Horiz. 2004, 47, 45–50. [Google Scholar] [CrossRef]
- Seligman, M.E.P.; Csikszentmihalyi, M. Positive psychology: An introduction. Am. Psychol. 2000, 55, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Burns, A.J.; Posey, C.; Roberts, T.L.; Lowry, P.B. Examining the relationship of organizational insiders’ psychological capital with information security threat and coping appraisals. Comput. Hum. Behav. 2017, 68, 190–209. [Google Scholar] [CrossRef]
- Stratman, J.L.; Youssef-Morgan, C.M. Can positivity promote safety? Psychological capital development combats cynicism and unsafe behavior. Saf. Sci. 2019, 116, 13–25. [Google Scholar] [CrossRef]
- Luthans, F.; Avey, J.B.; Avolio, B.J.; Norman, S.M.; Combs, G. Psychological Capital Development: Toward a Micro-intervention. J. Organ. Behav. 2006, 27, 387–393. [Google Scholar] [CrossRef]
- Wang, J.F.; Bu, L.R.; Li, Y.; Song, J.; Li, N. The mediating effect of academic engagement between psychological capital and academic burnout among nursing students during the COVID-19 pandemic: A cross-sectional study. Nurse Educ. Today 2021, 102, 104938. [Google Scholar] [CrossRef] [PubMed]
- Luthans, F.; Broad, J.D. Positive psychological capital to help combat the mental health fallout from the pandemic and VUCA environment. Organ. Dyn. 2020, 100817. [Google Scholar] [CrossRef]
- Dwyer, P.A.; Revell, S.M.H.; Sethares, K.A.; Ayotte, B.J. The influence of psychological capital, authentic leadership in preceptors, and structural empowerment on new graduate nurse burnout and turnover intent. Appl. Nurs. Res. 2019, 48, 37–44. [Google Scholar] [CrossRef]
- Ahayalimudin, N.; Osman, N.N.S. Disaster management: Emergency nursing and medical personnel’s knowledge, attitude and practices of the East Coast region hospitals of Malaysia. Australas. Emerg. Nurs. J. AENJ 2016, 19, 203–209. [Google Scholar] [CrossRef] [PubMed]
- O’Boyle, C.; Robertson, C.; Secor-Turner, M. Nurses’ beliefs about public health emergencies: Fear of abandonment. Am. J. Infect. Control. 2006, 34, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Via-Clavero, G.; Guardia-Olmos, J.; Falco-Pegueroles, A.; Gil-Castillejos, D.; Lobo-Civico, A.; De La Cueva-Ariza, L.; Romero-Garcia, M.; Delgado-Hito, P. Factors influencing critical care nurses’ intentions to use physical restraints adopting the theory of planned behaviour: A cross-sectional multicentre study. Aust. Crit. Care 2020, 33, 426–435. [Google Scholar] [CrossRef]
- Knowles, S.; Lam, L.T.; McInnes, E.; Elliott, D.; Hardy, J.; Middleton, S. Knowledge, attitudes, beliefs and behaviour intentions for three bowel management practices in intensive care: Effects of a targeted protocol implementation for nursing and medical staff. BMC Nurs. 2015, 14, 6. [Google Scholar] [CrossRef][Green Version]
- Corace, K.M.; Srigley, J.A.; Hargadon, D.P.; Yu, D.; MacDonald, T.K.; Fabrigar, L.R.; Garber, G.E. Using behavior change frameworks to improve healthcare worker influenza vaccination rates: A systematic review. Vaccine 2016, 34, 3235–3242. [Google Scholar] [CrossRef]
- Lai, M.K.; Aritejo, B.A.; Tang, J.S.; Chen, C.L.; Chuang, C.C. Predicting medical professionals’ intention to allow family presence during resuscitation: A cross sectional survey. Int. J. Nurs. Stud. 2017, 70, 11–16. [Google Scholar] [CrossRef]
- Ghaffari, M.; Rakhshanderou, S.; Safari-Moradabadi, A.; Barkati, H. Exploring determinants of hand hygiene among hospital nurses: A qualitative study. BMC Nurs. 2020, 19, 109. [Google Scholar] [CrossRef]
- Armitage, C.J.; Conner, M. Distinguishing Perceptions of Control from Self-Efficacy: Predicting Consumption of a Low-Fat Diet Using the Theory of Planned Behavior. J. Appl. Soc. Psychol. 2009, 39, 72–90. [Google Scholar] [CrossRef]
- Paek, H.J.; Hilyard, K.; Freimuth, V.; Barge, J.K.; Mindlin, M. Theory-Based Approaches to Understanding Public Emergency Preparedness: Implications for Effective Health and Risk Communication. J. Health Commun. 2010, 15, 428–444. [Google Scholar] [CrossRef]
- Al Khalaileh, M.A.; Bond, E.; Alasad, J.A. Jordanian nurses’ perceptions of their preparedness for disaster management. Int. Emerg. Nurs. 2012, 20, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Boldor, N.; Br-Dayan, Y.; Rosenbloom, T.; Shemer, J.; Bar-Dayan, Y. Optimism of health care workers during a disaster: A review of the literature. Emerg. Health Threat. J. 2012, 5, 7270. [Google Scholar] [CrossRef] [PubMed]
- Melnikov, S.; Itzhaki, M.; Kagan, I. Israeli Nurses’ Intention to Report for Work in an Emergency or Disaster. J. Nurs. Scholarsh. 2014, 46, 134–142. [Google Scholar] [CrossRef]
- Mache, S.; Vitzthum, K.; Wanke, E.; Groneberg, D.A.; Klapp, B.F.; Danzer, G. Exploring the impact of resilience, self-efficacy, optimism and organizational resources on work engagement. WORK-A J. Prev. Assess. Rehabil. 2014, 47, 491–500. [Google Scholar]
- McAllister, S.; Coxon, K.; Murrells, T.; Sandall, J. Healthcare professionals’ attitudes, knowledge and self-efficacy levels regarding the use of self-hypnosis in childbirth: A prospective questionnaire survey. Midwifery 2017, 47, 8–14. [Google Scholar] [CrossRef]
- Tang, N.; Han, L.; Yang, P.; Zhao, Y.; Zhang, H. Are mindfulness and self-efficacy related to presenteeism among primary medical staff: A cross-sectional study. Int. J. Nurs. Sci. 2019, 6, 182–186. [Google Scholar] [CrossRef]
- Nowakowska, I.; Rasinska, R.; Glowacka, M.D. The influence of factors of work environment and burnout syndrome on self-efficacy of medical staff. Ann. Agric. Environ. Med. 2016, 23, 304–309. [Google Scholar] [CrossRef]
- Wu, L.F.; Chang, L.F.; Hung, Y.C.; Lin, C.; Tzou, S.J.; Chou, L.J.; Pan, H.H. The Effect of Practice toward Do-Not-Resuscitate among Taiwanese Nursing Staff Using Path Modeling. Int. J. Environ. Res. Public Health 2020, 17, 6350. [Google Scholar] [CrossRef] [PubMed]
- Klaver, M.; van den Hoofdakker, B.J.; Wouters, H.; de Kuijper, G.; Hoekstra, P.J.; de Bildt, A. Exposure to challenging behaviours and burnout symptoms among care staff: The role of psychological resources. J. Intellect. Disabil. Res. 2021, 65, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Frey, R.; Robinson, J.; Wong, C.; Gott, M. Burnout, compassion fatigue and psychological capital: Findings from a survey of nurses delivering palliative care. Appl. Nurs. Res. 2018, 43, 1–9. [Google Scholar] [CrossRef]
- Ajzen, I. Perceived Behavioral Control, Self-Efficacy, Locus of Control, and the Theory of Planned Behavior. J. Appl. Soc. Psychol. 2002, 32, 665–683. [Google Scholar] [CrossRef]
- Probst, T.M.; Gailey, N.J.; Jiang, L.X.; Bohle, S.L. Psychological capital: Buffering the longitudinal curvilinear effects of job insecurity on performance. Saf. Sci. 2017, 100, 74–82. [Google Scholar] [CrossRef]
- Liu, Y.; Aungsuroch, Y.; Gunawan, J.; Zeng, D.J. Job Stress, Psychological Capital, Perceived Social Support, and Occupational Burnout Among Hospital Nurses. J. Nurs. Scholarsh. 2021, 53, 511–518. [Google Scholar] [CrossRef]
- Yildiz, H. The Interactive Effect of Positive Psychological Capital and Organizational Trust on Organizational Citizenship Behavior. SAGE Open 2019, 9, 1–15. [Google Scholar] [CrossRef]
- Luthans, F.; Avolio, B.J.; Avey, J.B.; Norman, S.M. Positive Psychological Capital: Measurement and Relationship with Performance and Satisfaction. Pers. Psychol. 2007, 60, 541–572. [Google Scholar] [CrossRef]
- Ajzen, I. Constructing a TPB Questionnaire: Conceptual and Methodological Considerations. Work. Pap. 2006. Available online: http://www.people.umass.edu/aizen/pdf/tpb.measurement.pdf (accessed on 27 June 2021).
- Miceli, R.; Sotgiu, I.; Settanni, M. Disaster preparedness and perception of flood risk: A study in an alpine valley in Italy. J. Environ. Psychol. 2008, 28, 164–173. [Google Scholar] [CrossRef]
- Murphy, S.T.; Cody, M.; Frank, L.B.; Glik, D.; Ang, A. Predictors of emergency preparedness and compliance. Disaster Med. Public Health Prep. 2009, 7, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.X.; Kim, J.S.; Xiong, L.H. Media exposure and individuals’ emergency preparedness behaviors for coping with natural and human-made disasters. J. Environ. Psychol. 2019, 63, 82–91. [Google Scholar] [CrossRef]
- Kohn, S.; Eaton, J.L.; Feroz, S.; Bainbridge, A.A.; Hoolachan, J.; Barnett, D.J. Personal Disaster Preparedness: An Integrative Review of the Literature. Disaster Med. Public Health Prep. 2012, 6, 217–231. [Google Scholar] [CrossRef]
- McNeill, C.C.; Killian, T.S.; Moon, Z.; Way, K.A.; Betsy Garrison, M.E. The Relationship Between Perceptions of Emergency Preparedness, Disaster Experience, Health-Care Provider Education, and Emergency Preparedness Levels. Int. Q. Community Health Educ. 2018, 38, 233–243. [Google Scholar] [CrossRef]
- Ndu, A.C.; Kassy, W.C.; Ochie, C.N.; Arinze-Onyia, S.U.; Okeke, T.A.; Aguwa, E.N.; Okwor, T.J.; Chinawa, A. Knowledge, Misperceptions, Preparedness, and Barriers towards Lassa Fever Control among Health Care Workers in a Tertiary Institution in Enugu, Nigeria. J. Health Care Poor Underserved 2019, 30, 1151–1164. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.B.; MacKinnon, D.P.; Tein, J.Y. Tests of the three-path mediated effect. Organ. Res. Methods 2008, 11, 241–269. [Google Scholar] [CrossRef]
- Biesanz, J.C.; Falk, C.F.; Savalei, V. Assessing Mediational Models: Testing and Interval Estimation for Indirect Effects. Multivar. Behav. Res. 2010, 45, 661–701. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y. Characteristics of Social Governing Organizations and Governance of Emergent Public Security Events from the Perspective of Public Safety. Rev. De Cercet. Interv. Soc. 2020, 69, 241–260. [Google Scholar]
| Variables | Measurement Items |
|---|---|
| HP | 1. If I should find myself in a jam, I could think of many ways to get out of it. |
| 2. At the present time, I am energetically pursuing my training goals. | |
| 3. There are lots of ways around any problem. | |
| OP | 1. When things are uncertain for me at work, I usually expect the best. |
| 2. I’m optimistic about what will happen to me in the future as it pertains to work. | |
| 3. I approach this job as if “every cloud has a silver lining.” | |
| RES | 1. When I have a setback at work, I have trouble recovering from it, moving on. |
| 2. I usually take stressful things at work in stride. | |
| 3. I feel I can handle many things at a time at work. | |
| SE | 1. I feel confident analyzing a long-term problem to find a solution |
| 2. I feel confident in representing my work area in meetings with management. | |
| 3. I feel confident contacting people outside my organization (e.g., patients) to discuss problems. | |
| AT | 1. I think it is important to participate in emergency preparedness. |
| 2. I think it is beneficial to participate in emergency preparedness. | |
| 3. I think it is necessary to participate in emergency preparedness. | |
| SN | 1. My families encouraged me to participate in emergency preparedness. |
| 2. My friends encouraged me to participate in emergency preparedness. | |
| 3. My managers encouraged me to participate in emergency preparedness. | |
| PBC | 1. I have enough skills of emergency preparedness. |
| 2. I have enough knowledge of emergency preparedness. | |
| 3. I have sufficient resources for conduct emergency preparedness. | |
| EPBI | 1. I will actively participate in the emergency drills in response to major emergencies. |
| 2. I will actively participate in the preparation of public health emergency plans. | |
| 3. I will actively popularize the knowledge and skills related to prevention of public health emergencies to the people around me. |
| Variables | Classification | Quantity | Percentage |
|---|---|---|---|
| Gender | Male | 47 | 19.3 |
| Female | 196 | 80.7 | |
| Age | 18~24 | 91 | 37.4 |
| 25~30 | 29 | 11.9 | |
| 31~40 | 70 | 28.8 | |
| 41~50 | 41 | 16.9 | |
| 51~60 | 12 | 4.9 | |
| Education | Senior high school degree or below | 10 | 4.1 |
| College degree | 58 | 23.9 | |
| Bachelor degree | 152 | 62.6 | |
| Graduate degree or above | 23 | 9.5 | |
| Occupation | Doctor | 58 | 23.9 |
| Nurse | 111 | 45.7 | |
| The administrative staff of the hospital | 12 | 4.9 | |
| The professional staff of the CDC | 1 | 0.4 | |
| The administrative staff of the CDC | 3 | 1.2 | |
| The administrative staff of other health management departments | 15 | 6.2 | |
| Department | Respiratory department | 12 | 4.9 |
| Infection department | 2 | 0.8 | |
| Critical care department | 2 | 0.8 | |
| Otolaryngology Department | 1 | 0.4 | |
| Operating Room | 5 | 2.1 | |
| Emergency department | 4 | 1.6 | |
| Others | 217 | 89.4 | |
| Experience | He/she had the experience of assisting Wuhan during the epidemic | 99 | 40.7 |
| He/she had no experience of assisting Wuhan during the epidemic | 144 | 59.3 |
| Latent Variables | Observation Variables | Mean | SD | Estimate | CR | AVE | Cronbach’s α |
|---|---|---|---|---|---|---|---|
| HP | HP1 | 4.69 | 0.848 | 0.830 | 0.841 | 0.638 | 0.841 |
| HP2 | 4.74 | 0.859 | 0.807 | ||||
| HP3 | 4.86 | 0.753 | 0.758 | ||||
| OP | OP1 | 4.71 | 0.891 | 0.891 | 0.921 | 0.796 | 0.921 |
| OP2 | 4.73 | 0.891 | 0.901 | ||||
| OP3 | 4.79 | 0.852 | 0.885 | ||||
| RES | RE1 | 4.86 | 0.766 | 0.746 | 0.860 | 0.672 | 0.849 |
| RE2 | 4.51 | 0.981 | 0.888 | ||||
| RE3 | 4.47 | 1.017 | 0.820 | ||||
| SE | SE1 | 4.74 | 0.819 | 0.697 | 0.834 | 0.628 | 0.835 |
| SE2 | 4.70 | 0.878 | 0.830 | ||||
| SE3 | 4.71 | 0.887 | 0.842 | ||||
| AT | AT1 | 4.33 | 0.588 | 0.849 | 0.931 | 0.818 | 0.926 |
| AT2 | 4.36 | 0.589 | 0.948 | ||||
| AT3 | 4.36 | 0.610 | 0.913 | ||||
| SN | SN1 | 4.04 | 0.751 | 0.859 | 0.884 | 0.719 | 0.874 |
| SN2 | 4.07 | 0.692 | 0.913 | ||||
| SN3 | 4.19 | 0.666 | 0.765 | ||||
| PBC | PBC1 | 3.74 | 0.874 | 0.821 | 0.908 | 0.767 | 0.903 |
| PBC2 | 3.82 | 0.798 | 0.864 | ||||
| PBC3 | 3.66 | 0.877 | 0.939 | ||||
| EPBI | EPBI1 | 4.18 | 0.674 | 0.884 | 0.891 | 0.732 | 0.887 |
| EPBI2 | 4.18 | 0.668 | 0.892 | ||||
| EPBI3 | 4.20 | 0.700 | 0.787 |
| Variables | HP | OP | RES | SE | AT | SN | PBC | EPBI |
|---|---|---|---|---|---|---|---|---|
| HP | 0.799 | |||||||
| OP | 0.873 *** | 0.892 | ||||||
| RES | 0.922 *** | 0.923 *** | 0.820 | |||||
| SE | 0.976 *** | 0.814 *** | 0.837 *** | 0.792 | ||||
| AT | 0.535 *** | 0.536 *** | 0.445 *** | 0.501 *** | 0.904 | |||
| SN | 0.586 *** | 0.586 *** | 0.562 *** | 0.598 *** | 0.747 *** | 0.848 | ||
| PBC | 0.578 *** | 0.643 *** | 0.662 *** | 0.594 *** | 0.532 *** | 0.723 *** | 0.876 | |
| EPBI | 0.635 *** | 0.637 *** | 0.570 *** | 0.596 *** | 0.821 *** | 0.650 *** | 0.606 *** | 0.856 |
| Hypotheses | β Coefficient | S.E. | C.R. | p-Value | Is it Established? |
|---|---|---|---|---|---|
| Hypothesis 1:AT→EPBI | 0.742 | 0.086 | 9.481 | <0.001 | Yes |
| Hypothesis 2:PBC→EPBI | 0.286 | 0.054 | 3.934 | <0.001 | Yes |
| Hypothesis 3:SN→EPBI | −0.097 | 0.087 | −1.051 | 0.293 | No |
| Hypothesis 4:SN→AT | 0.648 | 0.064 | 8.745 | <0.001 | Yes |
| Hypothesis 5:SN→PBC | 0.494 | 0.086 | 7.291 | <0.001 | Yes |
| Hypothesis 6:PsyCap→AT | 0.152 | 0.065 | 2.294 | 0.022 | Yes |
| Hypothesis 7:PsyCap→PBC | 0.367 | 0.099 | 5.377 | <0.001 | Yes |
| Hypothesis 8:PsyCap→SN | 0.608 | 0.080 | 8.639 | <0.001 | Yes |
| Paths | Indirect Effect | Bias-Corrected | Significance | ||
|---|---|---|---|---|---|
| 95%CI | |||||
| Estimate | Lower | Upper | p-Value | ||
| ①PsyCap→AT→EPBI | 0.122 | 0.005 | 0.279 | 0.040 | Significant |
| ②PsyCap→PBC→EPBI | 0.113 | 0.024 | 0.262 | 0.003 | Significant |
| ③PsyCap→SN→EPBI | −0.063 | −0.227 | 0.076 | 0.303 | Not significant |
| ④SN→AT→EPBI | 0.452 | 0.310 | 0.703 | <0.001 | Significant |
| ⑤SN→PBC→EPBI | 0.133 | 0.055 | 0.250 | 0.002 | Significant |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Zhao, J.; Wang, Y.; Hong, Y. Study on the Formation Mechanism of Medical and Health Organization Staff’s Emergency Preparedness Behavioral Intention: From the Perspective of Psychological Capital. Int. J. Environ. Res. Public Health 2021, 18, 8246. https://doi.org/10.3390/ijerph18168246
Wang H, Zhao J, Wang Y, Hong Y. Study on the Formation Mechanism of Medical and Health Organization Staff’s Emergency Preparedness Behavioral Intention: From the Perspective of Psychological Capital. International Journal of Environmental Research and Public Health. 2021; 18(16):8246. https://doi.org/10.3390/ijerph18168246
Chicago/Turabian StyleWang, Huihui, Jiaqing Zhao, Ying Wang, and Yuxiang Hong. 2021. "Study on the Formation Mechanism of Medical and Health Organization Staff’s Emergency Preparedness Behavioral Intention: From the Perspective of Psychological Capital" International Journal of Environmental Research and Public Health 18, no. 16: 8246. https://doi.org/10.3390/ijerph18168246
APA StyleWang, H., Zhao, J., Wang, Y., & Hong, Y. (2021). Study on the Formation Mechanism of Medical and Health Organization Staff’s Emergency Preparedness Behavioral Intention: From the Perspective of Psychological Capital. International Journal of Environmental Research and Public Health, 18(16), 8246. https://doi.org/10.3390/ijerph18168246







