An Attempt to Predict Changes in Heart Rate Variability in the Training Intensification Process among Cyclists
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
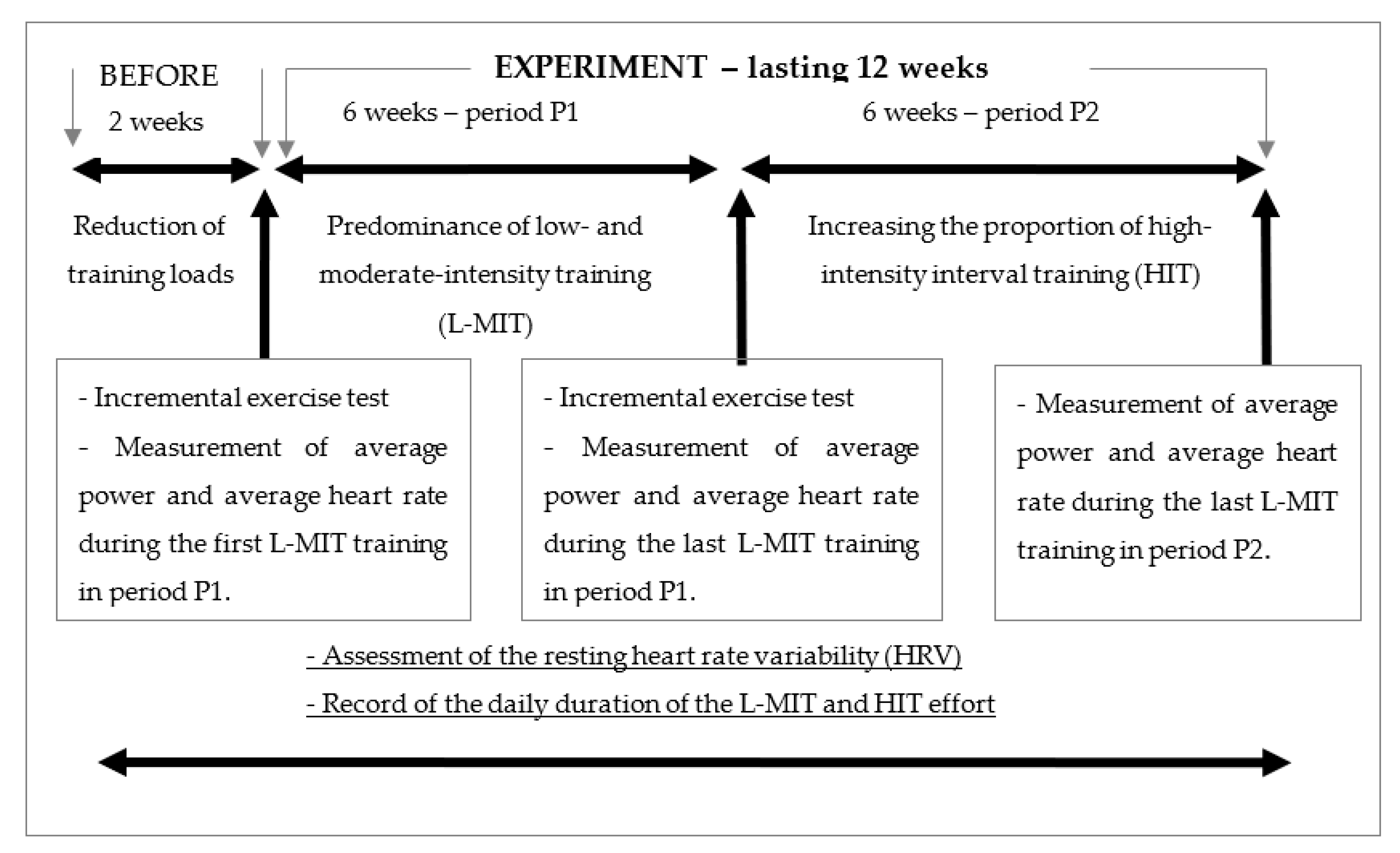
2.2. Experimental Design
- L-MIT trainings at a level of 70–85% power measured at VT2 and at 65–75% of maximal heart rate (HRmax); their duration equalled 2–4 h (Training 1—T1);
- trainings with exercises requiring high pedalling frequency, at a heart rate of 65–75% HRmax—repeated efforts with a pedalling frequency increased by 15–25 RPM compared to the individually preferred rhythm (determined on the basis of constant-intensity training observations) (Training 2—T2);
- training sessions with repeated exercises of high intensity (above 150% of maximal aerobic power (Pmax), determined in the incremental exercise test) lasting 15–20 s (Training 3—T3);
- trainings consisting of resistance exercises (e.g., semi-squats) alternated with cycling exercises of high pedalling frequency (increased by 15–25 RPM compared to the individually preferred rhythm), at a heart rate of 65–75% HRmax (Training 4—T4).
- L-MIT trainings at an intensity of 70–85% power measured at VT2 and at a heart rate of 65–75% HRmax; their duration equalled 2–3.5 h (Training 5—T5);
- HIT interval trainings involving repeated efforts at 130–160% Pmax lasting 25–50 s (Training 6—T6);
- HIT trainings comprised of repeated efforts at 105–120% Pmax lasting 1–2 min (Training 7—T7);
- HIT trainings consisting of repeated efforts at 90–100% Pmax lasting 3–6 min (Training 8—T8);
- trainings composed of resistance exercises (e.g., semi-squats) (Training 9—T9).
2.3. Exercise Test
2.4. Statistical Calculations and Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seiler, S. What is best practice for training intensity and duration distribution in endurance athletes? Int. J. Sports Physiol. Perform. 2010, 5, 276–291. [Google Scholar] [CrossRef] [PubMed]
- Solli, G.S.; Tønnessen, E.; Sandbakk, Ø. Block vs. traditional periodization of HIT: Two different paths to success for the world’s best cross-country skier. Front. Physiol. 2019, 10, 375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, D.J. A framework for understanding the training process leading to elite performance. Sports Med. 2003, 33, 1103–1126. [Google Scholar] [CrossRef] [PubMed]
- Hebisz, P.; Hebisz, R.; Zatoń, M.; Ochmann, B.; Mielnik, N. Concomitant application of sprint and high-intensity interval training on maximal oxygen uptake and work output in well-trained cyclists. Eur. J. Appl. Physiol. 2016, 116, 1495–1502. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Laursen, P.B. High-intensity interval training, solutions to the programming puzzle. Part 1: Cardiopulmonary emphasis. Sports Med. 2013, 43, 313–338. [Google Scholar] [CrossRef]
- Tschakert, G.; Hofmann, P. High-intensity intermittent exercise: Methodological and physiological aspects. Int. J. Sports Physiol. Perform. 2013, 8, 600–610. [Google Scholar] [CrossRef] [Green Version]
- Warr-di Piero, D.; Valverde-Esteve, T.; Redondo-Castán, J.C.; Pablos-Abella, C.; Sánchez-Alarcos Díaz-Pintado, J.V. Effects of work-interval duration and sport specificity on blood lactate concentration, heart rate and perceptual responses during high intensity interval training. PLoS ONE 2018, 13, e0200690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stöggl, T.; Sperlich, B. Polarized training has greater impact on key endurance variables than threshold, high intensity, or high volume training. Front. Physiol. 2014, 5, 33. [Google Scholar] [CrossRef] [Green Version]
- Levine, B.D. VO2max: What do we know, and what do we still need to know? J. Physiol. 2008, 586, 25–34. [Google Scholar] [CrossRef]
- Evertsen, F.; Medbo, J.I.; Jebens, E.; Nicolaysen, K. Hard training for 5 mo increases Na(+)-K+ pump concentration in skeletal muscle of cross-country skiers. Am. J. Physiol. 1997, 272, R1417–R1424. [Google Scholar] [CrossRef]
- Gaskill, S.E.; Serfass, R.C.; Bacharach, D.W.; Kelly, J.M. Responses to training in cross-country skiers. Med. Sci. Sports Exerc. 1999, 31, 1211–1217. [Google Scholar] [CrossRef]
- Da Silva, D.F.; Bianchini, J.A.; Antonini, V.D.; Hermoso, D.A.; Lopera, C.A.; Pagan, B.G.; McNeil, J.; Nardo Junior, N. Parasympathetic cardiac activity is associated with cardiorespiratory fitness in overweight and obese adolescents. Pediatr. Cardiol. 2014, 35, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.C.; Murray, C.; Janse van Rensburg, D.C.; Fletcher, L. A comparison between heart rate and heart rate variability as indicators of cardiac health and fitness. Front. Physiol. 2013, 4, 337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueno, L.M.; Hamada, T.; Moritani, T. Cardiac autonomic nervous activities and cardiorespiratory fitness in older men. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2002, 57, M605–M610. [Google Scholar] [CrossRef] [Green Version]
- Daanen, H.A.; Lamberts, R.P.; Kallen, V.L.; Jin, A.; Van Meeteren, N.L. A systematic review on heart-rate recovery to monitor changes in training status in athletes. Int. J. Sports Physiol. Perform. 2012, 7, 251–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaikkonen, P.; Hynynen, E.; Mann, T.; Rusko, H.; Nummela, A. Heart rate variability is related to training load variables in interval running exercises. Eur. J. Appl. Physiol. 2012, 112, 829–838. [Google Scholar] [CrossRef] [Green Version]
- Schmitt, L.; Regnard, J.; Desmarets, M.; Mauny, F.; Mourot, L.; Fouillot, J.P.; Coulmy, N.; Millet, G. Fatigue shifts and scatters heart rate variability in elite endurance athletes. PLoS ONE 2013, 8, e71588. [Google Scholar] [CrossRef]
- Earnest, C.P.; Jurca, R.; Church, T.S.; Chicharro, J.L.; Hoyos, J.; Lucia, A. Relation between physical exertion and heart rate variability characteristics in professional cyclists during Tour of Spain. Br. J. Sports Med. 2004, 38, 568–575. [Google Scholar] [CrossRef] [Green Version]
- Pichot, V.; Busso, T.; Roche, F.; Garet, M.; Costes, F.; Duverney, D.; Lacour, J.R.; Barthélémy, J.C. Autonomic adaptations to intensive and overload training periods: A laboratory study. Med. Sci. Sports Exerc. 2002, 34, 1660–1666. [Google Scholar] [CrossRef]
- Oliveira, R.S.; Leicht, A.S.; Bishop, D.; Barbero-Álvarez, J.C.; Nakamura, F.Y. Seasonal changes in physical performance and heart rate variability in high level futsal players. Int. J. Sports Med. 2013, 34, 424–430. [Google Scholar] [CrossRef]
- Botek, M.; McKune, A.J.; Krejci, J.; Stejskal, P.; Gaba, A. Change in performance in response to training load adjustment based on autonomic activity. Int. J. Sports Med. 2014, 35, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Høydal, K.L. Effects of exercise intensity on VO2max in studies comparing two or more exercise intensities: A meta-analysis. Sport Sci. Health 2017, 13, 239–252. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Issurin, V.B. Biological background of block periodized endurance training: A review. Sports Med. 2019, 49, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Figueira, T.R.; Caputo, F.; Machado, C.E.; Denadai, B.S. Aerobic Fitness Level Typical of Elite Athletes is not Associated With Even Faster VO2 Kinetics During Cycling Exercise. J. Sports Sci. Med. 2008, 7, 132–138. [Google Scholar] [PubMed]
- Joyner, M.J.; Coyle, E.F. Endurance exercise performance: The physiology of champions. J. Physiol. 2008, 586, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Kiely, J. Periodization Paradigms in the 21st Century: Evidence-Led or Tradition-Driven? Int. J. Sports Physiol. Perform. 2012, 7, 242–250. [Google Scholar] [CrossRef] [Green Version]
- Hebisz, R.; Hebisz, P.; Danek, N.; Michalik, K.; Zatoń, M. Predicting changes in maximal oxygen uptake in response to polarized training (sprint interval training, high-intensity interval training, and endurance training) in mountain bike cyclists. J. Strength Cond. Res. 2020. ahead of print. [Google Scholar] [CrossRef]
- Hebisz, R.; Hebisz, P.; Borkowski, J.; Zatoń, M. Effects of concomitant high-intensity interval training and sprint interval training on exercise capacity and response to exercise- induced muscle damage in mountain bike cyclists with different training backgrounds. Isokinet. Exerc. Sci. 2019, 27, 21–29. [Google Scholar] [CrossRef]
- Beltz, N.M.; Gibson, A.L.; Janot, J.M.; Kravitz, L.; Mermier, C.M.; Dalleck, L.C. Graded exercise testing protocols for the determination of VO2max: Historical perspectives, progress, and future considerations. J. Sports Med. 2016, 2016, 3968393. [Google Scholar] [CrossRef] [Green Version]
- Beaver, W.L.; Wasserman, K.; Whipp, B.J. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 1986, 60, 2020–2027. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.; Walker, T.; Burnet, S.; Jobson, S.A. The Reliability and Validity of the PowerTap P1 Power Pedals Before and After 100 Hours of Use. Int. J. Sports Physiol. Perform. 2019, 14, 855–858. [Google Scholar] [CrossRef] [PubMed]
- Boudreaux, B.D.; Hebert, E.P.; Hollander, D.B.; Williams, B.M.; Cormier, C.L.; Naquin, M.R.; Gillan, W.W.; Gusew, E.E.; Kraemer, R.R. Validity of Wearable Activity Monitors during Cycling and Resistance Exercise. Med. Sci. Sports Exerc. 2018, 50, 624–633. [Google Scholar] [CrossRef] [PubMed]
- Windt, J. Polar Beat: Train to your heart’s content. Br. J. Sports Med. 2016, 50, 441. [Google Scholar] [CrossRef]
- Plaza-Florido, A.; Migueles, J.H.; Mora-Gonzalez, J.; Molina-Garcia, P.; Rodriguez-Ayllon, M.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Solis-Urra, P.; de Teresa, C.; Gutiérrez, Á.; et al. Heart rate is a better predictor of cardiorespiratory fitness than heart rate variability in overweight/obese children: The ActiveBrains project. Front. Physiol. 2019, 10, 510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellenger, C.R.; Fuller, J.T.; Thomson, R.L.; Davison, K.; Robertson, E.Y.; Buckley, J.D. Monitoring athletic training status through autonomic heart rate regulation: A systematic review and meta-analysis. Sports Med. 2016, 46, 1461–1486. [Google Scholar] [CrossRef]
- Sandercock, G.R.; Bromley, P.D.; Brodie, D.A. Effects of exercise on heart rate variability: Inferences from meta-analysis. Med. Sci. Sports Exerc. 2005, 37, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Macor, F.; Fagard, R.; Amery, A. Power spectral analysis of RR interval and blood pressure short-term variability at rest and during dynamic exercise: Comparison between cyclists and controls. Int. J. Sports Med. 1996, 17, 175–181. [Google Scholar] [CrossRef]
- Pichot, V.; Roche, F.; Gaspoz, J.M.; Enjolras, F.; Antoniadis, A.; Minini, P.; Costes, F.; Busso, T.; Lacour, J.R.; Barthélémy, J.C. Relation between heart rate variability and training load in middle-distance runners. Med. Sci. Sports Exerc. 2000, 32, 1729–1736. [Google Scholar] [CrossRef] [Green Version]
- Schneider, C.; Wiewelhove, T.; Raeder, C.; Flatt, A.A.; Hoos, O.; Hottenrott, L.; Schumbera, O.; Kellmann, M.; Meyer, T.; Pfeiffer, M.; et al. Heart rate variability monitoring during strength and high-intensity interval training overload microcycles. Front. Physiol. 2019, 10, 582. [Google Scholar] [CrossRef] [Green Version]
- Daniłowicz-Szymanowicz, L.; Figura-Chmielewska, M.; Raczak, A.; Szwoch, M.; Ratkowski, W. The assessment of influence of long-term exercise training on autonomic nervous system activity in young athletes preparing for competitions. Pol. Merkur. Lek. 2011, 30, 19–25. [Google Scholar]
- Raczak, G.; Daniłowicz-Szymanowicz, L.; Kobuszewska-Chwirot, M.; Ratkowski, W.; Figura-Chmielewska, M.; Szwoch, M. Long-term exercise training improves autonomic nervous system profile in professional runners. Kardiol. Pol. 2006, 64, 135–140. [Google Scholar]
- Lamberts, R.P.; Swart, J.; Noakes, T.D.; Lambert, M.I. A novel submaximal cycle test to monitor fatigue and predict cycling performance. Br. J. Sports Med. 2011, 45, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Chalencon, S.; Pichot, V.; Roche, F.; Lacour, J.R.; Garet, M.; Connes, P.; Barthélémy, J.C.; Busso, T. Modeling of performance and ANS activity for predicting future responses to training. Eur. J. Appl. Physiol. 2015, 115, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, K.A.; Lopes, J.A.; de Souza, E.G.; Stanganelli, L.C.R. Effect of a training macrocycle on physiological indicators, body composition, and explosiveness among recreational runners. Hum. Mov. 2020, 21, 49–56. [Google Scholar] [CrossRef] [Green Version]
| Variables | S1 | S2 | S3 | S4 | S5 | S6 | S7 |
|---|---|---|---|---|---|---|---|
| Age [year] | 21 | 18 | 24 | 17 | 20 | 22 | 20 |
| Body mass [kg] | 75.4 | 55.8 | 73.2 | 49.3 | 62.2 | 70.9 | 54.7 |
| Body height [m] | 1.83 | 1.71 | 1.81 | 1.62 | 1.71 | 1.86 | 1.63 |
| VO2max [ml∙min−1∙kg−1] | 66.6 | 58.1 | 77.0 | 58.0 | 62.4 | 68.7 | 60.4 |
| Pmax1 [W∙kg−1] | 5.97 | 4.70 | 6.52 | 4.56 | 5.66 | 5.97 | 5.34 |
| Pmax1 [W] | 450 | 262 | 477 | 225 | 352 | 423 | 292 |
| Pmax2 [W] | 460 | 275 | 465 | 240 | 344 | 418 | 310 |
| VT21 [W] | 305 | 205 | 320 | 140 | 225 | 305 | 205 |
| VT22 [W] | 330 | 190 | 335 | 145 | 220 | 305 | 215 |
| HFb [ms2] | 546 | 689 | 1381 | 3922 | 3597 | 10,746 | 30,865 |
| LFb [ms2] | 137 | 890 | 3082 | 4060 | 2086 | 2526 | 5881 |
| RMSSDb [ms] | 39 | 53.1 | 86.1 | 119.3 | 111 | 168.3 | 333.4 |
| SDNNb [ms] | 27.9 | 43.2 | 72.3 | 93.1 | 81.1 | 133.7 | 207.7 |
| RRNNb [ms] | 1006 | 1267 | 1537 | 1140 | 1318 | 1197 | 1398 |
| Experience [y] | 7 | 4 | 9 | 3 | 6 | 7 | 5 |
| Cycling Training | S1 | S2 | S3 | S4 | S5 | S6 | S7 | |
|---|---|---|---|---|---|---|---|---|
| T1 | t (min) | 120–240 | 120–210 | 120–225 | 120–150 | 150–230 | 120–195 | 150–240 |
| P (W) | 215–260 | 145–175 | 225–270 | 100–120 | 160–190 | 215–260 | 145–175 | |
| Rep | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| T2 | t (min) | 10–20 | 10–15 | 10–15 | 5–10 | 10–15 | 10–15 | 10–20 |
| RPM | 103–113 | 101–111 | 97–107 | 106–116 | 100–110 | 98–108 | 106–116 | |
| P (W) | 215–260 | 145–175 | 225–270 | 100–120 | 160–190 | 215–260 | 145–175 | |
| Rep | 2–5 | 2–4 | 2–5 | 1–4 | 2–5 | 2–5 | 2–5 | |
| T3 | t (s) | 15 | 15 | 15 | 15 | 15 | 15 | 15 |
| P (W) | ≥675 | ≥393 | ≥715 | ≥337 | ≥528 | ≥634 | ≥438 | |
| Rep | 1–4 | 1–4 | 1–4 | 1–4 | 1–4 | 1–4 | 1–4 | |
| T4 | t (min) | 3 | 2 | 3 | 1.5 | 3 | 2 | 3 |
| RPM | 103–113 | 101–111 | 97–107 | 106–116 | 100–110 | 98–108 | 106–116 | |
| P (W) | 290–320 | 190–220 | 305–335 | 125–155 | 210–240 | 290–320 | 190–220 | |
| Rep | 3–7 | 3–6 | 3–7 | 2–5 | 3–7 | 3–7 | 3–7 | |
| T5 | t (min) | 120–195 | 120–160 | 120–195 | 120–135 | 135–195 | 120–180 | 140–210 |
| P (W) | 230–280 | 130–160 | 235–285 | 100–125 | 155–185 | 215–260 | 150–180 | |
| Rep | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| T6 | t (s) | 40–50 | 30–40 | 40–50 | 25–30 | 40–50 | 40–50 | 40–50 |
| P (W) | 600–650 | 380–420 | 605–655 | 355–385 | 450–500 | 540–590 | 400–440 | |
| Rep | 8–16 | 6–12 | 8–20 | 4–10 | 8–16 | 8–12 | 8–12 | |
| T7 | t (s) | 60–120 | 60–90 | 60–120 | 60–80 | 60–90 | 60–120 | 60–120 |
| P (W) | 480–520 | 290–330 | 485–525 | 250–290 | 370–410 | 440–480 | 325–365 | |
| Rep | 5–10 | 3–7 | 5–8 | 3–6 | 4–8 | 3–7 | 5–10 | |
| T8 | t (min) | 4–6 | 3–4 | 4–6 | 3–3.5 | 4–6 | 3–5 | 5–6 |
| P (W) | 410–450 | 250–275 | 415–455 | 215–240 | 310–345 | 375–415 | 280–310 | |
| Rep | 4–8 | 3–6 | 4–8 | 2–4 | 4–8 | 3–6 | 4–8 | |
| Participants | HF [ms2] | LF [ms2] | RMSSD [ms] | SDNN [ms] | RRNN [ms] | HIT [min] | L-MIT [min] |
|---|---|---|---|---|---|---|---|
| S1 | |||||||
| P1 (n = 31) | 367.7 ±217.8 | 64.1 ±57.1 | 31.9 ±9.8 | 22.5 ±6.7 | 978.8 ±53.0 | 0.3 ±0.9 | 94.2 ±77.7 |
| P2 (n = 30) | 644.1 ±401.0 ** | 119.3 ±71.4 ** | 42.3 ±13.9 ** | 29.8 ±8.9 ** | 991.1 ±44.7 | 8.0 ±13.3 ** | 82.0 ±58.7 |
| t | −3.36 | −3.34 | −3.37 | −3.62 | −0.98 | −3.24 | 0.69 |
| D | 0.89 | 0.86 | 0.88 | 0.94 | 0.25 | 1.08 | 0.18 |
| S2 | |||||||
| P1 (n = 35) | 927.7 ±439.1 | 743.5 ±687.2 | 64.9 ±15.8 | 44.7 ±11.6 | 1315.6 ±81.1 | 0.1 ±0.3 | 81.7 ±71.2 |
| P2 (n = 43) | 1184.6 ±566.5 * | 795.4 ±544.9 | 76.7 ±17.6 ** | 51.4 ±15.6 * | 1457.6 ±108.8 ** | 6.0 ±9.1 ** | 79.2 ±68.0 |
| t | −2.20 | −0.37 | −3.09 | −2.11 | −6.62 | −3.81 | −0.52 |
| D | 0.51 | 0.08 | 0.71 | 0.49 | 1.50 | 1.26 | 0.04 |
| S3 | |||||||
| P1 (n = 43) | 1023.8 ±524.3 | 1928.3 ±1048.5 | 76.6 ±16.3 | 60.4 ±13.1 | 1588.5 ±75.0 | 0.1 ±0.3 | 95.2 ±82.0 |
| P2 (n = 40) | 1522.1 ±816.5 ** | 2177.8 ±1723.2 | 81.0 ±13.4 | 64.9 ±14.1 | 1511.4 ±89.1 ** | 6.1 ±10.1 ** | 84.8 ±67.2 |
| t | −3.33 | −0.80 | −1.33 | −1.52 | 4.27 | −3.97 | 0.63 |
| D | 0.74 | 0.18 | 0.30 | 0.33 | 0.94 | 1.15 | 0.14 |
| S4 | |||||||
| P1 (n = 36) | 4101.4 ±1733.2 | 2272.9 ±1146.8 | 106.7 ±25.8 | 81.8 ±16.2 | 1043.6 ±83.1 | 0.6 ±1.7 | 53.9 ±56.3 |
| P2 (n = 39) | 4476.8 ±2349.7 | 2398.5 ±1111.0 | 109.3 ±25.1 | 85.7 ±15.4 | 1027.2 ±72.8 | 3.3 ±4.8 ** | 46.5 ±50.0 |
| t | −0.78 | −0.48 | −0.45 | −1.05 | 0.91 | −3.21 | 0.61 |
| D | 0.18 | 0.11 | 0.10 | 0.25 | 0.21 | 0.83 | 0.14 |
| S5 | |||||||
| P1 (n = 42) | 4330.1 ±1140.4 | 1719.9 ±789.5 | 122.4 ±14.6 | 85.1 ±9.6 | 1347.8 ±108.7 | 0.7 ±2.1 | 95.4 ±82.9 |
| P2 (n = 35) | 4699.2 ±1593.9 | 1997.4 ±1204.3 | 127.3 ±17.6 | 88.1 ±13.3 | 1339.7 ±85.5 | 8.51 ±12.9 ** | 71.1 ±60.3 |
| t | −1.17 | −1.20 | −1.33 | −1.11 | 0.35 | −3.85 | 1.44 |
| D | 0.27 | 0.28 | 0.30 | 0.26 | 0.08 | 1.04 | 0.34 |
| S6 | |||||||
| P1 (n = 34) | 7568.7 ±4036.0 | 4012.3 ±3715.5 | 148.1 ±40.3 | 118.4 ±32.7 | 1277.0 ±106.1 | 0.1 ±0.3 | 84.7 ±78.9 |
| P2 (n = 42) | 6529.8 ±4667.4 | 2747.4 ±2800.9 | 130.3 ±46.9 | 101.3 ±35.5 * | 1295.8 ±74.2 | 3.3 ±6.7 ** | 78.6 ±67.4 |
| t | 1.01 | 1.67 | 1.73 | 2.13 | −0.90 | −2.88 | 0.36 |
| D | 0.24 | 0.39 | 0.41 | 0.50 | 0.21 | 0.91 | 0.08 |
| S7 | |||||||
| P1 (n = 43) | 23,603.9 ±5928.9 | 6291.4 ±2258.2 | 317.2 ±41.6 | 193.1 ±19.4 | 1483.3 ±91.6 | 0.6 ±1.7 | 103.1 ±92.0 |
| P2 (n = 35) | 15,732.1 ±4225.4 ** | 4639.7 ±2137.8 ** | 264.2 ±40.1 ** | 161.6 ±21.4 ** | 1434.6 ±95.2 * | 8.7 ±16.3 ** | 96.7 ±77.8 |
| t | 6.60 | 3.29 | 5.69 | 6.82 | 2.29 | −3.26 | 0.33 |
| D | 1.55 | 0.75 | 1.30 | 1.54 | 0.52 | 0.90 | 0.08 |
| Mean | |||||||
| P1 | 6403.9 ±8471.5 | 2542.7 ±2637.1 | 129.5 ±93.6 | 89.7 ±55.8 | 1310.9 ±219.7 | 0.4 ±1.3 | 87.5 ±79.1 |
| P2 | 4773.9 ±5352.5 | 2092.2 ±2062.3 | 116.9 ±68.8 | 82.2 ±42.3 | 1312.2 ±207.2 | 5.9 ±10.7 | 74.9 ±65.3 |
| Participants | Variables | First L-MIT in P1 | Last L-MIT in P1 | Last L-MIT in P2 |
|---|---|---|---|---|
| S1 | Pav [W] | 212 | 232 | 275 |
| HRav [BPM] | 142 | 141 | 143 | |
| Pav/HRav [W∙BPM−1] | 1.49 | 1.65 | 1.92 | |
| S2 | Pav [W] | 152 | 155 | 175 |
| HRav [BPM] | 149 | 146 | 150 | |
| Pav/HRav [W∙BPM−1] | 1.02 | 1.06 | 1.17 | |
| S3 | Pav [W] | 252 | 265 | 284 |
| HRav [BPM] | 151 | 142 | 142 | |
| Pav/HRav [W∙BPM−1] | 1.67 | 1.87 | 2.00 | |
| S4 | Pav [W] | 153 | 141 | 160 |
| HRav [BPM] | 145 | 141 | 152 | |
| Pav/HRav [W∙BPM−1] | 1.05 | 1.00 | 1.05 | |
| S5 | Pav [W] | 208 | 227 | 234 |
| HRav [BPM] | 157 | 155 | 155 | |
| Pav/HRav [W∙BPM−1] | 1.32 | 1.46 | 1.51 | |
| S6 | Pav [W] | 237 | 271 | 251 |
| HRav [BPM] | 157 | 160 | 152 | |
| Pav/HRav [W∙BPM−1] | 1.51 | 1.69 | 1.65 | |
| S7 | Pav [W] | 160 | 164 | 176 |
| HRav [BPM] | 142 | 146 | 141 | |
| Pav/HRav [W∙BPM−1] | 1.13 | 1.12 | 1.25 | |
| Mean | Pav [W] | 196.3 ± 41.4 | 207.9 ± 53.8 | 222.1 ± 51.3 * |
| HRav [BPM] | 149.0 ± 6.4 | 147.3 ± 7.4 | 147.9 ± 5.7 | |
| Pav/HRav [W∙BPM−1] | 1.31 ± 0.25 | 1.41 ± 0.35 | 1.51 ± 0.37 * |
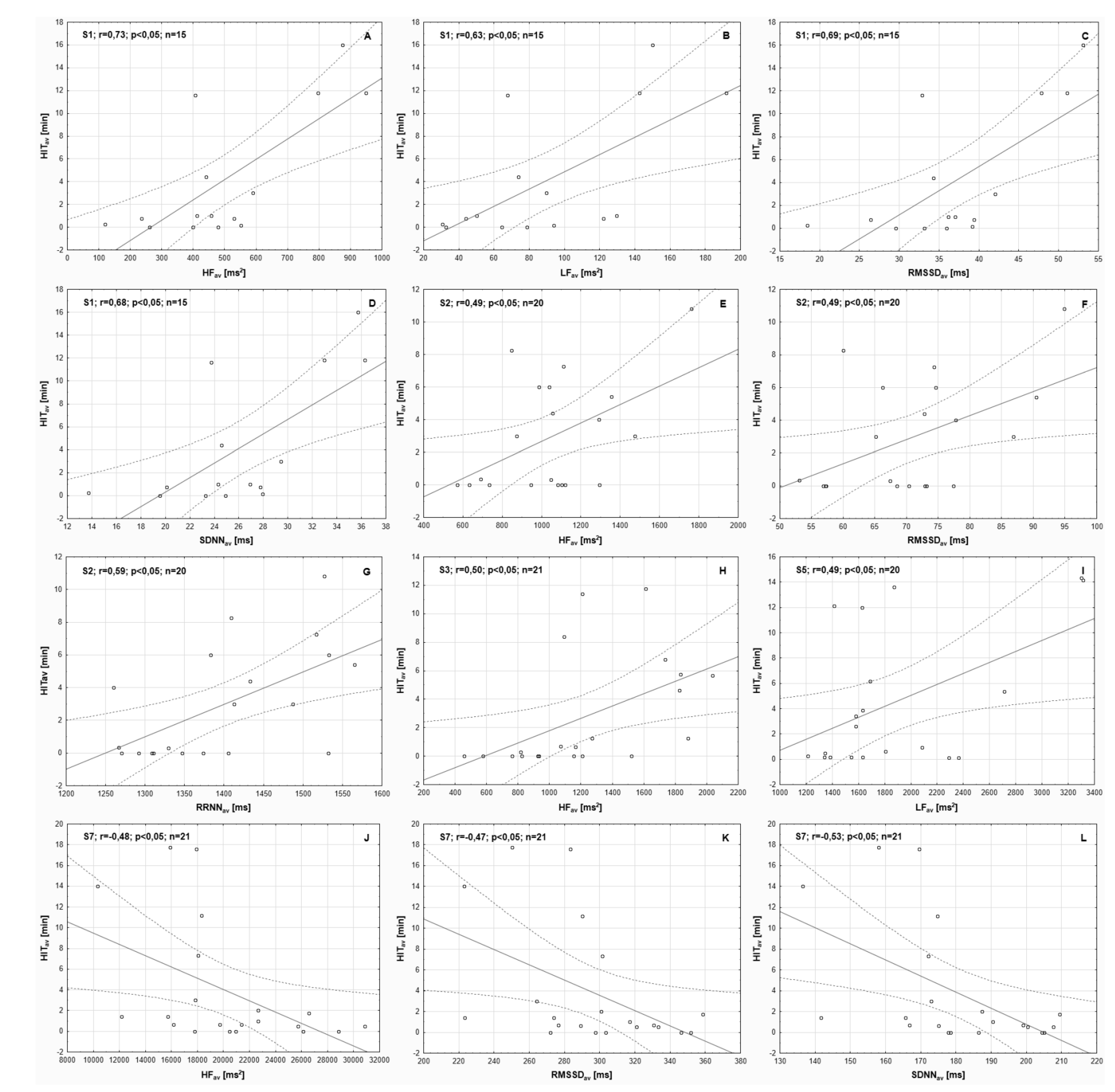
| Participants Training load | HFav [ms2] | LFav [ms2] | RMSSDav [ms] | SDNNav [ms] | RRNNav [ms] |
|---|---|---|---|---|---|
| S1 (n = 16) | |||||
| HITav [min] | 0.73 * | 0.63 * | 0.69 * | 0.68 * | 0.26 |
| L-MITav [min] | 0.04 | 0.23 | 0.00 | 0.04 | –0.45 |
| S2 (n = 20) | |||||
| HITav [min] | 0.49 * | 0.05 | 0.49 * | 0.38 | 0.59 * |
| L-MITav [min] | –0.11 | 0.11 | –0.21 | 0.03 | –0.39 |
| S3 (n = 21) | |||||
| HITav [min] | 0.50 * | 0.33 | 0.31 | 0.33 | –0.42 |
| L-MITav [min] | –0.11 | 0.18 | 0.06 | 0.24 | –0.23 |
| S4 (n = 23) | |||||
| HITav [min] | –0.14 | –0.07 | –0.07 | –0.10 | –0.18 |
| L-MITav [min] | 0.18 | –0.15 | 0.10 | 0.14 | 0.01 |
| S5 (n = 20) | |||||
| HITav [min] | 0.39 | 0.49 * | 0.33 | 0.40 | –0.30 |
| L-MITav [min] | 0.09 | –0.18 | 0.13 | 0.08 | 0.21 |
| S6 (n = 19) | |||||
| HITav [min] | –0.13 | –0.44 | –0.27 | –0.36 | 0.14 |
| L-MITav [min] | 0.19 | –0.11 | 0.28 | 0.23 | –0.38 |
| S7 (n = 21) | |||||
| HITav [min] | –0.48 * | –0.39 | –0.47 * | –0.53 * | –0.27 |
| L-MITav [min] | 0.04 | –0.14 | 0.14 | 0.07 | 0.38 |
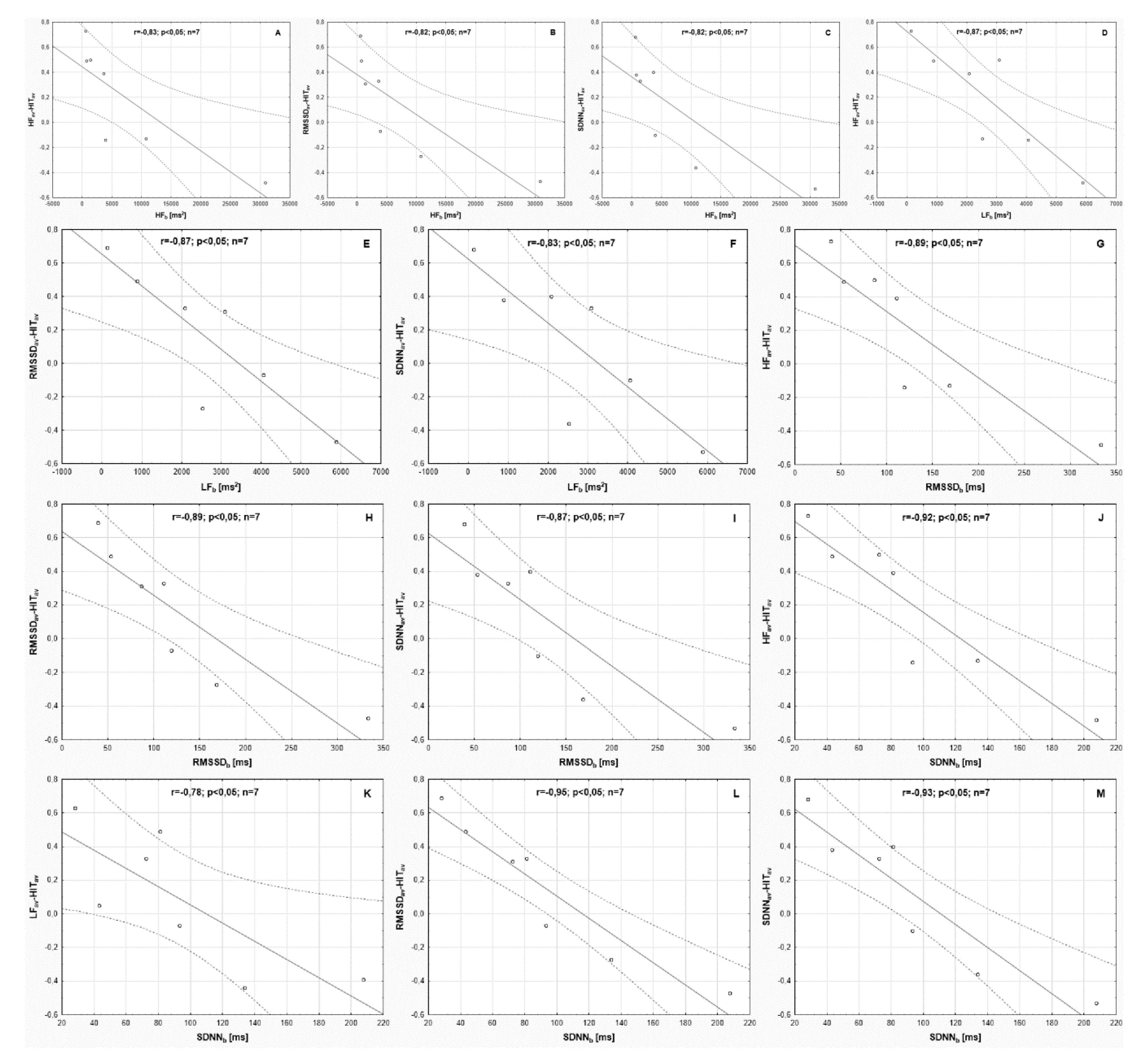
| Variables | HFav-HITav | LFav-HITav | RMSSDav-HITav | SDNNav-HITav | RRNNav-HITav |
|---|---|---|---|---|---|
| HFb [ms2] | –0.83 * | –0.69 | –0.82 * | –0.82 * | –0.31 |
| LFb [ms2] | –0.87 * | –0.64 | –0.87 * | –0.83 * | –0.67 |
| RMSSDb [ms] | –0.89 * | –0.72 | –0.89 * | –0.87 * | –0.42 |
| SDNNb [ms] | –0.92 * | –0.78 * | –0.95 * | –0.93 * | –0.44 |
| RRNNb [ms] | –0.15 | –0.14 | –0.25 | –0.21 | –0.57 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hebisz, P.; Hebisz, R.; Jastrzębska, A. An Attempt to Predict Changes in Heart Rate Variability in the Training Intensification Process among Cyclists. Int. J. Environ. Res. Public Health 2021, 18, 7636. https://doi.org/10.3390/ijerph18147636
Hebisz P, Hebisz R, Jastrzębska A. An Attempt to Predict Changes in Heart Rate Variability in the Training Intensification Process among Cyclists. International Journal of Environmental Research and Public Health. 2021; 18(14):7636. https://doi.org/10.3390/ijerph18147636
Chicago/Turabian StyleHebisz, Paulina, Rafał Hebisz, and Agnieszka Jastrzębska. 2021. "An Attempt to Predict Changes in Heart Rate Variability in the Training Intensification Process among Cyclists" International Journal of Environmental Research and Public Health 18, no. 14: 7636. https://doi.org/10.3390/ijerph18147636
APA StyleHebisz, P., Hebisz, R., & Jastrzębska, A. (2021). An Attempt to Predict Changes in Heart Rate Variability in the Training Intensification Process among Cyclists. International Journal of Environmental Research and Public Health, 18(14), 7636. https://doi.org/10.3390/ijerph18147636






