Health-Related Productivity Loss According to Health Conditions among Workers in South Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Health Conditions
2.3. Measurement of Health-Related Productivity Loss
2.4. Measurement of Other Variables
2.5. Statistical Analysis
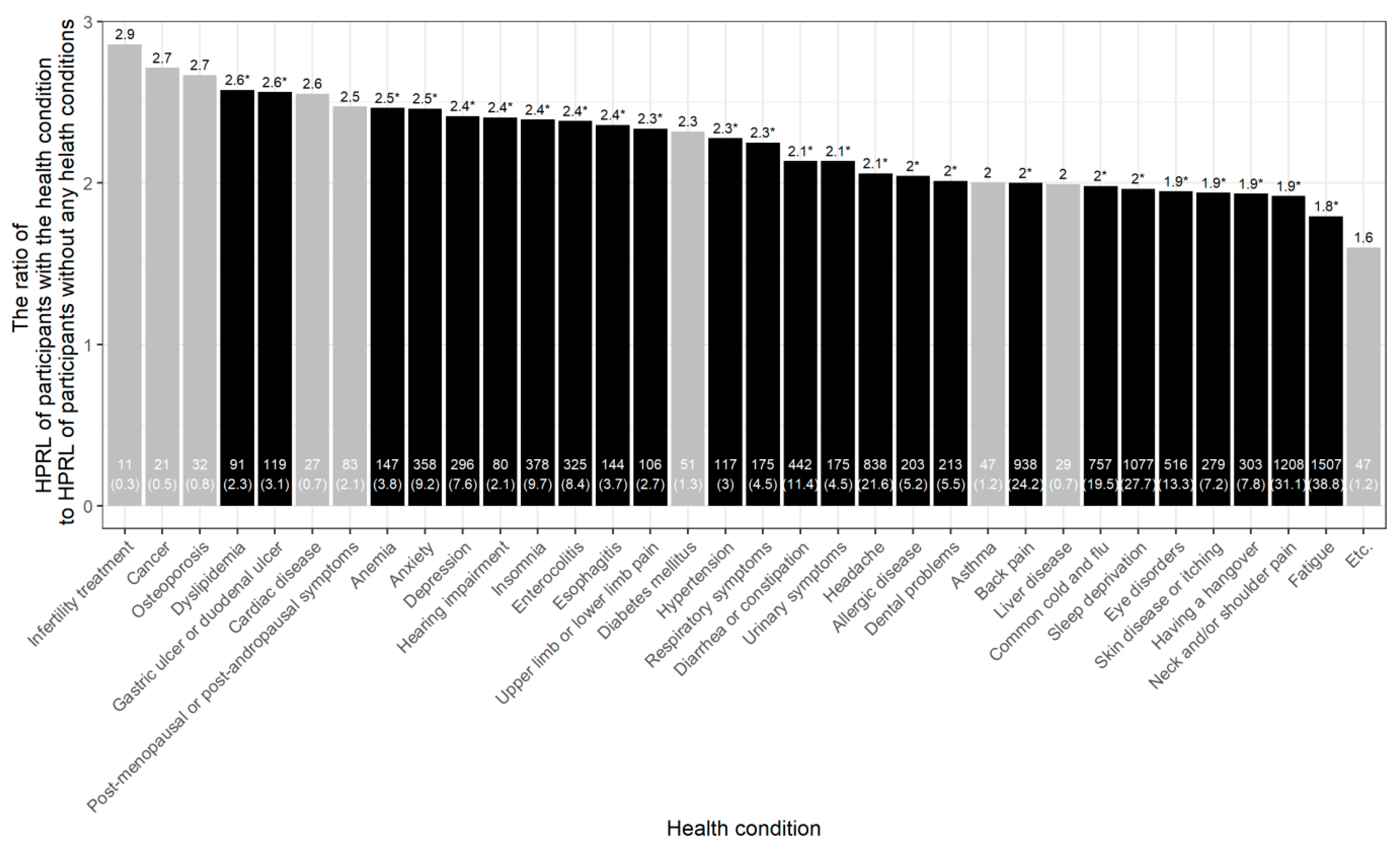
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Koopmanschap, M.; Burdorf, A.; Jacob, K.; Meerding, W.J.; Brouwer, W.; Severens, H. Measuring Productivity Changes in Economic Evaluation: Setting the Research Agenda. Pharmacoeconomics 2005, 23, 47–54. [Google Scholar] [CrossRef]
- Fouad, A.M.; Waheed, A.; Gamal, A.; Amer, S.A.; Abdellah, R.F.; Shebl, F.M. Effect of Chronic Diseases on Work Productivity: A Propensity Score Analysis. J. Occup. Environ. Med. 2017, 59, 480–485. [Google Scholar] [CrossRef]
- Schultz, A.B.; Chen, C.-Y.; Edington, D.W. The Cost and Impact of Health Conditions on Presenteeism to Employers: A Review of the Literature. Pharmacoeconomics 2009, 27, 365–378. [Google Scholar] [CrossRef]
- Oliva-Moreno, J. Loss of Labour Productivity Caused by Disease and Health Problems: What is the Magnitude of Its Effect on Spain’s Economy? Eur. J. Health Econ. 2012, 13, 605–614. [Google Scholar] [CrossRef] [PubMed]
- Loeppke, R.; Taitel, M.; Haufle, V.; Parry, T.; Kessler, R.C.; Jinnett, K. Health and Productivity as a Business Strategy: A Multiemployer Study. J. Occup. Environ. Med. 2009, 51, 411–428. [Google Scholar] [CrossRef]
- Nagata, T.; Mori, K.; Ohtani, M.; Nagata, M.; Kajiki, S.; Fujino, Y.; Matsuda, S.; Loeppke, R. Total Health-Related Costs Due to Absenteeism, Presenteeism, and Medical and Pharmaceutical Expenses in Japanese Employers. J. Occup. Environ. Med. 2018, 60, e273–e280. [Google Scholar] [CrossRef] [PubMed]
- Loeppke, R.; Taitel, M.; Richling, D.; Parry, T.; Kessler, R.C.; Hymel, P.; Konicki, D. Health and productivity as a business strategy. J. Occup. Environ. Med. 2007, 49, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Chimed-Ochir, O.; Nagata, T.; Nagata, M.; Kajiki, S.; Mori, K.; Fujino, Y. Potential Work Time Lost Due to Sickness Absence and Presence Among Japanese Workers. J. Occup. Environ. Med. 2019, 61, 682–688. [Google Scholar] [CrossRef]
- Wee, L.H.; Yeap, L.L.L.; Chan, C.M.H.; Wong, J.E.; Jamil, N.A.; Nantha, Y.S.; Siau, C.S. Anteceding Factors Predicting Absenteeism and Presenteeism in Urban Area in Malaysia. BMC Public Health 2019, 19, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Bialowolski, P.; McNeely, E.; VanderWeele, T.J.; Weziak-Bialowolska, D. Ill Health and Distraction at Work: Costs and Drivers for Productivity Loss. PLoS ONE 2020, 15, e0230562. [Google Scholar] [CrossRef]
- Dewa, C.S.; Loong, D.; Bonato, S.; Hees, H. Incidence Rates of Sickness Absence Related to Mental Disorders: A Systematic Literature Review. BMC Public Health 2014, 14, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wynne-Jones, G.; Cowen, J.; Jordan, J.L.; Uthman, O.; Main, C.J.; Glozier, N.; Van Der Windt, D. Absence from Work and Return to Work in People with Back Pain: A Systematic Review and Meta-Analysis. Occup. Environ. Med. 2014, 71, 448–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, J.G.; Nagar, S.P.; Dalal, A.A. Indirect costs in chronic obstructive pulmonary disease: A Review of the Economic Burden on Employers and Individuals in the United States. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 289–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadatsafavi, M.; Rousseau, R.; Chen, W.; Zhang, W.; Lynd, L.; FitzGerald, J.M. The Preventable Burden of Productivity Loss Due to Suboptimal Asthma Control: A Population-Based Study. Chest 2014, 145, 787–793. [Google Scholar] [CrossRef]
- Zhang, W.; Bansback, N.; Kopec, J.; Anis, A.H. Measuring Time Input Loss among Patients with Rheumatoid Arthritis: Validity and Reliability of the Valuation of Lost Productivity Questionnaire. J. Occup. Environ. Med. 2011, 53, 530–536. [Google Scholar] [CrossRef]
- Zhang, W.; McLeod, C.; Koehoorn, M. The Relationship between Chronic Conditions and Absenteeism and Associated Costs in Canada. Scand. J. Work Environ. Health 2016, 42, 413–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brouwer, W.B.; Koopmanschap, M.A.; Rutten, F.F. Productivity Losses without Absence: Measurement Validation and Empirical Evidence. Health Policy 1999, 48, 13–27. [Google Scholar] [CrossRef]
- Reilly, M.C.; Zbrozek, A.S.; Dukes, E.M. The Validity and Reproducibility of a Work Productivity and Activity Impairment Instrument. Pharmacoeconomics 1993, 4, 353–365. [Google Scholar] [CrossRef]
- Reilly Associates. WPAI Translations. Available online: http://www.reillyassociates.net/WPAI_Translations.html (accessed on 13 April 2021).
- Lee, K. Gender-Specific Relationships between Alcohol Drinking Patterns and Metabolic Syndrome: The Korea National Health and Nutrition Examination Survey 2008. Public Health Nutr. 2012, 15, 1917–1924. [Google Scholar] [CrossRef] [Green Version]
- Green, J.A. Too Many Zeros and/or Highly Skewed? A Tutorial on Modelling Health Behaviour as Count Data with Poisson and Negative Binomial Regression. Health Psychol. Behav. Med. 2021, 9, 436–455. [Google Scholar] [CrossRef]
- Besen, E.; Pranksy, G. Assessing the Relationship between Chronic Health Conditions and Productivity Loss Trajectories. J. Occup. Environ. Med. 2014, 56, 1249–1257. [Google Scholar] [CrossRef] [Green Version]
- Van Den Heuvel, S.G.; Geuskens, G.A.; Hooftman, W.E.; Koppes, L.L.J.; Van Den Bossche, S.N.J. Productivity Loss at Work; Health-Related and Work-Related Factors. J. Occup. Rehabil. 2010, 20, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Allen, D.; Hines, E.W.; Pazdernik, V.; Konecny, L.T.; Breitenbach, E. Four-Year Review of Presenteeism Data among Employees of a Large United States Health Care System: A Retrospective Prevalence Study. Hum. Resour. Health 2018, 16, 59. [Google Scholar] [CrossRef] [Green Version]
- Sagherian, K.; Unick, G.J.; Zhu, S.; Derickson, D.; Hinds, P.S.; Geiger-Brown, J. Acute Fatigue Predicts Sickness Absence in the Workplace: A 1-Year Retrospective Cohort Study in Paediatric Nurses. J. Adv. Nurs. 2017, 73, 2933–2941. [Google Scholar] [CrossRef]
- Keller, S.M. Effects of Extended Work Shifts and Shift Work on Patient Safety, Productivity, and Employee Health. AAOHN J. 2009, 57, 497–504. [Google Scholar] [CrossRef] [Green Version]
- Wadsworth, E.J.K.; Allen, P.H.; Wellens, B.T.; McNamara, R.L.; Smith, A.P. Patterns of Fatigue among Seafarers during a Tour of Duty. Am. J. Ind. Med. 2006, 49, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, M.; Tornqvist, E.W.; Toomingas, A. Self-Reported Reduced Productivity Due to Musculoskeletal Symptoms: Associations with Workplace and Individual Factors among White-Collar Computer Users. J. Occup. Rehabil. 2002, 12, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Meerding, W.J.; IJzelenberg, W.; Koopmanschap, M.A.; Severens, J.L.; Burdorf, A. Health Problems Lead to Considerable Productivity Loss at Work among Workers with High Physical Load Jobs. J. Clin. Epidemiol. 2005, 58, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.; Reed, J.I.; Massarotti, E.; Wester, L.M.; Burke, T.A. The Work Limitations Questionnaire’s Validity and Reliability among Patients with Osteoarthritis. J. Clin. Epidemiol. 2002, 55, 197–208. [Google Scholar] [CrossRef]
- Stewart, W.F.; Ricci, J.A.; Chee, E.; Morganstein, D.; Lipton, R. Lost Productive Time and Cost Due to Common Pain Conditions in the US Workforce. JAMA 2003, 290, 2443–2454. [Google Scholar] [CrossRef] [Green Version]
- Bernstrøm, V.H.; Houkes, I. A systematic Literature Review of the Relationship between Work Hours and Sickness Absence. Work Stress 2018, 32, 84–104. [Google Scholar] [CrossRef]
- Barnes, M.; Sax, P.E. Challenges of “Return to Work” in an Ongoing Pandemic. N. Engl. J. Med. 2020, 383, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Schultz, A.B.; Edington, D.W. Employee Health and Presenteeism: A Systematic Review. J. Occup. Rehabil. 2007, 17, 547–579. [Google Scholar] [CrossRef]
- Druss, B.G.; Schlesinger, M.; Allen, H.M., Jr. Depressive Symptoms, Satisfaction with Health Care, and 2-Year Work Outcomes in an Employed Population. Am. J. Psychiatry 2001, 158, 731–734. [Google Scholar] [CrossRef]
- Kim, H.-Y.; Choi, J.; Lim, H.-M.; Park, C.; Hong, Y.-C. The Association between Non-Regular Work Patterns and Insomnia among Korean Wage Workers: The Fifth Korean Working Condition Survey. Ann. Occup. Environ. Med. 2021, 33, e9. [Google Scholar] [CrossRef]
- Lee, H.-E.; Kim, M.-H.; Choi, M.; Kim, H.-R.; Kawachi, I. Variability in Daily or Weekly Working Hours and Self-Reported Mental Health Problems in Korea, Korean Working Condition Survey, 2017. Arch. Public Health 2021, 79, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Burton, J. WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]

| Total | Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HRPL (%) | HRPL (%) | HRPL (%) | |||||||
| n (%) | Mean | SD | n (%) | Mean | SD | n (%) | Mean | SD | |
| Total | 3882 (100) | 26.6 | 26.7 | 1944 (50.1) | 24.5 | 25.6 ** | 1938 (49.9) | 28.7 | 27.5 |
| Age | |||||||||
| 20–29 | 948 (24.4) | 30.0 | 27.6 ** | 400 (20.6) | 27.3 | 26.9 * | 548 (28.3) | 32.0 | 27.9 ** |
| 30–39 | 1098 (28.3) | 28.5 | 26.7 | 565 (29.1) | 25.1 | 25.5 | 533 (27.5) | 32.1 | 27.5 |
| 40–49 | 1117 (28.8) | 25.0 | 26.5 | 584 (30) | 24.2 | 25.8 | 533 (27.5) | 26.0 | 27.2 |
| 50–59 | 522 (13.5) | 21.8 | 24.8 | 278 (14.3) | 21.7 | 23.4 | 244 (12.6) | 21.8 | 26.3 |
| ≥60~ | 197 (5.1) | 21.5 | 24.2 | 117 (6.0) | 20.2 | 24.3 | 80 (4.1) | 23.5 | 24.2 |
| Education | |||||||||
| ≤High school | 748 (19.3) | 26.9 | 26.9 | 339 (17.4) | 25.3 | 26.0 | 409 (21.1) | 28.3 | 27.5 |
| College or University | 2750 (70.8) | 26.7 | 26.5 | 1399 (72.0) | 25.0 | 25.7 | 1351 (69.7) | 28.5 | 27.3 |
| Graduate school | 384 (9.9) | 25.3 | 27.0 | 206 (10.6) | 19.8 | 23.6 | 178 (9.2) | 31.6 | 29.3 |
| Annual Household income (KRW, million) | |||||||||
| 1st Tercile (–30) | 1276 (32.9) | 29.7 | 27.4 ** | 582 (29.9) | 29.9 | 27.5 ** | 694 (35.8) | 29.6 | 27.4 |
| 2nd Tercile (30–50) | 1311 (33.8) | 25.7 | 26.1 | 707 (36.4) | 23.3 | 24.9 | 604 (31.2) | 28.5 | 27.1 |
| 3rd Tercile (51–75) | 1295 (33.4) | 24.5 | 26.2 | 655 (33.7) | 21.0 | 23.7 | 640 (33.0) | 28.0 | 28.1 |
| Marital status | |||||||||
| Single | 1845 (47.5) | 28.7 | 26.9 ** | 834 (42.9) | 27.3 | 26.7 ** | 1011 (52.2) | 29.9 | 27.1 |
| Married | 1870 (48.2) | 24.7 | 26.3 | 1051 (54.1) | 22.2 | 24.4 | 819 (42.3) | 27.9 | 28.2 |
| Separated | 46 (1.2) | 33.2 | 30.0 | 14 (0.7) | 41.6 | 28.5 | 32 (1.7) | 29.5 | 30.3 |
| Widowed | 25 (0.6) | 19.4 | 22.1 | 6 (0.3) | 13.3 | 19.7 | 19 (1.0) | 21.4 | 23.0 |
| Divorced | 96 (2.5) | 21.7 | 24.0 | 39 (2.0) | 22.5 | 24.4 | 57 (2.9) | 21.1 | 23.9 |
| Employment status | |||||||||
| Regular | 3480 (89.6) | 26.3 | 26.5 | 1787 (91.9) | 24.0 | 25.4 * | 1693 (87.4) | 28.8 | 27.4 |
| Temporary | 310 (8.0) | 27.9 | 27.3 | 118 (6.1) | 28.3 | 26.2 | 192 (9.9) | 27.7 | 28.1 |
| Day labourer | 92 (2.4) | 32.0 | 30.4 | 39 (2.0) | 34.7 | 29.8 | 53 (2.7) | 30.1 | 30.9 |
| Occupation | |||||||||
| White collar | 2538 (65.4) | 26.3 | 26.4 | 1257 (64.7) | 23.8 | 25.3 | 1281 (66.1) | 28.7 | 27.3 |
| Blue collar | 1344 (34.6) | 27.2 | 27.1 | 687 (35.3) | 25.8 | 26.1 | 657 (33.9) | 28.7 | 28.0 |
| Weekly working hours | |||||||||
| <40 h/week | 552 (14.2) | 27.0 | 27.9 | 141 (7.3) | 24.9 | 25.4 | 411 (21.2) | 27.7 | 28.7 |
| =40 h/week | 1510 (38.9) | 24.9 | 26.3 | 651 (33.5) | 23.0 | 25.9 | 859 (44.3) | 26.4 | 26.5 |
| 41–52 h/week | 1190 (30.7) | 26.8 | 26.1 | 711 (36.6) | 23.3 | 24.5 | 479 (24.7) | 32.0 | 27.6 |
| >52 h/week | 630 (16.2) | 29.9 | 27.2 | 441 (22.7) | 28.4 | 26.6 | 189 (9.8) | 33.2 | 28.5 |
| Smoking | |||||||||
| No | 2878 (74.1) | 27.0 | 26.9 | 1140 (58.6) | 25.1 | 26.4 | 1738 (89.7) | 28.2 | 27.2 |
| Yes | 1004 (25.9) | 25.5 | 25.9 | 804 (41.4) | 23.6 | 24.4 | 200 (10.3) | 33.0 | 30.0 |
| Binge drinking | |||||||||
| No | 2204 (56.8) | 26.8 | 26.6 | 912 (46.9) | 25.1 | 25.8 | 1292 (66.7) | 28.0 | 27.1 |
| Yes | 1678 (43.2) | 26.3 | 26.8 | 1032 (53.1) | 24.0 | 25.4 | 646 (33.3) | 30.1 | 28.4 |
| Exercise | |||||||||
| No | 2973 (76.6) | 27.1 | 26.6 | 1375 (70.7) | 25.0 | 25.2 | 1598 (82.5) | 29.0 | 27.6 |
| Yes | 909 (23.4) | 24.9 | 26.9 | 569 (29.3) | 23.3 | 26.5 | 340 (17.5) | 27.6 | 27.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.-W.; Lee, J.; Kim, H.-R.; Kang, M.-Y. Health-Related Productivity Loss According to Health Conditions among Workers in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 7589. https://doi.org/10.3390/ijerph18147589
Lee D-W, Lee J, Kim H-R, Kang M-Y. Health-Related Productivity Loss According to Health Conditions among Workers in South Korea. International Journal of Environmental Research and Public Health. 2021; 18(14):7589. https://doi.org/10.3390/ijerph18147589
Chicago/Turabian StyleLee, Dong-Wook, Jongin Lee, Hyoung-Ryoul Kim, and Mo-Yeol Kang. 2021. "Health-Related Productivity Loss According to Health Conditions among Workers in South Korea" International Journal of Environmental Research and Public Health 18, no. 14: 7589. https://doi.org/10.3390/ijerph18147589
APA StyleLee, D.-W., Lee, J., Kim, H.-R., & Kang, M.-Y. (2021). Health-Related Productivity Loss According to Health Conditions among Workers in South Korea. International Journal of Environmental Research and Public Health, 18(14), 7589. https://doi.org/10.3390/ijerph18147589







