Repercussions of the COVID-19 Response in Pregnant Women in Western Uganda: Knowledge, Behavior, and Emotional State after the First Lockdown in 2020
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Knowledge of SARS-CoV-2
3.2. Hygiene Behavior and General Behavioral Adaptations
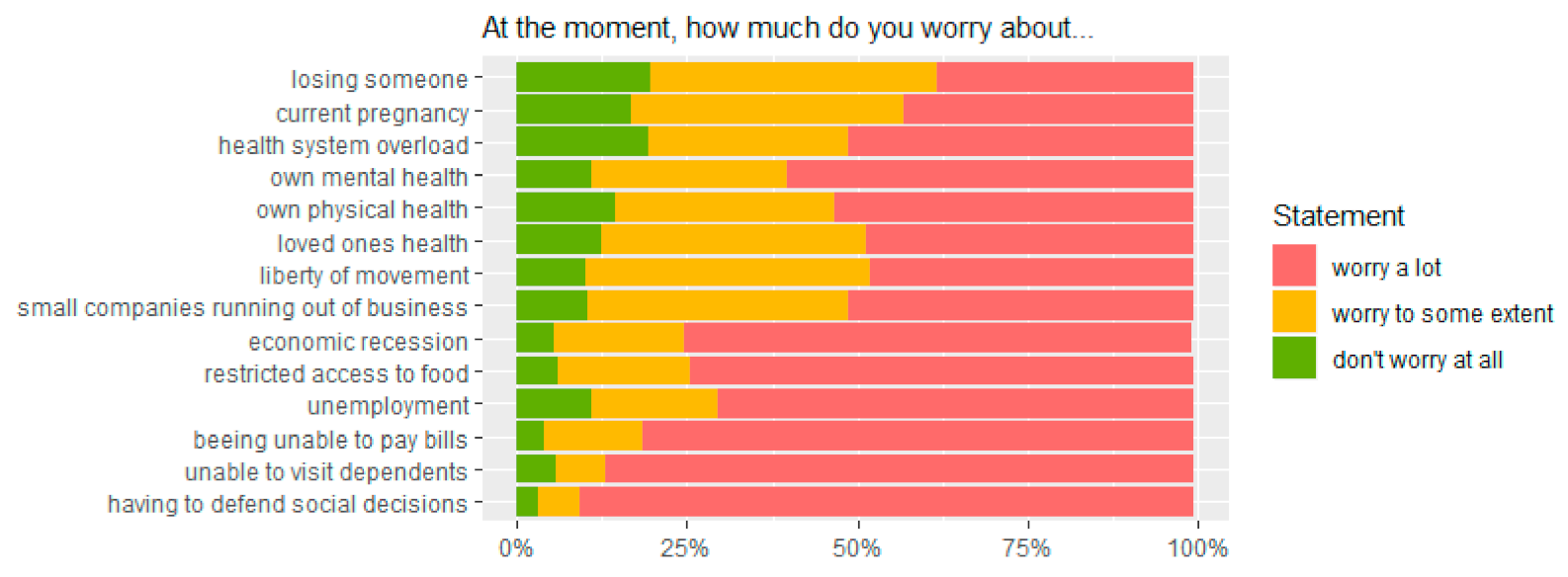
3.3. Psycho-Emotional Stress
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Addendum to Fact Sheet 15 on National Implementation Measures for the International Health Regulations 2005: COVID-19 as a Public Health Emergency of International Concern (PHEIC) under the IHR. 2020. Available online: https://extranet.who.int/sph/sites/default/files/document-library/document/FS15A_IHR_COVID19_EN_MAY_2020.pdf (accessed on 5 May 2021).
- Kapata, N.; Ihekweazu, C.; Ntoumi, F.; Raji, T.; Chanda-Kapata, P.; Mwaba, P.; Mukonka, V.; Bates, M.; Tembo, J.; Corman, V.; et al. Is Africa prepared for tackling the COVID-19 (SARS-CoV-2) epidemic. Lessons from past outbreaks, ongoing pan-African public health efforts, and implications for the future. Int. J. Infect. Dis. 2020, 93, 233–236. [Google Scholar] [CrossRef]
- El-Sadr, W.M.; Justman, J. Africa in the Path of Covid-19. N. Engl. J. Med. 2020, 383, e11. [Google Scholar] [CrossRef] [PubMed]
- Worldometer. COVID-19 Coronavirus Pandemic. Dover, Delaware: Worldometers.info. 2020. Available online: www.worldometers.info/coronavirus/ (accessed on 5 May 2021).
- WHO. Clinical Management of COVID-19. Interim Guidance. 27 May 2020. Available online: https://apps.who.int/iris/handle/10665/332196 (accessed on 5 May 2021).
- MoH Uganda, 2020. COVID-19 Preparedness and Response Plan. March 2020- June 2021. Available online: https://covid19.gou.go.ug/uploads/document_repository/authors/ministry_of_health/document/COVID19_PreparednessResponse_Plan_Signed_Vers_July20201.pdf (accessed on 5 May 2021).
- Mukaama, I.; Observer Research Foundation. The Expected Outcomes of the post-COVID19 Lockdown in Uganda. 4 June 2020. Available online: https://www.orfonline.org/expert-speak/the-expected-outcomes-of-the-post-COVID-19-lock-down-in-uganda-67299/ (accessed on 5 May 2021).
- Museveni, Y.K. Address by H.E. Yoweri Museveni President of the Republic of Uganda to the Nation on the Coronavirus (COVID-19) Guidelines on the Preventive Measures 18 March 2020 State House- Entebbe. Available online: https://kampala.diplo.de/blob/2315822/0468d91d79744d29cf6f2e8ce200da0d/corona-address-to-the-nation-data.pdf (accessed on 5 May 2021).
- Olum, R.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Bongomin, F. Coronavirus Disease-2019: Knowledge, Attitude, and Practices of Health Care Workers at Makerere University Teaching Hospitals, Uganda. Front. Public Health 2020, 8, 181. [Google Scholar] [CrossRef] [PubMed]
- Olum, R.; Kajjimu, J.; Kanyike, A.M.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Kemigisa, J.; Mulyamboga, P.; Muhoozi, O.K.; Nsenga, L.; et al. Perspective of Medical Students on the COVID-19 Pandemic: Survey of Nine Medical Schools in Uganda. JMIR Public Health Surveill. 2020, 6, e19847. [Google Scholar] [CrossRef] [PubMed]
- Kasozi, K.I.; MacLeod, E.; Ssempijja, F.; Mahero, M.W.; Matama, K.; Musoke, G.H.; Bardosh, K.; Ssebuufu, R.; Wakoko-Studstil, F.; Echoru, I.; et al. Misconceptions on COVID-19 Risk Among Ugandan Men: Results from a Rapid Exploratory Survey, April 2020. Front. Public Health 2020, 8, 416. [Google Scholar] [CrossRef] [PubMed]
- Ssebuufu, R.; Sikakulya, F.K.; Mambo, S.B.; Wasingya, L.; Nganza, S.K.; Ibrahim, B.; Kyamanywa, P. Knowledge, Attitude, and Self-Reported Practice Toward Measures for Prevention of the Spread of COVID-19 Among Ugandans: A Nationwide Online Cross-Sectional Survey. Front. Public Health 2020, 8, 618731. [Google Scholar] [CrossRef]
- Nwafor, J.I.; Aniukwu, J.K.; Anozie, B.O.; Ikeotuonye, A.C. Knowledge and practice of preventive measures against COVID-19 infection among pregnant women in a low-resource African setting. medRxiv 2020. [Google Scholar] [CrossRef]
- Ding, W.; Lu, J.; Zhou, Y.; Wei, W.; Zhou, Z.; Chen, M. Knowledge, attitudes, practices, and influencing factors of anxiety among pregnant women in Wuhan during the outbreak of COVID-19: A cross-sectional study. BMC Pregnancy Childbirth 2021, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Qiao, J. What are the risks of COVID-19 infection in pregnant women? Lancet 2020, 395, 760–762. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, D.A.; Graham, A.L. Potential Maternal and Infant Outcomes from Coronavirus 2019-nCoV (SARS-CoV-2) Infecting Pregnant Women: Lessons from SARS, MERS, and Other Human Coronavirus Infections. Viruses 2020, 12, 194. [Google Scholar] [CrossRef] [Green Version]
- Abdoli, A.; Falahi, S.; Kenarkoohi, A.; Shams, M.; Mir, H.; Jahromi, M.A.M. The COVID-19 pandemic, psychological stress during pregnancy, and risk of neurodevelopmental disorders in offspring: A neglected consequence. J. Psychosom. Obstet. Gynecol. 2020, 41, 247–248. [Google Scholar] [CrossRef]
- Uganda Ministry of Health. Guidance on Continuity of Essential Health Services during the COVID-19 Outbreak. April 2020. Available online: https://tciurbanhealth.org/wp-content/uploads/2020/05/MOH-GUIDANCE-ON-BUSINESS-CONTINUITY-000.docx3_.pdf (accessed on 16 July 2021).
- Uganda Ministry of Health. Annual Health Sector Performance Report. Financial Year 2019/2020. Available online: http://library.health.go.ug/publications/performance-management/annual-health-sector-performance-report-financial-year-201920 (accessed on 16 July 2021).
- Uganda National Council for Science and Technology. National Guidelines for Research involving Humans as Re-search Participants. Kampala, Uganda. 2014. Available online: http://mesau.mak.ac.ug/sites/default/files/Human%20Subjects%20Protection%20Guidelines%20July%202014_0.pdf (accessed on 11 May 2021).
- Schnack, A.; Rempis, E.; Decker, S.; Braun, V.; Rubaihayo, J.; Busingye, P.; Tumwesigye, N.M.; Harms, G.; Theuring, S. Prevention of Mother-to-Child Transmission of HIV in Option B+ Era: Uptake and Adherence During Pregnancy in Western Uganda. AIDS Patient Care STDs 2016, 30, 110–118. [Google Scholar] [CrossRef]
- Schumann, H.; Rubagumya, K.; Rubaihayo, J.; Harms, G.; Wanyenze, R.K.; Theuring, S. The incidence of HIV and associated risk factors among pregnant women in Kabarole District, Uganda. PLoS ONE 2020, 15, e0234174. [Google Scholar] [CrossRef]
- World Health Organisation Regional Office for Europe. Survey Tool and Guidance: Rapid, Simple, Flexible Behavioural Insights on COVID-19. Monitoring Knowledge, Risk Perceptions, Preventive Behaviours and Trust to Inform Pandemic Outbreak Response. Copenhagen, Denmark, 2020. Available online: https://www.psycharchives.org/bitstream/20.500.12034/2392/8/Guidance%20and%20protocol.BI%20for%20COVID-19_160420.pdf (accessed on 12 May 2021).
- Schroeder, K. Radio as a Tool of Health Education: What Makes for an Effective HIV/AIDS Radio Campaign in Sub-Saharan Africa? Intersect 2016, 9, 3. [Google Scholar]
- Gibson, L.; Rush, D. Novel Coronavirus in Cape Town Informal Settlements: Feasibility of Using Informal Dwelling Outlines to Identify High Risk Areas for COVID-19 Transmission from A Social Distancing Perspective. JMIR Public Health Surveill 2020, 6, e18844. [Google Scholar] [CrossRef] [PubMed]
- Iwuoha, V.C.; Aniche, E.T. Covid-19 lockdown and physical distancing policies are elitist: Towards an indigenous (Afro-centred) approach to containing the pandemic in sub-urban slums in Nigeria. Local Environ. 2020, 25, 631–640. [Google Scholar] [CrossRef]
- Wasdani, K.P.; Prasad, A. The impossibility of social distancing among the urban poor: The case of an Indian slum in the times of COVID-19. Local Environ. 2020, 25, 414–418. [Google Scholar] [CrossRef]
- Luo, Y.; Yao, L.; Hu, L.; Zhou, L.; Yuan, F.; Zhong, X. Urban and Rural Disparities of Personal Health Behaviors and the Influencing Factors During the COVID-19 Outbreak in China: Based on an Extended IMB Model. Disaster Med. Public Health Prep. 2020, 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, T.; Lueck, J.A.; Trujillo, K.L.; Ferdinand, A.O. Rural and Urban Differences in COVID-19 Prevention Behaviors. J. Rural. Health 2021, 37, 287–295. [Google Scholar] [CrossRef]
- McFarland, D.; Shen, M.J.; Parker, P.; Meyerson, S.; Holcombe, R.F. Does Hospital Size Affect Patient Satisfaction? Qual. Manag. Health Care 2017, 26, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Lubinga, E. ‘Uganda Can Protect Chinese Investors but Not Its Own Citizens?’ Paradoxical Perspectives in Xenophobic Narratives and Practices Fostering Otherness in Uganda. In Mediating Xenophobia in Africa; Moyo, D., Mpofu, S., Eds.; Palgrave Macmillan: Cham, Switzerland, 2020; pp. 207–227. [Google Scholar]
- Roberton, T.; Carter, E.; Chou, V.B.; Stegmuller, A.R.; Jackson, B.D.; Tam, Y.; Sawadogo-Lewis, T.; Walker, N. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: A modelling study. Lancet Glob. Health 2020, 8, e901–e908. [Google Scholar] [CrossRef]
- Dennis, C.-L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef]
- Ramchandani, P.G.; Richter, L.M.; Norris, S.A.; Stein, A. Maternal Prenatal Stress and Later Child Behavioral Problems in an Urban South African Setting. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mappa, I.; Distefano, F.A.; Rizzo, G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: A prospectic observational study. J. Périnat. Med. 2020, 48, 545–550. [Google Scholar] [CrossRef]
- Tang, X.; Lu, Z.; Hu, D.; Zhong, X. Influencing factors for prenatal Stress, anxiety and depression in early pregnancy among women in Chongqing, China. J. Affect. Disord. 2019, 253, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Manikkam, L.; Burns, J.K. Antenatal depression and its risk factors: An urban prevalence study in KwaZulu-Natal. S. Afr. Med J. 2012, 102, 940–944. [Google Scholar] [CrossRef]
- Brittain, K.; Myer, L.; Koen, N.; Koopowitz, S.; Donald, K.A.; Barnett, W.; Zar, H.J.; Stein, D.J. Risk factors for antenatal depression and associations with infant birth outcomes: Results from a south african birth cohort study. Paediatr. Périnat. Epidemiol. 2015, 29, 505–514. [Google Scholar] [CrossRef]
- Bilszta, J.L.C.; Tang, M.H.; Meyer, D.; Milgrom, J.; Ericksen, J.; Buist, A.E. Single motherhood versus poor partner relationship: Outcomes for antenatal mental health. Aust. N. Z. J. Psychiatry 2008, 42, 56–65. [Google Scholar] [CrossRef]
| Total n = 648 | N(%) |
|---|---|
| Age (n = 647) | 25.5 (5.8) (mean, standard deviation) |
| Marital Status (n = 648) | |
| Married Couple Single Divorced | 525 (81.0) 29 (4.5) 91 (14.0) 3 (0.5) |
| Health Facility (n = 648) | |
| Buhinga (urban, public) Virika (urban, private) Kibiito (rural, public) | 322 (49.7) 141 (21.8) 185 (28.6) |
| Completed Education (n = 646) | |
| None Primary Secondary Tertiary | 25 (3.9) 305 (47.2) 232 (35.9) 84 (13.0) |
| Occupation (n = 639) | |
| Farmer Trader/self-employed (unspecified) Homemaker Hair dresser Teacher Tailor Other | 246 (38.5) 122 (19.1) 118 (18.5) 27 (4.2) 20 (3.1) 20 (3.1) 86 (13.5) |
| Religion (n = 647) | |
| Christian Muslim Other | 604 (93.4) 35 (5.4) 8 (1.2) |
| Number of children living in household (n = 644) | 1 (0; 7) (median, range) |
| Wealth score [21,22] | |
| Lower (0–4) Higher (5–9) | 287 (44.3) 361 (55.7) |
| Partner occupation (n = 648) | |
| Farmer Trader/self-employed (unspecified) Workmen (e.g., builder, engineer, mechanic) Driver (e.g., taxi, motorbike taxi, truck) Civil service, armed forces Other | 172 (26.5) 133 (20.5) 106 (16.3) 88 (13.6) 51 (7.9) 98 (15.2) |
| Financially dependent on partner (n = 648) | |
| Completely For the most part For some part Not at all | 226 (34.9) 222 (34.3) 183 (28.2) 17 (2.6) |
| Physical violence and/or other partner harassment? (n = 647) | |
| Yes No | 59 (9.1) 588 (90.9) |
| Variable | Lower Knowledge Level n = 427 (67.24%) N (%) | OR (95% CI) | AOR (95% CI) |
|---|---|---|---|
| Age groups | |||
| <21 21–30 31–40 >40 | 92 (69.70) 254 (67.02) 76 (65.55) 5 (62.50) | reference 0.88 (0.57; 1.35) 0.83 (0.48; 1.41) 0.73 (0.17; 3.67) | reference 0.85 (0.53; 1.35) 0.80 (0.45; 1.42) 0.76 (0.17; 3.99) |
| Marital status | |||
| Married or couple Single or divorced | 362 (66.06) 65 (74.71) | reference 1.52 (0.92; 2.60) | reference 1.74 (1.01; 3.07) |
| Education | |||
| None Primary Secondary Tertiary | 17 (68.00) 201 (66.56) 146 (64.89) 63 (75.90) | reference 0.94 (0.37; 2.18) 0.87 (0.34; 2.05) 1.48 (0.54; 3.88) | reference 0.74 (0.29; 1.78) 0.79 (0.29; 1.98) 1.24 (0.39; 3.76) |
| Occupation | |||
| Not formally employed Formally employed | 329 (68.12) 98 (64.47) | reference 0.85 (0.58; 1.25) | reference 0.62 (0.38; 1.00) |
| Wealth score | |||
| 0–4 5–9 | 189 (67.50) 238 (67.04) | reference 0.98 (0.70; 1.37) | reference 0.95 (0.64; 1.40) |
| Source of knowledge | |||
| TV or Radio Social Media or Internet Community, other people Church or hospital | 395 (66.16) 4 (100) 17 (85.00) 8 (88.89) | reference 4.09 (0.74; 76.16) 2.90 (0.96; 12.52) -- | reference 4.12 (0.71; 78.03) 2.07 (0.65; 9.20) --- |
| Health Facility | |||
| Buhinga (urban, public) Virika (urban, private) Kibiito (rural, public) | 196 (62.82) 115 (82.14) 116 (63.39) | reference 2.72 (1.69; 4.52) 1.03 (0.70; 1.50) | reference 2.63 (1.57; 4.53) 1.02 (0.67; 1.56) |
| Variable | Lower Prevention Behavior Adherence n = 562 (88.64%) N (%) | OR (95% CI) | AOR (95% CI) |
|---|---|---|---|
| Age groups | |||
| <21 21–30 31–40 >40 | 125 (95.42) 331 (87.34) 99 (85.34) 7 (87.50) | reference 0.33 (0.12; 0.74) 0.28 (0.10; 0.70) 0.34 (0.05; 6.79) | 0.50 (0.18; 1.21) 0.44 (0.15; 1.19) 0.56 (0.07; 11.92) |
| Marital status | |||
| Married or couple Single, widow, divorced | 481 (87.77) 81 (94.19) | reference 2.26 (0.97; 6.59) | 1.58 (0.62; 4.88) |
| Education | |||
| None Primary Secondary Tertiary | 22 (88.00) 277 (92.03) 199 (88.44) 64 (77.11) | reference 1.57 (0.36; 4.98) 1.04 (0.24; 3.29) 0.46 (0.10; 1.52) | 1.28 (0.27; 4.40) 0.83 (0.17; 3.12) 0.68 (0.12; 3.15) |
| Occupation | |||
| Not formally employed Formally employed | 431 (89.42) 131 (86.18) | reference 0.74 (0.43; 1.30) | 0.92 (0.47; 1.89) |
| Wealth score [21,22] | |||
| 0–4 5–9 | 257 (92.11) 305 (85.02) | reference 0.52 (0.30; 0.88) | 0.54 (0.28; 1.02) |
| COVID-19 knowledge | |||
| Higher Lower | 184 (88.89) 378 (88.52) | reference 0.96 (0.56; 1.61) | 1.15 (0.64; 2.03) |
| Emotional stress level | |||
| Higher Lower | 214 (84.58) 348 (91.34) | reference 1.92 (1.17; 3.16) | 1.19 (0.66; 2.12) |
| Health Facility | |||
| Buhinga (urban, public) Virika (urban, private) Kibiito (rural, public) | 299 (95.83) 107 (76.43) 156 (85.71) | reference 0.14 (0.07; 0.27) 0.26 (0.13; 0.51) | 0.18 (0.08; 0.36) 0.17 (0.08; 0.36) |
| Variable | Higher Psycho-Emotional Stress Level n = 251 (39.84%) N (%) | OR (95% CI) | AOR (95% CI) |
|---|---|---|---|
| Age groups | |||
| <21 21–30 31–40 > 40 | 30 (22.90) 177 (46.95) 42 (36.52) 2 (28.57) | reference 2.98 (1.91; 4.76) 1.94 (1.11; 3.40) 1.35 (0.19; 6.60) | 1.97 (1.18; 3.35) 1.81 (0.92; 3.59) 2.05 (0.26; 11.78) |
| Marital status | |||
| Married/couple Single/divorced | 232 (42.65) 19 (22.09) | reference 0.38 (0.22; 0.64) | 0.42 (0.22; 0.77) |
| Education | |||
| None Primary Secondary Tertiary | 5 (20.83) 87 (29.00) 96 (43.05) 63 (75.90) | reference 1.55 (0.60; 4.80) 2.87 (1.11; 8.91) 11.97 (4.22; 39.98) | 1.67 (0.62; 5.34) 2.70 (0.95; 8.82) 6.80 (2.04; 25.80) |
| Occupation | |||
| Not formally employed Formally employed | 167 (34.79) 84 (56.00) | reference 2.39 (1.65; 3.47) | 1.38 (0.83; 2.27) |
| Wealth score | |||
| 0–4 5–9 | 91 (32.73) 160 (45.45) | reference 1.71 (1.24; 2.38) | 1.03 (0.68; 1.55) |
| Number of children living at home | |||
| 0–1 ≥2 | 153 (43.97) 98 (34.75) | reference 0.68 (0.49; 0.94) | 0.64 (0.42; 0.95) |
| Financial dependence on partner | |||
| Not at all For some part For the most part Completely | 4 (26.67) 80 (45.71) 92 (42.40) 75 (33.63) | reference 2.32 (0.76; 8.61) 2.02 (0.67; 7.49) 1.39 (0.46; 5.16) | 1.55 (0.44; 6.56) 1.49 (0.42; 6.32) 1.10 (0.31; 4.67) |
| Emotionally or physically threatened by partner | |||
| No Yes | 229 (40.03) 22 (37.93) | reference 0.92 (0.52; 1.58) | 1.63 (0.85; 3.09) |
| COVID-19 Knowledge | |||
| High Low | 104 (50.00) 147 (34.83) | reference 0.54 (0.38; 0.75) | 0.40 (0.27; 0.58) |
| Health Facility | |||
| Buhinga (urban, public) Virika (urban, private) Kibiito (rural, public) | 110 (35.60) 85 (60.71) 56 (30.94) | reference 2.80 (1.86; 4.24) 0.81 (0.55; 1.20) | 2.82 (1.73; 4.65) 1.28 (0.81; 2.03) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theuring, S.; Kengonzi, A.; Hafermann, L.; Herrmann, C.; Kabwama, S.N.; Rubaihayo, J. Repercussions of the COVID-19 Response in Pregnant Women in Western Uganda: Knowledge, Behavior, and Emotional State after the First Lockdown in 2020. Int. J. Environ. Res. Public Health 2021, 18, 7817. https://doi.org/10.3390/ijerph18157817
Theuring S, Kengonzi A, Hafermann L, Herrmann C, Kabwama SN, Rubaihayo J. Repercussions of the COVID-19 Response in Pregnant Women in Western Uganda: Knowledge, Behavior, and Emotional State after the First Lockdown in 2020. International Journal of Environmental Research and Public Health. 2021; 18(15):7817. https://doi.org/10.3390/ijerph18157817
Chicago/Turabian StyleTheuring, Stefanie, Agnes Kengonzi, Lorena Hafermann, Carolin Herrmann, Steven Ndugwa Kabwama, and John Rubaihayo. 2021. "Repercussions of the COVID-19 Response in Pregnant Women in Western Uganda: Knowledge, Behavior, and Emotional State after the First Lockdown in 2020" International Journal of Environmental Research and Public Health 18, no. 15: 7817. https://doi.org/10.3390/ijerph18157817
APA StyleTheuring, S., Kengonzi, A., Hafermann, L., Herrmann, C., Kabwama, S. N., & Rubaihayo, J. (2021). Repercussions of the COVID-19 Response in Pregnant Women in Western Uganda: Knowledge, Behavior, and Emotional State after the First Lockdown in 2020. International Journal of Environmental Research and Public Health, 18(15), 7817. https://doi.org/10.3390/ijerph18157817






