Can a Knee Brace Prevent ACL Reinjury: A Systematic Review
Abstract
1. Introduction
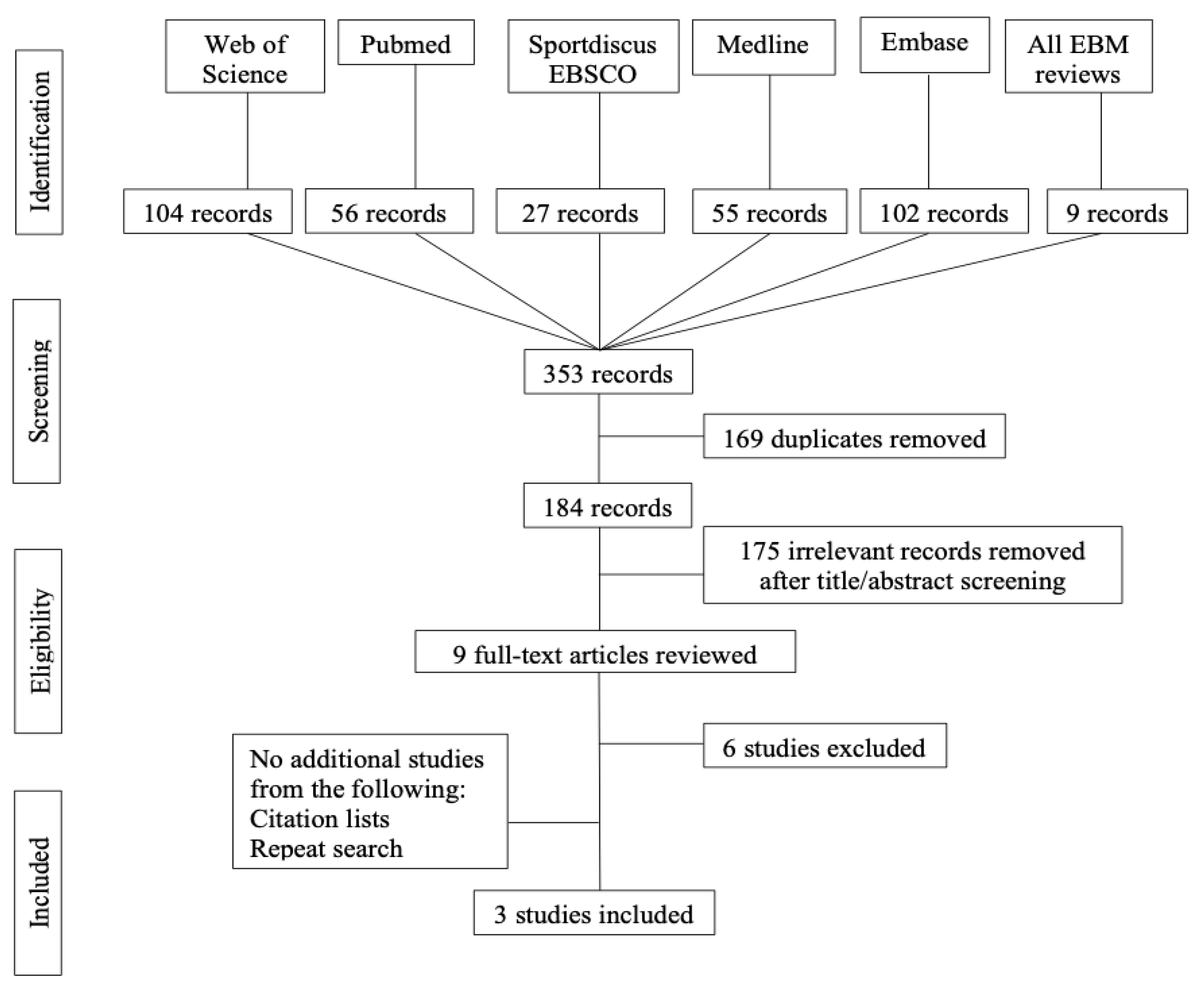
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
3. Results
3.1. Risk of bias assessment
3.2. Study Results
3.3. Subsequent Injuries
3.4. Compliance
3.5. Return to Sport Level
3.6. Quality of Life Questionnaires
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategies for the Systematic Review
| #1 | ACL | Anterior cruciate ligament[Mh] OR Anterior Cruciate Ligament Injuries[Mh] OR “Anterior cruciate ligament*”[tiab] OR “Anterior cruciate knee ligament*”[tiab] OR “ACL”[tiab] OR “cranial cruciate ligament*”[tiab] OR “Anterior cruciate ligament*”[OT] OR “Anterior cruciate knee ligament*”[OT] OR “ACL”[OT] OR “cranial cruciate ligament*”[OT] |
| #2 | Reconstruction | Surgery[sh] OR “Graft*”[tiab] OR “Allograft*”[tiab] OR “Autograft*”[tiab] OR “Reconstruct*”[tiab] OR “repair*”[tiab] OR “Surger*”[tiab] OR “Graft*”[OT] OR “Allograft*”[OT] OR “Autograft*”[OT] OR “Reconstruct*”[OT] OR “Surger*”[OT] OR “repair*”[OT] |
| #3 | Reconstruction ACL | Anterior Cruciate Ligament Reconstruction[Mh] |
| #4 | Orthotic | Braces[mh] OR Orthotic Devices[Mh:noexp] OR “Brace*”[tiab] OR “Bracing”[tiab] OR “Orthos*”[tiab] OR “Orthes*”[tiab] OR “Orthotic”[tiab] OR “Brace*”[OT] OR “Bracing”[OT] OR “Orthos*”[OT] OR “Orthes*”[OT] OR “Orthotic”[OT] |
| #5 | Second rupture | “Reinjur*”[tiab] OR “Re-injur*”[tiab] OR “Rerupture*”[tiab] OR “Re-rupture*”[tiab] OR “retear*”[tiab] OR “re-tear*”[tiab] OR “Graft failure*”[tiab] OR “Allograft failure*”[tiab] OR “Autograft failure*”[tiab] OR “Graft tear*”[tiab] OR “Allograft tear*”[tiab] OR “Autograft tear*”[tiab] OR “Graft injur*”[tiab] OR “Allograft injur*”[tiab] OR “Autograft injur*”[tiab] OR “Graft rupture*”[tiab] OR “Allograft rupture*”[tiab] OR “Autograft rupture*”[tiab] OR ((“Second*”[tiab] OR “contralateral”[tiab]) AND (“injur*”[tiab] OR “rupture*”[tiab] OR “tear*”[tiab])) OR “Reinjur*”[OT] OR “Re-injur*”[OT] OR “Rerupture*”[OT] OR “Re-rupture*”[OT] OR “retear*”[OT] OR “re-tear*”[OT] OR “Graft failure*”[OT] OR “Allograft failure*”[OT] OR “Autograft failure*”[OT] OR “Graft tear*”[OT] OR “Allograft tear*”[OT] OR “Autograft tear*”[OT] OR “Graft injur*”[OT] OR “Allograft injur*”[OT] OR “Autograft injur*”[OT] OR “Graft rupture*”[OT] OR “Allograft rupture*”[OT] OR “Autograft rupture*”[OT] OR ((“Second*”[OT] OR “contralateral”[OT]) AND (“injur*”[OT] OR “rupture*”[OT] OR “tear*”[OT])) |
| #6 | Combination and limitations | ((#1 AND #2) OR #3) AND #4 AND #5 AND (English[LA] OR French[LA]) 56 results |
| 1 | ACL | Anterior cruciate ligament/OR Anterior Cruciate Ligament Injuries/OR (Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*).ti,ab,kw,kf |
| 2 | Reconstruction | su.fs OR (Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*).ti,ab,kw,kf |
| 3 | Reconstruction ACL | Exp Anterior Cruciate Ligament Reconstruction/ |
| 4 | Orthotics | Braces/ OR Orthotic Devices/ OR (Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic).ti,ab,kw,kf |
| 5 | Second rupture | (Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))).ti,ab,kw,kf |
| 6 | Combination and limitations | ((1 AND 2) OR 3) AND 4 AND 5 AND (English OR French).lg 55 results |
| 1 | ACL | Anterior cruciate ligament/OR Anterior Cruciate Ligament Injuries/OR (Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*).ti,ab,kw,kf |
| 2 | Reconstruction | su.fs OR (Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*).ti,ab,kw,kf |
| 3 | Reconstruction ACL | Exp Anterior Cruciate Ligament Reconstruction/ |
| 4 | Orthotics | Braces/OR Orthotic Devices/OR (Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic).ti,ab,kw,kf |
| 5 | Second rupture | (Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))).ti,ab,kw,kf |
| 6 | Combination and limitations | ((1 AND 2) OR 3) AND 4 AND 5 AND (English OR French).lg 9 results |
| 1 | ACL | Anterior cruciate ligament/OR exp Anterior Cruciate Ligament Injury/OR (Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*).ti,ab,kw |
| 2 | Reconstruction | su.fs OR (Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*).ti,ab,kw |
| 3 | Reconstruction ACL | Anterior Cruciate Ligament Reconstruction/ |
| 4 | Orthotics | Exp knee orthosis/OR orthosis/OR brace/OR (Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic).ti,ab,kw |
| 5 | Second rupture | (Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))).ti,ab,kw |
| 6 | Combination and limitations | ((1 AND 2) OR 3) AND 4 AND 5 AND (English OR French).lg 102 results |
| S1 | ACL | DE(Anterior cruciate ligament) OR DE(Anterior Cruciate Ligament Injuries) OR TI(Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*) OR AB(Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*) OR KW(Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*) |
| S2 | Reconstruction | TI(Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*) OR AB(Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*) OR KW(Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*) |
| S3 | Reconstruction ACL | DE(Anterior cruciate ligament surgery) |
| S4 | Orthotics | DE(ORTHOPEDIC braces) OR DE(KNEE braces) OR TI(Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic) OR AB(Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic) OR KW(Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic) |
| S5 | Second rupture | TI(Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))) OR AB(Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))) OR KW(Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))) |
| S6 | Combination and limitations | ((S1 AND S2) OR S3) AND S4 AND S5 AND LA(English OR French) 27 results |
| #1 | ACL | TS = (Anterior cruciate ligament* OR Anterior cruciate knee ligament* OR ACL OR cranial cruciate ligament*) |
| #2 | Reconstruction | TS = (Graft* OR Allograft* OR Autograft* OR Reconstruct* OR repair* OR Surger*) |
| #3 | Orthotics | TS = (Brace* OR Bracing OR Orthos* OR Orthes* OR Orthotic) |
| #4 | Second rupture | TS = (Reinjur* OR Re-injur* OR Rerupture* OR Re-rupture* OR retear* OR re-tear* OR Graft failure* OR Allograft failure* OR Autograft failure* OR Graft tear* OR Allograft tear* OR Autograft tear* OR Graft injur* OR Allograft injur* OR Autograft injur* OR Graft rupture* OR Allograft rupture* OR Autograft rupture* OR ((Second* OR contralateral) AND (injur* OR rupture* OR tear*))) |
| #5 | Combination and limitations | #1 AND #2 AND #3 AND #4 AND LANGUAGE:(English OR French) 104 results |
References
- Frank, C.B.; Jackson, D.W. The science of reconstruction of the anterior cruciate ligament. J. Bone Jt. Surg. Am. 1997, 79, 1556–1576. [Google Scholar] [CrossRef]
- Perrone, G.S.; Webster, K.E.; Imbriaco, C.; Portilla, G.M.; Vairagade, A.; Murray, M.M.; Kiapour, A.M. Risk of Secondary ACL Injury in Adolescents Prescribed Functional Bracing after ACL Reconstruction. Orthop. J. Sports Med. 2019, 7, 2325967119879880. [Google Scholar] [CrossRef]
- Prodromos, C.C.; Han, Y.; Rogowski, J.; Joyce, B.; Shi, K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy 2007, 23, 1320–1325.e6. [Google Scholar] [CrossRef]
- Ahldén, M.; Samuelsson, K.; Sernert, N.; Forssblad, M.; Karlsson, J.; Kartus, J. The Swedish National Anterior Cruciate Ligament Register: A report on baseline variables and outcomes of surgery for almost 18,000 patients. Am. J. Sports Med. 2012, 40, 2230–2235. [Google Scholar] [CrossRef]
- Griffin, L.Y.; Albohm, M.J.; Arendt, E.A.; Bahr, R.; Beynnon, B.D.; DeMaio, M.; Dick, R.W.; Engebretsen, L.; Garrett, W.E.; Hannafin, J.A.; et al. Understanding and preventing noncontact anterior cruciate ligament injuries: A review of the Hunt Valley II meeting, January 2005. Am. J. Sports Med. 2006, 34, 1512–1532. [Google Scholar] [CrossRef]
- Grindem, H.; Snyder-Mackler, L.; Moksnes, H.; Engebretsen, L.; Risberg, M.A. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. Br. J. Sports Med. 2016, 50, 804–808. [Google Scholar] [CrossRef]
- Law, M.A.; Ko, Y.A.; Miller, A.L.; Lauterbach, K.N.; Hendley, C.L.; Johnson, J.E.; Tsai, L.C. Age, rehabilitation and surgery characteristics are re-injury risk factors for adolescents following anterior cruciate ligament reconstruction. Phys. Ther. Sport 2021, 49, 196–203. [Google Scholar] [CrossRef]
- Dai, B.; Butler, R.J.; Garrett, W.E.; Queen, R.M. Anterior cruciate ligament reconstruction in adolescent patients: Limb asymmetry and functional knee bracing. Am. J. Sports Med. 2012, 40, 2756–2763. [Google Scholar] [CrossRef]
- Sharafoddin-Shirazi, F.; Letafatkar, A.; Hogg, J.; Saatchian, V. Biomechanical asymmetries persist after ACL reconstruction: Results of a 2-year study. J. Exp. Orthop. 2020, 7, 86. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; Feller, J.A. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 2827–2832. [Google Scholar] [CrossRef]
- Filbay, S.R.; Ackerman, I.N.; Dhupelia, S.; Arden, N.K.; Crossley, K.M. Quality of Life in Symptomatic Individuals After Anterior Cruciate Ligament Reconstruction, With and Without Radiographic Knee Osteoarthritis. J. Orthop. Sports Phys. Ther. 2018, 48, 398–408. [Google Scholar] [CrossRef]
- Johnson, C.C.; Garcia, G.H.; Garner, M.R.; Marx, R.G. Quality of Life Following ACL Reconstruction: Baseline Predictors of Patient-Reported Outcomes. HSS J. 2016, 12, 94–97. [Google Scholar] [CrossRef]
- Bates, N.A.; Hewett, T.E. Motion Analysis and the Anterior Cruciate Ligament: Classification of Injury Risk. J. Knee Surg. 2016, 29, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Ong, T.Y.; Fu, S.C.; Yung, S.H. Prevalence of patellofemoral joint osteoarthritis after anterior cruciate ligament injury and associated risk factors: A systematic review. J. Orthop. Translat. 2019, 22, 14–25. [Google Scholar] [CrossRef]
- Mancuso, F.; Dodd, C.A.; Murray, D.W.; Pandit, H. Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J. Orthop. Traumatol. 2016, 17, 267–275. [Google Scholar] [CrossRef]
- Lindanger, L.; Strand, T.; Mølster, A.O.; Solheim, E.; Inderhaug, E. Return to Play and Long-term Participation in Pivoting Sports After Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2019, 47, 3339–3346. [Google Scholar] [CrossRef] [PubMed]
- Longstaffe, R.; Leiter, J.; Gurney-Dunlop, T.; McCormack, R.; MacDonald, P. Return to Play and Career Length After Anterior Cruciate Ligament Reconstruction Among Canadian Professional Football Players. Am. J. Sports Med. 2020, 48, 1682–1688. [Google Scholar] [CrossRef]
- Waldén, M.; Hägglund, M.; Magnusson, H.; Ekstrand, J. ACL injuries in men’s professional football: A 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br. J. Sports Med. 2016, 50, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef]
- Kvist, J.; Ek, A.; Sporrstedt, K.; Good, L. Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2005, 13, 393–397. [Google Scholar] [CrossRef] [PubMed]
- White, K.; Di Stasi, S.L.; Smith, A.H.; Snyder-Mackler, L. Anterior cruciate ligament- specialized post-operative return-to-sports (ACL-SPORTS) training: A randomized control trial. BMC Musculoskelet. Disord. 2013, 14, 108. [Google Scholar] [CrossRef]
- Beynnon, B.D.; Johnson, R.J.; Fleming, B.C.; Peura, G.D.; Renstrom, P.A.; Nichols, C.E.; Pope, M.H. The effect of functional knee bracing on the anterior cruciate ligament in the weightbearing and nonweightbearing knee. Am. J. Sports Med. 1997, 25, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Beynnon, B.D.; Fleming, B.C.; Churchill, D.L.; Brown, D. The effect of anterior cruciate ligament deficiency and functional bracing on translation of the tibia relative to the femur during nonweightbearing and weightbearing. Am. J. Sports Med. 2003, 31, 99–105. [Google Scholar] [CrossRef]
- Cawley, P.W.; France, E.P.; Paulos, L.E. Comparison of rehabilitative knee braces. A biomechanical investigation. Am. J. Sports Med. 1989, 17, 141–146. [Google Scholar] [CrossRef]
- Paulos, L.E.; France, E.P.; Rosenberg, T.D.; Jayaraman, G.; Abbott, P.J.; Jaen, J. The biomechanics of lateral knee bracing. Part I: Response of the valgus restraints to loading. Am. J. Sports Med. 1987, 15, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Rishiraj, N.; Taunton, J.E.; Lloyd-Smith, R.; Woollard, R.; Regan, W.; Clement, D.B. The potential role of prophylactic/functional knee bracing in preventing knee ligament injury. Sports Med. 2009, 39, 937–960. [Google Scholar] [CrossRef]
- Smith, S.D.; Laprade, R.F.; Jansson, K.S.; Arøen, A.; Wijdicks, C.A. Functional bracing of ACL injuries: Current state and future directions. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1131–1141. [Google Scholar] [CrossRef]
- Decoster, L.C.; Vailas, J.C. Functional anterior cruciate ligament bracing: A survey of current brace prescription patterns. Orthopedics 2003, 26, 701–706. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- McDevitt, E.R.; Taylor, D.C.; Miller, M.D.; Gerber, J.P.; Ziemke, G.; Hinkin, D.; Uhorchak, J.M.; Arciero, R.A.; St Pierre, P. Functional bracing after anterior cruciate ligament reconstruction: A prospective, randomized, multicenter study. Am. J. Sports Med. 2004, 32, 1887–1892. [Google Scholar] [CrossRef]
- MARS Group. Rehabilitation Predictors of Clinical Outcome Following Revision ACL Reconstruction in the MARS Cohort. J. Bone Jt. Surg. Am. 2019, 101, 779–786. [Google Scholar] [CrossRef]
- Higgins, L.D.; Taylor, M.K.; Park, D.; Ghodadra, N.; Marchant, M.; Pietrobon, R.; Cook, C. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Jt. Bone Spine 2007, 74, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Roos, E.M.; Roos, H.P.; Lohmander, L.S.; Ekdahl, C.; Beynnon, B.D. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J. Orthop. Sports Phys. Ther. 1998, 28, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.G.; Stump, T.J.; Jones, E.C.; Wickiewicz, T.L.; Warren, R.F. Development and evaluation of an activity rating scale for disorders of the knee. Am. J. Sports Med. 2001, 29, 213–218. [Google Scholar] [CrossRef]
- Dickerson, L.C.; Peebles, A.T.; Moskal, J.T.; Miller, T.K.; Queen, R.M. Physical Performance Improves with Time and a Functional Knee Brace in Athletes after ACL Reconstruction. Orthop. J. Sports Med. 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Focke, A.; Steingrebe, H.; Möhler, F.; Ringhof, S.; Sell, S.; Potthast, W.; Stein, T. Effect of Different Knee Braces in ACL-Deficient Patients. Front. Bioeng. Biotechnol. 2020, 8, 964. [Google Scholar] [CrossRef]
- Hanzlíková, I.; Richards, J.; Hébert-Losier, K.; Smékal, D. The effect of proprioceptive knee bracing on knee stability after anterior cruciate ligament reconstruction. Gait Posture 2019, 67, 242–247. [Google Scholar] [CrossRef]
- Hewlett, J.; Kenney, J. Innovations in functional and rehabilitative knee bracing. Ann. Transl. Med. 2019, 7 (Suppl. 7), S248. [Google Scholar] [CrossRef]
- Lowe, W.R.; Warth, R.J.; Davis, E.P.; Bailey, L. Functional Bracing After Anterior Cruciate Ligament Reconstruction: A Systematic Review. J. Am. Acad. Orthop. Surg. 2017, 25, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.G.; Feng, J.T.; He, X.; Wang, F.; Hu, Y.C. The effect of knee bracing on the knee function and stability following anterior cruciate ligament reconstruction: A systematic review and meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2019, 105, 1107–1114. [Google Scholar] [CrossRef]
- Di Miceli, R.; Marambio, C.B.; Zati, A.; Monesi, R.; Benedetti, M.G. Do Knee Bracing and Delayed Weight Bearing Affect Mid-Term Functional Outcome after Anterior Cruciate Ligament Reconstruction? Joints 2017, 5, 202–206. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Möller, E.; Forssblad, M.; Hansson, L.; Wange, P.; Weidenhielm, L. Bracing versus nonbracing in rehabilitation after anterior cruciate ligament reconstruction: A randomized prospective study with 2-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2001, 9, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Styf, J.R.; Lundin, O.; Gershuni, D.H. Effects of a functional knee brace on leg muscle function. Am. J. Sports Med. 1994, 22, 830–834. [Google Scholar] [CrossRef]
- Pietrosimone, B.G.; Grindstaff, T.L.; Linens, S.W.; Uczekaj, E.; Hertel, J. A systematic review of prophylactic braces in the prevention of knee ligament injuries in collegiate football players. J Athl. Train. 2008, 43, 409–415. [Google Scholar] [CrossRef]
- Maletis, G.B.; Inacio, M.C.; Funahashi, T.T. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am. J. Sports Med. 2015, 43, 641–647. [Google Scholar] [CrossRef]
- Schilaty, N.D.; Nagelli, C.; Bates, N.A.; Sanders, T.L.; Krych, A.J.; Stuart, M.J.; Hewett, T.E. Incidence of Second Anterior Cruciate Ligament Tears and Identification of Associated Risk Factors From 2001 to 2010 Using a Geographic Database. Orthop. J. Sports Med. 2017, 5. [Google Scholar] [CrossRef]
| Inclusion | Exclusion |
|---|---|
|
|
| Risk of Bias for Included Randomized Trials | |||||||
|---|---|---|---|---|---|---|---|
| Study | Random Sequence Generation | Allocation Concealment | Blinding of Subject/Personnel | Blinding Outcomes Assessment | Attrition | Selective Reporting | Overall |
| McDevitt et al., 2004 | Intermediate | Low | Intermediate | Intermediate | Low | Low | Intermediate |
| Risk of Bias for Included Nonrandomized Trials | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | Confounding | Subject Selection | Intervention Measurement | Departure From Intended Intervention | Attrition | Outcomes Measureent | Selective Reporting | Overall |
| Perrone et al., 2019 | Intermediate | Low | Low | Low | Low | Low | Low | Intermediate |
| MARS Group, 2019 | Low | Low | Intermediate | Low | Intermediate | Low | Low | Intermediate |
| KERRYPNX | Total ACLR | Total Re-Tears (n (%)) | p Value |
|---|---|---|---|
| (n = 1196) | (n = 73) | ||
| McDevitt et al., 2004 | >0.05 | ||
| Braced | 47 | 2 (4.3) | |
| Unbraced | 48 | 3 (6.3) | |
| Perrone et al., 2019 | 0.03 | ||
| Braced | 135 | 14 (10) | |
| Unbraced | 140 | 29 (21) | |
| MARS Group, 2019 | 0.23 | ||
| Braced | 253 | 5 (2) | |
| Unbraced | 573 | 20 (3.5) |
| Study | LOE | Dependent Variable | No of Patients (Males/Females) | Mean Age in Year (Range) | Reconstruction Technique | Follow Up | Outcomes Measured |
|---|---|---|---|---|---|---|---|
| McDevitt et al., 2004 | II | Clinical and functional outcomes | Brace: 47 No brace: 48 | NR: military personnel | BPTB autograph | Minimum 2 years | Subjective: IKDC, Lysholm Objective: Lachman, pivot shift, IKDC, functionl tests |
| Perrone et al., 2019 | II | Risk for future knee injury | Brace: 135 (31/104) No brace: 140 (86/54) | Brace: 15.8 ± 1.5 No brace: 17.2 ± 1.8 | Hamstring autograft | Minimum 3 years | Subjective: Marx activity score Objective: pivot shift, Lachman, MRI |
| MARS Group, 2019 | III | Clinical and functional outcomes | Brace: 253 No Brace: 590 (482/361) | 28.9 ± 10.5 | BPTB/Hamstring Autograph/Allograft | 2 years | Subjective: KOOS, IKDC, Marx activity scores Objective: subsequent ipsilateral knee surgery |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marois, B.; Tan, X.W.; Pauyo, T.; Dodin, P.; Ballaz, L.; Nault, M.-L. Can a Knee Brace Prevent ACL Reinjury: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7611. https://doi.org/10.3390/ijerph18147611
Marois B, Tan XW, Pauyo T, Dodin P, Ballaz L, Nault M-L. Can a Knee Brace Prevent ACL Reinjury: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(14):7611. https://doi.org/10.3390/ijerph18147611
Chicago/Turabian StyleMarois, Bianca, Xue Wei Tan, Thierry Pauyo, Philippe Dodin, Laurent Ballaz, and Marie-Lyne Nault. 2021. "Can a Knee Brace Prevent ACL Reinjury: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 14: 7611. https://doi.org/10.3390/ijerph18147611
APA StyleMarois, B., Tan, X. W., Pauyo, T., Dodin, P., Ballaz, L., & Nault, M.-L. (2021). Can a Knee Brace Prevent ACL Reinjury: A Systematic Review. International Journal of Environmental Research and Public Health, 18(14), 7611. https://doi.org/10.3390/ijerph18147611






