Full Zirconia Implant-Born Prosthetic Rehabilitation with CAD/CAM Technology after Accurate Digital Planning. A Case Report
Abstract
1. Introduction
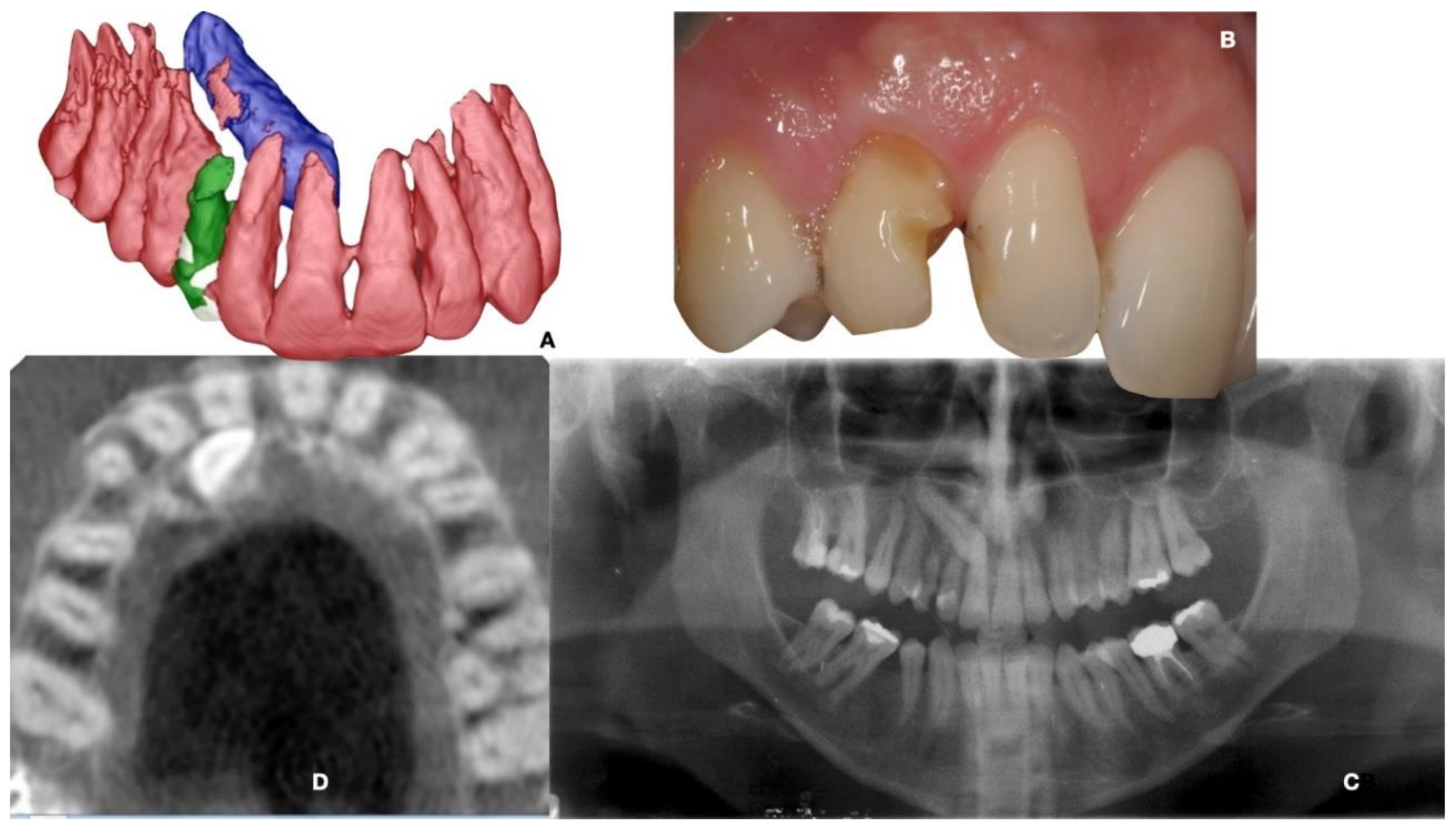
2. Materials and Methods
2.1. Planning
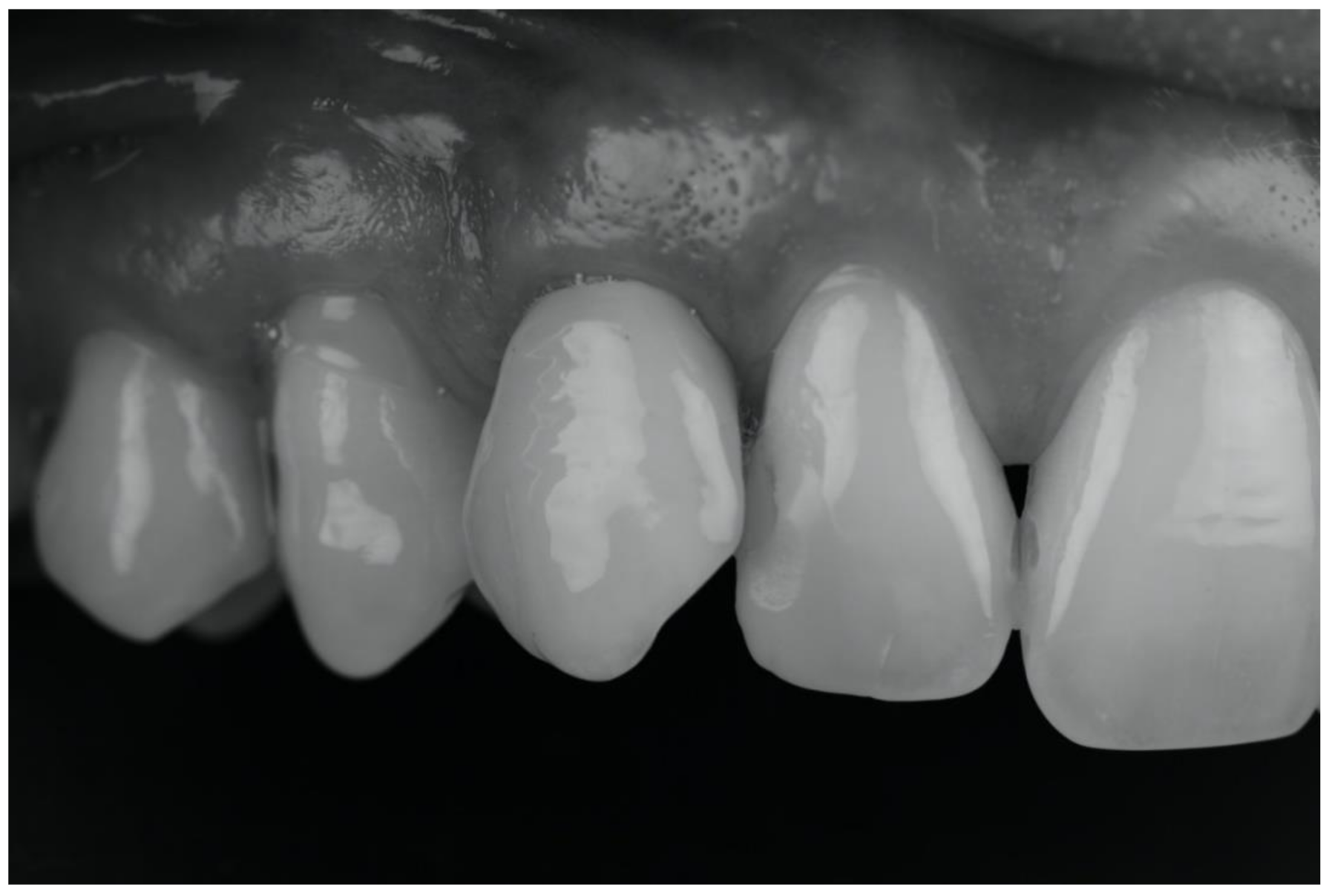
2.2. Surgical and Prosthetic Procedure
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef]
- Cionca, N.; Hashim, D.; Mombelli, A. Zirconia dental implants: Where are we now, and where are we heading? Periodontol 2000, 73, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Cionca, N.; Müller, N.; Mombelli, A. Two-piece zirconia implants supporting all-ceramic crowns: A prospective clinical study. Clin Oral Implant. Res. 2015, 26, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Cattoni, F.; Tetè, G.; Calloni, A.M.; Manazza, F.; Gastaldi, G.; Capparè, P. Milled versus moulded mock-ups based on the superimposition of 3D meshes from digital oral impressions: A comparative in vitro study in the aesthetic area. BMC Oral Health. 2019, 19, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Franchina, A.; Stefanelli, L.V.; Gorini, S.; Fedi, S.; Lizio, G.; Pellegrino, G. Digital Approach for the Rehabilitation of the Edentulous Maxilla with Pterygoid and Standard Implants: The Static and Dynamic Computer-Aided Protocols. Methods Protoc. 2020, 3, 84. [Google Scholar] [CrossRef]
- Bormann, K.H.; Gellrich, N.C.; Kniha, H.; Dard, M.; Wieland, M.; Gahlert, M. Biomechanical evaluation of a microstructured zirconia implant by a removal torque comparison with a standard Ti-SLA implant. Clin. Oral Implant. Res. 2012, 23, 1210–1216. [Google Scholar] [CrossRef]
- Kontonasaki, E.; Giasimakopoulos, P.; Rigos, A.E. Strength and aging resistance of monolithic zirconia: An update to current knowledge. Jpn. Dent. Sci. Rev. 2020, 56, 1–23. [Google Scholar] [CrossRef]
- Kapos, T.; Evans, C. CAD/CAM technology for implant abutments, crowns, and superstructures. Int. J. Oral Maxillofac. Implant. 2014, 29, 117–136. [Google Scholar] [CrossRef]
- Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef]
- Grohmann, P.; Bindl, A.; Hämmerle, C.; Mehl, A.; Sailer, I. Three-unit posterior zirconia-ceramic fixed dental prostheses (FDPs) veneered with layered and milled (CAD-on) veneering ceramics: 1-year follow-up of a randomized controlled clinical trial. Quintessence Int. 2015, 46, 871–880. [Google Scholar] [CrossRef]
- Müller, K.; Valentine-Thon, E. Hypersensitivity to titanium: Clinical and laboratory evidence. Neuro Endocrinol. Lett. 2006, 27 (Suppl. S1), 31–35. [Google Scholar]
- Oum’hamed, Z.; Garnotel, R.; Josset, Y.; Trenteseaux, C.; Laurent-Maquin, D. Matrix metalloproteinases MMP-2, -9 and tissue inhibitors TIMP-1, -2 expression and secretion by primary human osteoblast cells in response to titanium, zirconia, and alumina ceramics. J. Biomed. Mater. Research. Part A 2004, 68, 114–122. [Google Scholar] [CrossRef]
- Koth, D.L.; McKinney, R.V.; Steflik, D.E.; Davis, Q.B. Clinical and statistical analyses of human clinical trials with the single crystal aluminum oxide endosteal dental implant: Five-year results. J. Prosthet. Dent. 1988, 60, 226–234. [Google Scholar] [CrossRef]
- Sandhaus, S. Technic and instrumentation of the implant C.B.S. (Cristalline Bone Screw). Inf. Odonto-Stomatol. 1968, 4, 19–24. [Google Scholar]
- Balmer, M.; Spies, B.C.; Kohal, R.J.; Hämmerle, C.H.; Vach, K.; Jung, R.E. Zirconia implants restored with single crowns or fixed dental prostheses: 5-year results of a prospective cohort investigation. Clin. Oral Implant. Res. 2020, 31, 452–462. [Google Scholar] [CrossRef]
- Apratim, A.; Eachempati, P.; Krishnappa Salian, K.K.; Singh, V.; Chhabra, S.; Shah, S. Zirconia in dental implantology: A review. J. Int. Soc. Prev. Community Dent. 2015, 5, 147–156. [Google Scholar] [CrossRef]
- Covacci, V.; Bruzzese, N.; Maccauro, G.; Andreassi, C.; Ricci, G.A.; Piconi, C.; Marmo, E.; Burger, W.; Cittadini, A. In vitro evaluation of the mutagenic and carcinogenic power of high purity zirconia ceramic. Biomaterials 1999, 20, 371–376. [Google Scholar] [CrossRef]
- Roehling, S.; Gahlert, M.; Janner, S.; Meng, B.; Woelfler, H.; Cochran, D.L. Ligature-Induced Peri-implant Bone Loss Around Loaded Zirconia and Titanium Implants. Int. J. Oral Maxillofac. Implant. 2019, 34, 357–365. [Google Scholar] [CrossRef]
- Bömicke, W.; Rammelsberg, P.; Stober, T.; Schmitter, M. Short-Term Prospective Clinical Evaluation of Monolithic and Partially Veneered Zirconia Single Crowns. J. Esthet. Restor. Dent. 2017, 29, 22–30. [Google Scholar] [CrossRef]
- Moscovitch, M. Consecutive case series of monolithic and minimally veneered zirconia restorations on teeth and implants: Up to 68 months. Int. J. Periodontics Restor. Dent. 2015, 35, 315–323. [Google Scholar] [CrossRef]
- Sicilia, A.; Cuesta, S.; Coma, G.; Arregui, I.; Guisasola, C.; Ruiz, E.; Maestro, A. Titanium allergy in dental implant patients: A clinical study on 1500 consecutive patients. Clin. Oral Implant. Res. 2008, 19, 823–835. [Google Scholar] [CrossRef]
- Chappuis, V.; Cavusoglu, Y.; Gruber, R.; Kuchler, U.; Buser, D.; Bosshardt, D.D. Osseointegration of Zirconia in the Presence of Multinucleated Giant Cells. Clin. Implant Dent. Relat. Res. 2016, 18, 686–698. [Google Scholar] [CrossRef]
- Özkurt, Z.; Kazazoğlu, E. Zirconia dental implants: A literature review. J. Oral Implantol. 2011, 37, 367–376. [Google Scholar] [CrossRef]
- Tetè, G.; Sacchi, L.; Camerano, C.; Nagni, M.; Capelli, O.; Vercellin, S.G.; la Rocca, G.; Polizzi, E. Management of the delicate phase of the temporary crown: An in vitro study. J. Biol. Regul. Homeost Agents. 2020, 34 (Suppl. S3), 69–80. [Google Scholar]
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, D.S. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implant. Res. 2012, 23 (Suppl. S6), 2–21. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Thoma, D.; Jung, R.; Zwahlen, M.; Zembic, A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin. Oral Implant. Res. 2012, 23 (Suppl. S6), 22–38. [Google Scholar] [CrossRef] [PubMed]
- Laurell, L.; Lundgren, D. Marginal bone level changes at dental implants after 5 years in function: A meta-analysis. Clin. Implant Dent. Relat. Res. 2011, 13, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Borgonovo, A.E.; Censi, R.; Vavassori, V.; Arnaboldi, O.; Maiorana, C.; Re, D. Zirconia Implants in Esthetic Areas: 4-Year Follow-Up Evaluation Study. Int. J. Dent. 2015, 2015, 415029. [Google Scholar] [CrossRef] [PubMed]
- Roehling, S.; Woelfler, H.; Hicklin, S.; Kniha, H.; Gahlert, M. A Retrospective Clinical Study with Regard to Survival and Success Rates of Zirconia Implants up to and after 7 Years of Loading. Clin. Implant Dent. Relat. Res. 2016, 18, 545–558. [Google Scholar] [CrossRef]
- Ferrari, M.; Tricarico, M.G.; Cagidiaco, M.C.; Vichi, A.; Gherlone, E.F.; Zarone, F.; Sorrentino, R. 3-Year Random-ized Controlled Prospective Clinical Trial on Different CAD-CAM Implant Abutments. Clin. Implant Dent. Relat. Res. 2016, 18, 1134–1141. [Google Scholar] [CrossRef]
- Payer, M.; Heschl, A.; Koller, M.; Arnetzl, G.; Lorenzoni, M.; Jakse, N. All-ceramic restoration of zirconia two-piece implants--a randomized controlled clinical trial. Clin. Oral Implant. Res. 2015, 26, 371–376. [Google Scholar] [CrossRef]
- Becker, J.; John, G.; Becker, K.; Mainusch, S.; Diedrichs, G.; Schwarz, F. Clinical performance of two-piece zirconia implants in the posterior mandible and maxilla: A prospective cohort study over 2 years. Clin. Oral Implant. Res. 2017, 28, 29–35. [Google Scholar] [CrossRef]
- Brüll, F.; van Winkelhoff, A.J.; Cune, M.S. Zirconia dental implants: A clinical, radiographic, and microbiologic evaluation up to 3 years. Int. J. Oral Maxillofac. Implant. 2014, 29, 914–920. [Google Scholar] [CrossRef]
- Spies, B.C.; Balmer, M.; Jung, R.E.; Sailer, I.; Vach, K.; Kohal, R.J. All-ceramic, bi-layered crowns supported by zirconia implants: Three-year results of a prospective multicenter study. J. Dent. 2017, 67, 58–65. [Google Scholar] [CrossRef][Green Version]
- Ferrini, F.; Sannino, G.; Chiola, C.; Capparé, P.; Gastaldi, G.; Gherlone, E.F. Influence of Intra-Oral Scanner (I.O.S.) on The Marginal Accuracy of CAD/CAM Single Crowns. Int. J. Env. Res. Public Health 2019, 16, 544. [Google Scholar] [CrossRef]
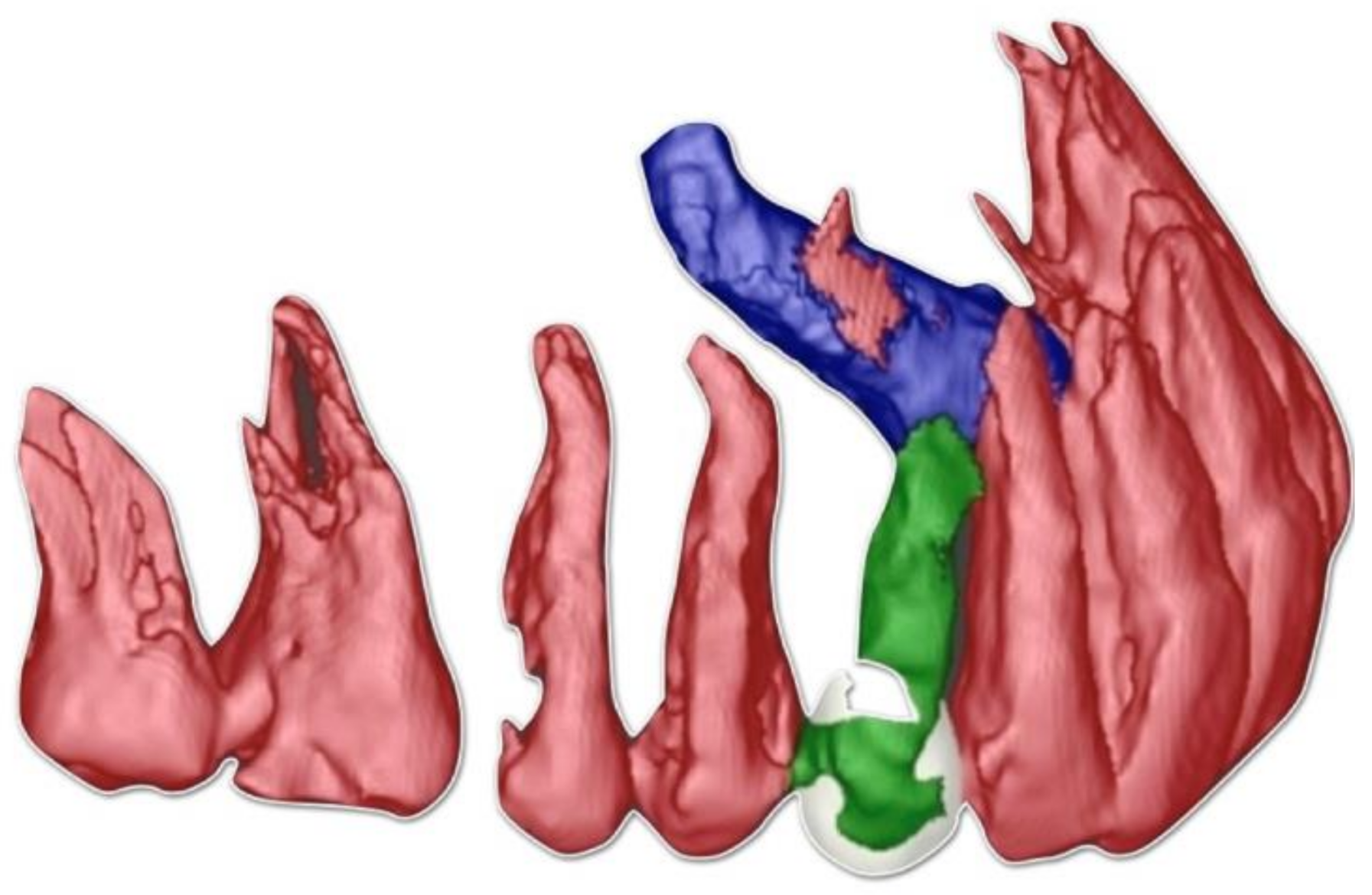




| (a) Surgical removal of the deciduous tooth and orthodontic extrusion, and taking in occlusion of the permanent canine |
| (b) Conservative treatment of the deciduous tooth living in situ with the impacted canine |
| (c) Removal of the deciduous tooth and involvement of the adjacent natural elements for a fixed conventional or adhesive bridge living in situ with the impacted canine |
| (d) Removal of the deciduous tooth and replacement with implant-borne-prosthesis living in situ with the impacted canine, accepting the compromise of involving the impacted tooth in the implant seating procedure |
| (e) Surgical removal of the impacted canine and, in a second stage, removal of the deciduous tooth and replacement with implant-borne-prosthesis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scaringi, R.; Nannelli, M.; Franchina, A.; Lizio, G.; Stefanelli, L.V.; Pagliarulo, M.; De Angelis, F.; Pellegrino, G. Full Zirconia Implant-Born Prosthetic Rehabilitation with CAD/CAM Technology after Accurate Digital Planning. A Case Report. Int. J. Environ. Res. Public Health 2021, 18, 7998. https://doi.org/10.3390/ijerph18157998
Scaringi R, Nannelli M, Franchina A, Lizio G, Stefanelli LV, Pagliarulo M, De Angelis F, Pellegrino G. Full Zirconia Implant-Born Prosthetic Rehabilitation with CAD/CAM Technology after Accurate Digital Planning. A Case Report. International Journal of Environmental Research and Public Health. 2021; 18(15):7998. https://doi.org/10.3390/ijerph18157998
Chicago/Turabian StyleScaringi, Riccardo, Michele Nannelli, Alessio Franchina, Giuseppe Lizio, Luigi V. Stefanelli, Michele Pagliarulo, Francesca De Angelis, and Gerardo Pellegrino. 2021. "Full Zirconia Implant-Born Prosthetic Rehabilitation with CAD/CAM Technology after Accurate Digital Planning. A Case Report" International Journal of Environmental Research and Public Health 18, no. 15: 7998. https://doi.org/10.3390/ijerph18157998
APA StyleScaringi, R., Nannelli, M., Franchina, A., Lizio, G., Stefanelli, L. V., Pagliarulo, M., De Angelis, F., & Pellegrino, G. (2021). Full Zirconia Implant-Born Prosthetic Rehabilitation with CAD/CAM Technology after Accurate Digital Planning. A Case Report. International Journal of Environmental Research and Public Health, 18(15), 7998. https://doi.org/10.3390/ijerph18157998










