Safety Performance of Healthcare Professionals: Validation and Use of the Adapted Workplace Health and Safety Instrument
Abstract
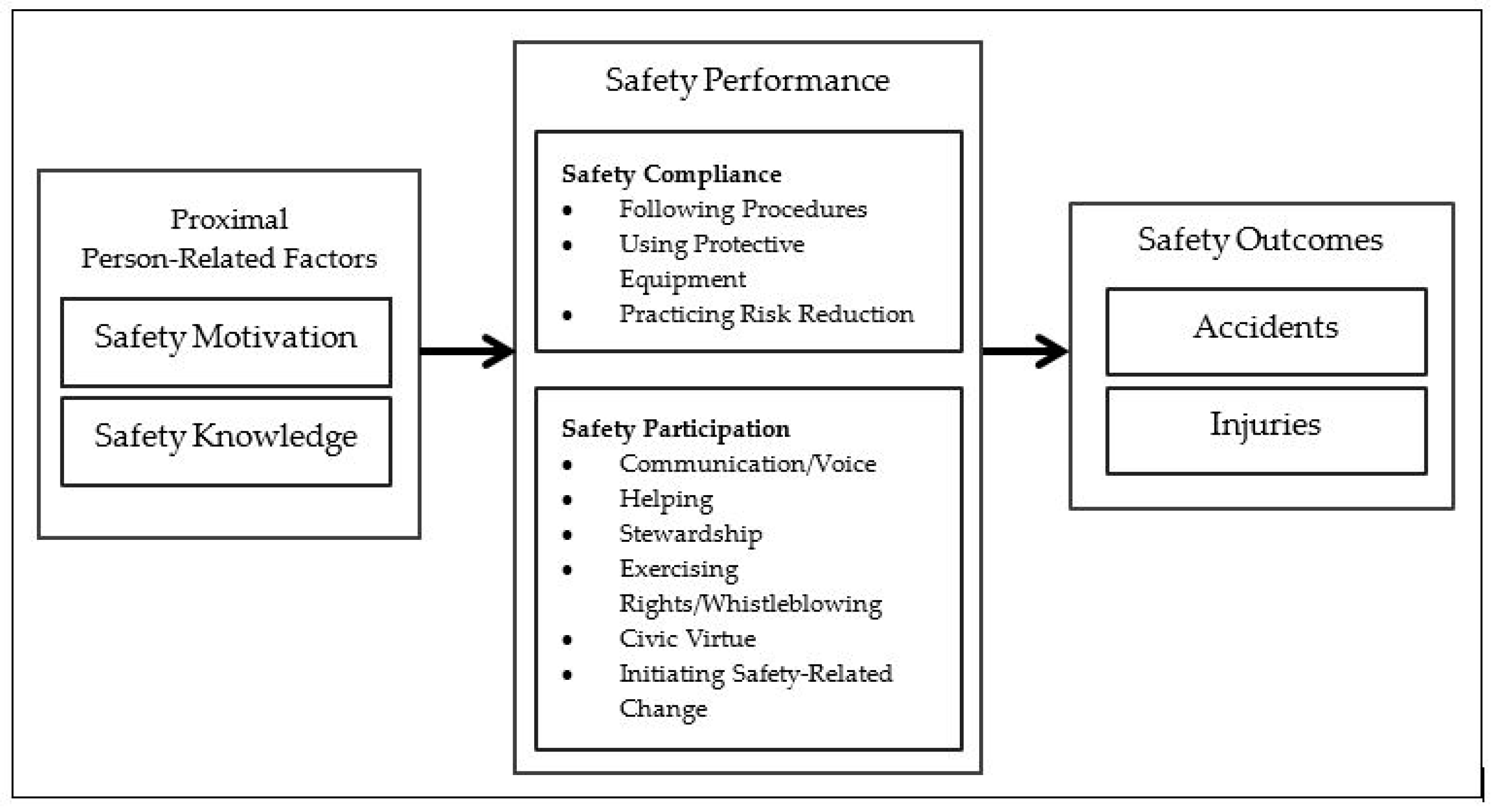
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Instrument
2.3. Setting, Procedure, and Sample
2.4. Analysis
3. Results
3.1. Study Sample and Descriptive Statistics
3.2. Analysis of Internal Consistency, Construct, and Factorial Validity
4. Discussion
4.1. Limitations
4.2. Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Concha-Barrientos, M.; Nelson, D.I.; Fingerhut, M.; Driscoll, T.; Leigh, J. The global burden due to occupational injury. Am. J. Ind. Med. 2005, 48, 470–481. [Google Scholar] [CrossRef]
- Hämäläinen, P.; Takala, J.; Saarela, K.L. Global estimates of occupational accidents. Saf. Sci. 2006, 44, 137–156. [Google Scholar] [CrossRef]
- Takala, J. Global Estimates of fatal occupational accidents. Epidemiology 1999, 10, 640–646. [Google Scholar] [CrossRef]
- German Social Accident Insurance. Statistics—Occupational Accidents 2019, Berlin. 2020. Available online: https://publikationen.dguv.de/widgets/pdf/download/article/3893 (accessed on 20 January 2021).
- de Vries, E.N.; Ramrattan, M.A.; Smorenburg, S.M.; Gouma, D.J.; Boermeester, M.A. The incidence and nature of in-hospital adverse events: A systematic review. Qual. Saf. Health Care 2008, 17, 216–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Towards Eliminating Avoidable Harm in Health Care: Draft Global Patient Safety Action Plan 2021–2030. Available online: https://cdn.who.int/media/docs/default-source/patient-safety/gpsap/final-draft-global-patient-safety-action-plan-2021-2030.pdf?sfvrsn=fc8252c5_5 (accessed on 21 July 2021).
- Ghahramani, A.; Khalkhali, H.R. Development and validation of a safety climate scale for manufacturing industry. Saf. Health Work 2015, 6, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Muñiz, B.; Montes-Peón, J.M.; Vázquez-Ordás, C.J. Safety climate in OHSAS 18001-certified organisations: Antecedents and consequences of safety behaviour. Accid. Anal. Prev. 2012, 45, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Mohr, D.C.; Lipkowitz Eaton, J.; McPhaul, K.M.; Hodgson, M.J.; Eaton, J.L. Does employee safety matter for patients too? Employee safety climate and patient safety culture in health care. J. Patient Saf. 2018, 14, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Rost, K.A.; Alvero, A.M. Participatory approaches to workplace safety management: Bridging the gap between behavioral safety and participatory ergonomics. Int. J. Occup. Saf. Ergon. 2018, 26, 194–203. [Google Scholar] [CrossRef]
- Reuter, E.; Camba, J.D. Understanding emergency workers’ behavior and perspectives on design and safety in the workplace. Appl. Ergon. 2017, 59, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Cooklin, A.; Joss, N.; Husser, E.; Oldenburg, B. Integrated approaches to occupational health and safety: A systematic review. Am. J. Health Promot. 2017, 31, 401–412. [Google Scholar] [CrossRef]
- Clarke, S. An integrative model of safety climate: Linking psychological climate and work attitudes to individual safety outcomes using meta-analysis. J. Occup. Organ. Psychol. 2010, 83, 553–578. [Google Scholar] [CrossRef]
- Wagner, A.; Rieger, M.A.; Manser, T.; Sturm, H.; Hardt, J.; Martus, P.; Lessing, C.; Hammer, A. Healthcare professionals’ perspectives on working conditions, leadership, and safety climate: A cross-sectional study. BMC Health Serv. Res. 2019, 19, 53. [Google Scholar] [CrossRef] [PubMed]
- Clarke, S.; Ward, K. The role of leader influence tactics and safety climate in engaging employees’ safety participation. Risk Anal. 2006, 26, 1175–1185. [Google Scholar] [CrossRef] [PubMed]
- Beus, J.M.; McCord, M.A.; Zohar, D. Workplace safety. Organ. Psychol. Rev. 2016, 6, 352–381. [Google Scholar] [CrossRef]
- Meyers, A.R.; Al-Tarawneh, I.S.; Bushnell, P.T.; Wurzelbacher, S.J.; Lampl, M.P.; Tseng, C.-Y.; Turner, D.M.; Morrison, C.A. Degree of integration between occupational safety and health programs and wellness programs: First-year results from an insurer-sponsored wellness grant for smaller employers. J. Occup. Environ. Med. 2019, 61, 704–717. [Google Scholar] [CrossRef]
- Jiang, L.; Yu, G.; Li, Y.; Li, F. Perceived colleagues’ safety knowledge/behavior and safety performance: Safety climate as a moderator in a multilevel study. Accid. Anal. Prev. 2010, 42, 1468–1476. [Google Scholar] [CrossRef] [PubMed]
- Gordon, M.; Darbyshire, D.; Baker, P. Non-technical skills training to enhance patient safety: A systematic review. Med. Educ. 2012, 46, 1042–1054. [Google Scholar] [CrossRef] [PubMed]
- Brasaitė, I.; Kaunonen, M.; Martinkėnas, A.; Mockienė, V.; Suominen, T. Health care professionals’ skills regarding patient safety. Medicina 2016, 52, 250–256. [Google Scholar] [CrossRef]
- Griffin, M.A.; Neal, A. Perceptions of safety at work: A framework for linking safety climate to safety performance, knowledge, and motivation. J. Occup. Health Psychol. 2000, 5, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Neal, A.; Griffin, M.A.; Hart, P.M. The impact of organizational climate on safety climate and individual behavior. Saf. Sci. 2000, 34, 99–109. [Google Scholar] [CrossRef]
- Christian, M.S.; Bradley, J.C.; Wallace, J.C.; Burke, M.J. Workplace safety: A meta-analysis of the roles of person and situation factors. J. Appl. Psychol. 2009, 94, 1103–1127. [Google Scholar] [CrossRef] [PubMed]
- Neal, A.; Griffin, M.A. A study of the lagged relationships among safety climate, safety motivation, safety behavior, and accidents at the individual and group levels. J. Appl. Psychol. 2006, 91, 946–953. [Google Scholar] [CrossRef] [Green Version]
- Kalteh, H.O.; Mortazavi, S.B.; Mohammadi, E.; Salesi, M. Psychometric properties of the Persian version of Neal and Griffin’s safety performance scale. Int. J. Occup. Saf. Ergon. 2021, 27, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Braunger, P.; Frank, H.; Korunka, C.; Lueger, M.; Kubicek, B. Validating a safety climate model in metal processing industries: A replication study. Int. J. Occup. Saf. Ergon. 2013, 19, 143–155. [Google Scholar] [CrossRef] [Green Version]
- Gracia, F.J.; Tomás, I.; Martínez-Córcoles, M.; Peiró, J.M. Empowering leadership, mindful organizing and safety performance in a nuclear power plant: A multilevel structural equation model. Saf. Sci. 2020, 123, 104542. [Google Scholar] [CrossRef]
- Toderi, S.; Gaggia, A.; Mariani, M.G.; Mancini, G.; Broccoli, M. Griffin and Neal’s safety model: Determinants and components of individual safety performance in the Italian context. La Med. Lav. 2015, 106, 447–459. [Google Scholar]
- Banville, D.; Desrosiers, P.; Genet-Volet, Y. Translating questionnaires and inventories using a cross-cultural translation technique. J. Teach. Phys. Educ. 2000, 19, 374–387. [Google Scholar] [CrossRef]
- Vallerand, R.J. Vers une méthodologie de validation trans-culturelle de questionnaires psychologiques: Implications pour la recherche en langue française. Can. Psychol. Psychol. Can. 1989, 30, 662–680. [Google Scholar] [CrossRef]
- van de Vijver, F.J.R. (Ed.) Test adaptations. In The ITC International Handbook of Testing and Assessment; Oxford University Press: Oxford, UK, 2016; pp. 364–376. ISBN 9780199356942. [Google Scholar]
- Miller, K.; Chepp, V.; Willson, S.; Padilla, J.-L. Cognitive Interviewing Methodology; Wiley: Hoboken, NJ, USA, 2014; ISBN 978-1118383544. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; Sage: Los Angeles, CA, USA; London, UK; New Delhi, India; Singapore; Washington, DC, USA; Melbourne, Australia, 2018; ISBN 978-1-5264-1951-4. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39. [Google Scholar] [CrossRef]
- Hair, J.F. Multivariate Data Analysis: A Global Perspective, 7th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2010; ISBN 978-0138132637. [Google Scholar]
- Kwon, O.-J.; Kim, Y.-S. An analysis of safeness of work environment in Korean manufacturing: The “safety climate” perspective. Saf. Sci. 2013, 53, 233–239. [Google Scholar] [CrossRef]
- Martínez-Córcoles, M.; Gracia, F.J.; Tomás, I.; Peiró, J.M.; Schöbel, M. Empowering team leadership and safety performance in nuclear power plants: A multilevel approach. Saf. Sci. 2013, 51, 293–301. [Google Scholar] [CrossRef]
- Clarke, S. The relationship between safety climate and safety performance: A meta-analytic review. J. Occup. Health Psychol. 2006, 11, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Manapragada, A.; Bruk-Lee, V.; Thompson, A.H.; Heron, L.M. When safety climate is not enough: Examining the moderating effects of psychosocial hazards on nurse safety performance. J. Adv. Nurs. 2018, 75, 1207–1218. [Google Scholar] [CrossRef] [PubMed]
| n | % | |
|---|---|---|
| Total sample | 160 | 100% |
| Profession | ||
| Physician | 23 | 14.40% |
| Nurse | 62 | 38.80% |
| Nurse in training | 56 | 35.00% |
| Other | 18 | 11.30% |
| Missing | 1 | 0.60% |
| Gender | ||
| Female | 115 | 71.90% |
| Male | 45 | 28.10% |
| Leadership functions | ||
| Yes | 24 | 15.00% |
| No | 132 | 82.50% |
| Missing | 4 | 2.50% |
| Tenure in the profession | ||
| <3 months | 2 | 1.30% |
| 3–12 months | 1 | 0.60% |
| 1–5 years | 76 | 47.50% |
| >5 years | 79 | 49.40% |
| Missing | 2 | 1.30% |
| Tenure in clinic | ||
| <3 months | 4 | 2.50% |
| 3–12 months | 6 | 3.80% |
| 1–5 years | 87 | 54.40% |
| >5 years | 62 | 38.80% |
| Missing | 1 | 0.60% |
| Age | ||
| <30 | 84 | 52.50% |
| 31–40 | 29 | 18.10% |
| 41–50 | 23 | 14.40% |
| >50 | 23 | 14.40% |
| Missing | 1 | 0.60% |
| Dimensions/Items | Missing | Floor Effect | Ceiling Effect | Mean Score | SD |
|---|---|---|---|---|---|
| Safety Knowledge | 0.0% | 0.0% | 42.5% | 4.19 | 0.63 |
| 0.0% | 0.0% | 45.0% | 4.35 | 0.68 |
| 1.9% | 0.6% | 41.9% | 4.15 | 0.89 |
| 3.1% | 0.0% | 31.9% | 4.08 | 0.80 |
| 2.5% | 0.0% | 36.3% | 4.19 | 0.77 |
| Safety Motivation | 0.0% | 0.0% | 91.3% | 4.83 | 0.30 |
| 0.0% | 0.0% | 93.1% | 4.90 | 0.42 |
| 1.9% | 0.0% | 78.1% | 4.77 | 0.49 |
| 0.6% | 0.0% | 78.8% | 4.77 | 0.46 |
| 0.6% | 0.0% | 88.8% | 4.89 | 0.34 |
| Safety Compliance | 1.3% | 0.0% | 38.8% | 4.18 | 0.64 |
| 1.3% | 0.0% | 36.9% | 4.22 | 0.74 |
| 3.1% | 1.3% | 44.4% | 4.21 | 0.90 |
| 2.5% | 0.6% | 33.1% | 4.21 | 0.72 |
| 2.5% | 0.6% | 29.4% | 4.10 | 0.76 |
| Safety Participation | 0.6% | 1.3% | 17.5% | 3.50 | 0.87 |
| 3.8% | 18.8% | 8.1% | 2.78 | 1.24 |
| 1.3% | 3.1% | 19.4% | 3.53 | 1.04 |
| 1.3% | 1.3% | 52.5% | 4.41 | 0.77 |
| 2.5% | 11.3% | 18.1% | 3.28 | 1.26 |
| α | AVE | √AVE | Spearman’s Correlation | |||
|---|---|---|---|---|---|---|
| SK | SM | SC | ||||
| SK—Safety Knowledge | 0.80 | 0.46 | 0.68 | |||
| SM—Safety Motivation | 0.72 | 0.45 | 0.67 | 0.24 * | ||
| SC—Safety Compliance | 0.84 | 0.54 | 0.73 | 0.54 * | 0.31 * | |
| SP—Safety Participation | 0.76 | 0.44 | 0.66 | 0.33 * | 0.14 + | 0.43 * |
| Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|
| Safety Knowledge | ||||
| 0.569 | −0.016 | 0.190 | 0.062 |
| 0.576 | −0.001 | 0.044 | 0.148 |
| 0.805 | 0.090 | −0.042 | −0.078 |
| 0.744 | 0.059 | −0.043 | −0.013 |
| Safety Motivation | ||||
| 0.121 | 0.370 | −0.051 | −0.026 |
| 0.007 | 0.630 | 0.118 | −0.066 |
| 0.136 | 0.567 | 0.064 | −0.067 |
| −0.069 | 0.968 | −0.054 | 0.077 |
| Safety Compliance | ||||
| 0.128 | 0.065 | 0.635 | 0.034 |
| −0.063 | 0.062 | 0.599 | 0.090 |
| 0.035 | −0.112 | 0.978 | −0.099 |
| −0.009 | 0.101 | 0.660 | 0.113 |
| Safety Participation | ||||
| 0.057 | −0.036 | 0.082 | 0.696 |
| 0.076 | −0.027 | −0.054 | 0.709 |
| −0.155 | 0.130 | 0.131 | 0.545 |
| 0.056 | −0.100 | −0.029 | 0.677 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heier, L.; Gambashidze, N.; Hammerschmidt, J.; Riouchi, D.; Weigl, M.; Neal, A.; Icks, A.; Brossart, P.; Geiser, F.; Ernstmann, N. Safety Performance of Healthcare Professionals: Validation and Use of the Adapted Workplace Health and Safety Instrument. Int. J. Environ. Res. Public Health 2021, 18, 7816. https://doi.org/10.3390/ijerph18157816
Heier L, Gambashidze N, Hammerschmidt J, Riouchi D, Weigl M, Neal A, Icks A, Brossart P, Geiser F, Ernstmann N. Safety Performance of Healthcare Professionals: Validation and Use of the Adapted Workplace Health and Safety Instrument. International Journal of Environmental Research and Public Health. 2021; 18(15):7816. https://doi.org/10.3390/ijerph18157816
Chicago/Turabian StyleHeier, Lina, Nikoloz Gambashidze, Judith Hammerschmidt, Donia Riouchi, Matthias Weigl, Andrew Neal, Andrea Icks, Peter Brossart, Franziska Geiser, and Nicole Ernstmann. 2021. "Safety Performance of Healthcare Professionals: Validation and Use of the Adapted Workplace Health and Safety Instrument" International Journal of Environmental Research and Public Health 18, no. 15: 7816. https://doi.org/10.3390/ijerph18157816
APA StyleHeier, L., Gambashidze, N., Hammerschmidt, J., Riouchi, D., Weigl, M., Neal, A., Icks, A., Brossart, P., Geiser, F., & Ernstmann, N. (2021). Safety Performance of Healthcare Professionals: Validation and Use of the Adapted Workplace Health and Safety Instrument. International Journal of Environmental Research and Public Health, 18(15), 7816. https://doi.org/10.3390/ijerph18157816






