COVID-19 Preparedness and Perceived Safety in Nursing Homes in Southern Portugal: A Cross-Sectional Survey-Based Study in the Initial Phases of the Pandemic
Abstract
:1. Introduction
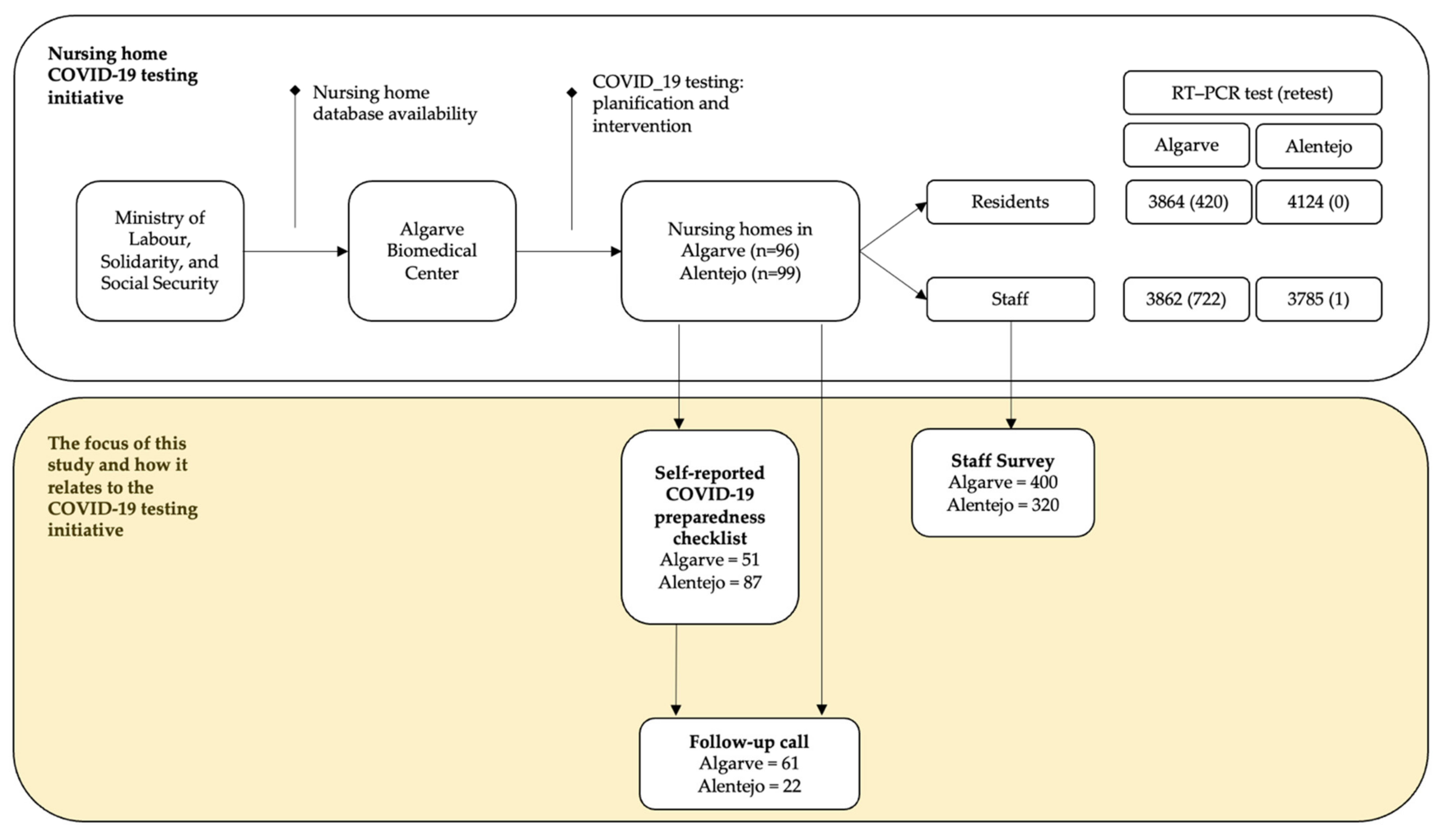
2. Materials and Methods
2.1. Study Design and Population
2.2. Instruments
2.2.1. COVID-19 Preparedness Checklist
2.2.2. Staff Survey
2.3. Statistical Analysis
3. Results
3.1. Nursing Home COVID-19 Preparedness
- poor communication channels, both internal and external, often failing to disseminate the contingency plan among key stakeholders (e.g., staff) and engaging with health and other competent authorities;
- inexistent or poor planning to isolate or transfer residents if need be;
- poor surveillance systems to monitor for symptoms among residents and staff;
- insufficient planning to overcome hindrances related to staff shortages and absenteeism, and infrastructure constraints (e.g., bed overcapacity in isolation rooms);
- the inexistent monitoring system of the effectiveness of the measures aiming at addressing behavioral factors, both at the institutional and individual level;
- misuse of personal protective equipment (PPE) attributed to poor training and a generalized shortage of specific equipment (e.g., gowns and FFP2 face masks).
- continuous revision of the contingency plan to reflect any updates to the guidelines set forth by the Directorate—General of Health and other relevant competent authorities;
- emergency protocol with the nearest primary health care centers for a quick response in case of an outbreak;
- systematically maintaining an inventory of PPE in close collaboration with governmental authorities;
- using social media and other platforms to update families and carers on residents’ well-being and on the public health measures that the nursing home is developing.
3.2. Perceived Safety and Well-Being among Nursing Home Staff
3.3. Fear and Absenteeism Attributed to COVID-19
3.4. Experiences with Coping with the Pandemic
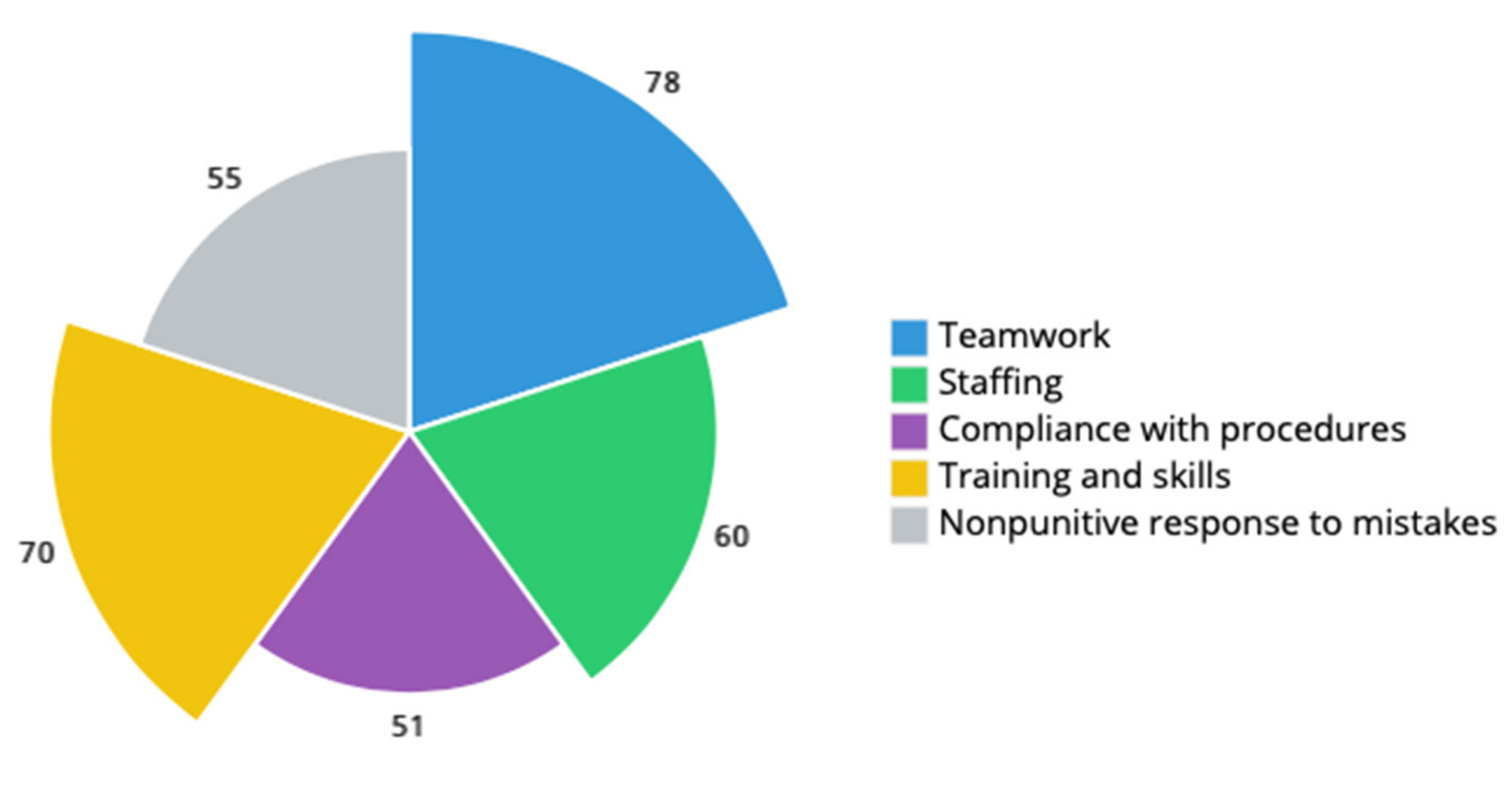
3.5. Nursing Home Resident Safety Culture
4. Discussion
Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021. [Google Scholar] [CrossRef] [PubMed]
- Merkur, S.; Maresso, A.; Cylus, J.; Ginneken Ev Lessof, S. Lessons from the first wave: The COVID-19 health system response monitor (HSPM). An evidence resource and a source of analysis. Eurohealth 2020, 26, 5–12. [Google Scholar]
- Green, C.; Manthorpe, J.; Steils, N.; Stevens, M.; Martineau, S.; Woolham, J.; Orellana, K.; Norrie, C.; Ionescu, A.; Wiskerke, E.; et al. International policy responses and early management of threats posed by the SARS-CoV-2 pandemic to social care. J. Long Term Care 2020, 108–117. [Google Scholar] [CrossRef]
- Quigley, D.D.; Dick, A.; Agarwal, M.; Jones, K.M.; Mody, L.; Stone, P.W. COVID-19 preparedness in nursing homes in the midst of the pandemic. J. Am. Geriatr. Soc. 2020, 68, 1164–1166. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.C.; Barbu, M.G.; Beiu, C.; Popa, L.G.; Mihai, M.M.; Berteanu, M.; Popescu, M.N. The impact of COVID-19 pandemic on long-term care facilities worldwide: An overview on international issues. Biomed. Res. Int. 2020, 2020, 8870249. [Google Scholar] [CrossRef]
- American Geriatrics Society. American Geriatrics Society policy brief: COVID-19 and nursing homes. J. Am. Geriatr. Soc. 2020, 68, 908–911. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Forum on Microbial Threats. The Threat of Pandemic Influenza: Are We Ready? Workshop Summary; Knobler, S.L., Mack, A., Mahmoud, A., Lemon, S.M., Eds.; National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- World Health Organization. WHO Report on Global Surveillance of Epidemic-Prone Infectious Diseases. Available online: http://apps.who.int/iris/handle/10665/66485 (accessed on 20 July 2021).
- Organisation for Economic Co-Operation and Development. Workforce and Safety in Long-Term Care during the COVID-19 Pandemic; OECD: Paris, France, 2020. [Google Scholar]
- Organisation for Economic Co-Operation and Development. Who Cares? Attracting and Retaining Care Workers for the Elderly; OECD: Paris, France, 2020. [Google Scholar]
- World Health Organization. Preventing and Managing COVID-19 across Long-Term Care Services: Policy Brief; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Yount, N.; Zebrak, K.A.; Famolaro, T.; Sorra, J.; Birch, R. Linking patient safety culture to quality ratings in the nursing home setting. J. Appl. Gerontol. 2020, 733464820969283. [Google Scholar] [CrossRef] [PubMed]
- Bonner, A.F.; Castle, N.G.; Perera, S.; Handler, S.M. Patient safety culture: A review of the nursing home literature and recommendations for practice. Ann. Long Term Care 2008, 16, 18–22, PMID: 21701601. [Google Scholar] [PubMed]
- Gartshore, E.; Waring, J.; Timmons, S. Patient safety culture in care homes for older people: A scoping review. BMC Health Serv. Res. 2017, 17, 752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Bienassis, K.; Kristensen, S.; Burtscher, M.; Brownwood, I.; Klazinga, N.S. Culture as a cure: Assessments of patient safety culture in OECD countries. In OECD Health Working Papers; OECD: Paris, France, 2020. [Google Scholar]
- Comas-Herrera, A.; Zalakaín, J.; Litwin, C.; Hsu, A.T.; Lemmon, E.; Henderson, D.; Litwin, C.; Hsu, A.T.; Schmidt, A.E.; Arling, G.; et al. Mortality Associated with COVID-19 Outbreaks in Care Homes: Early International Evidence. International Long Term Care Policy Network. 2020. Available online: https://ltccovid.org/2020/04/12/mortality-associated-with-covid-19-outbreaks-in-care-homes-early-international-evidence (accessed on 26 June 2020).
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19) Preparedness Checklist for Nursing Homes and Other Long-Term Care Setting. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/downloads/novel-coronavirus-2019-Nursing-Homes-Preparedness-Checklist_3_13.pdf (accessed on 20 July 2021).
- Ministério da Administração Interna. Relatório Sobre a Aplicação da 3.ª Declaração do Estado de Emergência; Ministério da Administração Interna: Lisbon, Portugal, 2020. [Google Scholar]
- Agency for Healthcare Research and Quality. Nursing Home Survey on Patient Safety Culture. 2020. Available online: https://www.ahrq.gov/sops/surveys/nursing-home/index.html (accessed on 20 July 2021).
- Psykiatric Center North Zealand. The WHO-5 Website. 2020. Available online: https://www.psykiatri-regionh.dk/who-5/Pages/default.aspx (accessed on 20 July 2021).
- Eurostat. Glossary: Minimum European Health Module (MEHM). Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php/Glossary:Minimum_European_Health_Module_(MEHM) (accessed on 20 July 2021).
- Directorate-General of Health. COVID-19 Update Brief; 9 June 2020. Report No.: 99; Ministry of Health/Directorate-General of Health: Lisbon, Portugal, 2020. [Google Scholar]
- Directorate-General of Health. COVID-19 Update Brief; 19 May 2020. Report No.: 78; Ministry of Health/Directorate-General of Health: Lisbon, Portugal, 2020. [Google Scholar]
- Directorate-General of Health. COVID-19 Update Brief; 21 July 2020. Report No.: 141; Ministry of Health/Directorate-General of Health: Lisbon, Portugal, 2020. [Google Scholar]
- Directorate-General of Health. COVID-19 Update Brief; 29 June 2020. Report No.: 119; Ministry of Health/Directorate-General of Health: Lisbon, Portugal, 2020. [Google Scholar]
- Tello, J.E.; Pardo-Hernandez, H.; Rodrigues, R.; Ilinca, S.; Leichsenring, K.; Aguirre, I.Y.; Huber, M.; Barbazza, E. A services delivery perspective to the provision of long-term care in Portugal. Public Policy Port. J. 2020, 5, 8–27. [Google Scholar]
- Barbazza, E.; Klazinga, N.; Kringos, D. Exploring the actionability of healthcare performance indicators for quality of care: A qualitative analysis of the literature, expert opinion and user experience. BMJ Qual. Saf. 2021. [Google Scholar] [CrossRef]
- Kringos, D.; Carinci, F.; Barbazza, E.; Bos, V.; Gilmore, K.; Groene, O.; Gulácsi, L.; Ivanković, D.; Jansen, T.; Johnsen, S.P.; et al. Managing COVID-19 within and across health systems: Why we need performance intelligence to coordinate a global response. Health Res. Policy Syst. 2020, 18, 80. [Google Scholar] [CrossRef]
- Ivanković, D.; Barbazza, E.; Bos, V.; Brito Fernandes, Ó.; Jamieson Gilmore, K.; Jansen, T.; Kara, P.; Larrain, N.; Lu, S.; Meza-Torres, B.; et al. Features constituting actionable COVID-19 dashboards: Descriptive assessment and expert appraisal of 158 public web-based COVID-19 dashboards. J. Med. Internet Res. 2021, 23, e25682. [Google Scholar] [CrossRef] [PubMed]
- Campos, A. Lar de Reguengos Continua com Falhas dois Meses Após as Mortes. Público. 3 September 2020. Available online: https://www.publico.pt/2020/09/03/sociedade/noticia/lar-reguengos-continua-falhas-dois-meses-apos-mortes-1930203 (accessed on 20 July 2021).
- Rada, A.G. Covid-19: The precarious position of Spain’s nursing homes. BMJ 2020, 369, m1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shang, J.; Chastain, A.M.; Perera, U.G.E.; Quigley, D.D.; Fu, C.J.; Dick, A.W.; Pogorzelska-Maziarz, M.; Stone, P.W. COVID-19 preparedness in US home health care agencies. J. Am. Med. Dir. Assoc. 2020, 21, 924–927. [Google Scholar] [CrossRef]
- Siu, H.Y.; Kristof, L.; Elston, D.; Hafid, A.; Mather, F. A cross-sectional survey assessing the preparedness of the long-term care sector to respond to the COVID-19 pandemic in Ontario, Canada. BMC Geriatr. 2020, 20, 421. [Google Scholar] [CrossRef]
- McGarry, B.E.; Grabowski, D.C.; Barnett, M.L. Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID-19 pandemic. Health Aff. 2020, 39, 1812–1821. [Google Scholar] [CrossRef] [PubMed]
- Lusa. Covid-19: Linha Covid Lares Apoiou Mais de 700 Instituições e Evitou Centenas de Surtos. Visão Saúde. 20 March 2021. Available online: https://visao.sapo.pt/visaosaude/2021-03-20-covid-19-linha-covid-lares-apoiou-mais-de-700-instituicoes-e-evitou-centenas-de-surtos (accessed on 20 July 2021).
- Ministry of Labour, Solidarity and Social Security. Formação de Gestão de Surtos em Lares Arranca em todo o País. 2020. Available online: https://www.portugal.gov.pt/download-ficheiros/ficheiro.aspx?v=%3D%3DBQAAAB%2BLCAAAAAAABAAzNDQwMgYAGCk%2FZAUAAAA%3D (accessed on 20 July 2021).
- Lusa. COVID-19. Quase Metade das Mortes em Lares Desde o Início da Pandemia Aconteceu este ano. Expresso. 8 February 2021. Available online: https://expresso.pt/coronavirus/2021-02-08-Covid-19.-Quase-metade-das-mortes-em-lares-desde-o-inicio-da-pandemia-aconteceu-este-ano (accessed on 20 July 2021).
- Langins, M.; Curry, N.; Lorenz-Dant, K.; Comas-Herrera, A.; Rajan, S. The COVID-19 pandemic and long-term care: What can we learn from the first wave about how to protect care homes? Eurohealth 2020, 26, 77–82. [Google Scholar]
- Ministry of Labour, Solidarity and Social Security. Programa MAREESS Prorrogado até Final de 2021. 2021. Available online: https://www.portugal.gov.pt/download-ficheiros/ficheiro.aspx?v=%3D%3DBQAAAB%2BLCAAAAAAABAAzNDSxMAcAV620ngUAAAA%3D (accessed on 20 July 2021).
- Miller, V.J.; Fields, N.L.; Anderson, K.A.; Kusmaul, N.; Maxwell, C. Nursing home social workers perceptions of preparedness and coping for COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020. [Google Scholar] [CrossRef]
- Senczyszyn, A.; Lion, K.M.; Szczesniak, D.; Trypka, E.; Mazurek, J.; Ciulkowicz, M.; Maćkowiak, M.; Duda-Sikuła, M.; Wallner, R.; Rymaszewska, J. Mental health impact of SARS-COV-2 pandemic on long-term care facility staff in Poland. J. Am. Med. Dir. Assoc. 2020, 21, 1576–1577. [Google Scholar] [CrossRef]
- Shallcross, L.; Burke, D.; Abbott, O.; Donaldson, A.; Hallatt, G.; Hayward, P.A.; Hopkins, S.; Krutikov, M.; Sharp, K.; Wardman, L.; et al. Factors associated with SARS-CoV-2 infection and outbreaks in long-term care facilities in England: A national cross-sectional survey. Lancet Healthy Longev. 2021, 2, e129–e142. [Google Scholar] [CrossRef]
- Embregts, P.; van Oorsouw, W.; Nijs, S. Impact of infection outbreak on long-term care staff: A rapid review on psychological well-being. J. Long Term Care 2020, 70–79. [Google Scholar] [CrossRef]
- Mo, S.; Shi, J. The psychological consequences of the COVID-19 on residents and staff in nursing homes. Work Aging Retire. 2020, 6, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Institute for Healthcare Improvement. “Psychological PPE”: Promote Health Care Workforce Mental Health and Well-Being. 2020. Available online: http://www.ihi.org/resources/Pages/Tools/psychological-PPE-promote-health-care-workforce-mental-health-and-well-being.aspx (accessed on 20 July 2021).
- Castle, N.G.; Wagner, L.M.; Ferguson, J.C.; Handler, S.M. Safety culture of nursing homes: Opinions of top managers. Health Care Manage. Rev. 2011, 36, 175–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desmedt, M.; Petrovic, M.; Beuckelaere, P.; Vandijck, D. Assessing resident safety culture in six nursing homes in Belgium. J. Patient Saf. 2018. [Google Scholar] [CrossRef] [PubMed]
- Ree, E.; Wiig, S. Employees’ perceptions of patient safety culture in Norwegian nursing homes and home care services. BMC Health Serv. Res. 2019, 19, 607. [Google Scholar] [CrossRef] [PubMed]
- Temkin-Greener, H.; Cen, X.; Li, Y. Nursing home staff turnover and perceived patient safety culture: Results from a national survey. Gerontologist 2020, 60, 1303–1311. [Google Scholar] [CrossRef] [PubMed]


| Item Grouping | COVID-19 Preparedness Compliance (%) a | ||
|---|---|---|---|
| Algarve (n = 51) | Alentejo (n = 87) | Total (n = 138) | |
| Structure for planning and decision-making | 65% | 79% | 74% |
| COVID-19 contingency plan | 75% | 87% | 83% |
| Elements of a COVID-19 Contingency Plan | |||
| General | 66% | 72% | 70% |
| Outbreak capacity | 35% | 45% | 41% |
| Communication | 79% | 76% | 77% |
| Supplies and resources | 68% | 79% | 75% |
| Education and training | 44% | 43% | 43% |
| Occupational health | 71% | 75% | 74% |
| Identification and management of ill residents | 87% | 81% | 83% |
| Access control | 83% | 81% | 82% |
| Total | Missing Data a | ||||
|---|---|---|---|---|---|
| N = 720 | |||||
| n | % | n | % | ||
| Individual | Sex | ||||
| Female | 667 | 93 | 7 | 1 | |
| Male | 46 | 6 | |||
| Age | |||||
| Mean (SD b) | 45 (11) | 3 | 0.4 | ||
| Education c | |||||
| Primary | 297 | 41 | 12 | 1.7 | |
| Secondary | 199 | 28 | |||
| Tertiary | 212 | 29 | |||
| Self-perceived health status | |||||
| Very good | 104 | 14 | 0 | 0 | |
| Good | 365 | 51 | |||
| Fair | 241 | 33 | |||
| Bad or Very bad | 10 | 1 | |||
| WHO Well-Being Index | |||||
| Mean (SD) | 15.5 (5.5) | 0 | 0 | ||
| Longstanding health problem | |||||
| Yes | 158 | 22 | 72 | 10 | |
| Household | Living with people aged 65 and over | ||||
| Yes | 147 | 20 | 8 | 1.1 | |
| Living with children (up to 12 years old) | |||||
| Yes | 255 | 35 | 2 | 0.3 | |
| Living with people in a professional group with increased risk | |||||
| Yes | 161 | 22 | 5 | 0.7 | |
| Work | Works directly with residents | ||||
| Yes | 525 | 73 | 0 | 0 | |
| Work contract duration | |||||
| Less than a year | 100 | 14 | 0 | 0 | |
| 1 to 2 years | 94 | 13 | |||
| 3 to 5 years | 127 | 18 | |||
| More than 5 years | 399 | 55 | |||
| Weekly working hours | |||||
| Less than 20 h | 52 | 7 | 0 | 0 | |
| 21 h up to 31 h | 19 | 3 | |||
| More than 31 h | 649 | 90 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brito Fernandes, Ó.; Lobo Julião, P.; Klazinga, N.; Kringos, D.; Marques, N. COVID-19 Preparedness and Perceived Safety in Nursing Homes in Southern Portugal: A Cross-Sectional Survey-Based Study in the Initial Phases of the Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 7983. https://doi.org/10.3390/ijerph18157983
Brito Fernandes Ó, Lobo Julião P, Klazinga N, Kringos D, Marques N. COVID-19 Preparedness and Perceived Safety in Nursing Homes in Southern Portugal: A Cross-Sectional Survey-Based Study in the Initial Phases of the Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(15):7983. https://doi.org/10.3390/ijerph18157983
Chicago/Turabian StyleBrito Fernandes, Óscar, Pedro Lobo Julião, Niek Klazinga, Dionne Kringos, and Nuno Marques. 2021. "COVID-19 Preparedness and Perceived Safety in Nursing Homes in Southern Portugal: A Cross-Sectional Survey-Based Study in the Initial Phases of the Pandemic" International Journal of Environmental Research and Public Health 18, no. 15: 7983. https://doi.org/10.3390/ijerph18157983
APA StyleBrito Fernandes, Ó., Lobo Julião, P., Klazinga, N., Kringos, D., & Marques, N. (2021). COVID-19 Preparedness and Perceived Safety in Nursing Homes in Southern Portugal: A Cross-Sectional Survey-Based Study in the Initial Phases of the Pandemic. International Journal of Environmental Research and Public Health, 18(15), 7983. https://doi.org/10.3390/ijerph18157983






