Environmental Air Pollutants Inhaled during Pregnancy Are Associated with Altered Cord Blood Immune Cell Profiles
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Ethics Statement
2.3. Cord Blood Collection
2.4. Flow Cytometry Analysis
2.5. Air Pollutant Assessment
2.6. Statistical Analysis
3. Results
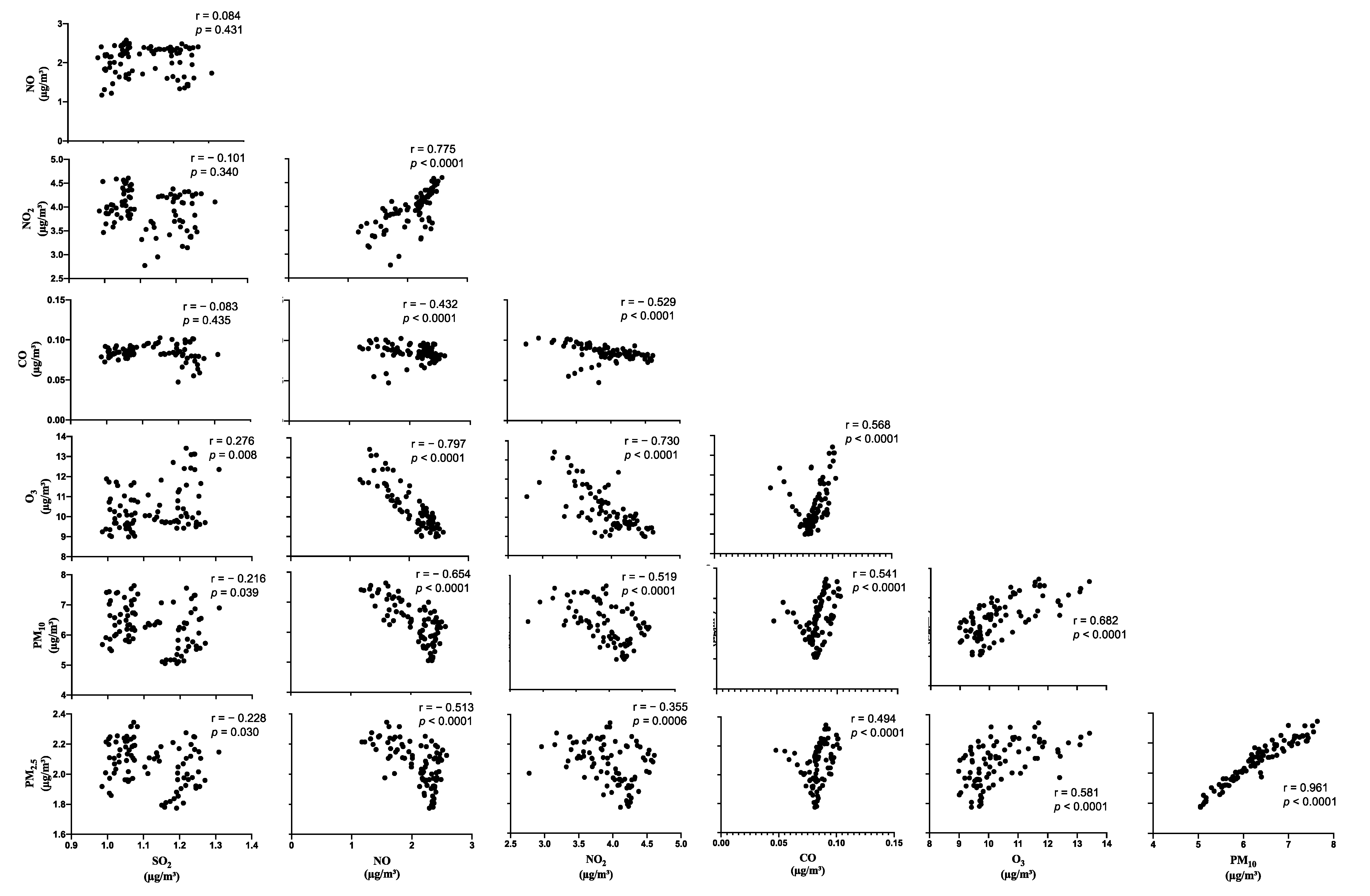
3.1. PCA from Air Pollutants Have Positive Loading for O3 and PM2.5
3.2. PCA from Cell Types Have Positive Loading for CD8 T cells, ILC1, CRTh2high ILC2, NCR− ILC3, Neutrophils, pDCs, and NCR+ ILC3
3.3. Air Pollutant PC2 Associates with Cell Type PC1 and Cell Type PC4
3.4. SO2 Associates with CD8 T Cells, CD4 T Cells and mDCs While PM2.5 Associates with pDCs in a Multipollutant Multivariable Regression Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murphy, V.E.; Namazy, J.A.; Powell, H.; Schatz, M.; Chambers, C.; Attia, J.; Gibson, P.G. A meta-analysis of adverse perinatal outcomes in women with asthma. BJOG 2011, 118, 1314–1323. [Google Scholar] [CrossRef] [PubMed]
- Murphy, V.E. Managing asthma in pregnancy. Breathe 2015, 11, 258–267. [Google Scholar] [CrossRef]
- Mendola, P.; Mannisto, T.I.; Leishear, K.; Reddy, U.M.; Chen, Z.; Laughon, S.K. Neonatal health of infants born to mothers with asthma. J. Allergy Clin. Immunol. 2014, 133, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Martel, M.J.; Rey, E.; Beauchesne, M.F.; Malo, J.L.; Perreault, S.; Forget, A.; Blais, L. Control and severity of asthma during pregnancy are associated with asthma incidence in offspring: Two-stage case-control study. Eur. Respir. J. 2009, 34, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Valadares, M.A.; Gurgel, R.Q.; Melo, E.V.; Guimaraes, A.M.; Guedes, K.M.; Rocha, N.A.; Almeida, M.L. Respiratory function in children of asthmatic mothers. J. Pediatr. 2013, 89, 158–163. [Google Scholar] [CrossRef][Green Version]
- Seeni, I.; Ha, S.; Nobles, C.; Liu, D.; Sherman, S.; Mendola, P. Air pollution exposure during pregnancy: Maternal asthma and neonatal respiratory outcomes. Ann. Epidemiol. 2018, 28, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Valavanidis, A.; Fiotakis, K.; Vlachogianni, T. Airborne particulate matter and human health: Toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J. Environ. Sci. Health Part C Environ. Carcinog. Ecotoxicol. Rev. 2008, 26, 339–362. [Google Scholar] [CrossRef] [PubMed]
- Nemmar, A.; Holme, J.A.; Rosas, I.; Schwarze, P.E.; Alfaro-Moreno, E. Recent advances in particulate matter and nanoparticle toxicology: A review of the in vivo and in vitro studies. Biomed. Res. Int. 2013, 2013, 279371. [Google Scholar] [CrossRef] [PubMed]
- Idowu, O.; Semple, K.T.; Ramadass, K.; O’Connor, W.; Hansbro, P.; Thavamani, P. Beyond the obvious: Environmental health implications of polar polycyclic aromatic hydrocarbons. Environ. Int. 2019, 123, 543–557. [Google Scholar] [CrossRef]
- Schraufnagel, D.E.; Balmes, J.R.; Cowl, C.T.; De Matteis, S.; Jung, S.H.; Mortimer, K.; Perez-Padilla, R.; Rice, M.B.; Riojas-Rodriguez, H.; Sood, A.; et al. Pollution and noncommunicable diseases: A review by the forum of international respiratory societies’ environmental committee, part 1: The damaging effects of air pollution. Chest 2019, 155, 409–416. [Google Scholar] [CrossRef]
- Schraufnagel, D.E.; Balmes, J.R.; Cowl, C.T.; De Matteis, S.; Jung, S.H.; Mortimer, K.; Perez-Padilla, R.; Rice, M.B.; Riojas-Rodriguez, H.; Sood, A.; et al. Air pollution and noncommunicable diseases: A review by the forum of international respiratory societies’ environmental committee, part 2: Air pollution and organ systems. Chest 2019, 155, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, K.; Dey, S.; Gupta, T.; Dhaliwal, R.S.; Brauer, M.; Cohen, A.J.; Stanaway, J.D.; Beig, G.; Joshi, T.K.; Aggarwal, A.N.; et al. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: The Global Burden of Disease Study 2017. Lancet Planet. Health 2019, 3, e26–e39. [Google Scholar] [CrossRef]
- Morakinyo, O.M.; Mokgobu, M.I.; Mukhola, M.S.; Hunter, R.P. Health outcomes of exposure to biological and chemical components of inhalable and respirable particulate matter. Int. J. Environ. Res. Public Health 2016, 13, 592. [Google Scholar] [CrossRef] [PubMed]
- Bontinck, A.; Maes, T.; Joos, G. Asthma and air pollution: Recent insights in pathogenesis and clinical implications. Curr. Opin. Pulm. Med. 2020, 26, 10–19. [Google Scholar] [CrossRef]
- Heindel, J.J.; Vandenberg, L.N. Developmental origins of health and disease: A paradigm for understanding disease cause and prevention. Curr. Opin. Pediatr. 2015, 27, 248. [Google Scholar] [CrossRef]
- Koren, G.; Ornoy, A. The role of the placenta in drug transport and fetal drug exposure. Expert Rev. Clin. Pharm. 2018, 11, 373–385. [Google Scholar] [CrossRef]
- Bove, H.; Bongaerts, E.; Slenders, E.; Bijnens, E.M.; Saenen, N.D.; Gyselaers, W.; Van Eyken, P.; Plusquin, M.; Roeffaers, M.B.J.; Ameloot, M.; et al. Ambient black carbon particles reach the fetal side of human placenta. Nat. Commun. 2019, 10, 3866. [Google Scholar] [CrossRef]
- Darrow, L.A.; Klein, M.; Strickland, M.J.; Mulholland, J.A.; Tolbert, P.E. Ambient air pollution and birth weight in full-term infants in Atlanta, 1994–2004. Environ. Health Perspect 2011, 119, 731–737. [Google Scholar] [CrossRef]
- Maisonet, M.; Bush, T.J.; Correa, A.; Jaakkola, J.J. Relation between ambient air pollution and low birth weight in the Northeastern United States. Environ. Health Perspect 2001, 109 (Suppl. 3), 351–356. [Google Scholar] [CrossRef]
- Trasande, L.; Wong, K.; Roy, A.; Savitz, D.A.; Thurston, G. Exploring prenatal outdoor air pollution, birth outcomes and neonatal health care utilization in a nationally representative sample. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 315–321. [Google Scholar] [CrossRef]
- Glinianaia, S.V.; Rankin, J.; Bell, R.; Pless-Mulloli, T.; Howel, D. Particulate air pollution and fetal health: A systematic review of the epidemiologic evidence. Epidemiology 2004, 15, 36–45. [Google Scholar] [CrossRef]
- Pinkerton, K.E.; Joad, J.P. Influence of air pollution on respiratory health during perinatal development. Clin. Exp. Pharm. Physiol. 2006, 33, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Herr, C.E.; Dostal, M.; Ghosh, R.; Ashwood, P.; Lipsett, M.; Pinkerton, K.E.; Sram, R.; Hertz-Picciotto, I. Air pollution exposure during critical time periods in gestation and alterations in cord blood lymphocyte distribution: A cohort of livebirths. Environ. Health 2010, 9, 46. [Google Scholar] [CrossRef] [PubMed]
- Hertz-Picciotto, I.; Dostal, M.; Dejmek, J.; Selevan, S.G.; Wegienka, G.; Gomez-Caminero, A.; Sram, R.J. Air pollution and distributions of lymphocyte immunophenotypes in cord and maternal blood at delivery. Epidemiology 2002, 13, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Hertz-Picciotto, I.; Herr, C.E.; Yap, P.S.; Dostal, M.; Shumway, R.H.; Ashwood, P.; Lipsett, M.; Joad, J.P.; Pinkerton, K.E.; Sram, R.J. Air pollution and lymphocyte phenotype proportions in cord blood. Environ. Health Perspect. 2005, 113, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Baiz, N.; Slama, R.; Bene, M.C.; Charles, M.A.; Kolopp-Sarda, M.N.; Magnan, A.; Thiebaugeorges, O.; Faure, G.; Annesi-Maesano, I. Maternal exposure to air pollution before and during pregnancy related to changes in newborn’s cord blood lymphocyte subpopulations. The EDEN study cohort. BMC Pregnancy Childbirth 2011, 11, 87. [Google Scholar] [CrossRef]
- Lura, M.P.; Gorlanova, O.; Muller, L.; Proietti, E.; Vienneau, D.; Reppucci, D.; Pavlovic, R.; Dahinden, C.; Roosli, M.; Latzin, P.; et al. Response of cord blood cells to environmental, hereditary and perinatal factors: A prospective birth cohort study. PLoS ONE 2018, 13, e0200236. [Google Scholar] [CrossRef]
- Herr, C.E.; Ghosh, R.; Dostal, M.; Skokanova, V.; Ashwood, P.; Lipsett, M.; Joad, J.P.; Pinkerton, K.E.; Yap, P.S.; Frost, J.D.; et al. Exposure to air pollution in critical prenatal time windows and IgE levels in newborns. Pediatr. Allergy Immunol. 2011, 22, 75–84. [Google Scholar] [CrossRef]
- Leonardi, G.S.; Houthuijs, D.; Steerenberg, P.A.; Fletcher, T.; Armstrong, B.; Antova, T.; Lochman, I.; Lochmanova, A.; Rudnai, P.; Erdei, E.; et al. Immune biomarkers in relation to exposure to particulate matter: A cross-sectional survey in 17 cities of Central Europe. Inhal. Toxicol. 2000, 12 (Suppl. 4), 1–14. [Google Scholar] [CrossRef]
- Ashley-Martin, J.; Lavigne, E.; Arbuckle, T.E.; Johnson, M.; Hystad, P.; Crouse, D.L.; Marshall, J.S.; Dodds, L. Air pollution during pregnancy and cord blood immune system biomarkers. J. Occup. Environ. Med. 2016, 58, 979–986. [Google Scholar] [CrossRef]
- Dietert, R.R.; Lee, J.E.; Hussain, I.; Piepenbrink, M. Developmental immunotoxicology of lead. Toxicol. Appl. Pharm. 2004, 198, 86–94. [Google Scholar] [CrossRef]
- Holladay, S.D.; Smialowicz, R.J. Development of the murine and human immune system: Differential effects of immunotoxicants depend on time of exposure. Environ. Health Perspect. 2000, 108, 463–473. [Google Scholar] [CrossRef]
- Luebke, R.W.; Chen, D.H.; Dietert, R.; Yang, Y.; King, M.; Luster, M.I.; Immunotoxicology, W. The comparative immunotoxicity of five selected compounds following developmental or adult exposure. J. Toxicol. Environ. Health 2006, 9, 1–26. [Google Scholar] [CrossRef]
- Latzin, P.; Frey, U.; Armann, J.; Kieninger, E.; Fuchs, O.; Roosli, M.; Schaub, B. Exposure to moderate air pollution during late pregnancy and cord blood cytokine secretion in healthy neonates. PLoS ONE 2011, 6, e23130. [Google Scholar] [CrossRef]
- Jennewein, M.F.; Abu-Raya, B.; Jiang, Y.; Alter, G.; Marchant, A. Transfer of maternal immunity and programming of the newborn immune system. Semin. Immunopathol. 2017, 39, 605–613. [Google Scholar] [CrossRef]
- Murphy, V.E.; Jensen, M.E.; Mattes, J.; Hensley, M.J.; Giles, W.B.; Peek, M.J.; Bisits, A.; Callaway, L.K.; McCaffery, K.; Barrett, H.L.; et al. The Breathing for Life Trial: A randomised controlled trial of fractional exhaled nitric oxide (FENO)-based management of asthma during pregnancy and its impact on perinatal outcomes and infant and childhood respiratory health. BMC Pregnancy Childbirth 2016, 16, 111. [Google Scholar] [CrossRef] [PubMed]
- NSW Department of Planning, Industry and Environment. New South Wales Air Quality Monitoring Network. Available online: https://www.environment.nsw.gov.au (accessed on 8 April 2020).
- Riley, M.; Kirkwood, J.; Jiang, N.; Ross, G.; Scorgie, Y. Air quality monitoring in NSW: From long term trend monitoring to integrated urban services. Air Qual. Clim. Chang. 2020, 54, 44–51. [Google Scholar]
- Ramsay, J.O.; Silverman, B.W. Principal components analysis for functional data. In Functional Data Analysis; Springer: New York, NY, USA, 2005; pp. 147–172. [Google Scholar]
- McDonald, J.H. Handbook of Biological Statistics, 3rd ed.; Sparky House Publishing: Baltimore, MA, USA, 2014. [Google Scholar]
- Ghazal, P.; Dickinson, P.; Smith, C.L. Early life response to infection. Curr. Opin. Infect. Dis. 2013, 26, 213–218. [Google Scholar] [CrossRef]
- Bakker, J.M.; Schmidt, E.D.; Kroes, H.; Kavelaars, A.; Heijnen, C.J.; Tilders, F.J.; Van Rees, E.P. Effects of short-term dexamethasone treatment during pregnancy on the development of the immune system and the hypothalamo-pituitary adrenal axis in the rat. J. Neuroimmunol. 1995, 63, 183–191. [Google Scholar] [CrossRef]
- Landreth, K.S. Critical windows in development of the rodent immune system. Hum. Exp. Toxicol. 2002, 21, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Vanders, R.L.; Murphy, V.E.; Gibson, P.G.; Hansbro, P.M.; Wark, P.A. CD8 T cells and dendritic cells: Key players in the attenuated maternal immune response to influenza infection. J. Reprod. Immunol. 2015, 107, 1–9. [Google Scholar] [CrossRef]
- Kaiko, G.E.; Horvat, J.C.; Beagley, K.W.; Hansbro, P.M. Immunological decision-making: How does the immune system decide to mount a helper T-cell response? Immunology 2008, 123, 326–338. [Google Scholar] [CrossRef] [PubMed]
- Maggi, E.; Parronchi, P.; Manetti, R.; Simonelli, C.; Piccinni, M.P.; Rugiu, F.S.; De Carli, M.; Ricci, M.; Romagnani, S. Reciprocal regulatory effects of IFN-gamma and IL-4 on the in vitro development of human Th1 and Th2 clones. J. Immunol. 1992, 148, 2142–2147. [Google Scholar] [PubMed]
- Thorburn, A.N.; Hansbro, P.M. Harnessing regulatory T cells to suppress asthma: From potential to therapy. Am. J. Respir. Cell Mol. Biol. 2010, 43, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Dietert, R.R.; Etzel, R.A.; Chen, D.; Halonen, M.; Holladay, S.D.; Jarabek, A.M.; Landreth, K.; Peden, D.B.; Pinkerton, K.; Smialowicz, R.J.; et al. Workshop to identify critical windows of exposure for children’s health: Immune and respiratory systems work group summary. Environ. Health Perspect. 2000, 108, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.B.; Du, J.B.; Cui, H. Sulfur dioxide, a double-faced molecule in mammals. Life Sci. 2014, 98, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Kajiyama, H.; Nojima, Y.; Mitsuhashi, H.; Ueki, K.; Tamura, S.; Sekihara, T.; Wakamatsu, R.; Yano, S.; Naruse, T. Elevated levels of serum sulfite in patients with chronic renal failure. J. Am. Soc. Nephrol. 2000, 11, 923–927. [Google Scholar] [CrossRef]
- Mitsuhashi, H.; Ikeuchi, H.; Yamashita, S.; Kuroiwa, T.; Kaneko, Y.; Hiromura, K.; Ueki, K.; Nojima, Y. Increased levels of serum sulfite in patients with acute pneumonia. Shock 2004, 21, 99–102. [Google Scholar] [CrossRef]
- Meng, Z.; Liu, Y.; Wu, D. Effect of sulfur dioxide inhalation on cytokine levels in lungs and serum of mice. Inhal. Toxicol. 2005, 17, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Novack, L.; Yitshak-Sade, M.; Landau, D.; Kloog, I.; Sarov, B.; Karakis, I. Association between ambient air pollution and proliferation of umbilical cord blood cells. Environ. Res. 2016, 151, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Zhang, Z.H.; Hu, D.; Ke, X.; Gu, Z.; Zou, Q.Y.; Hu, G.H.; Song, S.H.; Kang, H.Y.; Hong, S.L. The airway inflammation induced by nasal inoculation of PM2.5 and the treatment of bacterial lysates in rats. Sci. Rep. 2018, 8, 9816. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Fu, J.; Lin, S.H.; Sun, J.L.; Xia, L.; Lin, C.H.; Liu, L.; Zhang, C.; Yang, L.; Xue, P.; et al. Particulate matter of 2.5 mum or less in diameter disturbs the balance of TH17/regulatory T cells by targeting glutamate oxaloacetate transaminase 1 and hypoxia-inducible factor 1alpha in an asthma model. J. Allergy Clin. Immunol. 2020, 145, 402–414. [Google Scholar] [CrossRef]
- Prunicki, M.; Stell, L.; Dinakarpandian, D.; de Planell-Saguer, M.; Lucas, R.W.; Hammond, S.K.; Balmes, J.R.; Zhou, X.; Paglino, T.; Sabatti, C.; et al. Exposure to NO2, CO, and PM2.5 is linked to regional DNA methylation differences in asthma. Clin. Epigenetics 2018, 10, 2. [Google Scholar] [CrossRef]
- Melody, S.M.; Wills, K.; Knibbs, L.D.; Ford, J.; Venn, A.; Johnston, F. Maternal Exposure to Ambient Air Pollution and Pregnancy Complications in Victoria, Australia. Int. J. Environ. Res. Public Health 2020, 17, 2572. [Google Scholar] [CrossRef]
- Cunningham, M.W., Jr.; LaMarca, B. Risk of cardiovascular disease, end-stage renal disease, and stroke in postpartum women and their fetuses after a hypertensive pregnancy. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 315, R521–R528. [Google Scholar] [CrossRef] [PubMed]
- Ornoy, A.; Reece, E.A.; Pavlinkova, G.; Kappen, C.; Miller, R.K. Effect of maternal diabetes on the embryo, fetus, and children: Congenital anomalies, genetic and epigenetic changes and developmental outcomes. Birth Defects Res. Embryo Today 2015, 105, 53–72. [Google Scholar] [CrossRef] [PubMed]
- Hazlehurst, M.F.; Carroll, K.N.; Loftus, C.T.; Szpiro, A.A.; Moore, P.E.; Kaufman, J.D.; Kirwa, K.; LeWinn, K.Z.; Bush, N.R.; Sathyanarayana, S.; et al. Maternal exposure to PM2.5 during pregnancy and asthma risk in early childhood: Consideration of phases of fetal lung development. Environ. Epidemiol. 2021, 5, e130. [Google Scholar] [CrossRef]
- Tong, S. Air pollution and disease burden. Lancet Planet. Health 2019, 3, e49–e50. [Google Scholar] [CrossRef]
- Ogino, K.; Nagaoka, K.; Ito, T.; Takemoto, K.; Okuda, T.; Nakayama, S.F.; Ogino, N.; Seki, Y.; Hamada, H.; Takashiba, S.; et al. Involvement of PM2.5-bound protein and metals in PM2.5-induced allergic airway inflammation in mice. Inhal. Toxicol. 2018, 30, 498–508. [Google Scholar] [CrossRef]
- Falcon-Rodriguez, C.I.; Osornio-Vargas, A.R.; Sada-Ovalle, I.; Segura-Medina, P. Aeroparticles, composition, and lung diseases. Front. Immunol. 2016, 7, 3. [Google Scholar] [CrossRef]
- Nemmar, A.; Hoet, P.H.; Vanquickenborne, B.; Dinsdale, D.; Thomeer, M.; Hoylaerts, M.F.; Vanbilloen, H.; Mortelmans, L.; Nemery, B. Passage of inhaled particles into the blood circulation in humans. Circulation 2002, 105, 411–414. [Google Scholar] [CrossRef]
- Rogers, J.F.; Thompson, S.J.; Addy, C.L.; McKeown, R.E.; Cowen, D.J.; Decoufle, P. Association of very low birth weight with exposures to environmental sulfur dioxide and total suspended particulates. Am. J. Epidemiol. 2000, 151, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Sram, R.J.; Binkova, B.; Dejmek, J.; Bobak, M. Ambient air pollution and pregnancy outcomes: A review of the literature. Environ. Health Perspect. 2005, 113, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Dexter, S.C.; Pinar, H.; Malee, M.P.; Hogan, J.; Carpenter, M.W.; Vohr, B.R. Outcome of very low birth weight infants with histopathologic chorioamnionitis. Obs. Gynecol. 2000, 96, 172–177. [Google Scholar] [CrossRef]
- Yue, H.; Ji, X.; Li, G.; Hu, M.; Sang, N. Maternal exposure to PM2.5 affects fetal lung development at sensitive windows. Environ. Sci. Technol. 2020, 54, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, L.; Wang, F.; Li, C. Effect of fine particulate matter (PM2.5) on rat placenta pathology and perinatal outcomes. Med. Sci. Monit. 2016, 22, 3274–3280. [Google Scholar] [CrossRef] [PubMed]
- Shoenfelt, J.; Mitkus, R.J.; Zeisler, R.; Spatz, R.O.; Powell, J.; Fenton, M.J.; Squibb, K.A.; Medvedev, A.E. Involvement of TLR2 and TLR4 in inflammatory immune responses induced by fine and coarse ambient air particulate matter. J. Leukoc. Biol. 2009, 86, 303–312. [Google Scholar] [CrossRef]
- Becker, S.; Fenton, M.J.; Soukup, J.M. Involvement of microbial components and toll-like receptors 2 and 4 in cytokine responses to air pollution particles. Am. J. Respir. Cell Mol. Biol. 2002, 27, 611–618. [Google Scholar] [CrossRef]
- Goulaouic, S.; Foucaud, L.; Bennasroune, A.; Laval-Gilly, P.; Falla, J. Effect of polycyclic aromatic hydrocarbons and carbon black particles on pro-inflammatory cytokine secretion: Impact of PAH coating onto particles. J. Immunotoxicol. 2008, 5, 337–345. [Google Scholar] [CrossRef]
- Hopke, P.K.; Rossner, A. Exposure to airborne particulate matter in the ambient, indoor, and occupational environments. Clin. Occup. Environ. Med. 2006, 5, 747–771. [Google Scholar] [CrossRef]
- Inoue, K.; Takano, H.; Yanagisawa, R.; Hirano, S.; Ichinose, T.; Shimada, A.; Yoshikawa, T. The role of toll-like receptor 4 in airway inflammation induced by diesel exhaust particles. Arch. Toxicol. 2006, 80, 275–279. [Google Scholar] [CrossRef]
- Yu, P.; Xu, R.; Abramson, M.J.; Li, S.; Guo, Y. Bushfires in Australia: A serious health emergency under climate change. Lancet Planet. Health 2020, 4, e7–e8. [Google Scholar] [CrossRef]
- Nogrady, B. Bushfires: Australia issues health warnings as Sydney air quality plummets. BMJ 2019, 367, l6914. [Google Scholar] [CrossRef] [PubMed]
- Vardoulakis, S.; Marks, G.; Abramson, M.J. Lessons learned from the australian bushfires: Climate change, air pollution, and public health. JAMA Intern. Med. 2020, 180, 635–636. [Google Scholar] [CrossRef] [PubMed]
- Dharwal, V.; Paudel, K.R.; Hansbro, P.M. Impact of bushfire smoke on respiratory health. Med. J. Aust 2020, 213, 284. [Google Scholar] [CrossRef]
- Porter, M.; Karp, M.; Killedar, S.; Bauer, S.M.; Guo, J.; Williams, D.; Breysse, P.; Georas, S.N.; Williams, M.A. Diesel-enriched particulate matter functionally activates human dendritic cells. Am. J. Respir. Cell Mol. Biol. 2007, 37, 706–719. [Google Scholar] [CrossRef]
- Matthews, N.C.; Faith, A.; Pfeffer, P.; Lu, H.; Kelly, F.J.; Hawrylowicz, C.M.; Lee, T.H. Urban particulate matter suppresses priming of T helper type 1 cells by granulocyte/macrophage colony-stimulating factor-activated human dendritic cells. Am. J. Respir. Cell Mol. Biol. 2014, 50, 281–291. [Google Scholar] [CrossRef]
- Pfeffer, P.E.; Ho, T.R.; Mann, E.H.; Kelly, F.J.; Sehlstedt, M.; Pourazar, J.; Dove, R.E.; Sandstrom, T.; Mudway, I.S.; Hawrylowicz, C.M. Urban particulate matter stimulation of human dendritic cells enhances priming of naive CD8 T lymphocytes. Immunology 2018, 153, 502–512. [Google Scholar] [CrossRef]
- Bleck, B.; Tse, D.B.; Jaspers, I.; Curotto de Lafaille, M.A.; Reibman, J. Diesel exhaust particle-exposed human bronchial epithelial cells induce dendritic cell maturation. J. Immunol. 2006, 176, 7431–7437. [Google Scholar] [CrossRef]
- Bleck, B.; Tse, D.B.; Curotto de Lafaille, M.A.; Zhang, F.; Reibman, J. Diesel exhaust particle-exposed human bronchial epithelial cells induce dendritic cell maturation and polarization via thymic stromal lymphopoietin. J. Clin. Immunol. 2008, 28, 147–156. [Google Scholar] [CrossRef]
- Chairakaki, A.D.; Saridaki, M.I.; Pyrillou, K.; Mouratis, M.A.; Koltsida, O.; Walton, R.P.; Bartlett, N.W.; Stavropoulos, A.; Boon, L.; Rovina, N.; et al. Plasmacytoid dendritic cells drive acute asthma exacerbations. J. Allergy Clin. Immunol. 2018, 142, 542–556. [Google Scholar] [CrossRef]
- Hatchwell, L.; Collison, A.; Girkin, J.; Parsons, K.; Li, J.; Zhang, J.; Phipps, S.; Knight, D.; Bartlett, N.W.; Johnston, S.L.; et al. Toll-like receptor 7 governs interferon and inflammatory responses to rhinovirus and is suppressed by IL-5-induced lung eosinophilia. Thorax 2015, 70, 854–861. [Google Scholar] [CrossRef]
- Morten, M.; Collison, A.; Murphy, V.E.; Barker, D.; Oldmeadow, C.; Attia, J.; Meredith, J.; Powell, H.; Robinson, P.D.; Sly, P.D.; et al. Managing Asthma in Pregnancy (MAP) trial: FeNO levels and childhood asthma. J. Allergy Clin. Immunol. 2018, 142, 1765–1772. [Google Scholar] [CrossRef]
- Mattes, J.; Murphy, V.E.; Powell, H.; Gibson, P.G. Prenatal origins of bronchiolitis: Protective effect of optimised asthma management during pregnancy. Thorax 2014, 69, 383–384. [Google Scholar] [CrossRef]
- Halonen, M.; Lohman, I.C.; Stern, D.A.; Spangenberg, A.; Anderson, D.; Mobley, S.; Ciano, K.; Peck, M.; Wright, A.L. Th1/Th2 patterns and balance in cytokine production in the parents and infants of a large birth cohort. J. Immunol. 2009, 182, 3285–3293. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, I.; Herberth, G. Cord blood immune status: Predicting health or allergy? Allergy 2012, 67, 445–448. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, G.T.; Neas, L.; Vaughn, B.; Kattan, M.; Mitchell, H.; Crain, E.F.; Evans, R., 3rd; Gruchalla, R.; Morgan, W.; Stout, J.; et al. Acute respiratory health effects of air pollution on children with asthma in US inner cities. J. Allergy Clin. Immunol. 2008, 121, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Weinmayr, G.; Romeo, E.; De Sario, M.; Weiland, S.K.; Forastiere, F. Short-term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: A systematic review and meta-analysis. Environ. Health Perspect. 2010, 118, 449–457. [Google Scholar] [CrossRef]
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong-Neto, H.J.; Novakova, S.; Steiropoulos, P.; Kowal, K. Impact of Air Pollution on Asthma Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 6212. [Google Scholar] [CrossRef] [PubMed]
- Latzin, P.; Roosli, M.; Huss, A.; Kuehni, C.E.; Frey, U. Air pollution during pregnancy and lung function in newborns: A birth cohort study. Eur. Respir. J. 2009, 33, 594–603. [Google Scholar] [CrossRef]
- Korten, I.; Ramsey, K.; Latzin, P. Air pollution during pregnancy and lung development in the child. Paediatr. Respir. Rev. 2017, 21, 38–46. [Google Scholar] [CrossRef]
- Sbihi, H.; Tamburic, L.; Koehoorn, M.; Brauer, M. Perinatal air pollution exposure and development of asthma from birth to age 10 years. Eur. Respir. J. 2016, 47, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Stern, D.A.; Morgan, W.J.; Wright, A.L.; Guerra, S.; Martinez, F.D. Poor airway function in early infancy and lung function by age 22 years: A non-selective longitudinal cohort study. Lancet 2007, 370, 758–764. [Google Scholar] [CrossRef]
- Turner, S.W.; Palmer, L.J.; Rye, P.J.; Gibson, N.A.; Judge, P.K.; Cox, M.; Young, S.; Goldblatt, J.; Landau, L.I.; Le Souef, P.N. The relationship between infant airway function, childhood airway responsiveness, and asthma. Am. J. Respir. Crit. Care Med. 2004, 169, 921–927. [Google Scholar] [CrossRef]
- Filippone, M.; Sartor, M.; Zacchello, F.; Baraldi, E. Flow limitation in infants with bronchopulmonary dysplasia and respiratory function at school age. Lancet 2003, 361, 753–754. [Google Scholar] [CrossRef]
- Hoo, A.F.; Stocks, J.; Lum, S.; Wade, A.M.; Castle, R.A.; Costeloe, K.L.; Dezateux, C. Development of lung function in early life: Influence of birth weight in infants of nonsmokers. Am. J. Respir. Crit. Care Med. 2004, 170, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.D. The origins of asthma and chronic obstructive pulmonary disease in early life. Proc. Am. Thorac. Soc. 2009, 6, 272–277. [Google Scholar] [CrossRef]
- Junge, K.M.; Hornig, F.; Herberth, G.; Roder, S.; Kohajda, T.; Rolle-Kampczyk, U.; von Bergen, M.; Borte, M.; Simon, J.C.; Heroux, D.; et al. The LINA cohort: Cord blood eosinophil/basophil progenitors predict respiratory outcomes in early infancy. Clin. Immunol. 2014, 152, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Gern, J.E.; Calatroni, A.; Jaffee, K.F.; Lynn, H.; Dresen, A.; Cruikshank, W.W.; Lederman, H.M.; Sampson, H.A.; Shreffler, W.; Bacharier, L.B.; et al. Patterns of immune development in urban preschoolers with recurrent wheeze and/or atopy. J. Allergy Clin. Immunol. 2017, 140, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Hornsby, E.; Pfeffer, P.E.; Laranjo, N.; Cruikshank, W.; Tuzova, M.; Litonjua, A.A.; Weiss, S.T.; Carey, V.J.; O’Connor, G.; Hawrylowicz, C. Vitamin D supplementation during pregnancy: Effect on the neonatal immune system in a randomized controlled trial. J. Allergy Clin. Immunol. 2018, 141, 269–278. [Google Scholar] [CrossRef]
- Bullens, D.M.; Seys, S.; Kasran, A.; Dilissen, E.; Dupont, L.J.; Ceuppens, J.L. Low cord blood Foxp3/CD3gamma mRNA ratios: A marker of increased risk for allergy development. Clin. Exp. Allergy 2015, 45, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Perveen, K.; Quach, A.; McPhee, A.; Prescott, S.L.; Barry, S.C.; Hii, C.S.; Ferrante, A. Validation of monoclonal anti-PKC isozyme antibodies for flow cytometry analyses in human T cell subsets and expression in cord blood T cells. Sci. Rep. 2019, 9, 9263. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, E.; Harder, J.; Lacorcia, M.; Honkpehedji, Y.J.; Nouatin, O.P.; van Dam, G.J.; Corstjens, P.; Sartono, E.; Esen, M.; Lobmaier, S.M.; et al. Placental gene expression and antibody levels of mother-neonate pairs reveal an enhanced risk for inflammation in a helminth endemic country. Sci. Rep. 2019, 9, 15776. [Google Scholar] [CrossRef] [PubMed]
| Mean (Min–Max)/n (%) | Total (n) | |
|---|---|---|
| Demographic Characteristics | ||
| Maternal smoking during pregnancy | 11 (12.1) | 91 |
| Maternal recurrent asthma exacerbation during pregnancy | 4 (4.9) | 81 |
| Maternal age at delivery | 30.0 (19.0–41.5) | 91 |
| Gestational age at delivery (weeks) | 39 (34–41) | 91 |
| Caesarean section | 33 (36.3) | 90 |
| Mode of labor, spontaneous | 16 (17.8) | 90 |
| Mode of labor, augmented | 9 (10.0) | 90 |
| Mode of labor, induced | 48 (53.3) | 90 |
| Fetal heart rate decelerations during labor | 29 (32.2) | 90 |
| Male sex | 49 (53.8) | 91 |
| Older siblings | 46 (51.1) | 90 |
| Birth weight (kg) | 3.5 (2.1–4.9) | 90 |
| Birth length (cm) | 51.6 (30.7–58.0) | 86 |
| Air pollution exposure during pregnancy—Mean daily concentration | ||
| SO2 (µg/m³) | 4.2 (3.5–5.0) | 91 |
| PM10 (µg/m³) | 23.6 (20.4–26.8) | 91 |
| PM2.5 (µg/m³) | 7.8 (7.1–8.5) | 91 |
| NO (µg/m³) | 7.9 (4.1–9.7) | 91 |
| NO2 (µg/m³) | 15.0 (10.2–17.6) | 91 |
| CO (µg/m³) | 0.3 (0.2–0.4) | 91 |
| O3 (µg/m³) | 39.0 (34.6–44.4) | 91 |
| Humidity (%) | 69.9 (66.1–73.9) | 91 |
| Temperature (°C) | 18.6 (16.8–20.7) | 91 |
| Air Pollutants | PC1 | PC2 |
|---|---|---|
| SO2 | 0.144 | −0.719 |
| NO | −0.464 | −0.002 |
| NO2 | −0.430 | 0.260 |
| CO | 0.268 | 0.051 |
| O3 | 0.505 | −0.197 |
| PM10 | 0.396 | 0.386 |
| PM2.5 | 0.309 | 0.474 |
| Cell Types | PC1 | PC2 | PC3 | PC4 |
|---|---|---|---|---|
| Eosinophils | 0.006 | 0.045 | −0.683 | −0.005 |
| Neutrophils | −0.002 | 0.051 | 0.698 | −0.014 |
| Treg | −0.325 | −0.125 | 0.036 | 0.304 |
| TCD4 | −0.583 | −0.018 | −0.018 | −0.163 |
| TCD8 | 0.557 | 0.058 | −0.055 | −0.003 |
| NK cells | 0.362 | −0.234 | 0.110 | −0.050 |
| pDC | 0.183 | −0.064 | −0.063 | 0.585 |
| mDC | 0.196 | 0.047 | 0.071 | −0.402 |
| ILC1 | −0.172 | 0.488 | 0.041 | 0.064 |
| CRTh2high ILC2 | 0.063 | 0.564 | −0.093 | −0.158 |
| NCR− ILC3 | 0.086 | 0.586 | 0.078 | 0.115 |
| NCR+ ILC3 | 0.012 | 0.123 | 0.065 | 0.577 |
| Crude Regression | PC1 Cell Types | PC2 Cell Types | PC3 Cell Types | PC4 Cell Types | ||||
|---|---|---|---|---|---|---|---|---|
| Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | |
| PC1 Air pollutant | −0.021 (−0.173; 0.129) | 0.776 | 0.018 (−0.129; 0.165) | 0.804 | −0.055 (−0.198; 0.087) | 0.443 | 0.083 (−0.053; 0.219) | 0.230 |
| PC2 Air pollutant | −0.411 (−0.632; −0.190) | 0.0004 | −0.187 (−0.415; 0.040) | 0.106 | −0.320 (−0.535; −0.106) | 0.004 | 0.495 (0.305; 0.684) | 1.29 × 10−6 |
| Multivariable Regression * | PC1 Cell Types | PC3 Cell Types | PC4 Cell Types | |||
|---|---|---|---|---|---|---|
| Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | |
| PC2 Air pollutant | −0.429 (−0.618; −0.239) | 2.19 × 10−5 | −0.192 (−0.390; 0.005) | 0.056 | 0.471 (0.273; 0.668) | 8.91 × 10−6 |
| Multipollutant Multivariable Model * | ||||
|---|---|---|---|---|
| PM2.5 | SO2 | |||
| Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | |
| TCD8 † | −4.268 (−104.138; 95.602) | 0.932 | 260.242 (99.087; 421.397) | 0.002 |
| TCD4 † | 63.128 (−47.986; 174.242) | 0.262 | −234.283 (−413.582–54.984) | 0.011 |
| Multipollutant Multivariable Model * | ||||
|---|---|---|---|---|
| PM2.5 | SO2 | |||
| Coef. (95% CI) | p Value | Coef. (95% CI) | p Value | |
| pDC † | 155.158 (46.578; 263.738) | 0.006 | −169.378 (−344.588; 5.832) | 0.058 |
| mDC † | −90.800 (−311.056, 129.456) | 0.414 | 879.250 (523.834; 1234.666) | 4.43 × 10−6 |
| NCR + ILC3 ‡ | 0.149 (0.006; 0.290) | 0.041 | 0.011 (−0.219; 0.240) | 0.927 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martins Costa Gomes, G.; Karmaus, W.; Murphy, V.E.; Gibson, P.G.; Percival, E.; Hansbro, P.M.; Starkey, M.R.; Mattes, J.; Collison, A.M. Environmental Air Pollutants Inhaled during Pregnancy Are Associated with Altered Cord Blood Immune Cell Profiles. Int. J. Environ. Res. Public Health 2021, 18, 7431. https://doi.org/10.3390/ijerph18147431
Martins Costa Gomes G, Karmaus W, Murphy VE, Gibson PG, Percival E, Hansbro PM, Starkey MR, Mattes J, Collison AM. Environmental Air Pollutants Inhaled during Pregnancy Are Associated with Altered Cord Blood Immune Cell Profiles. International Journal of Environmental Research and Public Health. 2021; 18(14):7431. https://doi.org/10.3390/ijerph18147431
Chicago/Turabian StyleMartins Costa Gomes, Gabriela, Wilfried Karmaus, Vanessa E. Murphy, Peter G. Gibson, Elizabeth Percival, Philip M. Hansbro, Malcolm R. Starkey, Joerg Mattes, and Adam M. Collison. 2021. "Environmental Air Pollutants Inhaled during Pregnancy Are Associated with Altered Cord Blood Immune Cell Profiles" International Journal of Environmental Research and Public Health 18, no. 14: 7431. https://doi.org/10.3390/ijerph18147431
APA StyleMartins Costa Gomes, G., Karmaus, W., Murphy, V. E., Gibson, P. G., Percival, E., Hansbro, P. M., Starkey, M. R., Mattes, J., & Collison, A. M. (2021). Environmental Air Pollutants Inhaled during Pregnancy Are Associated with Altered Cord Blood Immune Cell Profiles. International Journal of Environmental Research and Public Health, 18(14), 7431. https://doi.org/10.3390/ijerph18147431






