Sleep Quality and Mood State in Resident Physicians during COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Breazzano, M.P.; Shen, J.; Abdelhakim, A.H.; Glass, L.R.D.; Horowitz, J.D.; Xie, S.X.; De Moraes, C.G.; Chen-Plotkin, A.; Chen, R.W.S. New York City COVID-19 resident physician exposure during exponential phase of pandemic. J. Clin. Investig. 2020, 130, 4726–4733. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; He, J. Challenges to the system of reserve medical supplies for public health emergencies: Reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci. Trends 2020, 14. [Google Scholar] [CrossRef] [Green Version]
- He, K.; Stolarski, A.; Whang, E.; Kristo, G. Addressing General Surgery Residents’ Concerns in the Early Phase of the COVID-19 Pandemic. J. Surg. Educ. 2020, 77, 735–738. [Google Scholar] [CrossRef]
- Aaronson, A.L.; Backes, K.; Agarwal, G.; Goldstein, J.L.; Anzia, J. Mental Health During Residency Training: Assessing the Barriers to Seeking Care. Acad. Psychiatry 2018, 42, 469–472. [Google Scholar] [CrossRef]
- Sauerteig, S.O.; Wijesuriya, J.; Tuck, M.; Barham-Brown, H. Doctors’ health and wellbeing: At the heart of the NHS’s mission or still a secondary consideration? Int. Rev. Psychiatry 2019, 31, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Ripp, J.; Peccoralo, L.; Charney, D. Attending to the Emotional Well-Being of the Health Care Workforce in a New York City Health System During the COVID-19 Pandemic. Acad. Med. 2020, 95, 1136–1139. [Google Scholar] [CrossRef]
- Briguglio, G.; Teodoro, M.; Italia, S.; Verduci, F.; Pollicino, M.; Coco, M.; De Vita, A.; Micali, E.; Alibrandi, A.; Lembo, G.; et al. Salivary biomarkers and work-related stress in night shift workers. Int. J. Environ. Res. Public Health 2021, 18, 3184. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Briguglio, G.; Mondello, S.; Teodoro, M.; Pollicino, M.; Canalella, A.; Verduci, F.; Italia, S.; Fenga, C. Perceived Stress in a Gender Perspective: A Survey in a Population of Unemployed Subjects of Southern Italy. Front. Public Health 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Ghasemi, H.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Khaledi-Paveh, B.; Hosseinian-Far, M. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: A systematic review and meta-analysis. Global. Health 2020, 16, 1–14. [Google Scholar]
- Abati, E.; Costamagna, G. Education Research: Effect of the COVID-19 pandemic on neurology trainees in Italy. Neurology 2020, 95, 1061–1066. [Google Scholar] [CrossRef]
- Lo, H.-Y.; Lin, S.-C.; Chaou, C.-H.; Chang, Y.-C.; Ng, C.-J.; Chen, S.-Y. What is the impact of the COVID-19 pandemic on emergency medicine residency training: An observational study. BMC Med. Educ. 2020, 20, 348. [Google Scholar] [CrossRef] [PubMed]
- Odedra, D.; Chahal, B.S.; Patlas, M.N. Impact of COVID-19 on Canadian Radiology Residency Training Programs. Can. Assoc. Radiol. J. 2020, 71, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Ostapenko, A.; McPeck, S.; Liechty, S.; Kleiner, D. Has COVID-19 Hurt Resident Education? A Network-Wide Resident Survey on Education and Experience During the Pandemic. J. Med. Educ. Curric. Dev. 2020, 7, 238212052095969. [Google Scholar] [CrossRef]
- Ey, S.; Soller, M.; Moffit, M. Protecting the Well-Being of Medical Residents and Faculty Physicians During the COVID-19 Pandemic: Making the Case for Accessible, Comprehensive Wellness Resources. Glob. Adv. Health Med. 2020, 9, 216495612097398. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, D.A.; Dawoud, S.A. Resident Perspectives on COVID-19: Three Takeaways. Am. J. Ophthalmol. 2020, 220, A2–A4. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Mondello, S.; Micali, E.; Indelicato, G.; Licciardello, A.A.; Vitale, E.; Briguglio, G.; Teodoro, M.; Fenga, C. Night shift work in resident physicians: Does it affect mood states and cognitive levels? J. Affect. Disord. 2020, 272, 289–294. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [Green Version]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Farnè, M.; Sebellico, A.; Gnugnoli, D.; Corallo, A. Profile od Mood State Manuale di Istruzioni; Organizzazioni Speciali Firenze: Firenze, Italy, 1991. [Google Scholar]
- Alnofaiey, Y.H.; Alshehri, H.A.; Alosaimi, M.M.; Alswat, S.H.; Alswat, R.H.; Alhulayfi, R.M.; Alghamdi, M.A.; Alsubaie, R.M. Sleep disturbances among physicians during COVID-19 pandemic. BMC Res. Notes 2020, 13. [Google Scholar] [CrossRef]
- Sun, Q.; Ji, X.; Zhou, W.; Liu, J. Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. J. Nurs. Manag. 2019, 27, 10–18. [Google Scholar] [CrossRef] [Green Version]
- Wickwire, E.M.; Geiger-Brown, J.; Scharf, S.M.; Drake, C.L. Shift Work and Shift Work Sleep Disorder: Clinical and Organizational Perspectives. Chest 2017, 151, 1156–1172. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, T.; Li, B.; Yu, X.; Ma, Z.; Cao, L.; Gu, Q.; Dong, C.; Jin, Y.; Fan, J.; et al. Job-related factors associated with changes in sleep quality among healthcare workers screening for 2019 novel coronavirus infection: A longitudinal study. Sleep Med. 2020, 75, 21–26. [Google Scholar] [CrossRef]
- Herrero San Martin, A.; Parra Serrano, J.; Diaz Cambriles, T.; Arias Arias, E.M.; Muñoz Méndez, J.; del Yerro Álvarez, M.J.; González Sánchez, M. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med. 2020, 75, 388–394. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Jiang, W.; Liu, X.; Zhang, J.; Feng, Z. Mental health status of Chinese residents during the COVID-19 epidemic. BMC Psychiatry 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Lasalvia, A.; Bonetto, C.; Porru, S.; Carta, A.; Tardivo, S.; Bovo, C.; Ruggeri, M.; Amaddeo, F. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol. Psychiatr. Sci. 2021, 30. [Google Scholar] [CrossRef]
- Collins, C.; Mahuron, K.; Bongiovanni, T.; Lancaster, E.; Sosa, J.A.; Wick, E. Stress and the Surgical Resident in the COVID-19 Pandemic. J. Surg. Educ. 2021, 78, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Arafa, A.; Mohammed, Z.; Mahmoud, O.; Elshazley, M.; Ewis, A. Depressed, anxious, and stressed: What have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J. Affect. Disord. 2021, 278, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Togo, F.; Yoshizaki, T.; Komatsu, T. Association between depressive symptoms and morningness-eveningness, sleep duration and rotating shift work in Japanese nurses. Chronobiol. Int. 2017, 34, 349–359. [Google Scholar] [CrossRef]
| Overall | Anesthesiology | Medicine | Service | Surgery | p-Value | |
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Sociodemographic factors | ||||||
| Total | 119 (100.00) | 29 (24.17) | 33 (27.50) | 32 (26.67) | 25 (20.83) | |
| Gender | ||||||
| Male | 56 (47.06) | 6 (20.69) | 14 (42.42) | 16 (50.00) | 20 (80.00) | <0.001 |
| Female | 63 (52.94) | 23 (79.31) | 19 (57.58) | 16 (50.00) | 5 (20.00) | |
| Age | ||||||
| Mean ± SD | 30.66 ± 3.04 | 31.79 ± 3.59 | 29.45 ± 1.86 | 31.06 ± 3.66 | 32.24 ± 6.22 | 0.015 |
| Range | 27–47 | 28–47 | 27–34 | 27–41 | 27–35 | |
| Marital status | ||||||
| Married | 15 (12.61) | 3 (10.34) | 3 (9.09) | 7 (21.88) | 2 (8.00) | 0.390 |
| Unmarried | 104 (87.39) | 26 (89.66) | 30 (90.91) | 25 (78.13) | 23 (92.00) | |
| Parenthood | ||||||
| Yes | 12 (10.08) | 1 (3.45) | 3 (9.09) | 7 (21.88) | 1 (4.00) | 0.099 |
| No | 107 (89.92) | 28 (96.55) | 30 (90.91) | 25 (78.13) | 24 (96.00) | |
| Health and lifestyle factors | ||||||
| BMI | ||||||
| Mean ± SD | 23.55 ± 3.25 | 23.21 ± 3.77 | 23.12 ± 3.11 | 23.18 ± 3.00 | 24.98 ± 2.82 | 0.059 |
| Smoking habit | ||||||
| Yes | 43 (36.13) | 11 (37.93) | 7 (21.21) | 13 (40.63) | 12 (48.00) | 0.170 |
| No | 76 (63.87) | 18 (62.07) | 26 (78.79) | 19 (59.38) | 13 (52.00) | |
| Alcohol intake | ||||||
| Yes | 56 (47.06) | 14 (48.28) | 16 (48.48) | 13 (40.63) | 13 (52.00) | 0.844 |
| No | 63 (52.94) | 15 (51.72) | 17 (51.52) | 19 (59.38) | 12 (48.00) | |
| Drugs | ||||||
| Yes | 20 (16.81) | 5 (17.24) | 8 (24.24) | 3 (9.38) | 4 (16.00) | 0.475 |
| No | 99 (83.19) | 24 (82.76) | 25 (75.76) | 29 (90.63) | 21 (84.00) | |
| Work-related factors | ||||||
| Year in residency program | ||||||
| First | 24 (20.00) | 0 (0.00) | 3 (9.09) | 14 (43.75) | 7 (28.00) | <0.001 |
| Second | 24 (20.00) | 3 (10.34) | 14 (42.42) | 3 (9.38) | 4 (16.00) | |
| Third | 39 (32.50) | 15 (51.72) | 10 (30.30) | 10 (31.25) | 3 (12.00) | |
| Fourth | 26 (21.67) | 8 (27.59) | 6 (18.18) | 5 (15.63) | 7 (28.00) | |
| Fifth | 7 (5.83) | 3 (10.34) | 0 (0.00) | 0 (0.00) | 4 (16.00) | |
| Night shifts | ||||||
| Yes | 75 (63.03) | 29 (100.00) | 18 (54.55) | 9 (28.13) | 19 (76.00) | <0.001 |
| No | 44 (36.97) | 0 (0.00) | 15 (45.45) | 23 (71.88) | 6 (24.00) | |
| Hours per week | ||||||
| Mean ± SD | 41.39 ± 6.86 | 40.62 ± 4.46 | 42.42 ± 8.43 | 39.22 ± 4.13 | 43.68 ± 8.78 | 0.067 |
| Overall | Anesthesiology | Medicine | Service | Surgery | p-Value | |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| ESS | 6.47 ± 2.98 | 7.17 ± 2.98 | 5.94 ± 2.67 | 5.88 ± 3.14 | 7.12 ± 3.05 | 0.233 |
| PSQI | 6.20 ± 2.83 | 6.03 ± 2.57 | 6.24 ± 3.61 | 6.28 ± 2.51 | 6.24 ± 2.47 | 0.790 |
| POMS | 43.09 ± 34.92 | 53.52 ± 40.55 | 43.15 ± 33.74 | 36.47 ± 32.36 | 39.40 ± 31.69 | 0.552 |
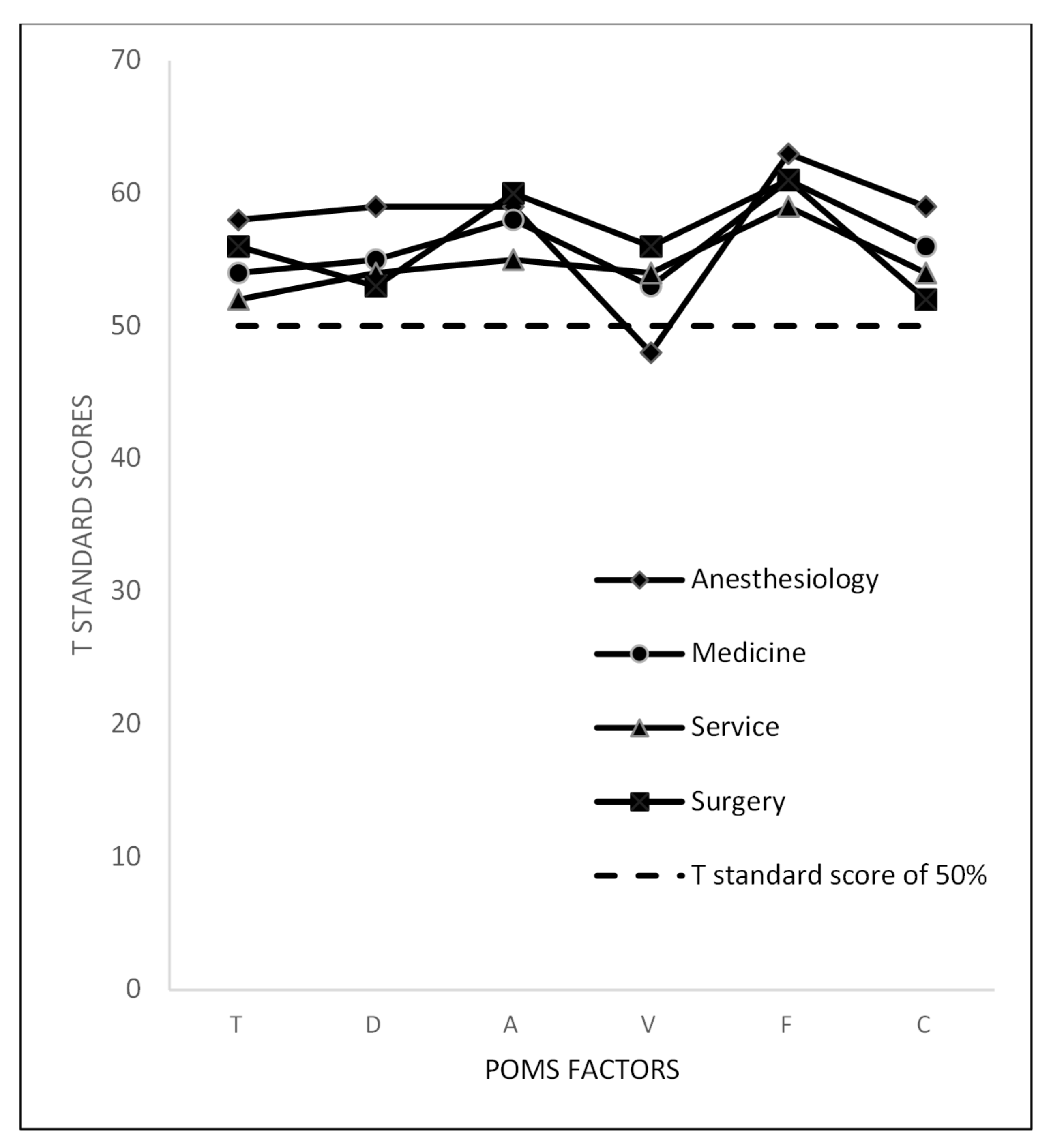
| POMS factors | ||||||
| Tension (T) | 12.31 ± 5.65 | 14.14 ± 5.95 | 11.79 ± 5.50 | 10.94 ± 5.36 | 12.64 ± 5.57 | 0.197 |
| Depression (D) | 12.98 ± 10.43 | 15.62 ± 13.18 | 12.82 ± 9.51 | 12.09 ± 10.24 | 11.28 ± 7.96 | 0.731 |
| Anger (A) | 13.17 ± 9.53 | 14.21 ± 11.03 | 12.97 ± 8.94 | 11.31 ± 9.43 | 14.60 ± 8.68 | 0.560 |
| Vigor (V) | 16.71 ± 5.26 | 14.00 ± 4.88 | 16.79 ± 5.05 | 17.44 ± 5.27 | 18.84 ± 4.92 | 0.010 |
| Fatigue (F) | 10.95 ± 4.66 | 11.76 ± 4.30 | 11.30 ± 4.99 | 9.91 ± 5.05 | 10.88 ± 4.10 | 0.512 |
| Confusion (C) | 10.39 ± 4.92 | 11.79 ± 4.69 | 11.06 ± 5.19 | 9.66 ± 4.75 | 8.84 ± 4.67 | 0.139 |
| Overall | Anesthesiology | Medicine | Service | Surgery | p-Value | |
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| ESS | ||||||
| ≤10 | 110 (92.44) | 25 (86.21) | 33 (100.00) | 30 (93.75) | 22 (88.00) | 0.107 |
| >10 | 9 (7.56) | 4 (13.79) | 0 (0.00) | 2 (6.25) | 3 (12.00) | |
| PSQI | ||||||
| ≤5 | 66 (55.46) | 19 (65.52) | 20 (60.61) | 16 (50.00) | 11 (44.00) | 0.531 |
| 6–10 | 41 (34.45) | 7 (24.14) | 9 (27.27) | 14 (43.75) | 11 (44.00) | |
| >10 | 12 (10.08) | 3 (10.34) | 4 (12.12) | 2 (6.25) | 3 (12.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, C.; Teodoro, M.; Briguglio, G.; Vitale, E.; Giambò, F.; Indelicato, G.; Micali, E.; Italia, S.; Fenga, C. Sleep Quality and Mood State in Resident Physicians during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 8023. https://doi.org/10.3390/ijerph18158023
Costa C, Teodoro M, Briguglio G, Vitale E, Giambò F, Indelicato G, Micali E, Italia S, Fenga C. Sleep Quality and Mood State in Resident Physicians during COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(15):8023. https://doi.org/10.3390/ijerph18158023
Chicago/Turabian StyleCosta, Chiara, Michele Teodoro, Giusi Briguglio, Ermanno Vitale, Federica Giambò, Giuliano Indelicato, Elvira Micali, Sebastiano Italia, and Concettina Fenga. 2021. "Sleep Quality and Mood State in Resident Physicians during COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 15: 8023. https://doi.org/10.3390/ijerph18158023
APA StyleCosta, C., Teodoro, M., Briguglio, G., Vitale, E., Giambò, F., Indelicato, G., Micali, E., Italia, S., & Fenga, C. (2021). Sleep Quality and Mood State in Resident Physicians during COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(15), 8023. https://doi.org/10.3390/ijerph18158023










