Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measurement
Definition of Hypertension
2.3. Assessment of Sleep Factors and Definition of a Sleep Pattern
2.4. Other Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Participants
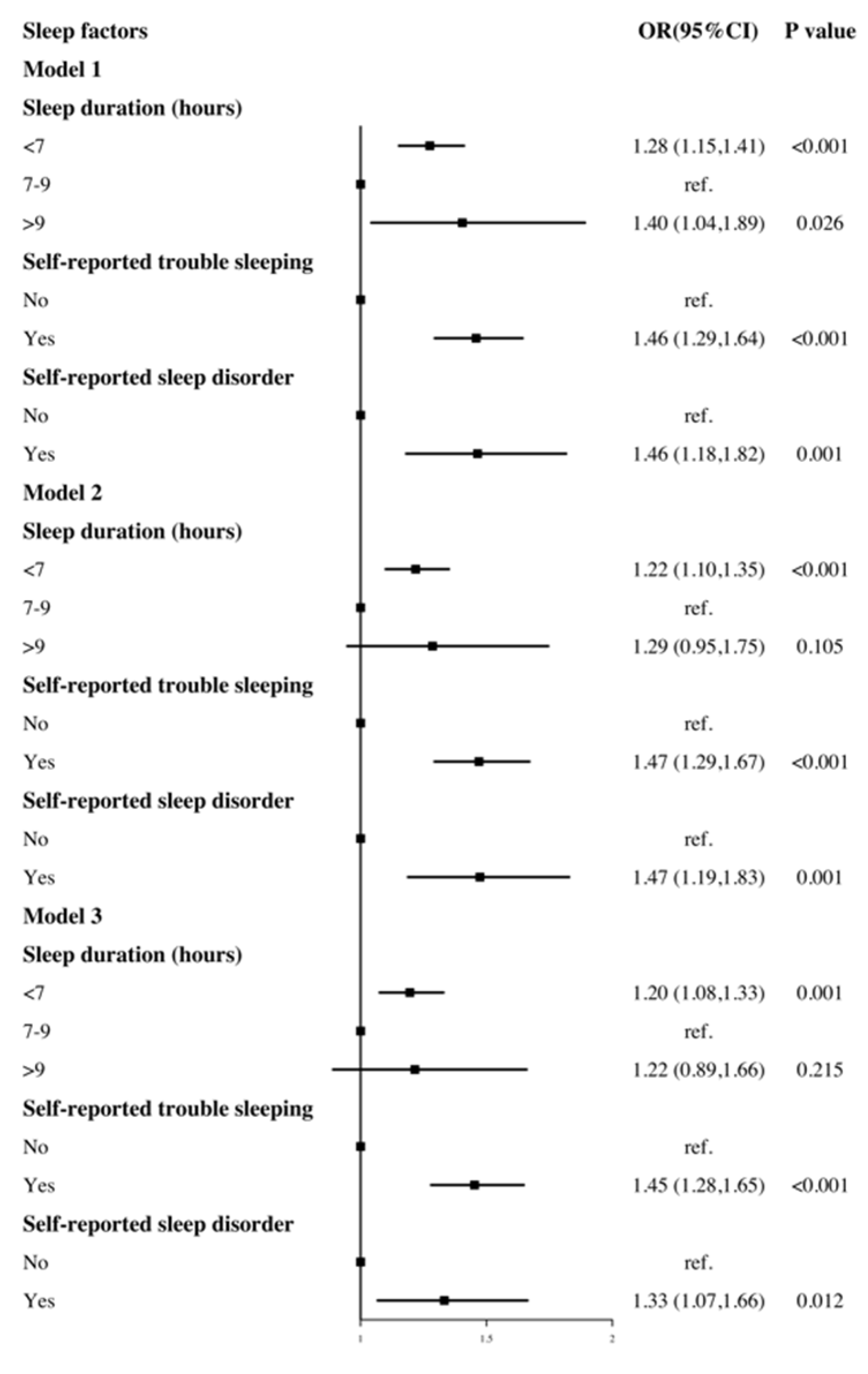
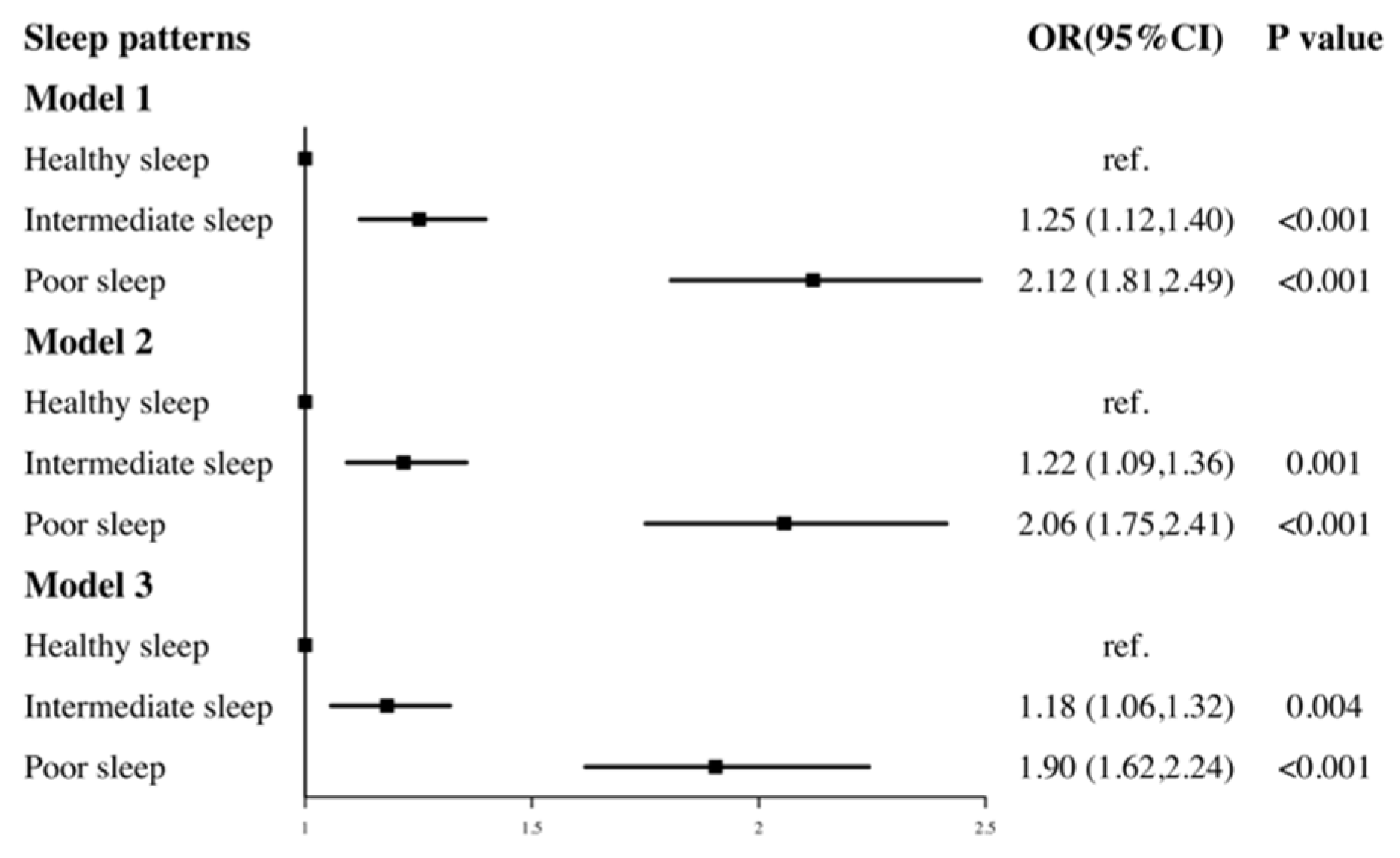
3.2. Associations of Sleep with Risk of Hypertension
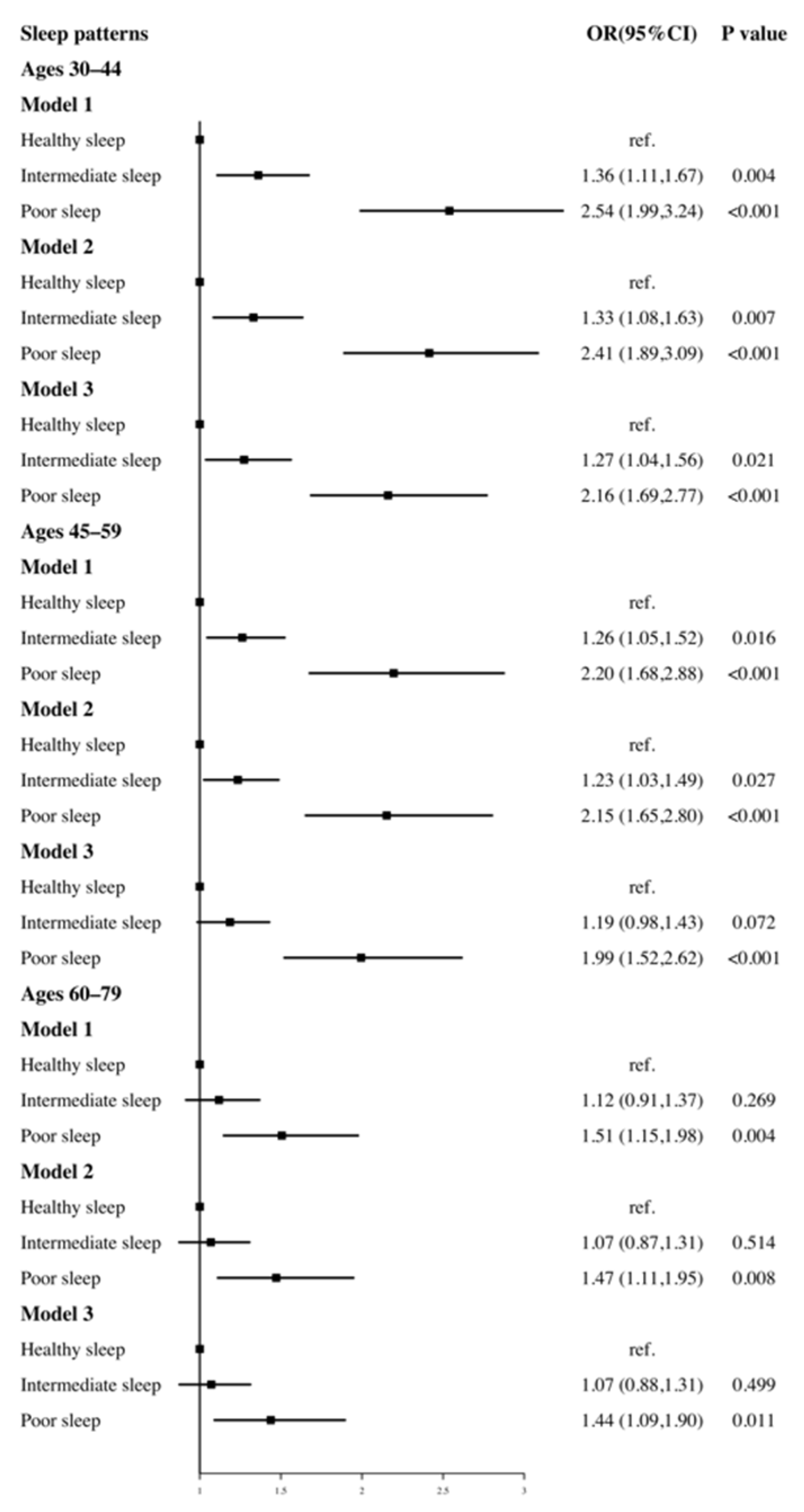
3.3. Associations of Sleep with Risk of Hypertension after Age Stratification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- Hertenstein, E.; Gabryelska, A.; Spiegelhalder, K.; Nissen, C.; Johann, A.F.; Umarova, R. Reference Data for Polysomnography-Measured and Subjective Sleep in Healthy Adults. J. Clin. Sleep Med. 2018, 14, 523–532. [Google Scholar] [CrossRef]
- Chaput, J.P.; Dutil, C.; Sampasa-Kanyinga, H. Sleeping hours: What is the ideal number and how does age impact this? Nat. Sci. Sleep 2018, 10, 421. [Google Scholar] [CrossRef]
- Guo, X.; Zheng, L.; Wang, J.; Zhang, X.; Zhang, X.; Li, J. Epidemiological evidence for the link between sleep duration and high blood pressure: A systematic review and meta-analysis. Sleep Med. 2013, 14, 324–332. [Google Scholar] [CrossRef]
- Wang, Y.; Mei, H.; Jiang, Y.R.; Sun, W.Q.; Song, Y.J.; Liu, S.J. Relationship between Duration of Sleep and Hypertension in Adults: A Meta-Analysis. J. Clin. Sleep Med. 2015, 11, 1047–1056. [Google Scholar] [CrossRef]
- Grandner, M.; Mullington, J.M.; Hashmi, S.D.; Redeker, N.S.; Watson, N.F.; Morgenthaler, T.I. Sleep Duration and Hypertension: Analysis of >700,000 Adults by Age and Sex. J. Clin. Sleep Med. 2018, 14, 1031–1039. [Google Scholar] [CrossRef] [PubMed]
- Pepin, J.L.; Borel, A.L.; Tamisier, R.; Baguet, J.P.; Levy, P.; Dauvilliers, Y. Hypertension and sleep: Overview of a tight relationship. Sleep Med. Rev. 2014, 18, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Liu, Q.; Li, Y.; Zhao, F.; Chang, H.; Lyu, J. Longitudinal study of the relationship between sleep duration and hypertension in Chinese adult residents (CHNS 2004–2011). Sleep Med. 2019, 58, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhao, X.; Li, Y.; Mao, Z.; Huo, W.; Jiang, J. Night sleep duration and sleep initiation time with hypertension in Chinese rural population: The Henan Rural Cohort. Eur. J. Public Health 2020, 30, 164–170. [Google Scholar] [CrossRef]
- Jike, M.; Itani, O.; Watanabe, N.; Buysse, D.J.; Kaneita, Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 2018, 39, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Palta, M.; Skatrud, J. Prospective study of the association between sleep-disordered breathing and hypertension. N. Engl. J. Med. 2000, 342, 1378–1384. [Google Scholar] [CrossRef]
- Marin, J.M.; Agusti, A.; Villar, I.; Forner, M.; Nieto, D.; Carrizo, S.J. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA 2012, 307, 2169–2176. [Google Scholar] [CrossRef]
- Fan, M.; Sun, D.; Zhou, T.; Heianza, Y.; Lv, J.; Li, L. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: A prospective study of 385 292 UK biobank participants. Eur. Heart J. 2020, 41, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xue, Q.; Wang, M.; Zhou, T.; Ma, H.; Heianza, Y. Adherence to a Healthy Sleep Pattern and Incident Heart Failure: A Prospective Study of 408 802 UK Biobank Participants. Circulation 2021, 143, 97–99. [Google Scholar] [CrossRef]
- Fernandez-Mendoza, J.; Vgontzas, A.N.; Liao, D.; Shaffer, M.L.; Vela-Bueno, A.; Basta, M. Insomnia with objective short sleep duration and incident hypertension: The Penn State Cohort. Hypertension 2012, 60, 929–935. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P.; Grandner, M.A.; Brown, D.; Conroy, M.B.; Jean-Louis, G.; Coons, M. Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e367–e386. [Google Scholar] [CrossRef]
- Bathgate, C.J.; Fernandez-Mendoza, J. Insomnia, Short Sleep Duration, and High Blood Pressure: Recent Evidence and Future Directions for the Prevention and Management of Hypertension. Curr. Hypertens. Rep. 2018, 20, 52. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L.J. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef]
- Rehm, C.D.; Penalvo, J.L.; Afshin, A.; Mozaffarian, D. Dietary Intake Among US Adults, 1999-2012. JAMA 2016, 315, 2542–2553. [Google Scholar] [CrossRef] [PubMed]
- Mellen, P.B.; Gao, S.K.; Vitolins, M.Z.; Goff, D.C.J. Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988–1994 and 1999–2004. Arch. Intern. Med. 2008, 168, 308–314. [Google Scholar] [CrossRef]
- Park, Y.M.; Steck, S.E.; Fung, T.T.; Zhang, J.; Hazlett, L.J.; Han, K. Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH) style diet, and metabolic health in U.S. adults. Clin. Nutr. 2017, 36, 1301–1309. [Google Scholar] [CrossRef]
- Mirel, L.B.; Mohadjer, L.K.; Dohrmann, S.M.; Clark, J.; Burt, V.L.; Johnson, C.L.; Curtin, L.R. National Health and Nutrition Examination Survey: Estimation procedures, 2007–2010. Vital Health Stat. 2. 2013, 159, 1–17. [Google Scholar]
- Chen, T.C.; Parker, J.D.; Clark, J.; Shin, H.C.; Rammon, J.R.; Burt, V.L. National Health and Nutrition Examination Survey: Estimation Procedures, 2011–2014. Vital Health Stat 2. 2018, 177, 1–26. [Google Scholar]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Hu, Y.; Wang, X.; Yang, S.; Chen, W.; Zeng, Z. The association between sleep duration and hypertension: A meta and study sequential analysis. J. Hum. Hypertens. 2021, 35, 621–626. [Google Scholar] [CrossRef]
- Li, H.; Ren, Y.; Wu, Y.; Zhao, X. Correlation between sleep duration and hypertension: A dose-response meta-analysis. J. Hum. Hypertens. 2019, 33, 218–228. [Google Scholar] [CrossRef] [PubMed]
- Gangwisch, J.E.; Heymsfield, S.B.; Boden-Albala, B.; Buijs, R.M.; Kreier, F.; Pickering, T.G. Short sleep duration as a risk factor for hypertension: Analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006, 47, 833–839. [Google Scholar] [CrossRef]
- Van Ryswyk, E.; Mukherjee, S.; Chai-Coetzer, C.L.; Vakulin, A.; McEvoy, R.D. Sleep Disorders, Including Sleep Apnea and Hypertension. Am. J. Hypertens. 2018, 31, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.J.; Calhoun, D. Sleep, insomnia, and hypertension: Current findings and future directions. J. Am. Soc. Hypertens. 2017, 11, 122–129. [Google Scholar] [CrossRef]
- Lo, K.; Woo, B.; Wong, M.; Tam, W. Subjective sleep quality, blood pressure, and hypertension: A meta-analysis. J. Clin. Hypertens. (Greenwich) 2018, 20, 592–605. [Google Scholar] [CrossRef]
- Meng, L.; Zheng, Y.; Hui, R. The relationship of sleep duration and insomnia to risk of hypertension incidence: A meta-analysis of prospective cohort studies. Hypertens. Res. 2013, 36, 985–995. [Google Scholar] [CrossRef]
- Tamisier, R.; Weiss, J.W.; Pepin, J.L. Sleep biology updates: Hemodynamic and autonomic control in sleep disorders. Metabolism 2018, 84, 3–10. [Google Scholar] [CrossRef]
- Yang, D.; Rundek, T.; Patel, S.R.; Cabral, D.; Redline, S.; Testai, F.D. Cerebral Hemodynamics in Sleep Apnea and Actigraphy-Determined Sleep Duration in a Sample of the Hispanic Community Health Study/ Study of Latinos. J. Clin. Sleep. Med. 2019, 15, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Chowdhuri, S.; Badr, M.S. Control of Ventilation in Health and Disease. Chest 2017, 151, 917–929. [Google Scholar] [CrossRef] [PubMed]
- Friedman, O.; Shukla, Y.; Logan, A.G. Relationship between self-reported sleep duration and changes in circadian blood pressure. Am. J. Hypertens. 2009, 22, 1205–1211. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Makarem, N.; Shechter, A.; Carnethon, M.R.; Mullington, J.M.; Hall, M.H.; Abdalla, M. Sleep Duration and Blood Pressure: Recent Advances and Future Directions. Curr. Hypertens. Rep. 2019, 21, 33. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovas, J.M. Short sleep duration and dietary intake: Epidemiologic evidence, mechanisms, and health implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Tasali, E.; Penev, P.; Cauter, E.V. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann. Intern. Med. 2004, 141, 846–850. [Google Scholar] [CrossRef]
- Gangwisch, J.E. A review of evidence for the link between sleep duration and hypertension. Am. J. Hypertens. 2014, 27, 1235–1242. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef]
- Cabeza de Baca, T.; Chayama, K.L.; Redline, S.; Slopen, N.; Matsushita, F.; Prather, A.A. Sleep debt: The impact of weekday sleep deprivation on cardiovascular health in older women. Sleep 2019, 42, zsz149. [Google Scholar] [CrossRef]
- Szmyd, B.; Rogut, M.; Bialasiewicz, P.; Gabryelska, A. The impact of glucocorticoids and statins on sleep quality. Sleep Med. Rev. 2021, 55, 101380. [Google Scholar] [CrossRef]
| Characteristics | Sleep Patterns (Col %) | |||
|---|---|---|---|---|
| Healthy (n = 5675) | Intermediate (n = 4539) | Poor (n = 1952) | p Value | |
| Demographics | ||||
| Age group (years) | 49.8 ± 13.6 | 49.5 ± 13.0 | 51.1 ± 12.6 | <0.001 |
| 30–44 | 2404 (42.4) | 1853 (40.8) | 663 (34.0) | |
| 45–59 | 1675 (29.5) | 1519 (33.5) | 749 (38.4) | |
| 60–79 | 1596 (28.1) | 1167 (25.7) | 540 (27.7) | |
| Gender | <0.001 | |||
| Male | 2743 (48.3) | 2217 (48.8) | 796 (40.8) | |
| Female | 2932 (51.7) | 2322 (51.2) | 1156 (59.2) | |
| Race | <0.001 | |||
| Non-white a | 3117 (54.9) | 2659 (58.6) | 928 (47.5) | |
| White | 2558 (45.1) | 1880 (41.4) | 1024 (52.5) | |
| Marriage status | <0.001 | |||
| Married/Living with partner | 3992 (70.3) | 2932 (64.6) | 1105 (56.6) | |
| Widowed/Divorced/ Separated/Never married | 1683 (29.7) | 1607 (35.4) | 847 (43.4) | |
| Education level | 0.543 | |||
| ≤High school | 2588 (45.6) | 2119 (46.7) | 895 (45.9) | |
| >High school | 3087 (54.4) | 2420 (53.3) | 1057 (54.1) | |
| Health insurance | <0.001 | |||
| No | 1518 (26.7) | 1093 (24.1) | 353 (18.1) | |
| Yes | 4157 (73.3) | 3446 (75.9) | 1599 (81.9) | |
| Clinical status | ||||
| BMI (kg/m2) | <0.001 | |||
| <25 | 1745 (30.7) | 1283 (28.3) | 446 (22.8) | |
| ≥25 | 3930 (69.3) | 3256 (71.7) | 1506 (77.2) | |
| Health behaviors | ||||
| DASH index | 0.007 | |||
| 0–3.5 | 4270 (75.2) | 3533 (77.9) | 1507 (77.2) | |
| 4–7.5 | 1405 (24.8) | 1006 (22.2) | 445 (22.8) | |
| Smoking status b | <0.001 | |||
| No | 3388 (59.7) | 2427 (53.5) | 929 (47.6) | |
| Yes | 2287 (40.3) | 2112 (46.5) | 1023 (52.4) | |
| Alcohol intake (gm/day) | 0.015 | |||
| 0–24.9 | 4815 (84.8) | 3839 (84.6) | 1703 (87.2) | |
| 25.1–550.1 | 860 (15.2) | 700 (15.4) | 249 (12.8) | |
| Physical activity (met-h/week) | <0.001 | |||
| 0 | 1279 (22.5) | 1077 (23.7) | 547 (28.0) | |
| >0 | 4396 (77.5) | 3462 (76.3) | 1405 (72.0) | |
| Sedentary time (hours) | <0.001 | |||
| <5 | 2611 (46.0) | 2023 (44.6) | 765 (39.2) | |
| ≥5 | 3064 (54.0) | 2516 (55.4) | 1187 (60.8) | |
| Characteristics | Hypertension (Col %) | ||
|---|---|---|---|
| No (n = 7571) | Yes (n = 4595) | p Value | |
| Demographics | |||
| Age (years) | 46.1 ± 11.9 | 56.2 ± 13.0 | <0.001 |
| 30–44 | 3911 (79.5) | 1009 (20.5) | |
| 45–59 | 2436 (61.8) | 1507 (38.2) | |
| 60–79 | 1224 (37.1) | 2079 (62.9) | |
| Gender | 0.261 | ||
| Male | 3552 (61.7) | 2204 (38.3) | |
| Female | 4019 (62.7) | 2391 (37.3) | |
| Race | 0.189 | ||
| Non-white a | 4137 (61.7) | 2567 (38.3) | |
| White | 3434 (62.9) | 2028 (37.1) | |
| Marital status | <0.001 | ||
| Married/Living with partner | 5198 (64.8) | 2831 (35.3) | |
| Widowed/Divorced/Separated/ Never married | 2373 (57.4) | 1764 (42.6) | |
| Education level | <0.001 | ||
| ≤High school | 3300 (58.9) | 2302 (41.1) | |
| >High school | 4271 (65.1) | 2293 (34.9) | |
| Health insurance | <0.001 | ||
| No | 2080 (70.2) | 884 (29.8) | |
| Yes | 5491 (59.7) | 3711 (40.3) | |
| Clinical status | |||
| BMI (kg/m2) | <0.001 | ||
| <25 | 2544 (73.2) | 930 (26.8) | |
| ≥25 | 5027 (57.8) | 3665 (42.2) | |
| Health behaviors | |||
| Sleep duration (hours) | <0.001 | ||
| <7 | 4546 (64.4) | 2514 (35.6) | |
| 7–9 | 2888 (59.2) | 1987 (40.8) | |
| >9 | 137 (59.3) | 94 (40.7) | |
| Self-reported trouble sleeping | <0.001 | ||
| No | 6043 (65.2) | 3227 (34.8) | |
| Yes | 1528 (52.8) | 1368 (47.2) | |
| Self-reported sleep disorder | <0.001 | ||
| No | 7145 (63.3) | 4142 (36.7) | |
| Yes | 426 (48.5) | 453 (51.5) | |
| Sleep patterns | <0.001 | ||
| Healthy sleep | 3757 (66.2) | 1918 (33.8) | |
| Intermediate sleep | 2852 (62.8) | 1687 (37.2) | |
| Poor sleep | 962 (49.3) | 990 (50.7) | |
| DASH index | 0.637 | ||
| 0–3.5 | 5783 (62.1) | 3527 (37.9) | |
| 4–7.5 | 1788 (62.6) | 1068 (37.4) | |
| Smoking status b | <0.001 | ||
| No | 4350 (64.5) | 2394 (35.5) | |
| Yes | 3221 (59.4) | 2201 (40.6) | |
| Alcohol intake (gm/day) | 0.378 | ||
| 0–24.9 | 6462 (62.4) | 3895 (37.6) | |
| 25.1–550.1 | 1109 (61.3) | 700 (38.7) | |
| Physical activity (met-h/week) | <0.001 | ||
| 0 | 1595 (54.9) | 1308 (45.1) | |
| >0 | 5976 (64.5) | 3287 (35.5) | |
| Sedentary time (hours) | <0.001 | ||
| <5 | 3459 (64.1) | 1940 (35.9) | |
| ≥5 | 4112 (60.8) | 2655 (39.2) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, C.; Shang, S. Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014). Int. J. Environ. Res. Public Health 2021, 18, 7867. https://doi.org/10.3390/ijerph18157867
Li C, Shang S. Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014). International Journal of Environmental Research and Public Health. 2021; 18(15):7867. https://doi.org/10.3390/ijerph18157867
Chicago/Turabian StyleLi, Chunnan, and Shaomei Shang. 2021. "Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014)" International Journal of Environmental Research and Public Health 18, no. 15: 7867. https://doi.org/10.3390/ijerph18157867
APA StyleLi, C., & Shang, S. (2021). Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014). International Journal of Environmental Research and Public Health, 18(15), 7867. https://doi.org/10.3390/ijerph18157867





