The Impact of Foot Orthoses and Exercises on Pain and Navicular Drop for Adult Flatfoot: A Network Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Interventions
2.3. Comparisons
2.4. Outcomes
2.5. Study Design
3. Results
3.1. Research Properties
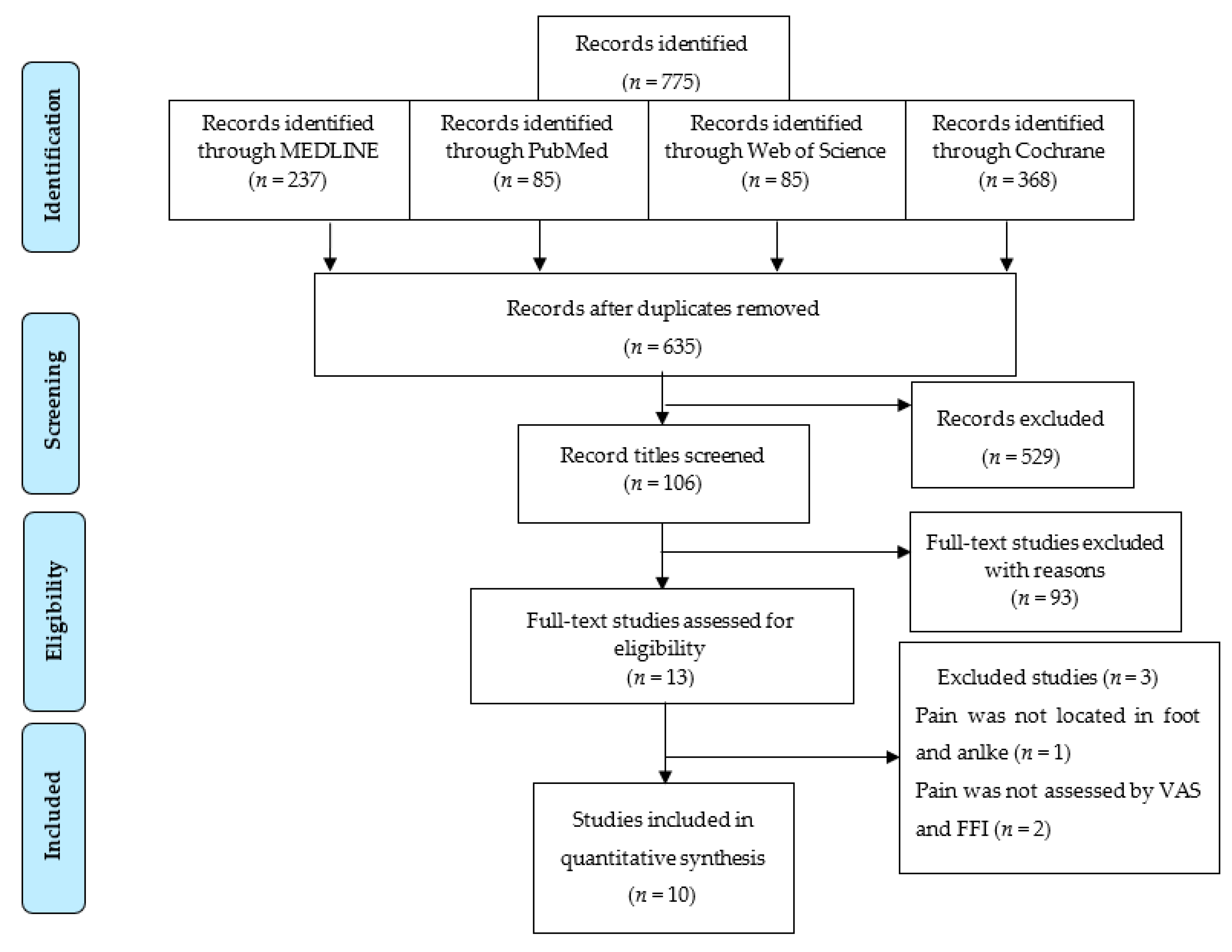
3.1.1. Eligible Studies
3.1.2. Trials and Study Characteristics
3.1.3. Intervention Design
| First Author | Number of Participants | Gender | Active Intervention | Passive Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Participants | Age | BMI | Participants | Age | BMI | Participants | Age | BMI | |||
| Yurt [17] | 45 | F, M | 0 | No | No | 22 | 21.73 (2.89) | 23.03 (3.48) | 23 | 21.09 (1.95) | 23.32 (3.28) |
| 22 | 23.05 (5.53) | 24.11 (4.15) | |||||||||
| Park [20] | 28 | F, M | 14 | 24.71 (1.77) | NR | 0 | No | No | 14 | 23.50 (2.03) | NR |
| Shih [21] | 24 | F, M (18 M, 6 F) | 0 | No | No | 12 | 31.3 (8.3) | 22.3 (2.9) | 12 | 34.4 (9.8) | 23.1 (2.8) |
| Andreasen [16] | 80 | F, M (65 F, 15 M) | 20 | 44 (13) | 26.8 (5.9) * | 20 | 41 (16.2) | 26.4 (5.6) * | 20 | 43 (11.9) | 25.8 (4.33) * |
| 20 | 44 (16.2) | 27.7 (4.8) * | |||||||||
| Kulig [18] | 36 | F, M (28 F, 8 M) | 12 | 55.3 (16.4) | 32.0 (9.24) * | 12 | 51.3 (17.2) | 28.7 (6.26) * | 0 | No | No |
| 12 | 49.4 (12.6) | 28.5 (7.09) * | |||||||||
| Houck [19] | 36 | F, M | 19 | 57 (12) | 30 (6)* | 17 | 58 (9) | 31 (5) * | 0 | No | No |
| Jeong [22] | 12 | F, M | 7 | 52.57 (16.13) | 22.6 (2.37) | 0 | No | No | 5 | 53.2 (12.61) | 24.02 (3.63) |
| Okamura [23] | 20 | F, M (17 F, 3M) | 10 | 19.7 (0.9) | 19.8 (1.4) | 0 | No | No | 10 | 20.2 (1.5) | 21.1 (2.1) |
| Pabón-Carrasco [24] | 90 | F, M | 45 | 19.45 (0.38) | 24.13 (4.16) | 0 | No | No | 45 | 20.92 (1.1) | 21.65 (3.35) |
| Kim [25] | 14 | F, M | 7 | 24.0 (1.9) | NR | 7 | 24.1 (1.5) | NR | 0 | No | No |
| No. | First Author, Year Study Design | Participant Recruitment | Active Intervention | Passive Intervention | Control | Assessment Tools | Follow-Up Time | Results |
|---|---|---|---|---|---|---|---|---|
| 1 | Okamura, 2020 RCT | FPI > 6 | Short foot exercises | No | Control: no intervention | Foot kinematics: 3D motion analysis, navicular drop during gait, FPI, ultrasound muscle thickness | 8 weeks | FPI: inversion/eversion significantly improved; time required for navicular height: minimum value decreased significantly |
| 2 | Pabón-Carrasco, 2020 RCT | FPI > 6 | Short foot exercises | No | Non-biomechanical function (NBF) exercise | NDT and FPI | 4 weeks | No values were found for foot posture between 2 groups; posture was modified in both groups in initial state, and ND value decreased in pain and posture |
| 3 | Yurt, 2018 RCT | FPI > 6 | No | CAD-CAM | Flat insoles | VAS, foot function index, short form−36 | 8 weeks | Pain on CAD-CAM, conventional lower than control after 2 months |
| 4 | Kim, 2016 RCT | NDT > 10 mm | Short foot exercises | Arch support insoles | No | Navicular height NDT, Y balance tests | 5 weeks | NDT: SFE showed significant decrease Y balance: both SFE and insoles showed significant increase |
| 5 | Houck, 2015 RCT | PTTD stage II | Orthoses and stretching and isotonic strengthening | Orthoses and stretching | No | FFI (pain) and short musculoskeletal function assessment | 6 and 12 weeks | Significantly improved pain and function |
| 6 | Andreasen, 2013 RCT | Calcaneal valgus > 6° | Exercise | Insoles | Standard intervention | Pain, static and dynamic foot postures: calcaneal angle, navicular drift, drop, and height | 4 and 12 months | Pain reduction during walking; no differences seen between groups at 4 months |
| Insole and exercise | ||||||||
| 7 | Park, 2012 RCT | Footprint | Abductor hallucis, digit. flexor, anterior and posterior tibialis strengthening | No | Control | Foot structure NDT, mass pressure, motion analysis | 8 weeks | Foot strengthening exercise is feasible and suitable for individuals with hallux valgus with flexible flatfoot Significantly increased outcomes of structural and plantar foot pressure |
| 8 | Shih, 2011 RCT | NDT > 10 mm | No | Custom-made insoles | Control: soft flat insoles | VAS | 2 weeks | Pain incidence reduced in treatment group after 2 weeks, pain intensity score decreased after orthosis application |
| 9 | Kulig, 2009 RCT | Arch index PTTD stage I, II | Orthoses and concentric exercise | Custom-made insoles, stretching | No | VAS pain, 5 MWT, FFI | 6 and 12 weeks | Pain reduced in all groups, orthoses eccentric most improved, orthoses least improved |
| Orthoses and eccentric exercise | ||||||||
| 10 | Jeong, 2007 RCT | PTTD stage I or IIa | Stretching and strengthening, balance training | No | No exercise | Pain, ROM, muscle, AOFAS, 5 MWT | 6 weeks | Reduced pain in exercise group, increased plantar/dorsiflexion |
| First Author | Design | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bilateral Heel Raise | Unilateral Heel Raise | Seated Heel Raise | PF and FAdd | Towel Grasp | Calf Stretching | Shor Foot Exercises | TA Resistance Strengthening | Abductor Halluces Strengthening | Toe Spread | Quadriceps Strengthening | Gluteus Strengthening | Number of Exercises | |
| Kulig [18] | No | No | No | Yes | No | Yes | No | No | No | No | No | No | 2 |
| Houck [19] | Yes | Yes | Yes | No | No | Yes | No | No | No | No | No | No | 4 |
| Yurt [17] | No | Yes | No | No | Yes | Yes | No | No | No | No | No | No | 3 |
| Shih [21] | No | No | No | No | No | No | No | No | No | No | No | No | 0 |
| Kim [25] | No | No | No | No | No | No | Yes | No | No | No | No | No | 1 |
| Andreasen [16] | Yes | Yes | No | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes | 8 |
| Okamura [23] | No | No | No | No | No | No | Yes | No | No | No | No | No | 1 |
| Jeong [22] | Week 3–6 | Week 5–6 | Week 1–6 | Week 1–6 | No | Yes | No | No | No | No | No | No | 5 |
| Pabón-Carrasco [24] | No | No | No | No | No | No | Yes | No | No | No | No | No | 1 |
| Park [20] | No | No | 5 min | No | 5 min | No | No | 5 min | 5 min | No | No | No | 4 |
| First Author | Foot Orthoses Design | Foot Orthoses Details and Properties | Posting | Frequency Wearing Foot Orthoses | |
|---|---|---|---|---|---|
| Rearfoot | MLA | ||||
| Kulig [18] | Orthoses | Biomechanical service, thermo-molded composite, rigid shell | NR | NR | 90% hours walking |
| Houck [19] | AirLift, Aircast | Aircast (DJO Global Inc, Vista, CA, USA) including ankle stirrup and MLA support | NR | NR | 9.9 h a day |
| Yurt [17] | CAD-CAM or conventional insoles | 35 shore A main insoles 3 mm thick, and 15 shore EVA for covering; 4 to 6 mm metatarsal pad | 6° medial heel wedge | 8–12 mm MLA | Frequent use, especially for outdoor activities |
| Shih [21] | Semi-rigid rearfoot medial wedge | 2 mm Poron (rubber-like) | Off-the-shelf 5° EVA | Wedge 6–8 mm from longitudinal midline to medial edge | While running on treadmill |
| Kim [25] | Custom-made orthoses | Thermoplastic (3.2 mm thick Aquaplast-T) | NR | MLA with shore 20°, height at least 15 mm with medial arch support | 30 min 3/week, 5 weeks |
| Andreasen [16] | Custom-made insoles | EVA shore A 35 made by orthotic | NR | NR | 2–8 h/day, compliance not monitored |
3.2. Data Analysis
3.2.1. Study Synthesis
3.2.2. Forest Plot of the Netsplit of Each Outcome
3.2.3. Treatment Effect Ranking
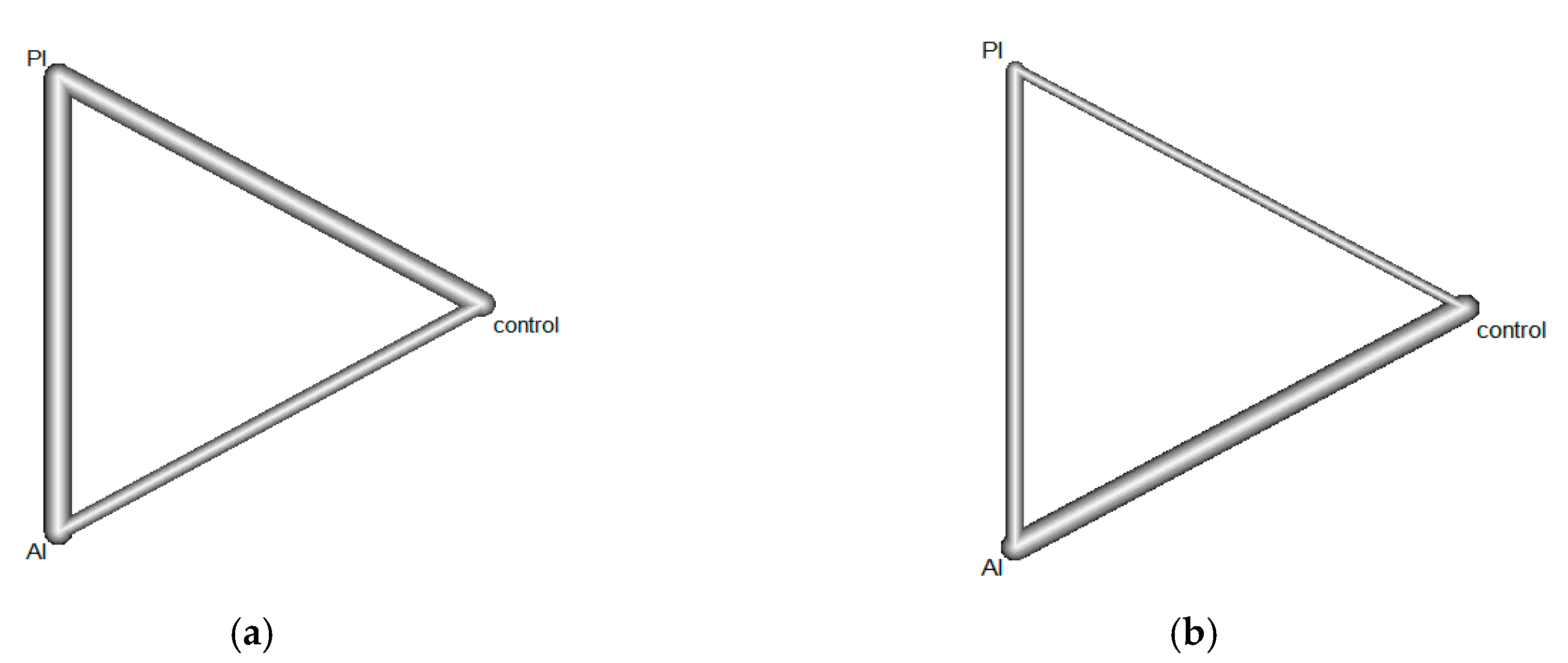
3.3. The Consistency between Evidences
3.4. Heterogeneity among Included Studies
3.5. The Impact of Combination of Exercises and Foot Orthoses Versus Foot Orthoses Alone in Pain on 12 to 16 Weeks Follow-Up
3.6. Risk of Bias and Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pfeiffer, M.; Kotz, R.; Ledl, T.; Hauser, G.; Sluga, M. Prevalence of flat foot in preschool-aged children. Pediatrics 2006, 118, 634–639. [Google Scholar] [CrossRef]
- Arachchige, S.N.K.; Chander, H.; Knight, A. Flatfeet: Biomechanical implications, assessment and management. Foot 2019, 38, 81–85. [Google Scholar] [CrossRef]
- Castro-Mendez, A.; Munuera, P.V.; Albornoz-Cabello, M. The short-term effect of custom-made foot orthoses in subjects with excessive foot pronation and lower back pain: A randomized, double-blinded, clinical trial. Prosthet. Orthot. Int. 2013, 37, 384–390. [Google Scholar] [CrossRef]
- Dabholkar, T. Quality of Life in Adult Population with Flat Feet. Int. J. Health Sci. Res. 2020, 10, 8. [Google Scholar]
- Starkey, C.; Brown, S.D. Examination of Orthopedic & Athletic Injuries; FA Davis: Philadelphia, PA, USA, 2015. [Google Scholar]
- Francisco, R.; Chiodo, C.P.; Wilson, M.G. Management of the rigid adult acquired flatfoot deformity. Foot Ankle Clin. 2007, 12, 317–327. [Google Scholar] [CrossRef]
- Giza, E.; Cush, G.; Schon, L.C. The flexible flatfoot in the adult. Foot Ankle Clin. 2007, 12, 251–271. [Google Scholar] [CrossRef]
- Pita-Fernandez, S.; Gonzalez-Martin, C.; Alonso-Tajes, F.; Seoane-Pillado, T.; Pertega-Diaz, S.; Perez-Garcia, S.; Seijo-Bestilleiro, R.; Balboa-Barreiro, V. Flat foot in a random population and its impact on quality of life and functionality. J. Clin. Diagn. Res. 2017, 11, LC22. [Google Scholar] [CrossRef]
- Haddad, S.L.; Myerson, M.S.; Younger, A.; Anderson, R.B.; Davis, W.H.; Manoli, A., II. Symposium: Adult acquired flatfoot deformity. Foot Ankle Int. 2011, 32, 95–111. [Google Scholar] [CrossRef]
- Nielsen, M.D.; Dodson, E.E.; Shadrick, D.L.; Catanzariti, A.R.; Mendicino, R.W.; Malay, D.S. Nonoperative care for the treatment of adult-acquired flatfoot deformity. J. Foot Ankle Surg. 2011, 50, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Esterman, A.; Pilotto, L. Foot shape and its effect on functioning in Royal Australian Air Force recruits. Part 2: Pilot, randomized, controlled trial of orthotics in recruits with flat feet. Mil. Med. 2005, 170, 629–633. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Jurado, I.; Juárez-Jiménez, J.M.; Munuera-Martínez, P.V. Orthotic treatment for stage I and II posterior tibial tendon dysfunction (flat foot): A systematic review. Clin. Rehabil. 2021, 35, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Banwell, H.A.; Mackintosh, S.; Thewlis, D. Foot orthoses for adults with flexible pes planus: A systematic review. J. Foot Ankle Res. 2014, 7, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, M.H.; Smith, M.D.; Mellor, R.; Vicenzino, B. Exercise for posterior tibial tendon dysfunction: A systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport Exerc. Med. 2018, 4, e000430. [Google Scholar] [CrossRef] [PubMed]
- Hadley, A.; Griffiths, S.; Griffiths, L.; Vicenzino, B. Antipronation taping and temporary orthoses. Effects on tibial rotation position after exercise. J. Am. Podiatr. Med. Assoc. 1999, 89, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.; Mølgaard, C.M.; Christensen, M.; Kaalund, S.; Lundbye-Christensen, S.; Simonsen, O.; Voigt, M. Exercise therapy and custom-made insoles are effective in patients with excessive pronation and chronic foot pain—A randomized controlled trial. Foot 2013, 23, 22–28. [Google Scholar] [CrossRef]
- YURT, SENER and YAKUT Comparison of Two Different Insole Types in Painful Flexible Flatfoot. 2016. Available online: https://clinicaltrials.gov/show/NCT02706327 (accessed on 16 March 2018).
- Kulig, K.; Reischl, S.F.; Pomrantz, A.B.; Burnfield, J.M.; Mais-Requejo, S.; Thordarson, D.B.; Smith, R.W. Nonsurgical Management of Posterior Tibial Tendon Dysfunction With Orthoses and Resistive Exercise: A Randomized Controlled Trial. Phys. Ther. 2009, 89, 26–37. [Google Scholar] [CrossRef] [Green Version]
- Houck, J.; Neville, C.; Tome, J.; Flemister, A. Randomized Controlled Trial Comparing Orthosis Augmented by Either Stretching or Stretching and Strengthening for Stage II Tibialis Posterior Tendon Dysfunction. Foot Ankle Int. 2015, 36, 1006–1016. [Google Scholar] [CrossRef] [Green Version]
- Park, J.H.; Kim, J.S.; Kim, K. The Effect of Foot Strengthening Exercise to Young of Hallux Valgus with Flexible Flatfoot. J. Korea Acad. Ind. Coop. Soc. 2012, 13, 5211–5217. [Google Scholar] [CrossRef]
- Shih, Y.-F.; Wen, Y.-K.; Chen, W.-Y. Application of wedged foot orthosis effectively reduces pain in runners with pronated foot: A randomized clinical study. Clin. Rehabil. 2011, 25, 913–923. [Google Scholar] [CrossRef] [PubMed]
- Jeong, T.H.; Oh, J.K.; Lee, H.J.; Yang, Y.J.; Nha, K.W.; Suh, J.S. The Effect of the Combined Stretching and Strengthening Exercise on the Clinical Symptoms in Posterior Tibial Tendon Dysfunction Patient. J. Korean Foot Ankle Soc. 2008, 12, 47–54. [Google Scholar]
- Okamura, K.; Fukuda, K.; Oki, S.; Ono, T.; Tanaka, S.; Kanai, S. Effects of plantar intrinsic foot muscle strengthening exercise on static and dynamic foot kinematics: A pilot randomized controlled single-blind trial in individuals with pes planus. Gait Posture 2020, 75, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Pabón-Carrasco, M.; Castro-Méndez, A.; Vilar-Palomo, S.; Jiménez-Cebrián, A.M.; García-Paya, I.; Palomo-Toucedo, I.C. Randomized Clinical Trial: The Effect of Exercise of the Intrinsic Muscle on Foot Pronation. Int. J. Environ. Res. Public Health 2020, 17, 4882. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.-K.; Kim, J.S. The effects of short foot exercises and arch support insoles on improvement in the medial longitudinal arch and dynamic balance of flexible flatfoot patients. J. Phys. Ther. Sci. 2016, 28, 3136–3139. [Google Scholar] [CrossRef] [Green Version]
- Rücker, G.; Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 2015, 15, 58. [Google Scholar] [CrossRef] [Green Version]
- Neumann, D.A. Kinesiology of the Musculoskeletal System-e-Book: Foundations for Rehabilitation; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Hollander, K.; De Villiers, J.E.; Sehner, S.; Wegscheider, K.; Braumann, K.-M.; Venter, R.; Zech, A. Growing-up (habitually) barefoot influences the development of foot and arch morphology in children and adolescents. Sci. Rep. 2017, 7, 8079. [Google Scholar] [CrossRef] [Green Version]
- Toullec, E. Adult flatfoot. Orthop. Traumatol. Surg. Res. 2015, 101, S11–S17. [Google Scholar] [CrossRef] [Green Version]
- Cifuentes-De la Portilla, C.; Larrainzar-Garijo, R.; Bayod, J. Analysis of the main passive soft tissues associated with adult acquired flatfoot deformity development: A computational modeling approach. J. Biomech. 2019, 84, 183–190. [Google Scholar] [CrossRef] [Green Version]
- Hamill, J.; Knutzen, K.M. Biomechanical Basis of Human Movement; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Schmalz, T.; Blumentritt, S.; Drewitz, H.; Freslier, M. The influence of sole wedges on frontal plane knee kinetics, in isolation and in combination with representative rigid and semi-rigid ankle-foot-orthoses. Clin. Biomech. 2006, 21, 631–639. [Google Scholar] [CrossRef]
- Michaud, T.C.; Nawoczenski, D.A. The influence of two different types of foot orthoses on first metatarsophalangeal joint kinematics during gait in a single subject. J. Manip. Physiol. Ther. 2006, 29, 60–65. [Google Scholar] [CrossRef]
- Nawoczenski, D.A.; Cook, T.M.; Saltzman, C.L. The effect of foot orthotics on three-dimensional kinematics of the leg and rearfoot during running. J. Orthop. Sports Phys. Ther. 1995, 21, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Tao, X.; Chen, W.; Tang, K. Surgical procedures for treatment of adult acquired flatfoot deformity: A network meta-analysis. J. Orthop. Surg. Res. 2019, 14, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banwell, H.A.; Thewlis, D.; Mackintosh, S. Adults with flexible pes planus and the approach to the prescription of customised foot orthoses in clinical practice: A clinical records audit. Foot 2015, 25, 101–109. [Google Scholar] [CrossRef] [PubMed]



| Outcome | Pain | Navicular Drop | ||||
|---|---|---|---|---|---|---|
| Comparison | AI Vs. PI | AI Vs. Control | PI Vs. Control | AI Vs. PI | AI Vs. Control | PI Vs. Control |
| Number of direct comparisons | 5 | 3 | 4 | 3 | 5 | 1 |
| Study contribution | Andreasen [16] (3) Andreasen [16] (5) Kulig [18] (1) Kulig [18] (2) Houck [19] | Andreasen [16] (2) Andreasen [16] (4) Jeong [22] | Andreasen [16] (1) Yurt [17] (1) Yurt [17] (2) Shih [21] | Kim [25] Andreasen [16] (3) Andreasen [16] (5) | Andreasen [16] (2) Andreasen [16] (4) Park [20] Okamura [23] Pabón-Carrasco [24] | Andreasen [16] (1) |
| Outcomes | Comparison | k | prop | nma | direct | indir | diff | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pain | AI vs. PI | 5 | 0.76 | −0.47 | −0.49 | −0.41 | −0.08 | 0.84 |
| AI vs. control | 3 | 0.5 | −1.23 | −1.19 | −1.27 | 0.08 | 0.84 | |
| PI vs. control | 4 | 0.74 | −0.76 | −0.69 | −0.70 | −0.08 | 0.84 | |
| Navicular drop test | AI vs. control | 5 | 0.72 | −0.19 | −0.26 | −0.01 | −0.25 | 0.61 |
| AI vs. PI | 3 | 0.88 | 0.02 | 0.05 | −0.20 | 0.25 | 0.61 | |
| PI vs. control | 1 | 0.40 | 0.20 | 0.06 | 0.30 | −0.25 | 0.61 |
| Study | Criteria | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | Quality | |
| Houck [19] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 | Fair |
| Kulig [18] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 4/10 | Fair |
| Jeong [22] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 | Good |
| Andreasen [16] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7/10 | Good |
| Kim [25] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4/10 | Fair |
| Park [20] | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 4/10 | Fair |
| Pabón-Carrasco [24] | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7/10 | Good |
| Okamura [23] | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7/10 | Good |
| Yurt [17] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 | Good |
| Shih [21] | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6/10 | Good |
| Méndez [3] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 8/10 | Good |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoang, N.-T.-T.; Chen, S.; Chou, L.-W. The Impact of Foot Orthoses and Exercises on Pain and Navicular Drop for Adult Flatfoot: A Network Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8063. https://doi.org/10.3390/ijerph18158063
Hoang N-T-T, Chen S, Chou L-W. The Impact of Foot Orthoses and Exercises on Pain and Navicular Drop for Adult Flatfoot: A Network Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(15):8063. https://doi.org/10.3390/ijerph18158063
Chicago/Turabian StyleHoang, Ngoc-Tuyet-Trinh, Shuya Chen, and Li-Wei Chou. 2021. "The Impact of Foot Orthoses and Exercises on Pain and Navicular Drop for Adult Flatfoot: A Network Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 15: 8063. https://doi.org/10.3390/ijerph18158063
APA StyleHoang, N.-T.-T., Chen, S., & Chou, L.-W. (2021). The Impact of Foot Orthoses and Exercises on Pain and Navicular Drop for Adult Flatfoot: A Network Meta-Analysis. International Journal of Environmental Research and Public Health, 18(15), 8063. https://doi.org/10.3390/ijerph18158063








