1. Introduction
The health consequences of tobacco use are extensive and known to include numerous cancers, cardiovascular disease (CVD), chronic obstructive pulmonary disease (COPD), and pregnancy complications [
1]. Most tobacco-related disease is attributed to the numerous toxicants present in tobacco and tobacco smoke [
1,
2]. However, as the addictive component of tobacco products, the effects of nicotine are often conflated with the effects of other tobacco constituents. The situation is complicated by the wide-range of nicotine containing products, and varying levels of nicotine delivered among them. Indeed, many in the general population misperceive nicotine as responsible for smoking-related health risks, including cancer [
3,
4,
5,
6]. For example, a survey reporting on data from two waves (2015 and 2017) of a large US national survey found that 51% of participants agreed that “nicotine is the substance that causes most of the cancer caused by smoking” [
7]. Another 2016 survey with adults ages 18–40 found that 66% believed that a relatively large or very large part of the “health risks of smoking” come from nicotine, and 60% believed that nicotine was responsible for a relatively large/very large part “of the cancer caused by smoking” [
6].
One might expect this misperception to be limited to the general population, but research studies have also documented such misperception among healthcare professionals. For example, a 2007 study found that 60% of nurses incorrectly perceived nicotine as carcinogenic [
8]. Indeed, our own national survey of US physicians in 2018 found that a majority of doctors ‘strongly agreed’ that “nicotine directly contributes” to the development of CVD, COPD, and cancer [
9]. Additionally, we found that misperceptions regarding nicotine’s role differed by physician specialty, with pulmonologists generally being least likely to hold nicotine misperceptions while family physicians were more likely than most other specialists to hold nicotine misperceptions. Similar findings of nicotine misperceptions have been noted among health care providers in other countries [
10].
A growing body of survey methods research highlights the importance of question wording and format when assessing perceptions [
11,
12,
13]. As such, we considered that the wording of survey questions about nicotine health effects may have contributed to our finding of prevalent nicotine misperceptions. For example, it is possible that some respondents may have answered by thinking about the health effects of tobacco use that are mediated by nicotine addiction rather than nicotine itself (i.e., nicotine causes addiction to smoking, which then leads to lung cancer). Moreover, survey satisficing—wherein respondents put forth the minimum amount of effort necessary to provide an acceptable response—has been posited as an explanation for acquiescence bias, or the tendency to agree with assertions contained in a question [
14]. If some of our respondents were satisficing, they may not have read the question with enough care in order to distinguish between nicotine and cigarettes more generally, contributing to the high amount of agreement we uncovered.
For these reasons, the wording of questions about nicotine’s health effects may impact how physicians report their perceptions on this topic. To evaluate this hypothesis, we conducted a randomized survey experiment to explore the effect of question wording on estimates of nicotine misperception among a national sample of US physicians.
2. Materials and Methods
We embedded a randomized split-sample experiment about nicotine risk perception questions in a 2019 national survey of US physicians designed to explore physicians’ knowledge and communication with patients about tobacco and electronic nicotine vapor products. Random samples of 750 physicians in each of three specialties (family medicine, internal medicine, and obstetrics/gynecology (OBGYN)) were selected from the AMA physician master file. To be eligible, physicians must have been board certified in their specialty and actively seeing outpatients. Sampled physicians were mailed a letter that included a link to the web-based survey, as well as two additional reminder mailings. In a fourth and final mailing, sampled physicians who had not yet responded were provided with a paper copy of the survey to return by postal mail. In total, 995 physicians participated in the study and 305 were ineligible, yielding an AAPOR response rate of 57.8%. The present analysis is restricted to 926 respondents who completed by web (and thus able to be randomized to the online experiment).
The survey included domains about demographic characteristics, treatment practices, and knowledge/perceptions about tobacco and electronic nicotine products (e.g., e-cigarettes). Participants were randomly assigned to receive one of two versions of a question matrix about health effects of nicotine: Version 1 (from our previous survey [
9], “Please indicate the extent to which you agree or disagree that nicotine directly contributes to the development of the following health problems by selecting your choice” and Version 2, “Please indicate the extent to which you agree or disagree that nicotine
on its own directly contributes to the development of the following health problems by selecting your choice.” Both versions then presented response options “Strongly Agree,” “Agree,” “Disagree,” and “Strongly Disagree” corresponding to each of five health outcomes: birth defects, cardiovascular disease, cancer, depression, and COPD (See
online supplement, Figure S1).
SAS software version 9.4 (SAS Institute, Cary, NC) were used for all analyses. We used descriptive statistics to characterize the study sample and compared demographics across survey condition to assess the success of randomization. To compare the distribution of responses by question version, we assigned numeric values ranging from 1 (Strongly Disagree) to 4 (Strongly Agree) and calculated the mean response for each health effect. Since the distributions were highly skewed, we compared response means using two-sided Wilcoxon Rank-Sum tests. We then estimated prevalence ratios adjusted for gender, age, and specialty using log-binomial regression to describe the association between question version and “strongly agreeing” that nicotine directly contributes to each health effect. We separately assessed effect modification by physician specialty and age by including a cross-product term (e.g., Version*Specialty, Version*Age) in the regression models. We repeated the regression analyses modeling the prevalence of “agreeing or strongly agreeing” as a function of question version, age, gender, and specialty.
3. Results
Of the 926 web-survey participants, 461 and 465 were randomized to Version 1 and Version 2, respectively. Version assignment did not differ by age, gender, race/ethnicity, graduation year, or specialty (
Table 1). Overall, about half (50.6%) of respondents were female, two-thirds (66.8%) were non-Hispanic white, and the median age was 51 years.
For the outcomes of birth defects, cardiovascular disease, cancer, and COPD, the distribution of responses to the nicotine health effects questions differed significantly by survey version, such that the response means were lower (towards strong disagreement) among the group that received Version 2 (
Table 2). In addition, smaller proportions of respondents in the Version 2 group relative to the Version 1 group “strongly agreed” that nicotine directly contributed to each health effect, with marked differences for the questions about cancer (69.6% vs. 85.0%) and COPD (67.3% vs. 85.2%).
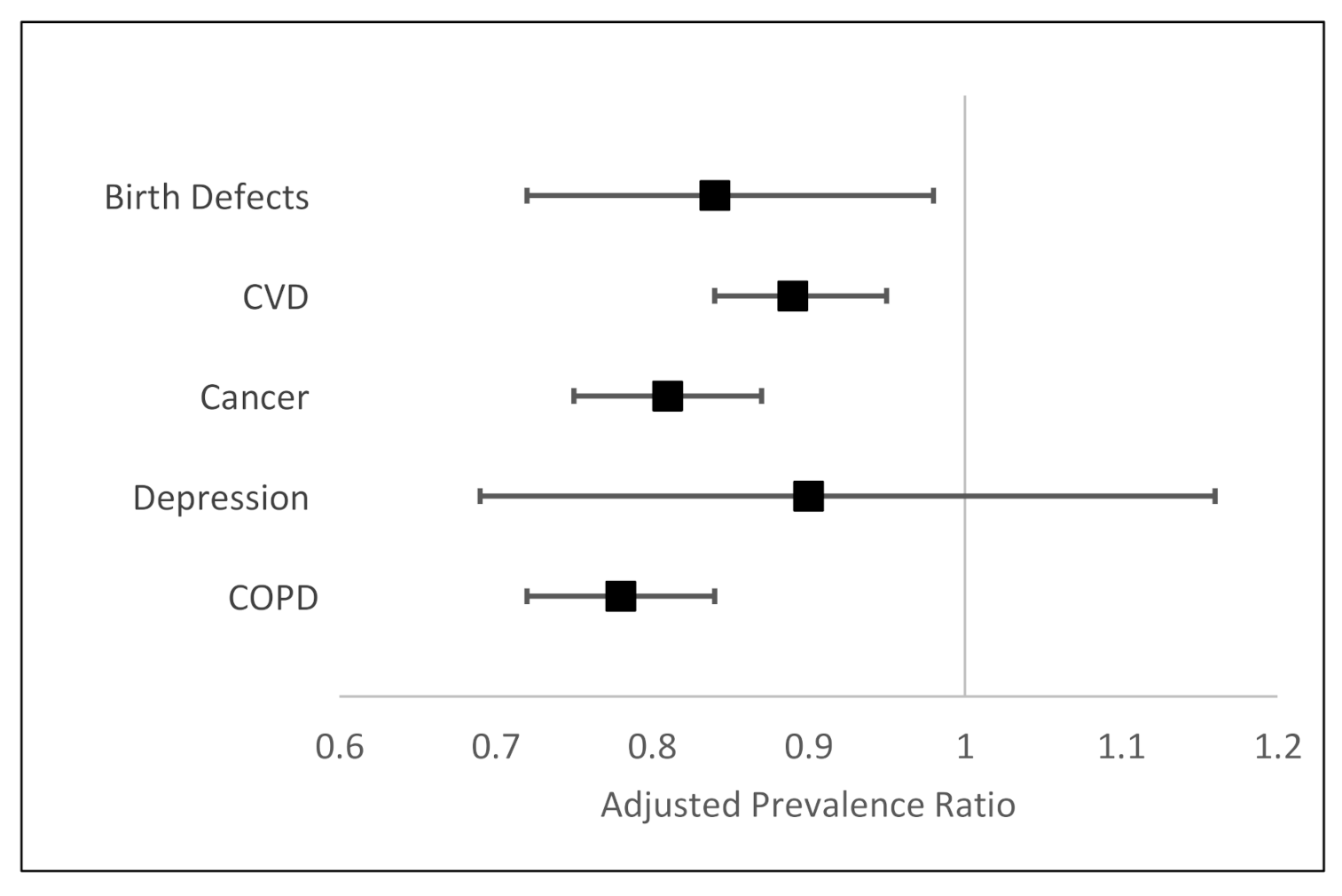
In regression analyses adjusted for gender, age, and specialty, physicians who received Version 2 were significantly less likely to “strongly agree” that nicotine directly caused birth defects (PR 0.84, 95% CI 0.72–0.98), CVD (PR 0.89, 95% CI 0.84–0.95), cancer (PR 0.81, 95% CI 0.75–0.87), and COPD (PR 0.78, 95% CI 0.72–0.84) (
Table 3,
Figure 1). We did not find evidence of effect modification by specialty or age (all
p-values for interaction >0.1, data not shown). The second set of regression models, modeling prevalence of “strongly agree or agree” versus “disagree or strongly disagree,” also found that physicians who received Version 2 were significantly less likely to perceive that nicotine directly contributes to CVD, cancer, and COPD, although these associations were not as strong (
Table 4). The association between question version and agreeing that nicotine directly contributes to birth defects was attenuated and not significant (PR 0.94, 95% CI 0.88–1.01).
Female physicians were significantly more likely to “strongly agree” that nicotine directly contributes to birth defects (PR 1.19, 95% CI 1.01–1.39) and cancer (PR 1.08 95% CI 1.01–1.15), even after adjusting for questionnaire version, age, and medical specialty (
Table 3). However, when modeling “strongly agree or agree” as the outcome, sex was not significantly associated with perceptions about nicotine’s direct contribution to any outcome.
Differences in perceptions were noted across specialty groups. For example, family medicine and internal medicine physicians were 74% (PR 1.74, 95% CI 1.41–2.13) and 69% (PR 1.69, 95% CI 1.35–2.11) more likely than OB/GYN specialists to “strongly agree” that nicotine directly contributes to birth defects, respectively (
Table 3). Family physicians were most likely to “strongly agree” that nicotine directly contributes to CVD, cancer, and COPD. In the second set of regression models, the associations between specialty group and “strongly agreeing or agreeing” that nicotine causes birth defects, CVD, cancer, and COPD were attenuated but still significant (
Table 4).
4. Discussion
In a follow-up to our prior research that observed misperceptions about the health effects of nicotine among a national sample of US physicians [
9], we sought to assess the impact of question wording on estimates of physician perceptions about nicotine using a randomized split-sample survey experiment. Indeed, question version was significantly associated with “strongly agreeing” that nicotine directly contributes to development of birth defects, CVD, cancer, and COPD, even after adjusting for age, sex, and medical specialty. Specifically, we found that physicians who answered a question version that more explicitly asked about the effects of nicotine “on its own” reported lower levels of misperceptions about the health effects caused by nicotine, suggesting the potential importance of this type of wording. Question version was still relevant when modeling “strongly agree or agree” as the outcome, suggesting that question wording is important for distinguishing agreement versus disagreement generally, as well as strong agreement versus moderate agreement or disagreement.
Even after accounting for question version, the proportion of surveyed physicians who believe that nicotine directly contributes to these health outcomes is alarmingly high. It is possible that participants are conflating the addictive effect of nicotine with the comparatively more harmful effects of tobacco use. This overestimation of the harms caused by nicotine may be exacerbated by a potential availability bias, as previous research has demonstrated that nicotine is the cigarette constituent most familiar to many people [
15]. As such, respondents may have made judgements and overestimations about the probability that nicotine causes harm based on the ease with which they associate nicotine and cigarettes more generally [
16]. We also observed differences in nicotine perceptions by gender and specialty. In general, females were more likely to endorse “strong agreement” that nicotine directly contributes to each health effect; however, these associations did not persist when modeling the more general “agree vs. disagree” outcome. Family medicine physicians were most likely to misperceive nicotine as a direct contributor to CVD, cancer, and COPD regardless of how the outcome was defined.
Our findings are consistent with our previous study. For example, our previous analysis of data collected during 2018 also found that females were more likely than males to misperceive nicotine as a direct contributor to CVD, cancer, and COPD; however, the magnitude of these associations were somewhat weaker in the present study than it was in 2018 (e.g., PR, females vs. males, for strongly agreeing that nicotine directly contributes to CVD was 1.10 (95% CI 1.04–1.17) previously and 1.04 (95% CI 0.98–1.10) currently). Future surveillance of physician perceptions across demographics and specialties is warranted to understand whether this tightening “gender gap” will continue.
These findings should be interpreted in the light of some limitations that are common to survey research. First, our findings that perceptions about nicotine vary by physician gender and specialty may be subject to selection bias if physicians who chose to participate in the survey differ from those who did not with respect to their perceptions about nicotine. However, sample representativeness is unlikely to threaten the validity of the finding that physician perceptions are impacted by question version, given that question version was randomly assigned and there were no differences in demographics or medical specialty across study groups. Second, participants received only one of the two different question versions when they completed the survey; inclusion of additional question versions in the experiment may have been more helpful for learning about how to best measure nicotine perceptions. Future planned studies will include version of the question explicitly emphasizing potential non-addiction-related effects. Additionally, future qualitative research may be useful for elucidating the underlying beliefs and reasons for the observed response patterns among physicians. Finally, although the survey sample was selected at random within specialty groups, results are not weighted to be representative of all family medicine, internal medicine, and OB/GYN physicians in the U.S.
Despite these limitations, this study of US physicians from several specialties demonstrates that question wording is important when assessing physician beliefs about nicotine health effects, and this finding would be likely to extend to surveys about physician perspectives about other topics as well. In addition, we found that even after accounting for question version, perceiving that nicotine directly contributes to certain health effects was very common, and there were differences in perceptions by sex and medical specialty. This highlights the importance of improving physician education about tobacco and nicotine, which may improve patient-provider communications about tobacco use, tobacco cessation, and use of nicotine containing products.
5. Conclusions
Our findings demonstrate that question wording is important when measuring physician beliefs about nicotine. However, even after accounting for question version, misperceptions about the direct health effects of nicotine were common, and perceptions about nicotine varied by sex and specialty. Provider education about tobacco and nicotine should be prioritized in order to optimize patient–provider communications about tobacco use and cessation.
Author Contributions
Conceptualization, M.T.B.M., M.B.S., O.A.W., B.S., C.D.D.; methodology, M.T.B.M., O.A.W., B.S., C.D.D.; software, C.D.D.; validation, M.T.B.M., B.S., W.J.Y.; formal analysis, M.T.B.M., W.J.Y.; investigation, M.T.B.M., M.B.S., O.A.W., B.S., C.D.D.; resources, C.D.D.; writing—original draft preparation, M.T.B.M.; writing—review and editing, M.T.B.M., M.B.S., O.A.W., B.S., W.J.Y., C.D.D.; project administration, B.S., M.B.S., C.D.D.; funding acquisition, C.D.D., M.B.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research and the APC was funded by National Institutes of Health, grant number R01CA190444/CA/NCI.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Rutgers, The State University of New Jersey (Pro2012001854).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- US Department of Health and Human Services 2014 Surgeon General’s Report: The Health Consequences of Smoking-50 Years of Progress. Available online: https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm (accessed on 4 June 2021).
- Gottlieb, S.; Zeller, M. A Nicotine-Focused Framework for Public Health. N. Engl. J. Med. 2017, 377, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- Cummings, K.M.; Hyland, A.; Giovino, G.; Hastrup, J.; Bauer, J.; Bansal, M. Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine Tob. Res. 2004, 6, 333–340. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.K.; Nguyen, A.B.; Persoskie, A.; Hoffman, A.C. U.S. adults’ addiction and harm beliefs about nicotine and low nicotine cigarettes. Prev. Med. 2017, 96, 94–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, S.Y.; Curbow, B.; Stillman, F.A. Harm perception of nicotine products in college freshmen. Nicotine Tob. Res. 2007, 9, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Villanti, A.C.; Naud, S.; West, J.C.; Pearson, J.L.; Wackowski, O.A.; Niaura, R.S.; Hair, E.; Rath, J.M. Prevalence and correlates of nicotine and nicotine product perceptions in U.S. young adults, 2016. Addict. Behav. 2019, 98, 106020. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.B.; Zhao, X.; Hoffman, L.; Morse, A.L.; Delahanty, J. Nicotine and addiction beliefs and perceptions among the US-born and foreign-born populations. Prev. Med. 2018, 114, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, B.; Novak, S.P. Nurses’ knowledge about the risk of light cigarettes and other tobacco “harm reduction” strategies. Nicotine Tob. Res. 2007, 9, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, M.B.; Bover Manderski, M.T.; Wackowski, O.A.; Singh, B.; Strasser, A.A.; Delnevo, C.D. Nicotine Risk Misperception Among US Physicians. J. Gen. Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Moysidou, A.; Farsalinos, K.; Voudris, V.; Merakou, K.; Kourea, K.; Barbouni, A. Knowledge and Perceptions about Nicotine, Nicotine Replacement Therapies and Electronic Cigarettes among Healthcare Professionals in Greece. Int. J. Environ. Res. Public Health 2016, 13, 514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holbert, R.L.; Koshy, A. Question Wording and Item Formulation. Int. Encycl. Media Psychol. 2020, 1–5. [Google Scholar] [CrossRef]
- Magelssen, M.; Supphellen, M.; Nortvedt, P.; Materstvedt, L.J. Attitudes towards assisted dying are influenced by question wording and order: A survey experiment. BMC Med. Ethics 2016, 17, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tourangeau, R.; Rips, L.J.; Rasinski, K. The Psychology of Survey Response; Cambridge University Press: Cambridge, UK, 2000. [Google Scholar]
- Holbrook, A. Acquiescence Response Bias. In Encyclopedia of Survey Research Methods; SAGE Publications, Inc: Thousand Oaks, CA, USA, 2008. [Google Scholar]
- Jeong, M.; Noar, S.M.; Zhang, D.; Mendel, J.R.; Agans, R.P.; Boynton, M.H.; Byron, M.J.; Baig, S.A.; Ranney, L.M.; Ribisl, K.M.; et al. Public Understanding of Cigarette Smoke Chemicals: Longitudinal Study of US Adults and Adolescents. Nicotine Tob. Res. 2019, 22, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Tversky, A.; Kahneman, D. Availability: A heuristic for judging frequency and probability. Cogn. Psychol. 1973, 5, 207–232. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).