Association of Vital Pulp Therapy Outcomes with Tooth Type, Arch Location, Treatment Type, and Number of Surfaces Destroyed in Deciduous Teeth: A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Study Sample
2.2. Consent for Using Patient Data
2.3. Data Extraction
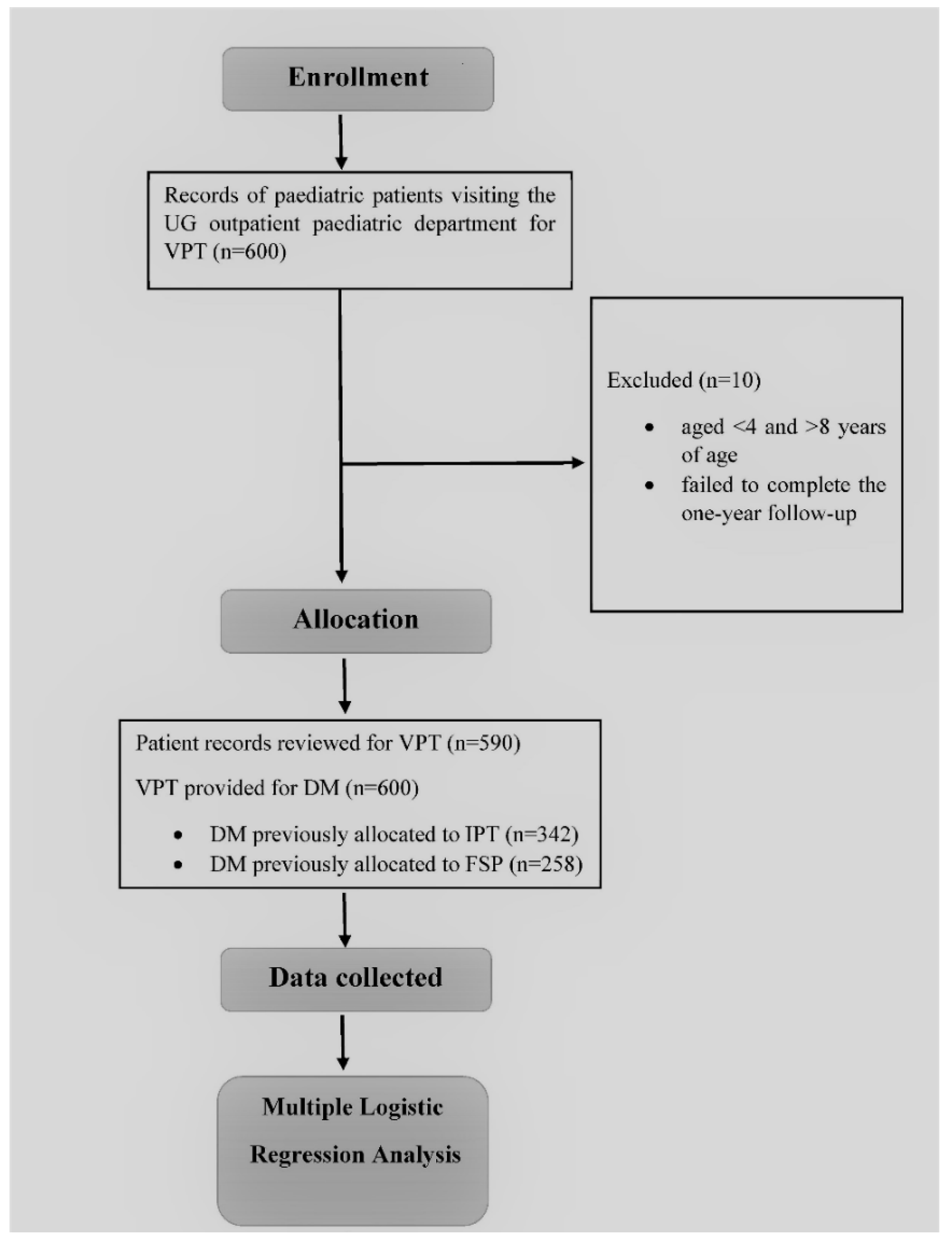
2.4. Patient Recruitment/Allocation
2.5. Inclusion/Exclusion Criteria
2.6. Operational Definitions
- Successful treatment—a treatment outcome was labeled as successful when there were no clinical signs of tenderness to percussion, normal tooth mobility, no sinus tract or abscess formation around the treated tooth, and no symptoms of spontaneous/nocturnal pain within a year (follow-up after 1 week, 3 months, 6 months, and 12 months) [16].
- Failed treatment—a treatment outcome was labeled as failed when any one of the following clinical or radiographic signs of failure were present, such as tenderness on percussion, abnormal tooth mobility according to Miller’s classification [17], presence of sinus tract or an abscess around the treated tooth, along with radiographic evidence of PDL widening, radiolucencies, or symptoms of spontaneous/nocturnal pain within a year (follow-up after 1 week, 3 months, 6 months, and 12 months) [16].
2.7. Procedure
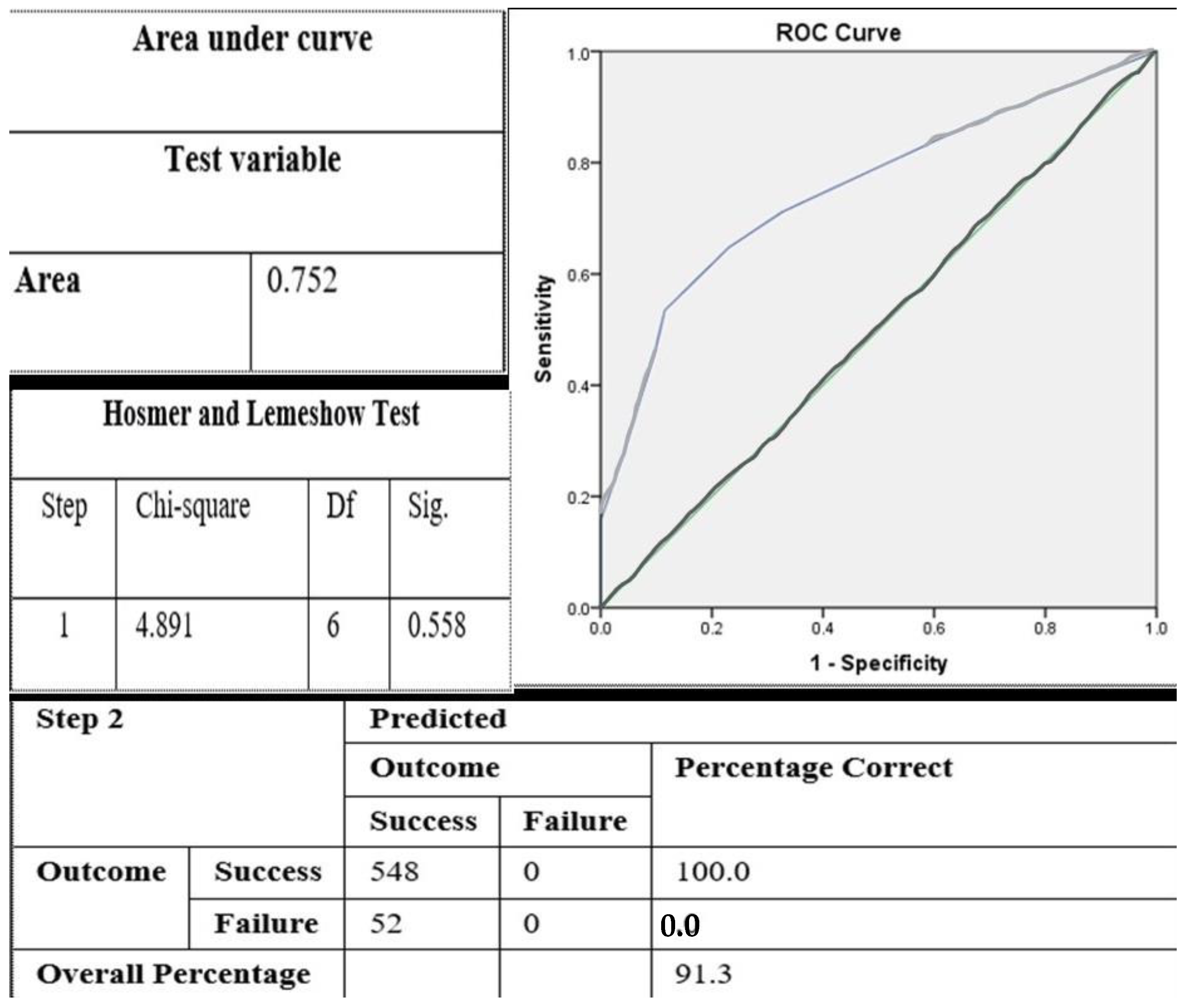
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parisay, I.; Ghoddusi, J.; Forghani, M. A review on vital pulp therapy in primary teeth. Iran. Endod. J. 2015, 10, 6–15. [Google Scholar]
- Fuks, A.B.; Kupietzky, A.; Guelmann, M. Pulp therapy for the primary dentition. In Pediatric Dentistry; Elsevier: Amsterdam, The Netherlands, 2019; pp. 329–351.e1. [Google Scholar]
- Al-Zayer, M.A.; Straffon, L.H.; Feigal, R.J.; Welch, K.B. Indirect pulp treatment of primary posterior teeth: A retrospective study. Pediatr. Dent. 2003, 25, 29–36. [Google Scholar]
- Dammaschke, T.; Leidinger, J.; Schäfer, E. Long-term evaluation of direct pulp capping—Treatment outcomes over an average period of 6.1 years. Clin. Oral Investig. 2010, 14, 559–567. [Google Scholar] [CrossRef]
- Karobari, M.I.; Maqbool, M.; Ahmad, P.; Abdul, M.S.M.; Marya, A.; Venugopal, A.; Shaik, G.M.; Scardina, G.A.; Messina, P.; Noorani, T.Y. Endodontic Microbiology: A Bibliometric Analysis of the Top 50 Classics. BioMed Res. Int. 2021, 2021, 6657167. [Google Scholar] [CrossRef]
- Vij, R.; Coll, J.A.; Shelton, P.; Farooq, N.S. Caries control and other variables associated with success of primary molar vital pulp therapy. Pediatr. Dent. 2004, 26, 214–220. [Google Scholar] [PubMed]
- Coll, J.A. Indirect pulp capping and primary teeth: Is the primary tooth pulpotomy out of date? Pediatr. Dent. 2008, 30, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Ye, L.; Guo, X.; Tan, H.; Zhou, X.; Wang, C.; Li, R. Evaluation of formocresol versus ferric sulphate primary molar pulpotomy: A systematic review and meta-analysis. Int. Endod. J. 2007, 40, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Fang, R.-R.; Chang, K.Y.; Lin, Y.T.; Lin, Y.T.J. Comparison of long-term outcomes between ferric sulfate pulpotomy and indirect pulp therapy in primary molars. J. Dent. Sci. 2019, 14, 134–137. [Google Scholar] [CrossRef]
- Mathur, V.P.; Dhillon, J.; Logani, A.; Kalra, G. Evaluation of indirect pulp capping using three different materials: A randomized control trial using cone-beam computed tomography. Indian J. Dent. Res. 2016, 27, 623–629. [Google Scholar] [CrossRef]
- Casagrande, L.; Westphalen Bento, L.; Martini Dalpian, D.; García-Godoy, F.; Borba de Araújo, F. Indirect pulp treatment in primary teeth: 4-year results. Am. J. Dent. 2010, 23, 34–38. [Google Scholar]
- Havale, R.; Anegundi, R.T.; Indushekar, K.R.; Sudha, P. Clinical and radiographic evaluation of pulpotomies in primary molars with formocresol, glutaraldehyde and ferric sulphate. Oral Health Dent Manag. 2013, 12, 24–31. [Google Scholar] [PubMed]
- Lin, Y.-T.; Lin, Y.-T.J. Survey of comprehensive restorative treatment for children under general anesthesia. J. Dent. Sci. 2015, 10, 296–299. [Google Scholar] [CrossRef] [Green Version]
- Capparè, P.; Tetè, G.; Sberna, M.T.; Panina-Bordignon, P. The emerging role of stem cells in regenerative dentistry. Curr. Gene Ther. 2020, 20, 259–268. [Google Scholar] [CrossRef]
- Young, D.A.; Nový, B.B.; Zeller, G.G.; Hale, R.; Hart, T.C.; Truelove, E.L. The American Dental Association caries classification system for clinical practice: A report of the American dental association council on scientific affairs. J. Am. Dent. Assoc. 2015, 146, 79–86. [Google Scholar] [CrossRef]
- Kvist, T. Endodontic retreatment. Aspects of decision making and clinical outcome. Swed. Dent. Journal. Suppl. 2001, 144, 1–57. [Google Scholar]
- Laster, L.; Laudenbach, K.W.; Stoller, N.H. An evaluation of clinical tooth mobility measurements. J. Periodontol. 1975, 46, 603–607. [Google Scholar] [CrossRef] [Green Version]
- Tronstad, L.; Asbjørnsen, K.; Døving, L.; Pedersen, I.; Eriksen, H.M. Influence of coronal restorations on the periapical health of endodontically treated teeth. Dent. Traumatol. 2000, 16, 218–221. [Google Scholar] [CrossRef]
- Dalpian, D.M.; Ardenghi, T.M.; Demarco, F.F.; Garcia-Godoy, F.; De Araujo, F.B.; Casagrande, L. Clinical and radiographic outcomes of partial caries removal restorations performed in primary teeth. Am. J. Dent. 2014, 27, 68–72. [Google Scholar]
- Garrocho-Rangel, A.; Quintana-Guevara, K.; Vázquez-Viera, R.; Arvizu-Rivera, J.M.; Flores-Reyes, H.; Escobar-García, D.M.; Pozos-Guillén, A. Bioactive tricalcium silicate-based dentin substitute as an indirect pulp capping material for primary teeth: A 12-month follow-up. Pediatr. Dent. 2017, 39, 377–382. [Google Scholar] [PubMed]
- Wang, Y.-L.; Chang, H.H.; Kuo, C.I.; Chen, S.K.; Guo, M.K.; Huang, G.F.; Lin, C.P. A study on the root canal morphology of primary molars by high-resolution computed tomography. J. Dent. Sci. 2013, 8, 321–327. [Google Scholar] [CrossRef] [Green Version]
- Junqueira, M.A.; Cunha, N.N.O.; Caixeta, F.F.; Marques, N.C.T.; Oliveira, T.M.; Moretti, A.B.D.S.; Cosme-Silva, L.; Sakai, V.T. Clinical, radiographic and histological evaluation of primary teeth Pulpotomy using MTA and ferric sulfate. Braz. Dent. J. 2018, 29, 159–165. [Google Scholar] [CrossRef]
- Wunsch, P.B.; Kuhnen, M.M.; Best, A.M.; Brickhouse, T.H. Retrospective study of the survival rates of indirect pulp therapy versus different pulpotomy medicaments. Pediatr. Dent. 2016, 38, 406–411. [Google Scholar] [PubMed]
- Casagrande, L.; Bento, L.W.; Rerin, S.O.; Resende Lucas, E.D.; Dalpian, D.M.; de Araujo, F.B. In vivo outcomes of indirect pulp treatment using a self-etching primer versus calcium hydroxide over the demineralized dentin in primary molars. J. Clin. Pediatr. Dent. 2008, 33, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, L.; Atar, M.; Daronch, M.; Honig, A.; Chey, M.; Funny, M.D.; Cruz, L. Observational: Prospective study of indirect pulp treatment in primary molars using resin-modified glass ionomer and 2% chlorhexidine gluconate: A 12-month follow-up. Pediatr. Dent. 2013, 35, 13–17. [Google Scholar]
- Chauhan, A.; Dua, P.; Saini, S.; Mangla, R.; Butail, A.; Ahluwalia, S. In vivo outcomes of indirect pulp treatment in primary posterior teeth: 6 months’ follow-up. Contemp. Clin. Dent. 2018, 9, S69–S73. [Google Scholar] [CrossRef] [PubMed]
- Boddeda, K.R.; Rani, C.R.; Vanga, N.R.V.; Chandrabhatla, S.K. Comparative evaluation of Biodentine, 2% chlorhexidine with RMGIC and calcium hydroxide as indirect pulp capping materials in primary molars: An in vivo study. J. Indian Soc. Pedod. Prev. Dent. 2019, 37, 60–66. [Google Scholar] [CrossRef]
- Smith, N.L.; Seale, N.S.; Nunn, M.E. Ferric sulfate pulpotomy in primary molars: A retrospective study. Pediatr. Dent. 2000, 22, 192–199. [Google Scholar] [PubMed]
- Farooq, N.S.; Coll, J.A.; Kuwabara, A.; Shelton, P. Success rates of formocresol pulpotomy and indirect pulp therapy in the treatment of deep dentinal caries in primary teeth. Pediatr. Dent. 2000, 22, 278–286. [Google Scholar] [PubMed]
- Papagiannoulis, L. Clinical studies on ferric sulphate as a pulpotomy medicament in primary teeth. Eur. J. Paediatr. Dent. 2002, 3, 126–132. [Google Scholar]
- Maqbool, M.; Noorani, T.Y.; Asif, J.A.; Makandar, S.D.; Jamayet, N.B. Controversies in endodontic access cavity design: A literature review. Dent. Update 2020, 47, 747–754. [Google Scholar] [CrossRef]
- Huth, K.C.; Paschos, E.; Hajek-Al-Khatar, N.; Hollweck, R.; Crispin, A.; Hickel, R.; Folwaczny, M. Effectiveness of 4 pulpotomy techniques—randomized controlled trial. J. Dent. Res. 2005, 84, 1144–1148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aps, J. Cone beam computed tomography in paediatric dentistry: Overview of recent literature. Eur. Arch. Paediatr. Dent. 2013, 14, 131–140. [Google Scholar] [CrossRef] [PubMed]

| Based on Sex and Age | |||
|---|---|---|---|
| Frequency | Percentage (%) | ||
| Gender | |||
| Male | 350 | 59.3 | |
| Female | 240 | 40.7 | |
| Total | 590 | 100.0 | |
| Age | |||
| Mean (SD) | 6.54 (1.18) | ||
| Based on Deciduous Molar Type | |||
| Treatment Outcome | S (%) | F (%) | Total |
| 1st Deciduous Molar | 237 (85.3) | 41 (14.7) | 278 |
| 2nd Deciduous Molar | 311 (96.6) | 11 (3.4) | 322 |
| Based on Arch Type | |||
| Treatment Outcome | S (%) | F (%) | Total |
| Maxillary Arch | 226 (96.6) | 8 (3.4) | 234 |
| Mandibular Arch | 322 (88.0) | 44 (12.0) | 366 |
| Based on treatment type | |||
| Treatment Outcome | S (%) | F (%) | Total |
| Type of VPT | |||
| IPT | 320 (93.6) | 22 (6.4) | 342 |
| FSP | 228 (88.4) | 30 (11.6) | 258 |
| Final VPT Outcome | 548 (91.3) | 52 (8.6) | 600 |
| Based on Number of Surfaces Involved | |||
| Treatment Outcome | S (%) | F (%) | Total |
| One surface involved | 331 (91.2) | 32 (8.8) | 363 |
| Multiple surfaces involved | 217 (91.6) | 20 (8.4) | 237 |
| B | S.E. | Wald | p-Value | OR | |
|---|---|---|---|---|---|
| Type of Deciduous Molar (2nd D.M. as an indicator) | 1.587 | 0.353 | 20.534 | <0.0001 * | 4.89 (2.46–9.72) |
| Arch Type (Maxillary as indicator) | 1.352 | 0.348 | 11.752 | 0.001 * | 3.86 (1.78–8.36) |
| Treatment Type (IPT as indicator) | 0.652 | 0.294 | 4.881 | 0.027 * | 1.91 (1.08–3.40) |
| Surfaces Involved (One surface as indicator) | 0.048 | 0.298 | 0.026 | 0.873 | 0.95 (0.53–1.71) |
| Variables | B | S.E. | Wald | Crude OR | p-Value | Adjusted OR | p-Value |
|---|---|---|---|---|---|---|---|
| Type of Deciduous Molar (Second DM) | 1.434 | 0.355 | 16.331 | 4.89 (2.46, 9.72) | <0.001 * | 4.19 (2.09, 8.41) | <0.001 * |
| Arch Type (Maxillary) | 1.183 | 0.401 | 8.702 | 3.86 (1.78, 8.35) | 0.001 * | 3.27 (1.49, 7.17) | 0.003 * |
| Type of Tx (IPT) | 0.634 | 0.303 | 4.379 | 1.91 (1.08, 3.40) | 0.027 * | 1.89 (1.04, 3.42) | 0.036 * |
| Follow-Up Period | 1 Week | 3 Months | 6 Months | 12 Months | |
|---|---|---|---|---|---|
| Cause of Failure/Total (n) | IPT/FSP | IPT/FSP | IPT/FSP | IPT/FSP | |
| Nocturnal pain | 27 | 16/9 | 0/2 | - | - |
| Grade II/III Mobility | 10 | - | 1/9 | - | - |
| Sinus tract | 5 | - | 2/3 | - | - |
| Abscess | 10 | 1/2 | 2/5 | - | - |
| Total | 52 | 17/11 | 5/19 | ||
| 28 | 24 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maqbool, M.; Noorani, T.Y.; Samsudin, N.A.; Awang Nawi, M.A.; Rossi-Fedele, G.; Karobari, M.I.; Messina, P.; Scardina, G.A. Association of Vital Pulp Therapy Outcomes with Tooth Type, Arch Location, Treatment Type, and Number of Surfaces Destroyed in Deciduous Teeth: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 7970. https://doi.org/10.3390/ijerph18157970
Maqbool M, Noorani TY, Samsudin NA, Awang Nawi MA, Rossi-Fedele G, Karobari MI, Messina P, Scardina GA. Association of Vital Pulp Therapy Outcomes with Tooth Type, Arch Location, Treatment Type, and Number of Surfaces Destroyed in Deciduous Teeth: A Retrospective Study. International Journal of Environmental Research and Public Health. 2021; 18(15):7970. https://doi.org/10.3390/ijerph18157970
Chicago/Turabian StyleMaqbool, Manahil, Tahir Yusuf Noorani, Norsamsu Arni Samsudin, Mohamad Arif Awang Nawi, Giampiero Rossi-Fedele, Mohmed Isaqali Karobari, Pietro Messina, and Giuseppe Alessandro Scardina. 2021. "Association of Vital Pulp Therapy Outcomes with Tooth Type, Arch Location, Treatment Type, and Number of Surfaces Destroyed in Deciduous Teeth: A Retrospective Study" International Journal of Environmental Research and Public Health 18, no. 15: 7970. https://doi.org/10.3390/ijerph18157970
APA StyleMaqbool, M., Noorani, T. Y., Samsudin, N. A., Awang Nawi, M. A., Rossi-Fedele, G., Karobari, M. I., Messina, P., & Scardina, G. A. (2021). Association of Vital Pulp Therapy Outcomes with Tooth Type, Arch Location, Treatment Type, and Number of Surfaces Destroyed in Deciduous Teeth: A Retrospective Study. International Journal of Environmental Research and Public Health, 18(15), 7970. https://doi.org/10.3390/ijerph18157970








