The Impact of the Affordable Care Act on Dental Care: An Integrative Literature Review
Abstract
:1. Introduction
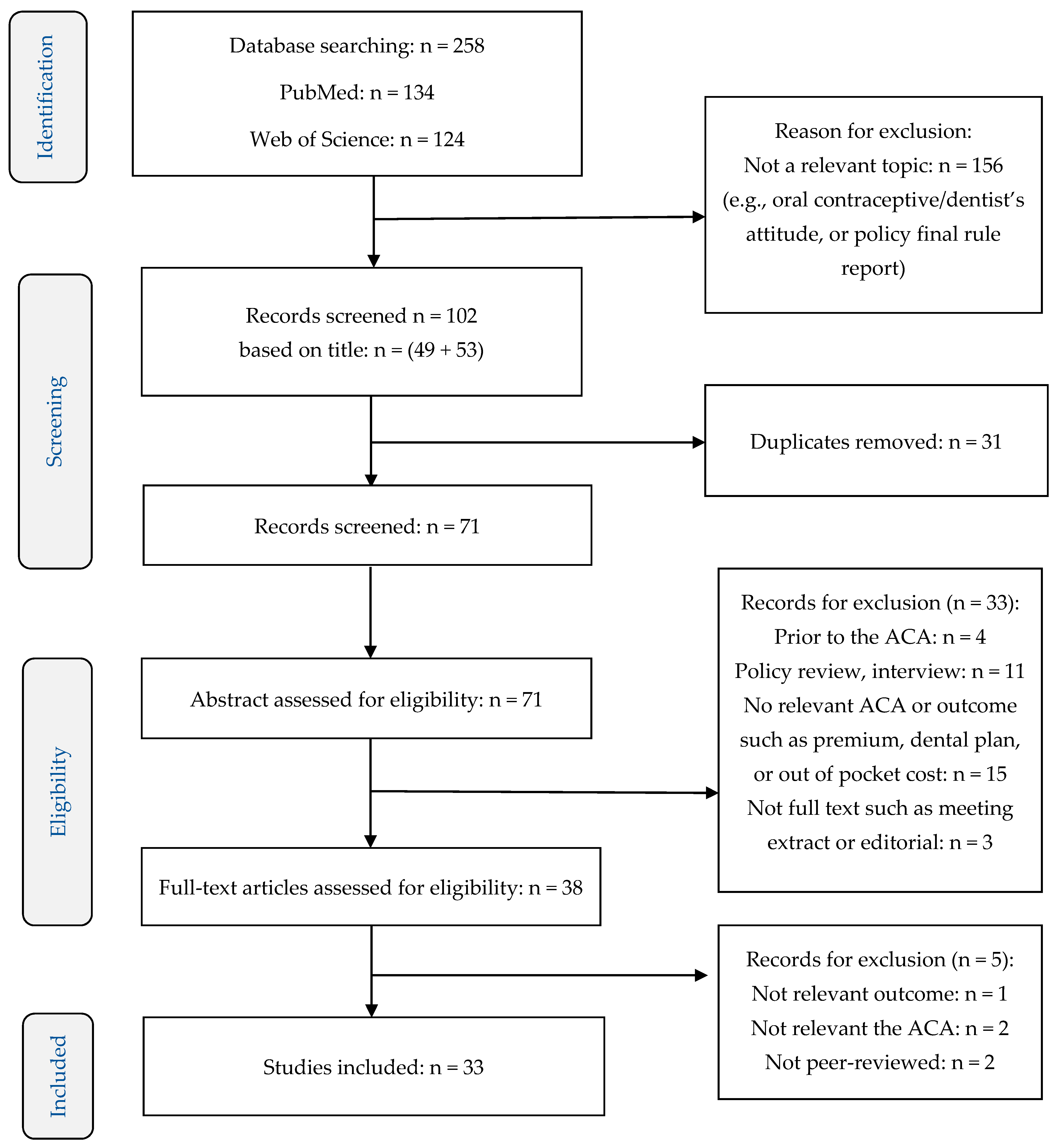
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion Criteria and Screening
2.3. Data Extraction
3. Results
3.1. Description of Studies
3.2. Dental Care Coverage for Adults
3.3. Dental Coverage for Children
3.4. Dental Care Access and Utilization
3.5. Emergency Department (ED) Visits
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- The Public Health and Welfare. Available online: https://www.govinfo.gov/content/pkg/USCODE-2010-title42/pdf/USCODE-2010-title42-chap157-subchapIII-partA-sec18022.pdf (accessed on 13 January 2020).
- American Dental Association. Dental Care Utilization in the U.S. ADA Health Policy Institute—Infographic. 2017. Available online: https://www.ada.org/~/media/ADA/ScienceandResearch/HPI/Files/HPIgraphic_1117_2.pdf?la=en (accessed on 14 July 2021).
- Centers for Medicare & Medicaid Services. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical (accessed on 14 July 2021).
- Currie, R.B.; Pretty, I.A.; Tickle, M.; Maupomé, G. Conundrums in health care reform: Current experiences across the North Atlantic. J. Public Health Dent. 2012, 72, 143–148. [Google Scholar] [CrossRef]
- Shane, D.M.; Ayyagari, P. Spillover Effects of the Affordable Care Act? Exploring the Impact on Young Adult Dental Insurance Coverage. Health Serv. Res. 2014, 50, 1109–1124. [Google Scholar] [CrossRef] [Green Version]
- French, M.T.; Homer, J.; Gumus, G.; Hickling, L. Key Provisions of the Patient Protection and Affordable Care Act (ACA): A Systematic Review and Presentation of Early Research Findings. Health Serv. Res. 2016, 51, 1735–1771. [Google Scholar] [CrossRef]
- Howell, E.M.; Kenney, G.M. The impact of the medicaid/CHIP expansions on children: A synthesis of the evidence. Med. Care Res. Rev. 2012, 69, 372–396. [Google Scholar] [CrossRef]
- Shane, D.M.; Wehby, G.L. Were Patient Protection and Affordable Care Act spillover gains to private dental coverage for dependents widely shared? An analysis using Medical Expenditure Panel Survey data. J. Am. Dent. Assoc. 2020, 151, 182–189. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumont, D.M.; Oh, J.; Cooper, T. State-Level Surveillance of Underinsurance and Health Care-Related Financial Burden. J. Public Health Manag. Pr. 2017, 23, e10–e16. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.S. Spillovers from the Patient Protection and Affordable Care Act to employer-sponsored dental insurance enrollment. J. Am. Dent. Assoc. 2018, 149, 1049–1056.e1. [Google Scholar] [CrossRef] [PubMed]
- Shane, D.M.; Wehby, G.L. The Impact of the Affordable Care Act’s Dependent Coverage Mandate on Use of Dental Treatments and Preventive Services. Med. Care 2017, 55, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Vujicic, M.; Yarbrough, C.; Nasseh, K. The Effect of the Affordable Care Act’s Expanded Coverage Policy on Access to Dental Care. Med. Care 2014, 52, 715–719. [Google Scholar] [CrossRef]
- Kranz, A.M.; Dick, A.W. Changes in pediatric dental coverage and visits following the implementation of the affordable care act. Health Serv. Res. 2018, 54, 1–9. [Google Scholar] [CrossRef]
- Kranz, A.M.; Dick, A.W. Low rates of pediatric dental coverage for families purchasing marketplace insurance plans. J. Public Health Dent. 2019, 79, 275–278. [Google Scholar] [CrossRef] [PubMed]
- Cawley, J.; Soni, A.; Simon, K. Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S. J. Gen. Intern. Med. 2018, 33, 1495–1497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farietta, T.P.; Lu, B.; Tumin, R. Ohio’s Medicaid Expansion and Unmet Health Needs Among Low-Income Women of Reproductive Age. Matern. Child Health J. 2018, 22, 1771–1779. [Google Scholar] [CrossRef]
- Han, X.; Nguyen, B.T.; Drope, J.; Jemal, A. Health-Related Outcomes among the Poor: Medicaid Expansion vs. Non-Expansion States. PLoS ONE 2015, 10, e0144429. [Google Scholar] [CrossRef] [PubMed]
- Johansen, M.E.; Richardson, C.R. The Ecology of Medical Care Before and After the Affordable Care Act: Trends From 2002 to 2016. Ann. Fam. Med. 2019, 17, 526–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotagal, M.; Carle, A.C.; Kessler, L.G.; Flum, D.R. Limited Impact on Health and Access to Care for 19- to 25-Year-Olds Following the Patient Protection and Affordable Care Act. JAMA Pediatr. 2014, 168, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.S.; Adams, S.H.; Park, M.J.; Boscardin, W.J.; Irwin, C.E. Improvement in preventive care of young adults after the affordable care act: The affordable care act is helping. JAMA Pediatr. 2014, 168, 1101–1106. [Google Scholar] [CrossRef] [Green Version]
- Lyu, W.; Shane, D.M.; Wehby, G.L. Effects of the Recent Medicaid Expansions on Dental Preventive Services and Treatments. Med. Care 2020, 58, 749–755. [Google Scholar] [CrossRef]
- Peck, J.; Sedgley, C.M.; Schwarz, E.; Replogle, K.J. The impact of the Affordable Care Act on provision of endodontic services within a dental school setting in Oregon. J. Public Health Dent. 2019, 79, 175–180. [Google Scholar] [CrossRef]
- Seo, V.; Baggett, T.P.; Thorndike, A.N.; Hull, P.; Hsu, J.; Newhouse, J.P.; Fung, V. Access to care among Medicaid and uninsured patients in community health centers after the Affordable Care Act. BMC Health Serv. Res. 2019, 19, 291. [Google Scholar] [CrossRef]
- Simon, K.; Soni, A.; Cawley, J. The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions. J. Policy Anal. Manag. 2017, 36, 390–417. [Google Scholar] [CrossRef]
- Singhal, A.; Damiano, P.; Sabik, L. Medicaid Adult Dental Benefits Increase Use of Dental Care, But Impact of Expansion on Dental Services Use Was Mixed. Health Aff. 2017, 36, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Wehby, G.L.; Lyu, W.; Shane, D.M. The Impact of the ACA Medicaid Expansions on Dental Visits by Dental Coverage Generosity and Dentist Supply. Med. Care. 2019, 57, 781–787. [Google Scholar] [CrossRef]
- Zwetchkenbaum, S.; Oh, J. More Rhode Island Adults Have Dental Coverage After the Medicaid Expansion: Did More Adults Receive Dental Services? Did More Dentists Provide Services? Rhode Isl. Med. J. 2017, 100, 51–53. [Google Scholar]
- Nasseh, K.; Vujicic, M. The impact of the affordable care act’s Medicaid expansion on dental care use through 2016. J. Public Health Dent. 2017, 77, 290–294. [Google Scholar] [CrossRef]
- Khouja, T.; Dmd, J.M.B.; Donohue, J.M.; Roberts, E.T. Association between Medicaid expansion, dental coverage policies for adults, and children’s receipt of preventive dental services. Health Serv. Res. 2020, 55, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Kino, S.; Kawachi, I. The impact of ACA Medicaid expansion on socioeconomic inequality in health care services utilization. PLoS ONE 2018, 13, e0209935. [Google Scholar] [CrossRef] [Green Version]
- Nasseh, K.; Vujicic, M. Early Impact of the Affordable Care Act’s Medicaid Expansion on Dental Care Use. Health Serv. Res. 2016, 52, 2256–2268. [Google Scholar] [CrossRef] [Green Version]
- Yörük, B.K. Health insurance coverage and health care utilization: Evidence from the Affordable Care Act’s dependent coverage mandate. Forum Health Econ. Policy 2018, 21, 1–24. [Google Scholar] [CrossRef]
- Soni, A. The effects of public health insurance on health behaviors: Evidence from the fifth year of Medicaid expansion. Health Econ. 2020, 29, 1586–1605. [Google Scholar] [CrossRef]
- Chalmers, N.; Grover, J.; Compton, R. After Medicaid Expansion in Kentucky, Use of Hospital Emergency Departments For Dental Conditions Increased. Health Aff. 2016, 35, 2268–2276. [Google Scholar] [CrossRef]
- Laniado, N.; Badner, V.M.; Silver, E.J. Expanded Medicaid dental coverage under the Affordable Care Act: An analysis of Minnesota emergency department visits. J. Public Health Dent. 2017, 77, 344–349. [Google Scholar] [CrossRef]
- Rampa, S.; Veeratrishul, A.; Raimondo, M.; Connolly, C.; Allareddy, V.; Nalliah, R. Hospital-based Emergency Department Visits with Periapical Abscess: Updated Estimates from 7 Years. J. Endod. 2019, 45, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Elani, H.W.; Kawachi, I.; Sommers, B.D. Changes in emergency department dental visits after Medicaid expansion. Health Serv. Res. 2020, 55, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Laniado, A.N.; Brow, R.; Tranby, E.; Badner, V.M. Trends in non-traumatic dental emergency department use in New York and New Jersey: A look at Medicaid expansion from both sides of the Hudson River. J. Public Health Dent. 2020, 80, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Edelstein, B.L.; Samad, F.; Mullin, L.; Booth, M. Oral Health Provisions in U.S. Health Care Reform. J. Am. Dent. Assoc. 2010, 141, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- Kenney, G.M.; Zuckerman, S.; Dubay, L. Opting in to the Medicaid Expansion under the ACA: Who Are the Uninsured Adults Who Could Gain Health Insurance Coverage? Available online: http://www.urban.org/sites/default/files/publication/25706/412630-Opting-in-to-the-Medicaid-Expansion-under-the-ACA.PDF (accessed on 13 January 2020).
- Medicaid. Dental Care. Available online: https://www.medicaid.gov/medicaid/benefits/dental-care/index.html (accessed on 13 January 2020).
- The Henry J. Kaiser Family Foundation. Status of State Medicaid Expansion Decisions. 2021. Available online: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ (accessed on 13 January 2020).
- Center for Health Care Strategies, Medicaid Adults Dental Benefits: An Overview. Center for Health Care Strategies. 2019. Available online: http://www.ada.org/~/media/ADA/ScienceandResearch/HPI/Files/HPIBrief_1016_1.pdf (accessed on 13 January 2020).
- Gooch, B.F.; Berkey, D.B. Subjective factors affecting the utilization of dental services by the elderly. Gerodontics 1987, 3, 65–69. [Google Scholar]
- Manski, M.R.J.; Macek, D.; Moeller, J.F. Private dental coverage: Who has it and how does it influence dental visits and expenditures? J. Am. Dent. Assoc. 2002, 133, 1551–1559. [Google Scholar] [CrossRef]
- Manski, R.; Brown, E. Dental Use, Expenses, Private Dental Coverage, and Changes, 1996 and 2004. Available online: https://www.meps.ahrq.gov/mepsweb/data_stats/Pub_ProdResults_Details.jsp?pt=Chartbook&opt=2&id=827 (accessed on 10 February 2020).
- Nasseh, K.; Vujicic, M.; Yarbrough, C. A ten-year, state-by-state, analysis of Medicaid fee-for-service reimbursement rates for dental care services. Am. Dent. Assoc. 2014, 20, 21. [Google Scholar]
- Kino, S.; Kawachi, I. Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance? Health Educ. Behav. 2019, 47, 134–142. [Google Scholar] [CrossRef] [PubMed]
- ADA Health Policy Institute Data Center. Supply & Profile of Dentists. Available online: https://www.ada.org/en/science-research/health-policy-institute/data-center/supply-and-profile-of-dentists (accessed on 16 February 2021).
- Logan, H.L.; Catalanotto, F.; Guo, Y.; Marks, J.; Dharamsi, S. Barriers to Medicaid Participation among Florida Dentists. J. Health Care Poor Underserved 2015, 26, 154–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institute of Medicine and National Research Council. Improving Access to Oral Health Care for Vulnerable and Underserved Populations; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Congressional Budget Office. Federal Subsidies for Health Insurance Coverage for People Under Age 65:2018 to 2028. Available online: www.cbo.gov/publication/53826 (accessed on 5 March 2021).
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Wiley Online Books; Wiley: Hoboken, NJ, USA, 2008. [Google Scholar]
| Search Engine | Search Term |
|---|---|
| PubMed | “Patient protection and Affordable Care Act” [MeSH Terms] † AND (dental* OR oral*) [Title/Abstract] |
| Web of Science | “Patient protection and Affordable Care Act” OR “Affordable care act” [Topic] AND (dental* OR oral*) [Topic] |
| Citation | Data Sources, Analyses | Study Population | Measures | Findings |
|---|---|---|---|---|
| Shane and Ayyagari (2015) [5] ACA (dependent expansion) | The MEPS, 2006–2009, and 2011 Difference-in-differences analysis | Adults aged 19–25 and 27–30 | Private dental coverage | Private dental coverage for adults aged 19–25 increased by 6.7 percent points in 2011 compared to adults aged 27–30, relative to pre-ACA (p < 0.05). Private dental coverage for adults aged 19–25 with household incomes between 125 and 400 FPL increased by 14 percent points compared to adults aged 27–30, relative to pre-ACA (p < 0.05). There was no significant effect of the dependent mandate on private dental coverage among poorer (<125 FPL) or higher household income (>400 FPL) individuals. |
| Shane and Wehby (2020) [8] The dependent mandate | The MEPS, 2006–2015 Difference-in-differences | 19–25 years and 27–30 years | Private dental insurance Preventive dental service use Dental treatment Any (preventive + treatment) | Regardless of race, young adults (19–25 years) had higher rates of private dental coverage after the implementation of the dependent mandate compared with adults aged 27–30 years (non-Hispanic black [12 percentage points increase]; Hispanic [7 percentage points increase]; and non-Hispanic white [8 percentage points]). Among non-Hispanic blacks aged 19–25 years, dental visits increased by 7.8 percentage points after the implementation of the dependent mandate, compared with non-Hispanic black adults 27–30 years (CI: 0.013–0.143). Among non-Hispanic blacks aged 19–25 years, preventive dental visits increased by 5.6 percentage points after the implementation of the dependent mandate, compared with non-Hispanic black adults aged 27–30 years (CI: −0.001–0.113); however, there was no statistically significant changes in receipt of dental treatment for these age 19 to 25. There were no statistically significant changes in preventive treatment, or both services for non-Hispanic white and Hispanics. There were significant increases in dental coverage among young adults (19–25) with low income (<200% FPL) and with high income (>200% FPL) compared with adults aged 27–30 (7.1 percentage points in low-income adults vs 9.2 percentage points in high-income adults). There were no significant changes in dental service use among low-income adults aged 19–25 compared with low-income adults aged 27–30, whereas there was a marginally significant increase in any dental visits (3.6 percentage points) and dental treatment (2.4 percentage points) among high-income adults aged 19–25 compared with high-income adults aged 27–30. |
| Dumont, Oh, and Copper (2017) [10] | The BRFSS in Rhode Island, 1 January–1 October, 2013 and full year of 2014 | Adults age 18 and older | Absence of dental coverage between 2013 and 2014 | The percentage of dentally uninsured adults did not change significantly: 29.6% (95% CI 28.0–31.2) in 2014 compared with 32.5% (95% CI, 30.2–34.7) before October 2013. |
| Huang (2018) [11] Dependent expansion | Delta Dental of Michigan, 2008–2013 Difference-in-differences linear regression | Young adults aged 20–24 years and older adults 30–34 years | Dental plan enrollment Oral health care use rates | Dental plan enrollment among young adults increased 1.3 percentage points after implementing dependent expansion, relative to the older adult group (p < 0.01). Oral care use among young adults increased 0.39 percentage points after implementing dependent expansion, relative to the older adult group (p < 0.05). |
| Shane and Wehby (2017) [12] ACA (dependent mandate) | The MEPS, 2006–2013 Difference-in-differences analysis | Adults aged 25 and 27 | Private dental coverage Preventive dental service use Any dental treatment | Private dental coverage for 25 years increased by eight percentage points in post-ACA compared with 27 years, relative to pre-ACA (p < 0.05). There was no significant effect of dependent mandate on preventive dental service use among 25 years compared with 27 years. Dental treatments for 25 years increased by 4.8 percentage points in the post-ACA compared to 27 years, relative to the pre-ACA (p < 0.05). |
| Vujicic, Yarbrough, and Nasseh (2014) [13] ACA (dependent expansion) | The NHIS, 2008–2012 Difference-in-differences | Adults aged 19–25 and 26–34 | Private dental benefit coverage Dental care visits in the last 12 months Financial barriers to obtaining needed dental care | Private dental benefit coverage for adults aged 19–25 increased by 5.6% in 2011 compared with adults aged 26–34 (p < 0.01), relative to pre-ACA passing (2008–2010). Private dental benefit coverage for adults aged 19–25 increased by 6.9% in 2012 compared with adults aged 26–34, relative to pre-ACA (2008–2010) (p < 0.01). Dental care visits for adults aged 19–25 increased by 2.8% in 2011 compared with adults aged 26–34, relative to pre-ACA (p = 0.062). Dental care visits for adults aged 19–25 increased by 3.3% in 2012 compared with adults aged 26–34, relative to pre-ACA (p = 0.038). The percentage of adults aged 19–25 reporting financial barriers to dental care declined by 2.1% in 2011 compared with adults aged 26–34, relative to pre-ACA (p = 0.068). The percentage of adults aged 19–25 reporting financial barriers to dental care declined by 2.1% in 2012 compared with adults aged 26–34, relative to pre-ACA (p = 0.087). |
| Kranz and Dick (2018) [14] ACA (10 essential health benefits) | The NHIS, 2010–2015 Difference-in-differences multivariate linear probability regression | Children aged 1–18 without public health insurance (n = 16,404) | Rates of dental insurance Rates of dental visit in the past 12 months | Private dental coverage increased by 4.6 percentage points among children who were affected by the ACA’s essential health benefits (EHB) compared to children who were not affected by the ACA’s EHB in 2014–2015, relative to the pre-ACA period of 2010–2013 (p = 0.013). The percentage of having a dental visit in the past year increased by 2.7 percentage points for children who were affected by the ACA’s EHB compared to children who were not affected by the ACA’s EHB in the post ACA period, but it was not statistically significant (p = 0.071). |
| Kranz and Dick (2019) [15] ACA (dental coverage via the market place) | The NHIS, 2014–2015 | Children age 0–18 (n = 696) | Parent reported rate of pediatric dental coverage | During 2014–2015, 14.5% of children obtaining medical insurance from marketplaces offering optional dental coverage reported they had dental insurance. During 2014–2015, 9.0% of children obtaining medical insurance from marketplaces requiring purchase of dental coverage reported they had dental insurance. During 2014–2015, 2015, 23.7% of children obtaining medical insurance from marketplaces with dental coverage embedded in all medical plans reported that they had dental insurance. |
| Cawley, Soni, and Simon (2018) [16] Medicaid expansion | The Behavioral Risk Factor Surveillance System (BRFSS), 2010–2016 Difference-in-differences analysis | Low-income childless adults aged 19–64 (n = 80,200) | A dental care visit in the past 12 months | Medicaid expansion increased the probability of having visited a dentist in the past 12 months by 2.5 percentage points (95% CI 0.0001–0.050, p = 0.05). |
| Farietta, Lu, and Tumin (2018) [17] Medicaid expansion | Data: Ohio Medicaid Assessment Survey (OMAS), 2012 and 2015 Logistic regression | Low-income women aged 19–44 who were newly eligible for Medicaid after expansion (n = 489 in 2012 & 1273 in 2015) | Unmet dental needs during the past 12 months A dental care visit in the past year | Low-income women had significantly lower odds of reporting an unmet dental care need in 2015 than in 2012 (OR = 0.72, 95% CI 0.54, 0.95). Odds of low-income women having a dental care visit after Medicaid expansion were not significantly increased (OR = 1.05, 95% CI 0.80, 1.37). |
| Han, Ngyuyen, Drope, and Jemal (2015) [18] Medicaid expansion | The Medical Expenditure Panel Survey (MEPS), 2010–2012 Multivariate logistic, and two parts modeling approach with a logistic regression and Poisson regression | Low-income adults aged 18–64 (n = 9755 in Medicaid expanding states & 7455 in nonexpanding states) | Unmet dental care need Preventive dental service (dental checkup) Number of dental visits | The Medicaid non-expansion group was more likely to be unable to get or delay necessary dental care than the Medicaid expansion group, but the difference was not statistically significant (12.5% vs 14.0%, PR = 1.19, CI 0.98–1.43). The non-expansion group was less likely to have dental check-ups than the Medicaid expansion group (37.7% vs 42.7%, PR = 0.86, CI 0.79–0.94). The non-expansion group had 0.08 fewer dental visits annually than those in the Medicaid expansion group (CI 0.01–0.14). |
| Johansen and Richardson (2019) [19] ACA | The MEPS, 2012–2015 Analyses: adjusted Wald test | Adults aged 18 and older | The number of individuals per 1000 persons who had dental visits per month | The number of individuals who had received dental services in the past month increased in post ACA (67 persons per 1000 per month in 2012–2013 compared to 70 persons per 1000 per month in 2014–2015, p = 0.035). |
| Kotagal, Carle, Kessler, and Flum (2014) [20] ACA | The National Health Interview Survey (NHIS), 2009 and 2012 Difference-in-differences analysis | Adults aged 19–25 years and 26–34 years | Rates of inability to afford dental care in the past year | There was no significant difference in young adults’ (aged 19–25 years) reports of inability to afford dental care in the past year between 2009 and 2012 compared with adults aged 26–34 (DID = −2.6%, 95% CI, −5.61 to 0.61). |
| Lau, Adams, Park, Boscardin, and Irwin (2014) [21] ACA | The MEPS, 2009 and 2011 Logistic regression | Adults aged 18–25 (n = 3768 in 2009 & 3717 in 2011) | Rates of annual dental visit in past year | The rate of receiving an annual dental visit increased from 55.2% in 2009 to 60.9% in 2012 (p < 0.001). Adults aged 18–25 were more likely to receive an annual dental visit in 2012 compared with 2009 (OR = 1.3 CI, 1.1–1.4). After controlling for insurance types (full-year private; full year public; partial year uninsured; full-year uninsured), the degree of difference between 2009 and 2011 decreased, but remained significant (OR = 1.2, CI, 1.0–1.3, p < 0.05). After controlling for covariates, adults aged 18–25 were more likely to receive an annual dental visit in 2012 compared with in 2009 (OR = 1.3 CI, 1.1–1.5, p < 0.01). |
| Lyu, et al. (2020) [22] Medicaid expansion | The MEPS, 2011–2016 Difference-in-differences | Adults aged 19–64 whose newly eligible income level (below 138% FPL) for Medicaid | Preventive dental visit Dental treatments | Among states offering extensive dental benefits, the likelihood of preventive dental visits for Medicaid expansion states increased by five percentage points after implementation of Medicaid expansion (2014–2016) compared with non-Medicaid expansion states. Among states offering extensive dental benefits, the likelihood of dental treatments for Medicaid expansion states increased by four–five percentage points in 2014–2015, but the effect of Medicaid expansion decreased and became insignificant in 2016. Among states offering limited dental benefits, the likelihood of preventive dental visits for Medicaid expansion states increased by seven–eight percentage points after implementation of Medicaid expansion of the ACA (in 2014 and 2015) compared with non-Medicaid expansion states, but the effect of the Medicaid expansion decreased and became insignificant in 2016. Among states offering limited dental benefits, the likelihood of dental treatments for Medicaid expansion states increased by three–five percentage points after implementation of Medicaid expansion (2014–2016), but the increase was insignificant. Among states offering emergency only coverage, the likelihood of preventive dental visits for Medicaid expansion states increased by five–eight percentage points after implementation of Medicaid expansion compared with non-Medicaid expansion states, but increases were not significant. Among states offering emergency only coverage, the likelihood of dental treatments for Medicaid expansion states increased by five percentage points in 2015 and 2016 compared with non-Medicaid expansion states, but the increase in 2014 was not significant. |
| Peck, Sedgley, and Schwarz (2019) [23] ACA (dental benefits for Medicaid as part of Oregon Health Plan (OHP) | Electronic health records in the Oregon Health & Science University Graduate Endodontic Clinic (GES), 2010–2017 Chi-square | Patients (children 0–20 and adults 21–64) who attended in Graduate Endodontic Clinic | The number of non-surgical root canal therapy (NS-RCT) | There was significant increase in the number of NS-RCT provided for patients covered by OHP post-ACA compared to pre-ACA (152 in pre-ACA vs 674 in post-ACA, 363% increase), whereas there was a significant decrease in the number of NS-RCT provided for non-OHP patients (1032 in pre-ACA vs 844 in post-ACA) (p < 0.00001). The number of both of adults and children whose NS-RCT was covered by OHP increased their receipt of NS-RCT services in the post-ACA period, whereas the number of non-OHP adults and children decreased their receipt of NS-RCT (p < 0.00001). |
| Seo, et al. (2019) [24] ACA on access to community health centers | The Health Center Patient Survey, 2014 Logistic regression | Adults aged 18 or older who sought care at Community Health Center | Delayed or unable to get dental care need in the past 12 months | Those uninsured were more likely to have delayed or no dental care in the past 12 months than those with Medicaid (OR = 2.4, CI, 1.3–4.6). |
| Simon, Soni, and Cawley (2017) [25] ACA | The BRFSS, 2010, 2012, 2014, and 2015 Difference-in-differences analysis | Low-income (below 100% FPL) adults aged 19–64 | Dental visit in the past year | There was no significant effect of Medicaid expansion on dental visits for low-income adults. Among childless adults, the probability of a dental visit increased by 4.1 percentage points post-ACA implementation, relative to pre-ACA passing (p < 0.01). |
| Singhal, Damiano, and Sabik (2017) [26] Medicaid expansion | The BRFSS, 2010 and 2014 Multivariate linear regression model | Low-income (annual household income $ <15,000) adults aged 21–64 | Dental visit in the past 12 months | The probability of having had a dental visit in the past year among low-income residents of Medicaid expansion states with dental benefits decreased from 52.3% in 2010 to 50.4% in 2014 (p < 0.001). Among states that provided dental benefits, the probability of low-income parents visiting a dentist decreased from 56.0% in 2010 to 47.9% in 2014 in Medicaid expansion states (p < 0.0001). Among states that provided dental benefits, the probability of childless adults having had a dental visit in the past year increased from 48.6% in 2010 to 50.4% in 2014 in Medicaid expansion states (p < 0.0001). |
| Wehby, Lyu, and Shane (2019) [27] ACA on dental care use by dental benefits and dental supply (dentist availability in states) | The BRFSS, 2012, 2014 and 2016 Difference-in-differences | Low-income (<138% FPL) adults aged 18–64 | Dental visit in the past 12 months | Low-income adults residing in Medicaid expansion states which offered extensive dental coverage were 5.8 percentage points more likely to have a dental visit in 2016 when compared to 2012 (p < 0.01). Low-income adults residing in Medicaid expansion states which offered limited dental benefits were 1.1 percentage points more likely to have a dental visit in 2016 when compared with 2012, but it was not significant. Low-income adults residing in Medicaid expansion states which offered emergency dental benefits were 7.1 percentage points less likely to have a dental visit in 2016 when compared with 2012 (p < 0.05). There was a significant effect of Medicaid expansion with extensive dental coverage in states with high numbers of available dentist or high dentist availability (the likelihood of dental visits increased by 6.7 percentage points in states with high dentist availability). There was no significant effect of Medicaid expansion providing limited dental coverage in areas with low or high concentrations of available dentists. |
| Zwetchkenbaum and Oh (2017) [28] Medicaid expansion | Medicaid enrollment & dental claims from Rhode Island Medicaid Management Information system, 2012–2015 | Medicaid enrollees aged 18–64 | Annual unduplicated numbers of dental care service use Percentage of Medicaid enrollees who had dental service | The number of Medicaid enrollees who received dental services increased by 46% between 2013 (33,800) and 2015 (49,312). However, the percentage of Medicaid enrollees who received dental services decreased from 39% in 2013 to 32% in 2015. |
| Nasseh and Vujicic (2017) [29] ACA | The Gallup-Healthways Wellbeing Index survey, 2010–2016 Difference-in-differences analysis of data | Adults aged 21–64 with household income at or below 138% FPL | Receiving a dental service in the last year | The younger age group increased by 0.39 percentage points in oral care use after implementing dependent expansion, relative to older age group (p < 0.05) Dental care use among low-income adults in expansion states with adult Medicaid dental benefits increased by 2.8% in 2015 (p = 0.049) and 2.8% in 2016 (p = 0.042), relative to states with non-Medicaid expansion states and without dental benefits. Dental care use among low-income adults in expansion states with adult Medicaid dental benefits increased by 2.6% in 2015 (p = 0.007) and 6.4% in 2016 (p < 0.001), relative to states with non-Medicaid expansion and with Medicaid-provided dental benefits to adults. Dental care use among low-income adults in expansion states with adult Medicaid dental benefits increased by 0.01% in 2015 (p = 0.995) and 5.8% 2016 (0.001), relative to states with Medicaid expansion and without Medicaid-provided dental benefits to adults. |
| Khoujs et al., (2020) [30] Medicaid expansion | The MEPS, 2011–2016 | Dyads of children (6–18 years old) and parents (21–64 years old) in family below 125% FPL | Preventive dental service (cleaning, fluoride treatment or sealant application) | In states that covered preventive dental services for adults with Medicaid, the implementation of Medicaid expansion was not statistically significant with regard to the probability of children receiving preventive dental services (1.26 percentage points, CI: −3.74–6.27). In states that did not cover preventive dental services for adults with Medicaid, the implementation of the ACA was not followed by statistically significant changes in the probability of children receiving preventive dental services (3.3 percentage points, CI:−2.76–8.81). |
| Kino and Kawachi (2018) [31] ACA (Medicaid expansion) | The BRFSS, 2011–2016 Difference-in-differences analysis | Adults aged 18–64 years (n = 1,875,151) | Two indices of socioeconomic inequality in health service utilization (Having a dental visit in the past year): SII: Slope Index of Inequality RII: Relative Index of Inequality | Medicaid expansion was not associated with a reduction in income-based inequalities for having a dental visit in the past year. |
| Nasseh & Vujicic (2017) [32] ACA | The Gallup-Healthways Wellbeing Index survey, 2010–2014 Difference-in-differences analysis | Low-income (<138% FPL) adults aged 21–64 | Having a dental visit in the past 12 months | Dental care use for low-income adults residing in Medicaid expansion states (providing dental benefits) increased by 2.9 percentage points (from pre- to post-ACA) compared with low-income adults residing in non-Medicaid expansion states without dental benefits. (p = 0.083). Dental care use for low-income adults residing in Medicaid expansion states (providing dental benefits) increased by 6.2 percentage points (from pre-to post-ACA) compared with low-income adults residing in non-Medicaid expansion states with dental benefits. (p = 0.043). Dental care use for low-income adults residing in Medicaid expansion states (providing dental benefits) increased by 1.2 percentage points (from pre- to post-ACA) compared with low-income adults residing in non-Medicaid expansion states with dental benefits. (p = 0.763). |
| Yoruk. (2018) [33] Dependent mandate | The MEPS, 2011–2013 | Adults aged 23–29 | Dental visits | The probability of dental care utilization decreased by 1.0–2.1 percentage points when young adults turned 26 and the number of dental office visit decreased at this cutoff age (from 0.014 to 0.030 times per month). |
| Soni. (2020) [34] | The BRFSS, 2010–2018 Difference-in-differences | Childless low-income adults aged 19–64 (below 100% FPL) | Visited a dentist in the past year | For low-income adults without children, ACA Medicaid expansion increased the probability of a dentist visit by 2.3 percentage points (p < 0.05). |
| Chalmers, Grover, and Compton (2016) [35] Medicaid expansion | The State Emergency Department Databases of the Healthcare Cost and Utilization (HCUP) in Kentucky, 2010–2014 Descriptive | Adults older than 21 | ED discharges for conditions related to dental or oral health | The percentage of discharges for dental or oral health conditions by Medicaid increased (17.6% in 2013 to 49.7% in 2014). The percentage of discharges for dental or oral health conditions by the uninsured decreased (56.8% in 2013 to 20.5% in 2014). The percentage of those discharged with dental or oral health conditions among Medicaid enrollees increased in 2014 compared to 2013 (3.7% vs 2.7%). |
| Laniado, Badner, and Silver (2017) [36] ACA | The State Emergency Department Database for Minnesota, 2008 and 2014 Chi-square tests | Adult aged 18 and older | The total number of ED visits with non-traumatic dental conditions The rates of dental ED visits per 100,000 population and the number of dental ED visits (a percentage of total dental ED visits) | There was a 9.7% decrease in ED visits involving non-traumatic dental conditions between 2008 and 2014. The rate of ED visits involving non-traumatic dental conditions per 100,000 population decreased by 13.1% (612/100,000 in 2018 and 531/100,000 in 2014). |
| Rampa, et al. (2019) [37] ACA on ED use for periapical abscess | The Nationwide Emergency Department Sample (NEDS), 2008–2014 Chi-square | Patients who visited the ED with periapical abscess. | The rate of ED with periapical abscess visits per 100,000 people | The rate of ED visits with periapical abscess per 100,000 people increased from 151.31 in 2008 to 171.27 in 2014. |
| Elani et al. (2020) [38] Medicaid expansion | The state Emergency Department database (SEDD), 2012 & 2014 | Low-income adults aged 19–64 | ED visits with dental conditions | There was an overall increase in ED visits with dental conditions from 175,746 in 2012 to 200,198 in 2014. However, states that expanded Medicaid by offering adult dental benefits decreased ED visits for dental conditions (−14.1%). |
| Laniado, et al. (2020) [39] Medicaid expansion | The State Emergency Department Database for New York and New Jersey, 2010–2014 | ED discharge with non-traumatic dental conditions | The percentage of ED discharges with non-traumatic dental conditions decreased in NY and NJ from 2010 to 2014. In NJ, ED discharges with non-traumatic dental conditions by uninsured patients decreased by 35 percent, whereas discharges with non-traumatic dental conditions by Medicaid patients increased by 57 percent. In NY, ED discharges with non-traumatic dental conditions decreased steadily from 2010 to 2014, whereas discharges with non-traumatic dental conditions by Medicaid patients remained relatively steady between 2010 and 2014. | |
| Lee et al. (2020) * ACA | The MEPS, 2011–2016 | Adults older than 18 | Preventive oral checkup The number of dental treatment | There was an increase in preventive oral checkups received between pre-ACA and post-ACA, but the difference was not significant after controlling for education and poverty level. There was an increase in the number of dental treatments received between pre-ACA and post-ACA, but the difference was not significant after controlling for adults’ education and poverty level. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.; Kim, J.N.; Tomar, S.; Wong, L.N. The Impact of the Affordable Care Act on Dental Care: An Integrative Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 7865. https://doi.org/10.3390/ijerph18157865
Song J, Kim JN, Tomar S, Wong LN. The Impact of the Affordable Care Act on Dental Care: An Integrative Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(15):7865. https://doi.org/10.3390/ijerph18157865
Chicago/Turabian StyleSong, Jihee, Jeong Nam Kim, Scott Tomar, and Lauren N. Wong. 2021. "The Impact of the Affordable Care Act on Dental Care: An Integrative Literature Review" International Journal of Environmental Research and Public Health 18, no. 15: 7865. https://doi.org/10.3390/ijerph18157865
APA StyleSong, J., Kim, J. N., Tomar, S., & Wong, L. N. (2021). The Impact of the Affordable Care Act on Dental Care: An Integrative Literature Review. International Journal of Environmental Research and Public Health, 18(15), 7865. https://doi.org/10.3390/ijerph18157865






