The NUPHAC-EU Framework for Nurses’ Role in Interprofessional Pharmaceutical Care: Cross-Sectional Evaluation in Europe
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Framework and Survey Development
2.4. Data Collection
2.5. Data Analysis
3. Results
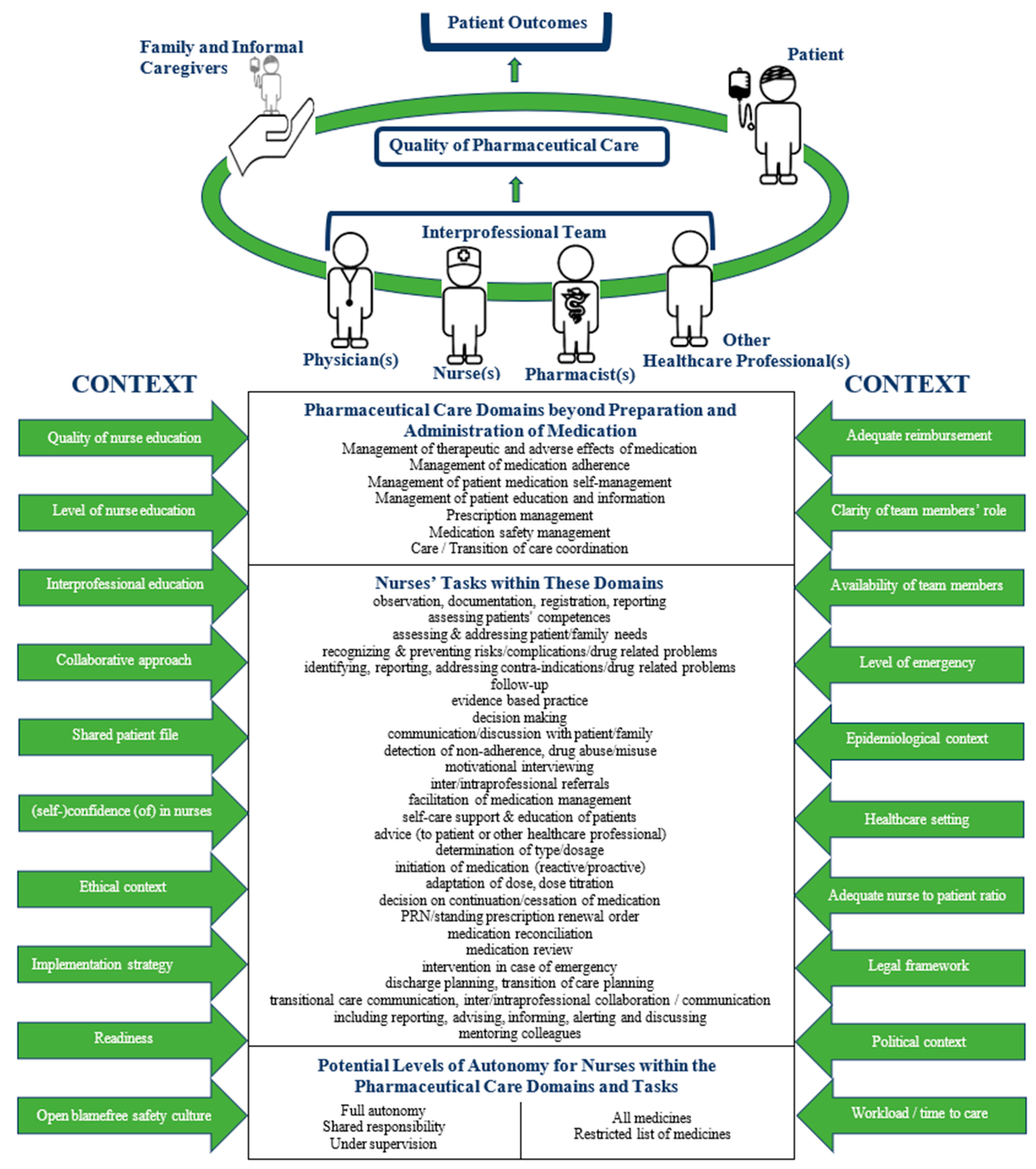
3.1. The NUPHAC-EU Framework for Nurses’ Role in Interprofessional Pharmaceutical Care in Europe
3.2. Research Population to Evaluate the NUPHAC-EU Framework
3.3. Healthcare Professionals’ Opinions about the Level of Nurse Responsibility for Nurses Performing Tasks in Interprofessional Pharmaceutical Care
3.3.1. Levels of Nurse Responsibility for European Nurses
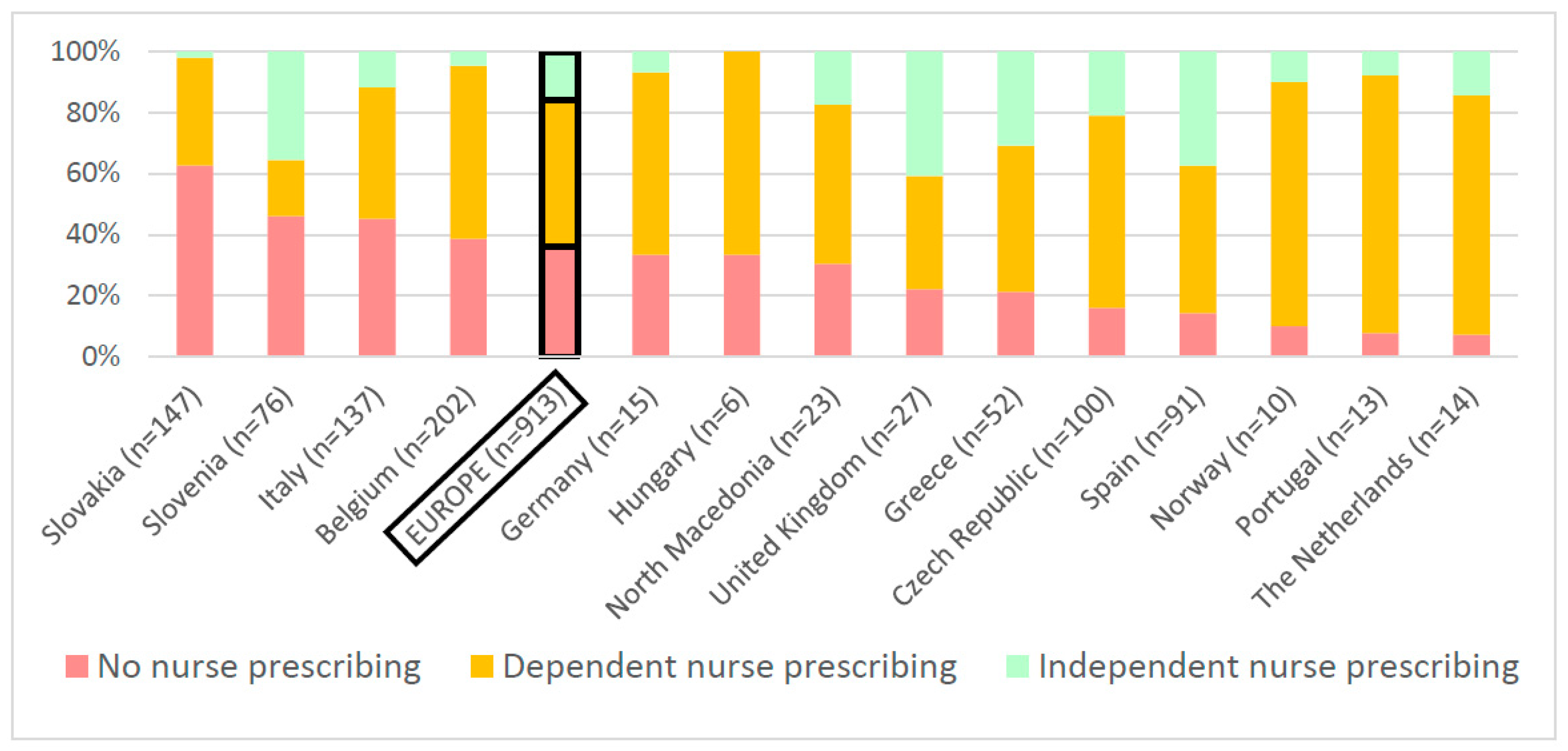
3.3.2. The Ideal Level of Nurse Prescribing
3.3.3. Differences in Levels of Nurse Responsibility between Countries
3.3.4. Levels of Nurse Responsibility for European Nurses of Different Educational Levels
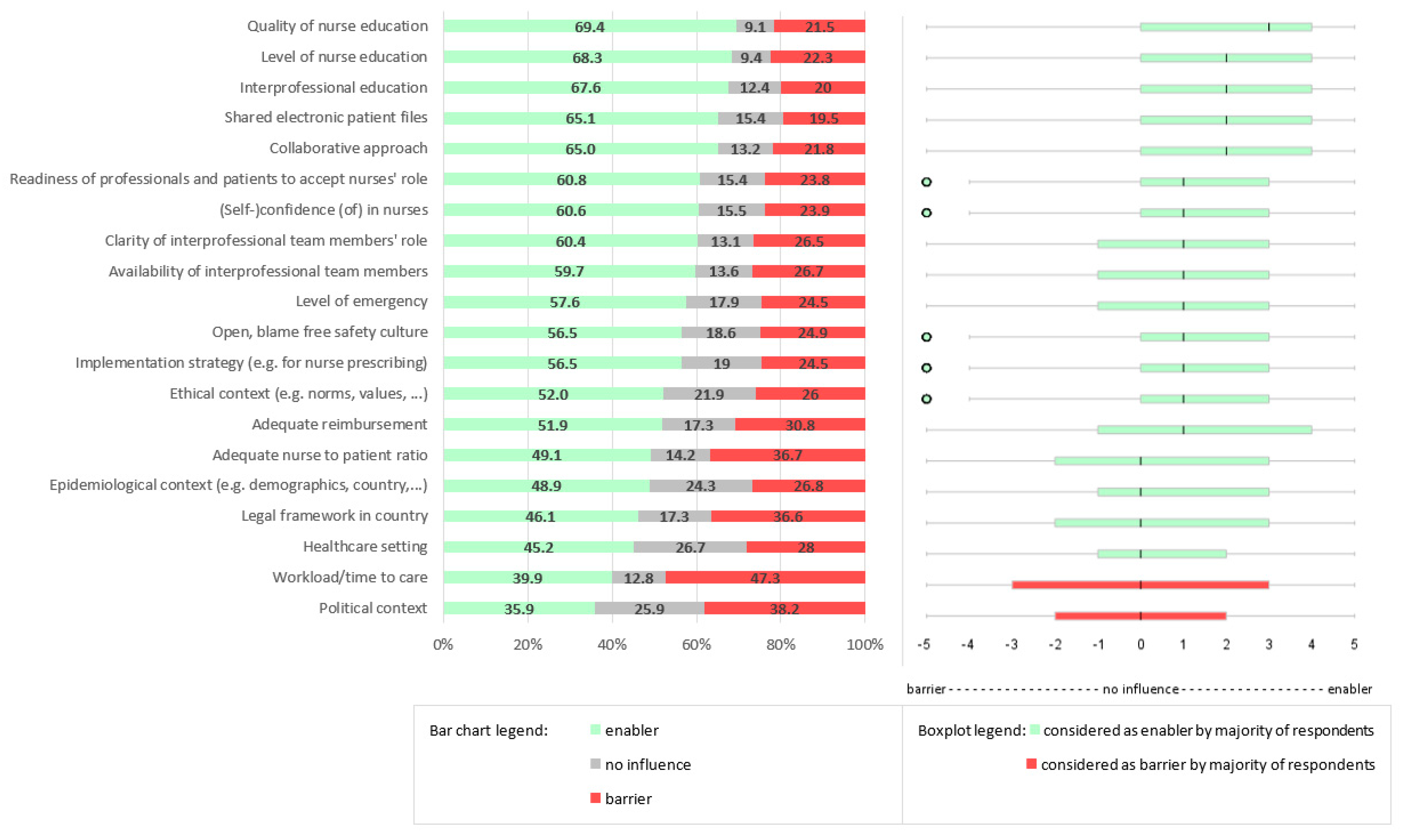
3.4. Contextual Factors of Nurses’ Role in Current Interprofessional PC
4. Discussion
4.1. Implications for Clinical Practice, Research, Education, and Policy
4.2. Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Management of Therapeutic and Adverse Effects (n = 734) | Management of Medicines Adherence (n = 796) | Management of Medication Self-Management (n = 726) | Management of Patient Education and Information (n = 731) | Prescription Management (n = 669) | Medication Safety Management (n = 738) | (Transition of) Care Coordination (n = 711) | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Task number | Nurses (n = 486) | Physicians (n = 133) | Pharmacists (n = 115) | * If p < 0.05 | Nurses (n = 513) | Physicians (n = 136) | Pharmacists (n = 101) | * If p < 0.05 | Nurses (n = 487) | Physicians (n = 141) | Pharmacists (n = 103) | * If p < 0.05 | Nurses (n = 449) | Physicians (n = 133) | Pharmacists (n = 115) | * If p < 0.05 | Nurses (n = 486) | Physicians (n = 127) | Pharmacists (n = 93) | * If p < 0.05 | Nurses (n = 494) | Physicians (n = 142) | Pharmacists (n = 102) | * If p < 0.05 | Nurses (n = 474) | Physicians (n = 135) | Pharmacists (n = 102) | * If p < 0.05 |
| 1 | 98.0 | 95.8 | 89.8 | * | 96.3 | 97.2 | 92.5 | 97.3 | 100 | 85.7 | * | 97.5 | 97.2 | 85.6 | * | 77.1 | 55.3 | 48.4 | * | 96.9 | 67.8 | 87.7 | * | 95.4 | 68.8 | 87.0 | * | |
| 2 | 95.5 | 95.6 | 91.2 | 95.4 | 97.7 | 94.2 | 98.0 | 98.6 | 89.1 | * | 97.0 | 97.2 | 83.7 | * | 80.3 | 55.6 | 47.8 | * | 97.2 | 65.1 | 85.7 | * | 95.7 | 68.1 | 87.5 | * | ||
| 3 | 96.3 | 98.5 | 90.2 | * | 97.5 | 97.8 | 93.1 | * | 97.6 | 99.3 | 90.5 | * | 97.2 | 97.9 | 89.6 | * | 82.1 | 86.4 | 68.9 | * | 96.8 | 95.1 | 88.6 | * | 95.9 | 95.7 | 88.7 | * |
| 4 | 96.9 | 93.9 | 85.7 | * | 96.8 | 98.5 | 81.5 | * | 97.4 | 97.1 | 85.4 | * | 80.8 | 86.6 | 53.1 | * | 96.7 | 93.8 | 81.6 | * | 96.0 | 92.1 | 81.2 | * | ||||
| 5 | 91.3 | 91.0 | 79.1 | * | 93.7 | 91.8 | 78.4 | * | 94.8 | 96.3 | 77.7 | * | 80.0 | 85.3 | 60.0 | * | 95.0 | 92.1 | 78.6 | * | 92.9 | 93.9 | 77.2 | * | ||||
| 6 | 94.1 | 93.9 | 83.9 | * | 95.2 | 97.1 | 85.0 | * | 96.1 | 96.5 | 82.9 | * | 95.0 | 97.2 | 86.8 | * | 78.9 | 88.5 | 69.4 | * | 96.2 | 91.7 | 85.8 | * | 94.5 | 93.6 | 82.5 | * |
| 7 | 94.9 | 87.6 | 82.0 | * | 94.3 | 92.1 | 81.5 | * | 93.9 | 94.0 | 83.2 | * | 94.3 | 93.9 | 79.8 | * | 76.3 | 83.6 | 54.5 | * | 94.2 | 89.9 | 77.1 | * | 93.9 | 89.1 | 83.8 | * |
| 8 | 84.7 | 79.1 | 73.9 | * | 88.0 | 83.8 | 70.5 | * | 88.4 | 85.5 | 73.5 | * | 90.1 | 87.9 | 71.4 | * | 67.3 | 75.2 | 36.7 | * | 87.5 | 81.9 | 65.3 | * | 86.3 | 80.9 | 71.6 | * |
| 9 | 94.0 | 91.3 | 86.1 | * | 95.3 | 95.5 | 86.9 | * | 96.3 | 97.2 | 85.0 | * | 95.5 | 97.9 | 83.7 | * | 79.7 | 90.6 | 66.3 | * | 95.2 | 95.0 | 89.4 | 95.3 | 92.1 | 85.6 | * | |
| 10 | 96.6 | 98.5 | 85.3 | * | ||||||||||||||||||||||||
| 11 | 96.8 | 96.2 | 89.8 | * | 95.2 | 96.5 | 88.3 | * | 95.3 | 97.9 | 82.5 | * | ||||||||||||||||
| 12 | 87.2 | 84.4 | 80.4 | 90.3 | 88.7 | 78.7 | * | 88.9 | 91.2 | 80.2 | * | 89.7 | 87.5 | 72.5 | * | 71.5 | 80.2 | 50 | * | 88.8 | 86.8 | 77.6 | * | 88.6 | 85.6 | 77.1 | * | |
| 13 | 85.4 | 64.9 | 63.2 | * | 88.9 | 63.6 | 68.5 | * | 88.1 | 92.0 | 72.0 | * | 88.6 | 88.8 | 63.4 | * | 69.1 | 81.4 | 47.9 | * | 88.9 | 85.6 | 62.5 | * | 89.2 | 65.9 | 71.8 | * |
| 14 | 96.3 | 69.5 | 80.0 | * | 97.5 | 96.2 | 88.1 | * | 97.0 | 97.1 | 84.3 | * | 97.8 | 97.2 | 82.7 | * | 96.4 | 93.0 | 85.6 | * | 95.6 | 93.3 | 85.4 | * | ||||
| 15 | 93.6 | 89.2 | 82.5 | * | 95.2 | 92.5 | 82.7 | * | 93.4 | 90.4 | 80.8 | * | 94.1 | 92.1 | 81.0 | * | 73.9 | 82.5 | 50.5 | * | 93.1 | 92.2 | 81.4 | * | 93.2 | 84.0 | 82.0 | * |
| 16 | 53.8 | 40.6 | 26.9 | * | ||||||||||||||||||||||||
| 17 | 57.1 | 38.1 | 27.7 | * | ||||||||||||||||||||||||
| 18 | 55.2 | 39.0 | 28.1 | * | ||||||||||||||||||||||||
| 19 | 57.0 | 35.2 | 26.9 | * | ||||||||||||||||||||||||
| 20 | 64.8 | 54.0 | 43.0 | * | ||||||||||||||||||||||||
| 21 | 68.5 | 59.4 | 38.3 | * | ||||||||||||||||||||||||
| 22 | 66.0 | 49.2 | 43.7 | * | ||||||||||||||||||||||||
| 23 | 77.8 | 65.2 | 45.7 | * | 94.8 | 94.6 | 85.4 | * | ||||||||||||||||||||
| 24 | 88.4 | 90.2 | 76.0 | * | ||||||||||||||||||||||||
| 25 | 90.6 | 90.2 | 84.7 | * | 94.2 | 92.4 | 86.5 | * | 94.3 | 92.2 | 86.4 | * | 92.9 | 94.2 | 79.8 | * | 78.6 | 68.2 | 55.4 | * | 92.8 | 93.5 | 85.7 | * | 91.8 | 93.3 | 84.7 | * |
| 26 | 95.3 | 86.6 | 86.8 | * | 93.8 | 93.8 | 85.1 | * | 92.3 | 97.7 | 82.8 | * | 94.3 | 95.6 | 83 | * | 75.9 | 66.7 | 53.7 | * | 92.3 | 94.3 | 85.6 | * | 92.7 | 93.2 | 84.8 | * |
| Restrictions | All % (n) | Physicians % (n) | Pharmacists % (n) | Nurses % (n) | p-Value |
|---|---|---|---|---|---|
| Only after specific training | 60.9 (325) | 57.6 (38) | 78.7 (37) | 59.1 (247) | 0.028 |
| Only a restricted list of medicines | 54.1 (289) | 62.1 (41) | 57.4 (27) | 52.9 (221) | 0.34 |
| Only in a specific context, pathology/specialisation | 43.3 (231) | 51.5 (34) | 51.1 (24) | 40.9 (171) | 0.14 |
| Only within individual patient clinical management plan | 36.3 (194) | 47.0 (31) | 46.8 (22) | 33.5 (140) | 0.032 |
| Only low risk medicines | 31.1 (166) | 28.8 (19) | 44.7 (21) | 29.9 (125) | 0.106 |
| Only long-term chronic medicines | 30.3 (162) | 39.4 (26) | 51.1 (24) | 26.8 (112) | 0.001 |
| Only in emergency | 23.2 (124) | 25.8 (17) | 17.0 (8) | 23.7 (99) | 0.524 |
| Prescription-only medicines only | 19.1 (102) | 18.2 (12) | 19.1 (9) | 19.4 (81) | 0.974 |
| No restrictions | 6.8 (39) | 2.9 (2) | 4.1 (2) | 7.7 (35) | 0.251 |
| Other | 1.7 (9) | 4.5 (3) | 0 | 1.4 (6) | 0.123 |
 |  |  |  |  |  |  |  |  |  |  |  |  |  | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Belgium n = 710 * | Czech Republic n = 233 * | Germany n = 48 * | Greece n = 218 * | Hungary n = 24 * | Italy n = 676 * | The Nether-lands n = 54 * | North Macedo-nia n = 75 * | Norway n = 50 * | Portugal n = 64 * | Slovakia n = 691 * | Slovenia n = 400 * | Spain n = 337 * | Wales + England n = 107 * | ||
| T1 | 97.4 | 93.3 | 94.6 | 98.6 | 75.9 | 98.1 | 98.7 | 88.0 | 100 | 100 | 83.4 | 93.3 | 93.9 | 93.9 | <0.001 |
| T2 | 95.9 | 95.4 | 88.7 | 97.4 | 77.8 | 98.1 | 100 | 87.7 | 100 | 100 | 85.4 | 93.3 | 93.0 | 92.1 | <0.001 |
| T3 | 95.5 | 95.8 | 94.4 | 96.6 | 77.8 | 98.9 | 96.8 | 87.3 | 100 | 100 | 97.9 | 92.2 | 94.4 | 94.5 | <0.001 |
| T4 | 92.5 | 94.1 | 97.7 | 97.3 | 78.3 | 98.4 | 100 | 82.6 | 100 | 100 | 94.5 | 91.9 | 93.4 | 96.3 | <0.001 |
| T5 | 85.0 | 92.0 | 95.3 | 96.8 | 77.3 | 97.1 | 86.1 | 70.5 | 100 | 100 | 93.1 | 88.8 | 90.8 | 91.6 | <0.001 |
| T6 | 88.8 | 92.2 | 98.0 | 98.2 | 76.0 | 95.2 | 98.1 | 90.8 | 100 | 100 | 99.0 | 88.8 | 92.0 | 94.9 | <0.001 |
| T7 | 83.6 | 92.0 | 93.5 | 96.1 | 76.9 | 96.0 | 98.0 | 80.3 | 93.8 | 100 | 96.8 | 87.8 | 91.6 | 95.2 | <0.001 |
| T8 | 69.9 | 93.8 | 71.4 | 88.2 | 73.1 | 92.6 | 90.4 | 64.9 | 97.1 | 97.0 | 86.7 | 85.5 | 84.0 | 88.2 | <0.001 |
| T9 | 90.8 | 95.9 | 90.6 | 93.1 | 69.2 | 97.3 | 98.4 | 87.2 | 100 | 100 | 97.5 | 90.1 | 90.2 | 97.6 | <0.001 |
| T10 | 96.1 | 90.9 | 97.9 | 98.5 | 96.6 | 89.2 | 94.1 | <0.001 | |||||||
| T11 | 95.6 | 94.7 | 96.6 | 91.5 | 97.6 | 96.8 | 78.9 | 100 | 100 | 98.6 | 89.5 | 91.6 | 90.7 | <0.001 | |
| T12 | 74.8 | 90.1 | 63.6 | 93.5 | 70.8 | 95.7 | 89.4 | 72.2 | 91.9 | 100 | 90.4 | 86.8 | 85.7 | 89.0 | <0.001 |
| T13 | 77.1 | 90.4 | 90.4 | 92.6 | 69.6 | 96.9 | 96.7 | 82.4 | 100 | 100 | 65.5 | 84.2 | 84.6 | 80.0 | <0.001 |
| T14 | 93.1 | 95.9 | 98.0 | 96.6 | 76.9 | 97.2 | 100 | 93.4 | 100 | 100 | 92.8 | 88.1 | 93.2 | 96.0 | <0.001 |
| T15 | 85.4 | 92.2 | 94.0 | 96.6 | 76.9 | 94.7 | 100 | 83.6 | 100 | 100 | 96.8 | 96.0 | 90.1 | 87.1 | <0.001 |
| T23 | 90.2 | 88.4 | 97.6 | 97.1 | 97.9 | 90.0 | 95.7 | <0.001 | |||||||
| T24 | 81.6 | 80.0 | 97.6 | 94.2 | 88.3 | 78.8 | 82.8 | <0.001 | |||||||
| T25 | 85.5 | 91.9 | 94.0 | 93.8 | 75.0 | 95.6 | 100 | 87.2 | 98.1 | 100 | 94.7 | 87.7 | 90.9 | 94.8 | <0.001 |
| T26 | 89.6 | 92.3 | 95.8 | 95.6 | 76.0 | 93.8 | 100 | 84.8 | 100 | 100 | 95.3 | 87.9 | 89.0 | 95.0 | <0.001 |
 |  |  |  |  |  |  | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Belgium n = 134 | Czech Republic n = 38 | Greece n = 43 | Italy n = 130 | Slovakia n = 127 | Slovenia n = 74 | Spain n = 64 | ||
| T1 | 76.3 | 77.5 | 81.8 | 85.1 | 15.4 | 81.6 | 81.8 | <0.001 |
| T2 | 79.5 | 81.8 | 86.4 | 87.8 | 17.3 | 83.3 | 82.4 | <0.001 |
| T3 | 79.4 | 80.0 | 86.0 | 93.0 | 64.8 | 82.2 | 89.4 | <0.001 |
| T4 | 76.1 | 74.4 | 88.4 | 91.5 | 56.2 | 81.6 | 83.3 | <0.001 |
| T5 | 71.5 | 71.8 | 88.4 | 91.5 | 64.6 | 81.6 | 80.3 | <0.001 |
| T6 | 70.1 | 76.3 | 88.6 | 87.7 | 71.4 | 75.8 | 80.3 | <0.001 |
| T7 | 62.1 | 66.7 | 87.8 | 89.2 | 63.5 | 78.4 | 82.0 | <0.001 |
| T8 | 47.6 | 68.6 | 75.0 | 84.1 | 46.0 | 78.4 | 68.8 | <0.001 |
| T9 | 77.8 | 74.4 | 84.4 | 90.7 | 65.9 | 82.4 | 85.7 | <0.001 |
| T12 | 57.9 | 67.6 | 85.4 | 86.6 | 48.0 | 80.8 | 82.0 | <0.001 |
| T13 | 60.0 | 66.7 | 86.0 | 89.3 | 42.6 | 73.3 | 71.0 | <0.001 |
| T15 | 70.7 | 69.2 | 88.9 | 86.0 | 50.0 | 81.3 | 67.7 | <0.001 |
| T16 | 30.7 | 53.3 | 72.1 | 78.0 | 11.1 | 51.4 | 65.6 | <0.001 |
| 117 | 37.7 | 55.8 | 68.9 | 77.1 | 12.5 | 51.4 | 65.1 | <0.001 |
| T18 | 39.7 | 52.3 | 66.7 | 76.6 | 11.1 | 52.1 | 58.7 | <0.001 |
| T19 | 39.4 | 60.5 | 62.8 | 75.4 | 10.2 | 50.0 | 66.7 | <0.001 |
| T20 | 79.0 | 61.1 | 76.2 | 79.8 | 14.0 | 49.3 | 67.7 | <0.001 |
| T21 | 75.4 | 75.7 | 76.2 | 82.0 | 21.5 | 53.4 | 75.0 | <0.001 |
| T22 | 56.6 | 61.5 | 67.4 | 77.3 | 13.3 | 76.3 | 82.1 | <0.001 |
| T23 | 78.2 | 70.0 | 88.6 | 92.2 | 18.4 | 81.6 | 81.5 | <0.001 |
| T25 | 73.2 | 77.8 | 90.7 | 91.4 | 31.8 | 84.9 | 85.7 | <0.001 |
| T26 | 75.4 | 66.7 | 90.2 | 85.2 | 33.6 | 81.7 | 80.6 | <0.001 |
| Management of Therapeutic and Adverse Effects (n = 336) | Management of Medicines Adherence (n = 356) | Management of Medication self-Management (n = 338) | Management of Patient Education (n = 328) | Prescription Management (n = 250) | Medication Safety Management (n = 335) | (Transition of) Care Coordination (n = 311) | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Task Number | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse | Level 5 Nurse | Level 6 Nurse | Level 7 Nurse | Level 8 Nurse |
| 1 | 98.6 | 99.7 | 100 | 100 | 99.7 | 100 | 99.7 | 100 | 99.7 | 100 | 99.7 | 100 | 98.9 | 100 | 100 | 100 | 95.0 | 98.6 | 99.3 | 99.6 | 99.2 | 99.7 | 100 | 100 | 99.1 | 99.4 | 100 | 99.7 |
| 2 | 99.1 | 100 | 100 | 100 | 99.2 | 100 | 99.7 | 100 | 99.4 | 100 | 99.7 | 100 | 99.4 | 100 | 100 | 100 | 96.0 | 98.2 | 99.6 | 99.6 | 99.4 | 100 | 100 | 100 | 99.7 | 99.1 | 99.7 | 99.4 |
| 3 | 98.9 | 100 | 100 | 100 | 98.6 | 100 | 99.7 | 100 | 99.2 | 100 | 99.7 | 100 | 99.4 | 100 | 100 | 100 | 97.5 | 97.9 | 99.6 | 99.6 | 99.7 | 100 | 100 | 100 | 99.7 | 99.1 | 99.7 | 99.4 |
| 4 | 98.0 | 100 | 100 | 100 | 98.4 | 99.7 | 99.5 | 99.7 | 98.9 | 99.7 | 99.4 | 100 | 95.8 | 97.9 | 100 | 100 | 98.9 | 99.5 | 99.4 | 99.7 | 98.1 | 99.4 | 99.7 | 99.4 | ||||
| 5 | 97.3 | 99.1 | 100 | 100 | 96.2 | 99.2 | 99.4 | 99.7 | 98.2 | 100 | 99.4 | 99.7 | 96.0 | 97.9 | 99.6 | 100 | 98.5 | 99.1 | 99.7 | 99.7 | 98.1 | 99.1 | 99.7 | 99.3 | ||||
| 6 | 97.9 | 99.4 | 99.7 | 100 | 97.8 | 99.2 | 99.7 | 100 | 97.4 | 99.7 | 99.4 | 99.7 | 97.9 | 100 | 100 | 100 | 96.0 | 98.6 | 100 | 100 | 98.6 | 99.7 | 100 | 100 | 98.1 | 99.4 | 100 | 99.7 |
| 7 | 94.7 | 97.9 | 99.4 | 100 | 96.4 | 98.0 | 99.7 | 100 | 96.9 | 99.1 | 99.7 | 100 | 95.9 | 99.4 | 100 | 100 | 93.6 | 97.7 | 100 | 100 | 96.6 | 98.8 | 100 | 100 | 97.0 | 98.4 | 99.3 | 99.0 |
| 8 | 95.7 | 99.4 | 99.7 | 99.7 | 93.1 | 97.0 | 98.2 | 99.4 | 97.7 | 99.0 | 99.7 | 100 | 96.7 | 100 | 100 | 100 | 90.0 | 96.6 | 99.2 | 99.6 | 96.3 | 98.7 | 98.7 | 99.3 | 95.4 | 97.2 | 99.3 | 98.9 |
| 9 | 98.0 | 100 | 100 | 100 | 98.1 | 100 | 99.7 | 100 | 99.2 | 100 | 99.4 | 100 | 99.1 | 100 | 100 | 100 | 95.4 | 98.6 | 100 | 100 | 98.8 | 100 | 100 | 100 | 98.8 | 99.7 | 100 | 99.7 |
| 10 | 98.4 | 100 | 99.7 | 100 | ||||||||||||||||||||||||
| 11 | 97.5 | 99.7 | 99.7 | 100 | 98.8 | 99.4 | 99.4 | 99.7 | 98.5 | 99.7 | 100 | 100 | ||||||||||||||||
| 12 | 95.5 | 97.2 | 99.4 | 100 | 93.5 | 98.8 | 99.7 | 100 | 96.7 | 98.4 | 99.0 | 100 | 95.9 | 99.3 | 100 | 100 | 93.1 | 95.9 | 99.6 | 100 | 96.0 | 99.3 | 100 | 100 | 95.2 | 98.0 | 99.0 | 99.3 |
| 13 | 95.3 | 98.2 | 100 | 100 | 97.0 | 98.5 | 99.4 | 99.7 | 97.3 | 99.0 | 99.7 | 100 | 97.6 | 98.7 | 99.7 | 99.7 | 93.7 | 98.1 | 99.6 | 100 | 96.5 | 99.4 | 100 | 100 | 96.2 | 99.0 | 99.7 | 99.3 |
| 14 | 98.5 | 99.7 | 100 | 100 | 97.8 | 99.5 | 99.7 | 100 | 98.6 | 99.7 | 99.7 | 100 | 98.9 | 99.4 | 100 | 100 | 98.0 | 99.4 | 100 | 100 | 98.8 | 98.8 | 100 | 99.7 | ||||
| 15 | 95.6 | 98.8 | 99.7 | 99.7 | 96.5 | 99.2 | 99.4 | 100 | 98.7 | 99.7 | 99.7 | 100 | 96.6 | 99.7 | 100 | 100 | 91.4 | 96.6 | 100 | 100 | 98.2 | 100 | 100 | 100 | 93.2 | 84.0 | 82.0 | 99.3 |
| 16 | 83.3 | 90.2 | 96.4 | 98.9 | ||||||||||||||||||||||||
| 17 | 82.1 | 91.3 | 96.1 | 98.0 | ||||||||||||||||||||||||
| 18 | 80.2 | 89.1 | 96.0 | 97.5 | ||||||||||||||||||||||||
| 19 | 84.4 | 90.1 | 97.0 | 98.5 | ||||||||||||||||||||||||
| 20 | 89.3 | 99.1 | 98.7 | |||||||||||||||||||||||||
| 21 | 91.4 | 95.8 | 99.2 | 99.1 | ||||||||||||||||||||||||
| 22 | 89.2 | 93.6 | 98.3 | 98.7 | ||||||||||||||||||||||||
| 23 | 93.6 | 97.2 | 100 | 99.6 | 96.8 | 99.4 | 100 | 100 | ||||||||||||||||||||
| 24 | 94.1 | 97.3 | 99.0 | 99.0 | ||||||||||||||||||||||||
| 25 | 95.4 | 99.4 | 100 | 100 | 97.1 | 99.1 | 99.7 | 100 | 98.2 | 99.7 | 99.7 | 100 | 97.8 | 99.7 | 100 | 100 | 94.7 | 97.0 | 100 | 100 | 97.8 | 99.7 | 99.6 | 99.7 | 96.1 | 99.0 | 100 | 99.7 |
| 26 | 93.3 | 98.2 | 99.7 | 100 | 94.2 | 98.8 | 99.4 | 100 | 95.9 | 99.4 | 99.4 | 99.7 | 95.2 | 99.4 | 100 | 100 | 91.7 | 95.4 | 99.6 | 100 | 96.3 | 99.1 | 99.7 | 99.7 | 95.3 | 98.7 | 100 | 99.7 |
References
- Institute of Medicine Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System; National Academies Press (US): Washington, DC, USA, 2000. [Google Scholar] [CrossRef]
- Dilles, T.; Stichele, R.H.V.; Van Bortel, L.M.; Elseviers, M.M. The Development and Test of an Intervention to Improve ADR Screening in Nursing Homes. J. Am. Med. Dir. Assoc. 2013, 14, 379.e1–379.e6. [Google Scholar] [CrossRef]
- Parretta, E.; Rafaniello, C.; Magro, L.; Pittoni, A.C.; Sportiello, L.; Ferrajolo, C.; Mascolo, A.; Sessa, M.; Rossi, F.; Capuano, A. Improvement of patient adverse drug reaction reporting through a community pharmacist-based intervention in the Campania region of Italy. Expert Opin. Drug Saf. 2014, 13, 21–29. [Google Scholar] [CrossRef]
- Lopez-Gonzalez, E.; Herdeiro, M.T.; Piñeiro-Lamas, M.; Figueiras, A. Effect of An Educational Intervention to Improve Adverse Drug Reaction Reporting in Physicians: A Cluster Randomized Controlled Trial. Drug Saf. 2015, 38, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Banner, T.; Gabe-Walters, M.; Mikhail, J.M.; Panes, G.; Round, J.; Snelgrove, S.; Storey, M.; Hughes, D. Nurse-led medicines’ monitoring in care homes, implementing the Adverse Drug Reaction (ADRe) Profile improvement initiative for mental health medicines: An observational and interview study. PLoS ONE 2019, 14, e0220885. [Google Scholar] [CrossRef]
- Dürr, P.; Schlichtig, K.; Kelz, C.; Deutsch, B.; Maas, R.; Eckart, M.J.; Wilke, J.; Wagner, H.; Wolff, K.; Preuß, C.; et al. The Randomized AMBORA Trial: Impact of Pharmacological/Pharmaceutical Care on Medication Safety and Patient-Reported Outcomes During Treatment with New Oral Anticancer Agents. J. Clin. Oncol. 2021, 39, 1983–1994. [Google Scholar] [CrossRef]
- WHO Global Patient Safety Challenge: Medication Without Harm; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/initiatives/medication-without-harm (accessed on 11 May 2021).
- Lehnbom, E.C.; Stewart, M.J.; Manias, E.; Westbrook, J. Impact of Medication Reconciliation and Review on Clinical Outcomes. Ann. Pharmacother. 2014, 48, 1298–1312. [Google Scholar] [CrossRef]
- Bergqvist, M.; Ulfvarson, J.; Karlsson, E.A. Nurse-led medication reviews and the quality of drug treatment of elderly hospitalized patients. Eur. J. Clin. Pharmacol. 2009, 65, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Leguelinel-Blache, G.; Arnaud, F.; Bouvet, S.; Dubois, F.; Castelli, C.; Roux-Marson, C.; Ray, V.; Sotto, A.; Kinowski, J.-M. Impact of admission medication reconciliation performed by clinical pharmacists on medication safety. Eur. J. Intern. Med. 2014, 25, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Scullin, C.; Scott, M.; Hogg, A.; McElnay, J.C. An innovative approach to integrated medicines management. J. Eval. Clin. Pract. 2007, 13, 781–788. [Google Scholar] [CrossRef]
- Pomare, C.; Long, J.C.; Churruca, K.; Ellis, L.A.; Braithwaite, J. Interprofessional collaboration in hospitals: A critical, broad-based review of the literature. J. Interprof. Care 2020, 34, 509–519. [Google Scholar] [CrossRef]
- Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010; Available online: http://apps.who.int/iris/bitstream/handle/10665/70185/WHO_HRH_HPN_10.3_eng.pdf;jsessionid=A5FAE753BE7A2DCB751B601E3254463A?sequence=1 (accessed on 11 May 2021).
- Köberlein-Neu, J.; Mennemann, H.; Hamacher, S.; Waltering, I.; Jaehde, U.; Schaffert, C.; Rose, O. Interprofessional Medication Management in Patients with Multiple Morbidities. Dtsch. Aerzteblatt Int. 2016, 113, 741–748. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Sugaya, N.; Saigusa, Y.; Inamori, M. Effect of interprofessional collaboration among nursing home professionals on end-of-life care in nursing homes. Drug Discov. Ther. 2021, 15, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 6, CD000072. [Google Scholar] [CrossRef]
- Global Forum on Innovation in Health Professional Education; Board on Global Health; Institute of Medicine. Interprofessional Education for Collaboration: Learning How to Improve Health from Interprofessional Models Across the Continuum of Education to Practice: Workshop Summary; National Academies Press: Washington, DC, USA, 2013. [Google Scholar]
- Makowsky, M.J.; Schindel, T.J.; Rosenthal, M.; Campbell, K.; Tsuyuki, R.T.; Madill, H.M. Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting. J. Interprof. Care 2009, 23, 169–184. [Google Scholar] [CrossRef]
- Donovan, A.L.; Aldrich, J.M.; Gross, A.K.; Barchas, D.M.; Thornton, K.C.; Schell-Chaple, H.M.; Gropper, M.A.; Lipshutz, A.K.M. Interprofessional Care and Teamwork in the ICU. Crit. Care Med. 2018, 46, 980–990. [Google Scholar] [CrossRef]
- Choo, J.; Hutchinson, A.; Bucknall, T. Nurses’ role in medication safety. J. Nurs. Manag. 2010, 18, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Thoma, J.E.; Waite, M.A. Experiences of nurse case managers within a central discharge planning role of collaboration between physicians, patients and other healthcare professionals: A sociocultural qualitative study. J. Clin. Nurs. 2018, 27, 1198–1208. [Google Scholar] [CrossRef] [PubMed]
- Lillebo, B.; Faxvaag, A. Continuous interprofessional coordination in perioperative work: An exploratory study. J. Interprof. Care 2015, 29, 125–130. [Google Scholar] [CrossRef]
- Van Leijen-Zeelenberg, J.E.; Van Raak, A.J.A.; Duimel-Peeters, I.G.P.; Kroese, M.E.A.L.; Brink, P.R.G.; Vrijhoef, H. Interprofessional communication failures in acute care chains: How can we identify the causes? J. Interprof. Care 2015, 29, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Suter, E.; Arndt, J.; Arthur, N.; Parboosingh, J.; Taylor, E.; Deutschlander, S. Role understanding and effective communication as core competencies for collaborative practice. J. Interprof. Care 2009, 23, 41–51. [Google Scholar] [CrossRef]
- Brault, I.; Kilpatrick, K.; D’Amour, D.; Contandriopoulos, D.; Chouinard, V.; Dubois, C.-A.; Perroux, M.; Beaulieu, M.-D. Role Clarification Processes for Better Integration of Nurse Practitioners into Primary Healthcare Teams: A Multiple-Case Study. Nurs. Res. Pract. 2014, 2014, 17051. [Google Scholar] [CrossRef]
- Ensing, H.T.; Stuijt, C.C.; Bemt, B.J.V.D.; Van Dooren, A.A.; Karapinar-Çarkit, F.; Koster, E.S.; Bouvy, M.L. Identifying the Optimal Role for Pharmacists in Care Transitions: A Systematic Review. J. Manag. Care Spéc. Pharm. 2015, 21, 614–636. [Google Scholar] [CrossRef]
- Borrott, N.; Kinney, S.; Newall, F.; Williams, A.; Cranswick, N.; Wong, I.; Manias, E. Medication communication between nurses and doctors for paediatric acute care: An ethnographic study. J. Clin. Nurs. 2017, 26, 1978–1992. [Google Scholar] [CrossRef] [PubMed]
- Rosemann, T.; Joest, K.; Körner, T.; Schaefert, R.; Heiderhoff, M.; Szecsenyi, J. How can the practice nurse be more involved in the care of the chronically ill? The perspectives of GPs, patients and practice nurses. BMC Fam. Pract. 2006, 7, 14. [Google Scholar] [CrossRef][Green Version]
- Pullon, S.; McKinlay, E.; Stubbe, M.; Todd, L.; Badenhorst, C. Patients’ and health professionals’ perceptions of teamwork in primary care. J. Prim. Health Care 2011, 3, 128–135. [Google Scholar] [CrossRef]
- Jaruseviciene, L.; Liseckiene, I.; Valius, L.; Kontrimiene, A.; Jarusevicius, G.; Lapão, L.V. Teamwork in primary care: Perspectives of general practitioners and community nurses in Lithuania. BMC Fam. Pract. 2013, 14, 118. [Google Scholar] [CrossRef] [PubMed]
- Vedel, I.; Ghadi, V.; De Stampa, M.; Routelous, C.; Bergman, H.; Ankri, J.; Lapointe, L. Diffusion of a collaborative care model in primary care: A longitudinal qualitative study. BMC Fam. Pract. 2013, 14, 3. [Google Scholar] [CrossRef]
- Orchard, C.; Stevenson, K.; Bassendowski, S. A National Interprofessional Competency Framework: Canadian Interprofessional Health Collaborative; University of British Columbia: Vancouver, BC, Canada, 2010; Available online: https://www.academia.edu/25496437/A_National_Interprofessional_Competency_Framework (accessed on 31 March 2021).
- De Baetselier, E.; Van Rompaey, B.; Batalha, L.M.; Bergqvist, M.; Czarkowska-Paczek, B.; De Santis, A.; Dijkstra, N.E.; Fernandes, M.I.; Filov, I.; Grøndahl, V.A.; et al. EUPRON: Nurses’ practice in interprofessional pharmaceutical care in Europe. A cross-sectional survey in 17 countries. BMJ Open 2020, 10, e036269. [Google Scholar] [CrossRef] [PubMed]
- De Baetselier, E.; Dilles, T.; Batalha, L.M.; Dijkstra, N.E.; Fernandes, M.I.; Filov, I.; Friedrichs, J.; Grondahl, V.A.; Heczkova, J.; Helgesen, A.K.; et al. Perspectives of nurses’ role in interprofessional pharmaceutical care across 14 European countries: A qualitative study in pharmacists, physicians and nurses. PLoS ONE 2021, 16, e0251982. [Google Scholar] [CrossRef]
- De Baetselier, E.; Dilles, T.; Feyen, H.; Haegdorens, F.; Mortelmans, L.; Van Rompaey, B. Nurses’ responsibilities and tasks in pharmaceutical care: A scoping review. Nurs. Open 2021, 8. [Google Scholar] [CrossRef]
- Dossey, B.M. Florence Nightingale: A 19th-century mystic. J. Holist. Nurs. 2010, 28, 10–35. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Initiative, F.T.S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Charan, J.; Biswas, T. How to calculate sample size for different study designs in medical research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef]
- Allemann, S.; van Mil, F.; Botermann, L.; Berger, K.; Griese, N.; Hersberger, K.E. Pharmaceutical Care: The PCNE definition 2013. Int. J. Clin. Pharm. 2014, 36, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Hepler, C.D.; Strand, L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Hosp. Pharm. 1990, 47, 533–543. [Google Scholar] [CrossRef]
- Kijlstra, N.; Ridge, K.; Walser, S. Pharmaceutical Care: Where Do We Stand—Where Should We Go? Key Concepts in Pharmaceutical Care, Quality Assessment of Pharmaceutical Care in Europe, Sources of Information: Survey Report; European Directorate for the Quality of Medicines & HealthCare (EDQM): Strasbourg, France, 2009. [Google Scholar]
- Keitel, S. Pharmaceutical Care—Policies and Practices for a Safer, More Responsible and Cost-Effective Health System; European Directorate for the Quality of Medicines & HealthCare (EDQM): Strassbourg, France, 2012. [Google Scholar]
- European Qualifications Framework (EQF). Available online: https://www.cedefop.europa.eu/en/events-and-projects/projects/european-qualifications-framework-eqf (accessed on 18 February 2021).
- Cope, L.C.; Abuzour, A.S.; Tully, M. Nonmedical prescribing: Where are we now? Ther. Adv. Drug Saf. 2016, 7, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Review of Prescribing, Supply and Administration of Medicines. Final Report (Crown II Report); Department of Health: London, UK, 1999. Available online: https://www.publichealth.hscni.net/sites/default/files/directorates/files/Review%20of%20prescribing,%20supply%20and%20administration%20of%20medicines.pdf (accessed on 2 April 2021).
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Celio, J.; Ninane, F.; Bugnon, O.; Schneider, M.P. Pharmacist-nurse collaborations in medication adherence-enhancing interventions: A review. Patient Educ. Couns. 2018, 101, 1175–1192. [Google Scholar] [CrossRef]
- Khan, A.N.; Khan, M.U.; Shoaib, M.H.; Yousuf, R.I.; Mir, S.A. Practice Nurses and Pharmacists: A Perspective on the Expectation and Experience of Nurses for Future Collaboration. Oman. Med. J. 2014, 29, 271–275. [Google Scholar] [CrossRef]
- While, A.; Shah, R.; Nathan, A. Interdisciplinary working between community pharmacists and community nurses: The views of community pharmacists. J. Interprof. Care 2005, 19, 164–170. [Google Scholar] [CrossRef]
- Krautscheid, L.C. Defining Professional Nursing Accountability: A Literature Review. J. Prof. Nurs. 2014, 30, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Hoeve, Y.T.; Jansen, G.; Roodbol, P. The nursing profession: Public image, self-concept and professional identity. A discussion paper. J. Adv. Nurs. 2014, 70, 295–309. [Google Scholar] [CrossRef]
- Zamanzadeh, V.; Roshangar, F.; Fathi-Azar, E.; Valizadeh, L.; Kirkwood, J. Experiences of Newly Graduated Nurses on Strategies of Gaining Self-Confidence during Their Initial Work: A qualitative study. J. Nurs. Res. 2014, 22, 283–291. [Google Scholar] [CrossRef]
- Gurková, E.; Kalánková, D.; Kurucová, R.; Žiaková, K. Assessment of patient safety climate by nurses in Slovak Public and private hospitals. J. Nurs. Manag. 2020, 28, 1644–1652. [Google Scholar] [CrossRef] [PubMed]
- Sims, S.; Hewitt, G.; Harris, R. Evidence of a shared purpose, critical reflection, innovation and leadership in interprofessional healthcare teams: A realist synthesis. J. Interprof. Care 2015, 29, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Foronda, C.; MacWilliams, B.; McArthur, E. Interprofessional communication in healthcare: An integrative review. Nurse Educ. Pract. 2016, 19, 36–40. [Google Scholar] [CrossRef]
- Aiken, L.H. Educational Levels of Hospital Nurses and Surgical Patient Mortality. JAMA 2003, 290, 1617–1623. [Google Scholar] [CrossRef]
- Kroezen, M.; Francke, A.L.; Groenewegen, P.; van Dijk, L. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: A survey on forces, conditions and jurisdictional control. Int. J. Nurs. Stud. 2012, 49, 1002–1012. [Google Scholar] [CrossRef]
- Maier, C.B. Nurse prescribing of medicines in 13 European countries. Hum. Resour. Health 2019, 17, 1–10. [Google Scholar] [CrossRef]
- Clark, C.E.; Smith, L.F.P.; Taylor, R.S.; Campbell, J. Nurse-led interventions used to improve control of high blood pressure in people with diabetes: A systematic review and meta-analysis. Diabet. Med. 2011, 28, 250–261. [Google Scholar] [CrossRef]
- Wallymahmed, M.E.; Morgan, C.; Gill, G.V.; Macfarlane, I.A. Nurse-led cardiovascular risk factor intervention leads to improvements in cardiovascular risk targets and glycaemic control in people with Type 1 diabetes when compared with routine diabetes clinic attendance. Diabet. Med. 2011, 28, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.H.; Eisert, S.L.; Everhart, R.M.; Durfee, M.J.; Moore, S.L.; Soria, S.; Stell, D.I.; Rice-Peterson, C.; MacKenzie, T.D.; Estacio, R.O. Nurse-run, telephone-based outreach to improve lipids in people with diabetes. Am. J. Manag. Care 2012, 18, 77–84. [Google Scholar]
- Houweling, S.T.; Kleefstra, N.; Van Hateren, K.J.; Groenier, K.H.; Jong, B.M.-D.; Bilo, H.J. Can diabetes management be safely transferred to practice nurses in a primary care setting? A randomised controlled trial. J. Clin. Nurs. 2011, 20, 1264–1272. [Google Scholar] [CrossRef]
- Courtenay, M.; Carey, N.; Stenner, K.; Lawton, S.; Peters, J. Patients’ views of nurse prescribing: Effects on care, concordance and medicine taking. Br. J. Dermatol. 2011, 164, 396–401. [Google Scholar] [CrossRef]
- Carey, N.; Stenner, K.; Courtenay, M. An exploration of how nurse prescribing is being used for patients with respiratory conditions across the east of England. BMC Health Serv. Res. 2014, 14, 1–13. [Google Scholar] [CrossRef]
- Fairall, L.; O Bachmann, M.; Lombard, C.; Timmerman, V.; Uebel, K.; Zwarenstein, M.; Boulle, A.; Georgeu, D.; Colvin, C.J.; Lewin, S.; et al. Task shifting of antiretroviral treatment from doctors to primary-care nurses in South Africa (STRETCH): A pragmatic, parallel, cluster-randomised trial. Lancet 2012, 380, 889–898. [Google Scholar] [CrossRef]
- Wilkinson, J.; Carryer, J.; Adams, J. Evaluation of a diabetes nurse specialist prescribing project. J. Clin. Nurs. 2013, 23, 2355–2366. [Google Scholar] [CrossRef] [PubMed]
- Cleary, M.; Kornhaber, R.; Sayers, J.; Gray, R. Mental health nurse prescribing: A qualitative, systematic review. Int. J. Ment. Health Nurs. 2017, 26, 541–553. [Google Scholar] [CrossRef] [PubMed]
- Council of Europe. Resolution CM/res(2020)3 on the Implementation of Pharmaceutical Care for the Benefit of Patients and Health Services. 2020. Available online: https://search.coe.int/cm/pages/result_details.aspx?objectid=09000016809cdf26 (accessed on 2 April 2021).
- Harvey, C.; Thompson, S.; Otis, E.; Willis, E. Nurses’ views on workload, care rationing and work environments. J. Nurs. Manag. 2020, 28, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Glinos, I.A. Health professional mobility in the European Union: Exploring the equity and efficiency of free movement. Health Policy 2015, 119, 1529–1536. [Google Scholar] [CrossRef] [PubMed]
- Lauxen, O.; Larsen, C.; Slotala, L. The international recruitment of nurses as a strategy for managing labour shortages in Germany: The case of Hesse. Bundesgesundheitsblatt Gesundh. Gesundh. 2019, 62, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Baron-Epel, O.; Kaplan, G.; Weinstein, R.; Green, M.S. Extreme and acquiescence bias in a bi-ethnic population. Eur. J. Public Health 2010, 20, 543–548. [Google Scholar] [CrossRef] [PubMed]


| Domain 1 * | Domain 2 * | Domain 3 * | Domain 4 * | Domain 5 * | Domain 6 * | Domain 7 * | ||
|---|---|---|---|---|---|---|---|---|
| Task 1 | Observation, documentation, registration, reporting | |||||||
| Task 2 | Assessing patients’ competences | |||||||
| Task 3 | Assessing & addressing patient/family needs | |||||||
| Task 4 | Recognising & preventing risks/complications/drug related problems | |||||||
| Task 5 | Identifying, reporting, addressing contra-indications/drug related problems | |||||||
| Task 6 | Follow-up | |||||||
| Task 7 | Evidence-based practice | |||||||
| Task 8 | Decision making | |||||||
| Task 9 | Communication/discussion with patient/family | |||||||
| Task 10 | Detection of non-adherence, drug abuse/misuse | |||||||
| Task 11 | Motivational interviewing | |||||||
| Task 12 | Inter/intraprofessional referrals | |||||||
| Task 13 | Facilitation of medication management | |||||||
| Task 14 | Self-care support & education of patients | |||||||
| Task 15 | Advice (to patient or other healthcare professional) | |||||||
| Task 16 | Determination of type/dosage | |||||||
| Task 17 | Initiation of medication (reactive/proactive) | |||||||
| Task 18 | Adaptation of dose, dose titration | |||||||
| Task 19 | Decision on continuation/cessation of medication | |||||||
| Task 20 | PRN/standing prescription renewal order | |||||||
| Task 21 | Medication reconciliation | |||||||
| Task 22 | Medication review | |||||||
| Task 23 | Intervention in case of emergency | |||||||
| Task 24 | Discharge planning, transition of care planning | |||||||
| Task 25 | Transitional care communication, inter/intraprofessional collaboration/communication including reporting, advising, informing, alerting and discussing | |||||||
| Task 26 | Mentoring colleagues | |||||||
| CONTEXTUAL FACTORS | ||||||||
| Level of emergency | Adequate nurse to patient ratio | |||||||
| Level of nurse education | Shared digital / electronic patient files and records | |||||||
| Quality of nurse education | Legal framework in a country | |||||||
| Interprofessional education | (Self-)confidence in nurses | |||||||
| Adequate reimbursement | Readiness of healthcare professionals and patients | |||||||
| Clarity of interprofessional team members’ role | Healthcare setting | |||||||
| Availability of interprofessional team members | Ethical context (e.g., norms, values, …) | |||||||
| Workload/time to care | Political context | |||||||
| Collaborative approach between nurses, pharmacists and physicians | Epidemiological context (e.g., demographics, patient needs, professional needs, …) | |||||||
| All (n = 1385) | Nurses (n = 923) | Physicians (n = 240) | Pharmacists (n = 199) | |
|---|---|---|---|---|
| Demographical Data | % of Total (n) | % | % | % |
| Country | ||||
| Slovakia | 18.8 (261) | 9.8 | 35.8 | 40.7 |
| Belgium | 18.2 (252) | 15.2 | 29.2 | 19.1 |
| Italy | 13.4 (186) | 15.4 | 16.3 | 2 |
| Slovenia | 11.0 (153) | 13.1 | 1.7 | 13.1 |
| Czech Republic | 9.3 (129) | 11.6 | 3.3 | 4.5 |
| Spain | 8.4 (117) | 10.7 | 4.6 | 3 |
| Greece | 7.6 (105) | 9.8 | 2.9 | 3.5 |
| United Kingdom (Wales + England) | 3.1 (43) | 3.7 | 1.3 | 2.5 |
| Republic of North Macedonia | 3.0 (41) | 3.6 | 1.7 | 1.5 |
| Portugal | 1.8 (25) | 1.7 | 1.3 | 3 |
| The Netherlands | 1.6 (22) | 1.3 | 0.8 | 3.5 |
| Germany | 1.5 (21) | 1.2 | 1.3 | 2.5 |
| Norway | 1.4 (20) | 2.1 | - | 0.5 |
| Hungary | 0.7 (10) | 1 | - | 0.5 |
| Gender | ||||
| Female | 73.0 (992) | 80.2 | 50 | 66.8 |
| Male | 26.8 (364) | 19.4 | 50 | 33.2 |
| Other | 0.1 (1) | 0.1 | - | - |
| Prefer not to say | 0.1 (2) | 0.2 | - | - |
| Age (years), mean (min-max) | 40.8 (18–71) | 40.5 (18–71) | 42.9 (25–69) | 38.7 (23–68) |
| Job Characteristics | ||||
| Work experience in HC (years), mean (min-max) | 17.5 (0.3–60) | 18.0 (0.5–60) | 17.1 (0.5–47) | 15.7 (0.3–45) |
| Work experience in HC (setting) † | ||||
| Hospital care | 74.7 (985) | 76.9 | 81.1 | 56.7 |
| Community or primary care | 26.6 (351) | 22.5 | 20.2 | 52.9 |
| Residential care | 17.1 (225) | 21.2 | 12.6 | 2.7 |
| Mental healthcare | 8.0 (106) | 10 | 3.8 | 4.3 |
| Current employment † | ||||
| Clinical practice | 83.2 (1078) | 81.7 | 85.8 | 86.7 |
| Education | 23.5 (304) | 26.8 | 18.8 | 14.4 |
| Research | 12.1 (157) | 9.6 | 22.6 | 10.8 |
| Policy making | 10.5 (136) | 10.7 | 11.7 | 8.2 |
| Educational Characteristics | ||||
| Highest level of nursing education (EQF) | Only nurses questioned | |||
| Level 5 | 24.9 | |||
| Level 6 | 42.1 | |||
| Level 7 | 26.6 | |||
| Level 8 | 6.4 |
| Level of Nurse Prescribing | All % (n) | Physicians % (n) | Pharmacists % (n) | Nurses % (n) | p-Value |
|---|---|---|---|---|---|
| No nurse prescribing | 36.1 (330) | 54.6 (83) | 58.1 (68) | 27.7 (176) | <0.001 |
| Dependent nurse prescribing | 47.9 (437) | 44.1 (67) | 37.6 (44) | 51.0 (324) | |
| Independent nurse prescribing | 16.0 (146) | 1.3 (2) | 4.3 (5) | 21.3 (135) |
 |  |  |  |  |  |  |  |  |  |  |  |  |  | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Belgium n = 622 * | Czech Republic n = 199 * | Germany n = 56 * | Greece n = 193 * | Hungary n = 29 * | Italy n = 595 * | The Netherlands n = 52 * | North Macedonia n = 52 * | Norway n = 72 * | Portugal n = 80 * | Slovakia n = 603 * | Slovenia n = 350 * | Spain n = 295 * | Wales + England n = 118 * | ||
| T1 | 94.7 | 91.5 | 89.9 | 96.3 | 74.2 | 96.3 | 97.5 | 87.3 | 98.4 | 98.8 | 73.4 | 91.8 | 92.2 | 94.7 | <0.001 |
| T2 | 93.8 | 94.0 | 86.2 | 95.9 | 75.9 | 96.6 | 100 | 86.5 | 98.4 | 98.8 | 76.5 | 92.0 | 91.5 | 92.5 | <0.001 |
| T3 | 93.4 | 94.1 | 90.8 | 95.2 | 75.9 | 98.1 | 96.9 | 82.0 | 100 | 98.8 | 93.6 | 90.9 | 93.7 | 93.9 | <0.001 |
| T4 | 90.0 | 91.4 | 94.6 | 95.9 | 97.3 | 98.0 | 79.3 | 100 | 98.6 | 88.6 | 90.3 | 91.8 | 96.1 | <0.001 | |
| T5 | 82.8 | 89.2 | 92.7 | 95.4 | 96.2 | 84.2 | 70.5 | 100 | 98.6 | 88.7 | 87.6 | 89.1 | 92.2 | <0.001 | |
| T6 | 86.3 | 90.3 | 92.1 | 96.9 | 94.1 | 96.4 | 88.1 | 100 | 97.5 | 96.0 | 88.0 | 90.3 | 94.9 | <0.001 | |
| T7 | 80.7 | 88.9 | 87.5 | 95.0 | 75.0 | 95.1 | 96.2 | 77.9 | 94.5 | 97.4 | 92.5 | 86.5 | 90.3 | 94.5 | <0.001 |
| T8 | 66.9 | 90.9 | 65.0 | 86.3 | 91.4 | 88.9 | 60.2 | 89.1 | 94.9 | 81.4 | 84.5 | 81.9 | 88.4 | <0.001 | |
| T9 | 89.1 | 93.4 | 85.9 | 91.9 | 67.9 | 96.4 | 97.0 | 85.7 | 100 | 98.8 | 93.4 | 89.1 | 89.6 | 97.3 | <0.001 |
| T10 | 96.1 | 90.9 | 97.9 | 98.5 | 96.6 | 89.2 | 94.1 | <0.001 | |||||||
| T11 | 95.6 | 94.7 | 96.6 | 91.5 | 97.6 | 96.8 | 78.9 | 100 | 100 | 98.6 | 89.5 | 91.6 | 90.7 | <0.001 | |
| T12 | 72.6 | 87.7 | 58.5 | 92.3 | 94.5 | 89.8 | 68.4 | 90.9 | 98.8 | 84.9 | 86.0 | 85.2 | 89.8 | <0.001 | |
| T13 | 74.8 | 87.1 | 87.5 | 91.7 | 95.8 | 96.9 | 79.3 | 98.3 | 98.8 | 62.5 | 82.7 | 82.8 | 80.0 | <0.001 | |
| T14 | 93.1 | 95.9 | 98.0 | 96.6 | 76.9 | 97.2 | 100 | 93.4 | 100 | 100 | 92.8 | 88.1 | 93.2 | 96.0 | <0.001 |
| T15 | 83.4 | 89.4 | 88.7 | 95.5 | 75.0 | 93.5 | 98.4 | 79.5 | 100 | 98.7 | 90.7 | 85.4 | 87.2 | 88.6 | <0.001 |
| T16 | 30.7 | 53.3 | 72.1 | 78.0 | 11.1 | 51.4 | 65.6 | <0.001 | |||||||
| T17 | 37.7 | 55.8 | 68.9 | 77.1 | 12.5 | 51.4 | 65.1 | <0.001 | |||||||
| T18 | 39.7 | 52.3 | 66.7 | 76.6 | 11.1 | 52.1 | 58.7 | <0.001 | |||||||
| T19 | 39.4 | 60.5 | 62.8 | 75.4 | 10.2 | 50.0 | 66.7 | <0.001 | |||||||
| T20 | 79.0 | 61.1 | 76.2 | 79.8 | 14.0 | 49.3 | 67.7 | <0.001 | |||||||
| T21 | 75.4 | 75.7 | 76.2 | 82.0 | 21.5 | 53.4 | 75.0 | <0.001 | |||||||
| T22 | 56.6 | 61.5 | 67.4 | 77.3 | 13.3 | 76.3 | 82.1 | <0.001 | |||||||
| T23 | 84.4 | 79.5 | 71.4 | 93.0 | 94.8 | 77.8 | 95.2 | 60.7 | 86.1 | 88.9 | 93.0 | <0.001 | |||
| T24 | 81.6 | 80.0 | 97.6 | 94.2 | 88.3 | 78.8 | 82.8 | <0.001 | |||||||
| T25 | 83.9 | 90.3 | 88.7 | 93.4 | 95.0 | 98.0 | 83.9 | 98.3 | 100 | 86.3 | 87.3 | 90.2 | <0.001 | ||
| T26 | 87.7 | 88.6 | 91.4 | 94.8 | 75.0 | 92.6 | 96.1 | 80.0 | 100 | 98.7 | 86.9 | 87.1 | 87.8 | 95.1 | <0.001 |
 |  |  |  |  |  |  | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Belgium n = 622 * | Czech Republic n = 199 * | Greece n = 193 * | Italy n = 595 * | Slovakia n = 603 * | Slovenia n = 350 * | Spain n = 295 * | ||
| T1 | 94.7 | 91.5 | 96.3 | 96.3 | 73.4 | 91.8 | 92.2 | <0.001 |
| T2 | 93.8 | 94.0 | 95.9 | 96.6 | 76.5 | 92.0 | 91.5 | <0.001 |
| T3 | 93.4 | 94.1 | 95.2 | 98.1 | 93.6 | 90.9 | 93.7 | <0.001 |
| T4 | 90.0 | 91.4 | 95.9 | 97.3 | 88.6 | 90.3 | 91.8 | <0.001 |
| T5 | 82.8 | 89.2 | 95.4 | 96.2 | 88.7 | 87.6 | 89.1 | <0.001 |
| T6 | 86.3 | 90.3 | 96.9 | 94.1 | 96.0 | 88.0 | 90.3 | <0.001 |
| T7 | 80.7 | 88.9 | 95.0 | 95.1 | 92.5 | 86.5 | 90.3 | <0.001 |
| T8 | 66.9 | 90.9 | 86.3 | 91.4 | 81.4 | 84.5 | 81.9 | <0.001 |
| T9 | 89.1 | 93.4 | 91.9 | 96.4 | 93.4 | 89.1 | 89.6 | <0.001 |
| T10 | 96.1 | 90.9 | 97.9 | 98.5 | 96.6 | 89.2 | 94.1 | <0.001 |
| T11 | 95.6 | 94.7 | 91.5 | 97.6 | 98.6 | 89.5 | 91.6 | <0.001 |
| T12 | 72.6 | 87.7 | 92.3 | 94.5 | 84.9 | 86.0 | 85.2 | <0.001 |
| T13 | 74.8 | 87.1 | 91.7 | 95.8 | 62.5 | 82.7 | 82.8 | <0.001 |
| T14 | 93.1 | 95.9 | 96.6 | 97.2 | 92.8 | 88.1 | 93.2 | <0.001 |
| T15 | 83.4 | 89.4 | 95.5 | 93.5 | 90.7 | 85.4 | 87.2 | <0.001 |
| T16 | 30.7 | 53.3 | 72.1 | 78.0 | 11.1 | 51.4 | 65.6 | <0.001 |
| T17 | 37.7 | 55.8 | 68.9 | 77.1 | 12.5 | 51.4 | 65.1 | <0.001 |
| T18 | 39.7 | 52.3 | 66.7 | 76.6 | 11.1 | 52.1 | 58.7 | <0.001 |
| T19 | 39.4 | 60.5 | 62.8 | 75.4 | 10.2 | 50.0 | 66.7 | <0.001 |
| T20 | 79.0 | 61.1 | 76.2 | 79.8 | 14.0 | 49.3 | 67.7 | <0.001 |
| T21 | 75.4 | 75.7 | 76.2 | 82.0 | 21.5 | 53.4 | 75.0 | <0.001 |
| T22 | 56.6 | 61.5 | 67.4 | 77.3 | 13.3 | 76.3 | 82.1 | <0.001 |
| T23 | 84.4 | 79.5 | 93.0 | 94.8 | 60.7 | 86.1 | 88.9 | <0.001 |
| T24 | 81.6 | 80.0 | 97.6 | 94.2 | 88.3 | 78.8 | 82.8 | <0.001 |
| T25 | 83.9 | 90.3 | 93.4 | 95.0 | 86.3 | 87.3 | 90.2 | <0.001 |
| T26 | 87.7 | 88.6 | 94.8 | 92.6 | 86.9 | 87.1 | 87.8 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Baetselier, E.; Van Rompaey, B.; Dijkstra, N.E.; Sino, C.G.; Akerman, K.; Batalha, L.M.; Fernandez, M.I.D.; Filov, I.; Grøndahl, V.A.; Heczkova, J.; et al. The NUPHAC-EU Framework for Nurses’ Role in Interprofessional Pharmaceutical Care: Cross-Sectional Evaluation in Europe. Int. J. Environ. Res. Public Health 2021, 18, 7862. https://doi.org/10.3390/ijerph18157862
De Baetselier E, Van Rompaey B, Dijkstra NE, Sino CG, Akerman K, Batalha LM, Fernandez MID, Filov I, Grøndahl VA, Heczkova J, et al. The NUPHAC-EU Framework for Nurses’ Role in Interprofessional Pharmaceutical Care: Cross-Sectional Evaluation in Europe. International Journal of Environmental Research and Public Health. 2021; 18(15):7862. https://doi.org/10.3390/ijerph18157862
Chicago/Turabian StyleDe Baetselier, Elyne, Bart Van Rompaey, Nienke E. Dijkstra, Carolien G. Sino, Kevin Akerman, Luis M. Batalha, Maria I. D. Fernandez, Izabela Filov, Vigdis A. Grøndahl, Jana Heczkova, and et al. 2021. "The NUPHAC-EU Framework for Nurses’ Role in Interprofessional Pharmaceutical Care: Cross-Sectional Evaluation in Europe" International Journal of Environmental Research and Public Health 18, no. 15: 7862. https://doi.org/10.3390/ijerph18157862
APA StyleDe Baetselier, E., Van Rompaey, B., Dijkstra, N. E., Sino, C. G., Akerman, K., Batalha, L. M., Fernandez, M. I. D., Filov, I., Grøndahl, V. A., Heczkova, J., Helgesen, A. K., Keeley, S., Kolovos, P., Langer, G., Ličen, S., Lillo-Crespo, M., Malara, A., Padyšáková, H., Prosen, M., ... Dilles, T. (2021). The NUPHAC-EU Framework for Nurses’ Role in Interprofessional Pharmaceutical Care: Cross-Sectional Evaluation in Europe. International Journal of Environmental Research and Public Health, 18(15), 7862. https://doi.org/10.3390/ijerph18157862










