A Generalized Structural Equation Model Approach to Long Working Hours and Near-Misses among Healthcare Professionals in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Measures
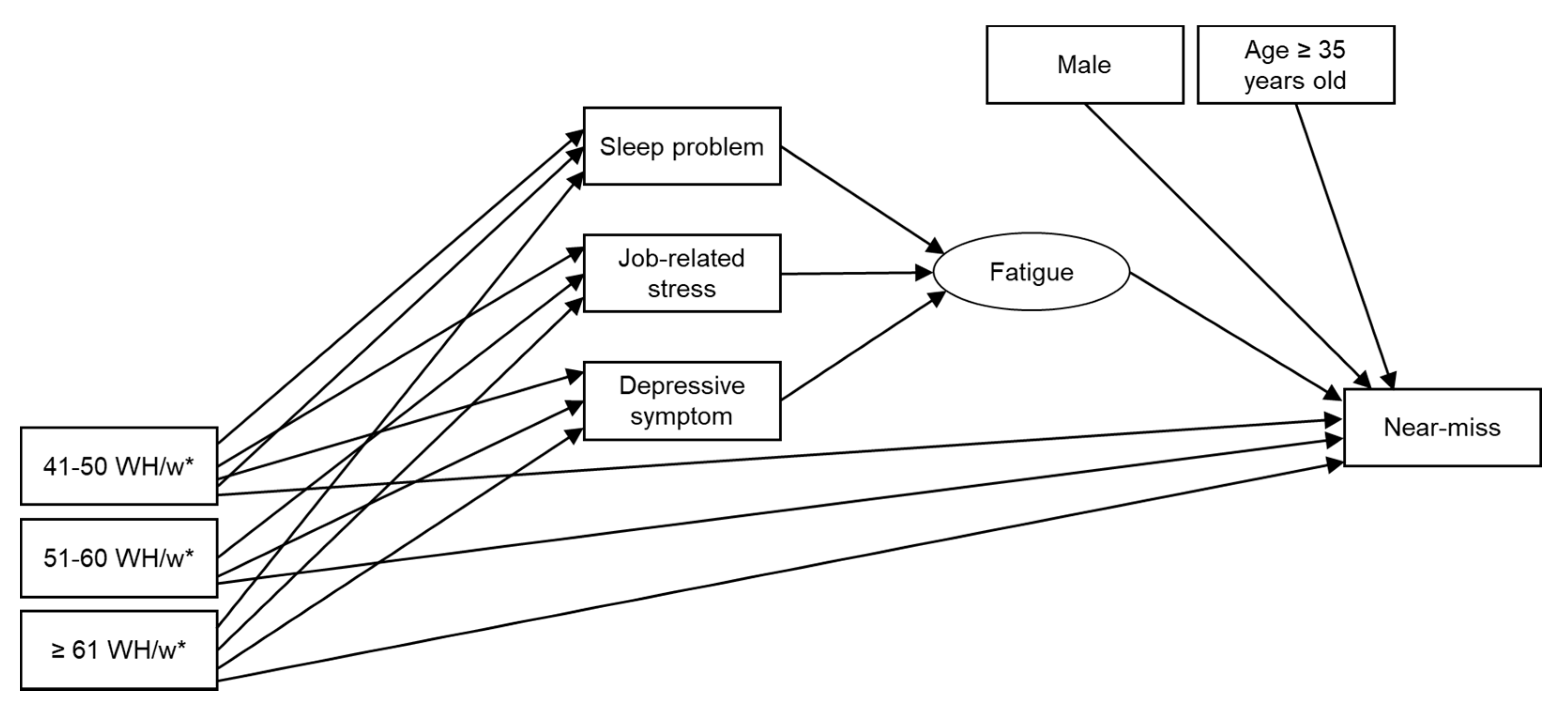
2.2. Structure Model
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- English, K.M.; Langley, J.M.; McGeer, A.; Hupert, N.; Tellier, R.; Henry, B.; Halperin, S.A.; Johnston, L.; Pourbohloul, B. Contact among healthcare workers in the hospital setting: Developing the evidence base for innovative approaches to infection control. BMC Infect. Dis. 2018, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, R.; Monsalve, M.; Thomas, G.W.; Herman, T.; Segre, A.M.; Polgreen, P.M.; Suneja, M. Estimating Time Physicians and Other Health Care Workers Spend with Patients in an Intensive Care Unit Using a Sensor Network. Am. J. Med. 2018, 131. [Google Scholar] [CrossRef] [PubMed]
- National Safety Council Near Miss Reporting Systems. Available online: https://www.atlantictraining.com/blog/wp-content/uploads/2018/05/294734832-Near-Miss-Reporting-Systems.pdf (accessed on 22 April 2021).
- McKinnon, R.C. Safety Management: Near Miss Identification, Recognition, and Investigation; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar] [CrossRef]
- Alamgir, H.; Yu, S.; Gorman, E.; Ngan, K.; Guzman, J. Near miss and minor occupational injury: Does it share a common causal pathway with major injury? Am. J. Ind. Med. 2009, 52. [Google Scholar] [CrossRef]
- Yamauchi, T.; Takahashi, K.; Suka, M.; Sasaki, T.; Takahashi, M.; Yoshikawa, T.; Okoshi, H.; Umezaki, S.; Yanagisawa, H. Longitudinal association between near-misses/minor injuries and moderate/severe injuries in industrial settings by presence/absence of depressive symptoms in a nationally representative sample of workers in Japan. Occup. Environ. Med. 2020, 77. [Google Scholar] [CrossRef] [PubMed]
- Landrigan, C.P.; Rahman, S.A.; Sullivan, J.P.; Vittinghoff, E.; Barger, L.K.; Sanderson, A.L.; Wright, K.P.; O’Brien, C.S.; Qadri, S.; St. Hilaire, M.A.; et al. Effect on Patient Safety of a Resident Physician Schedule without 24-Hour Shifts. N. Engl. J. Med. 2020, 382. [Google Scholar] [CrossRef]
- Scott, S.D.; Hirschinger, L.E.; Cox, K.R.; McCoig, M.; Brandt, J.; Hall, L.W. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual. Saf. Heal. Care 2009, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, A.E.; Hwang, W.T.; Scott, L.D.; Aiken, L.H.; Dinges, D.F. The working hours of hospital staff nurses and patient safety. Health Aff. 2004, 23. [Google Scholar] [CrossRef] [Green Version]
- Yamauchi, T.; Sasaki, T.; Takahashi, K.; Umezaki, S.; Takahashi, M.; Yoshikawa, T.; Suka, M.; Yanagisawa, H. Long working hours, sleep-related problems, and near-misses/injuries in industrial settings using a nationally representative sample of workers in Japan. PLoS ONE 2019, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagstaff, A.S.; Lie, J.A.S. Shift and night work and long working hours—A systematic review of safety implications. Scand. J. Work Environ. Health 2011, 37. [Google Scholar] [CrossRef] [Green Version]
- International Labour Organization Employment Distribution by Weekly Hours Actualluy Worked (by Sex) (%) Annual. Available online: https://ilostat.ilo.org/topics/working-time/ (accessed on 22 April 2021).
- Ogawa, R.; Seo, E.; Maeno, T.; Ito, M.; Sanuki, M.; Maeno, T. The relationship between long working hours and depression among first-year residents in Japan. BMC Med. Educ. 2018, 18. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health Labour and Welfare Study Group on the Reform of Work Styles of Doctors. Available online: https://www.mhlw.go.jp/stf/shingi/other-isei_469190.html (accessed on 22 April 2021).
- Gai, R.; Tobe, M. Managing healthcare delivery system to fight the COVID-19 epidemic: Experience in Japan. Glob. Health Res. Policy 2020, 5. [Google Scholar] [CrossRef]
- Ministry of Health Labour and Welfare Study Group on Supply and Demand of Healthcare Workers. Available online: https://www.mhlw.go.jp/stf/newpage_07927.html (accessed on 22 April 2021).
- Lee, K.; Suh, C.; Kim, J.E.; Park, J.O. The impact of long working hours on psychosocial stress response among white-collar workers. Ind. Health 2017, 55. [Google Scholar] [CrossRef] [Green Version]
- Kim, W.; Park, E.C.; Lee, T.H.; Kim, T.H. Effect of working hours and precarious employment on depressive symptoms in South Korean employees: A longitudinal study. Occup. Environ. Med. 2016, 73. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.M.; Wipfli, H.; Platz, E.A.; Bhavsar, N. A Dictionary of Epidemiology, Fifth Edition: Edited by Miquel Porta. Am. J. Epidemiol. 2009, 170. [Google Scholar] [CrossRef] [Green Version]
- Goldenhar, L.M.; Williams, L.J.; Swanson, N.G. Modelling relationships between job stressors and injury and near-miss outcomes for construction labourers. Work Stress 2003, 17, 218–240. [Google Scholar] [CrossRef]
- Amorim, L.D.A.F.; Fiaccone, R.L.; Santos, C.A.S.T.; dos Santos, T.N.; de Moraes, L.T.L.P.; Oliveira, N.F.; Barbosa, S.O.; dos Santos, D.N.; dos Santos, L.M.; Matos, S.M.A.; et al. Structural equation modeling in epidemiology. Cad. Saude Publica 2010, 26. [Google Scholar] [CrossRef] [PubMed]
- Kupek, E. Beyond logistic regression: Structural equations modelling for binary variables and its application to investigating unobserved confounders. BMC Med. Res. Methodol. 2006, 6. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Internal Affairs and Communications Labour Force Survey. Available online: https://www.e-stat.go.jp/en/stat-search/files?page=1&layout=datalist&toukei=00200531&tstat=000000110001&cycle=7&year=20170&month=0&tclass1=000001040276&tclass2=000001040283&tclass3=000001040284&result_back=1.&tclass4val=0 (accessed on 22 April 2021).
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28. [Google Scholar] [CrossRef]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000, 97. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1. [Google Scholar] [CrossRef]
- Tsutsumi, A.; Shimazu, A.; Eguchi, H.; Inoue, A.; Kawakami, N. A Japanese Stress Check Program screening tool predicts employee long-term sickness absence: A prospective study. J. Occup. Health 2018, 60. [Google Scholar] [CrossRef] [Green Version]
- Muthén, B.; Asparouhov, T. Causal Effects in Mediation Modeling: An Introduction With Applications to Latent Variables. Struct. Equ. Model. 2015, 22. [Google Scholar] [CrossRef]
- Seki, Y.; Yamazaki, Y. Effects of working conditions on intravenous medication errors in a Japanese hospital. J. Nurs. Manag. 2006, 14. [Google Scholar] [CrossRef]
- Japan Council for Quality Health Care Project to Collect Medical Near-Miss/Adverse Event Information 2019 Annual Report. Available online: https://www.med-safe.jp/pdf/year_report_english_2019.pdf (accessed on 17 June 2021).
- British Standards Institute OHSAS 18001. Occupational Health and Safety Management Systems—Requirements; BSI Global: London, UK, 2007. [Google Scholar]
- Zhou, Z.; Li, C.; Mi, C.; Qian, L. Exploring the potential use of near-miss information to improve construction safety performance. Sustainability 2019, 11, 1264. [Google Scholar] [CrossRef] [Green Version]
- The Japan Council for Quality Health Care Statistics. Available online: http://www.med-safe.jp/contents/report/html/StatisticsMenu.html (accessed on 22 April 2021).
- Robb, G.; Sultana, S.; Ameratunga, S.; Jackson, R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj. Prev. 2008, 14. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.; Lombardi, D.A.; Folkard, S.; Stutts, J.; Courtney, T.K.; Connor, J.L. The link between fatigue and safety. Accid. Anal. Prev. 2011, 43. [Google Scholar] [CrossRef]
- Roll, L.C.; Siu, O.L.; Li, S.Y.W.; de Witte, H. Human error: The impact of job insecurity on attention-related cognitive errors and error detection. Int. J. Environ. Res. Public Health 2019, 16, 2427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health Labour and Welfare Stress Check Programs. Available online: http://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/%0A (accessed on 22 April 2021).
- Härmä, M. Workhours in relation to work stress, recovery and health. Scand. J. Work Environ. Health 2006, 32. [Google Scholar] [CrossRef]
- Afonso, P.; Fonseca, M.; Pires, J.F. Impact of working hours on sleep and mental health. Occup. Med. 2017, 67. [Google Scholar] [CrossRef] [Green Version]
- Harrington, J.M. Health effects of shift work and extended hours of work. Occup. Environ. Med. 2001, 58. [Google Scholar] [CrossRef] [Green Version]
- Sagaspe, P.; Taillard, J.; Bayon, V.; Lagarde, E.; Moore, N.; Boussuge, J.; Chaumet, G.; Bioulac, B.; Philip, P. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J. Sleep Res. 2010, 19. [Google Scholar] [CrossRef] [PubMed]
- Achttien, R.; Van Lieshout, J.; Wensing, M.; Van Der Sanden, M.N.; Staal, J.B. Symptoms of depression are associated with physical inactivity but not modified by gender or the presence of a cardiovascular disease; A cross-sectional study. BMC Cardiovasc. Disord. 2019, 19. [Google Scholar] [CrossRef]
- Li, L.; Ai, H.; Gao, L.; Zhou, H.; Liu, X.; Zhang, Z.; Sun, T.; Fan, L. Moderating effects of coping on work stress and job performance for nurses in tertiary hospitals: A cross-sectional survey in China. BMC Health Serv. Res. 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization World Alliance for Patient Safety: WHO Draft Guidelines for Adverse Event Reporting and Learning Systems: From Information to Action. Available online: https://apps.who.int/iris/handle/10665/69797 (accessed on 22 April 2021).
- Arlinghaus, A.; Lombardi, D.A.; Willetts, J.L.; Folkard, S.; Christiani, D.C. A structural equation modeling approach to fatigue-related risk factors for occupational injury. Am. J. Epidemiol. 2012, 176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Healthcare Professionals (N = 1490) | |
|---|---|
| Female, n (%) | 1143 (76.7) |
| Age, n (%) | |
| 20–34 years | 529 (35.5) |
| 35–64 years | 961 (64.5) |
| Work hours per week, n (%) | |
| 35–40 h/w | 507 (34.0) |
| 41–50 h/w | 665 (44.6) |
| 51–60 h/w | 170 (11.4) |
| ≥61 h/w | 148 (9.9) |
| Night/shift work, n (%) | 553 (37.1) |
| Work experience, n (%) | |
| ≤3 years | 283 (19.0) |
| 4–10 years | 481 (32.3) |
| ≥11 years | 726 (48.7) |
| Job-related stress (total score), mean (SD) | 44.0 (6.3) |
| Depressive symptom (total score), mean (SD) | 16.5 (9.7) |
| Sleep problem (total score), mean (SD) | 5.8 (3.0) |
| Near-miss, n (%) | 732 (49.1) |
| Standardized Coefficient (95% CI) | Odds Ratio 1 (95% CI) | |
|---|---|---|
| Working hours → Near-misses | ||
| 35–40 h/w | reference | 1.00 |
| 41–50 h/w | 0.100 (−0.153, 0.346) | 1.11 (0.85, 1.41) |
| 51–60 h/w | 0.087 (−0.261, 0.467) | 1.09 (0.77, 1.60) |
| ≥61 h/w | 0.016 (−0.375, 0.394) | 1.02 (0.69,1.48) |
| Working hours → Job-related stress | ||
| 35–40 h/w | reference | - |
| 41–50 h/w | 0.290 (0.176, 0.404) | - |
| 51–60 h/w | 0.556 (0.382, 0.728) | - |
| ≥61 h/w | 0.690 (0.524, 0.859) | - |
| Working hours → Sleep problem | ||
| 35–40 h/w | reference | - |
| 41–50 h/w | 0.056 (−0.063, 0.171) | - |
| 51–60 h/w | 0.168 (−0.019, 0.349) | - |
| ≥61 h/w | 0.263 (0.082, 0.442) | - |
| Working hours → Depressive symptom | ||
| 35–40 h/w | reference | - |
| 41–50 h/w | 0.007 (−0.108, 0.126) | - |
| 51–60 h/w | 0.142 (−0.021, 0.297) | - |
| ≥61 h/w | 0.362 (0.139, 0.580) | - |
| Job–related stress → Fatigue (latent variable) | 0.397 (0.278, 0.532) | - |
| Sleep problem → Fatigue (latent variable) | 0.239 (0.114, 0.365) | - |
| Depressive symptom → Fatigue (latent variable) | −0.021 (−0.166, 0.121) | - |
| Fatigue (latent variable) → Near–misses | 1.000 2 | - |
| Sex → Near–misses | ||
| Female | reference | 1.00 |
| Male | 0.070 (−0.179, 0.311) | 1.07 (0.84, 1.37) |
| Age → Near–misses | ||
| < 35 years old | reference | 1.00 |
| ≥35 years old | −0.157 (−0.378, 0.072) | 0.85 (0.68, 1.07) |
| n/Number of Near-Misses | Direct Effect | Indirect Effect | Total Effect (Direct + Indirect) | |||
|---|---|---|---|---|---|---|
| Working Hour → Near-Miss | Working Hour → Job-Related Stress → Fatigue → Near-Miss | Working Hour → Sleep Problem → Fatigue → Near-Miss | Working Hour → Depressive Symptom → Fatigue → Near-Miss | |||
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | ||
| Working hours/week | ||||||
| 35–40 h/w | 507/231 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 41–50 h/w | 665/338 | 1.11 (0.85, 1.41) | 1.12 (1.07, 1.21) | 1.01 (0.99, 1.05) | 1.00 (0.99, 1.01) | 1.26 (0.97, 1.61) |
| 51–60 h/w | 170/92 | 1.09 (0.77, 1.60) | 1.25 (1.14, 1.41) | 1.04 (1.00, 1.10) | 1.00 (0.97, 1.02) | 1.41 (0.99, 2.06) |
| ≥61 h/w | 148/80 | 1.02 (0.69, 1.48) | 1.31 (1.18, 1.51) | 1.07 (1.02, 1.13) | 0.99 (0.93, 1.05) | 1.41 (0.96, 2.06) |
| n/Number of Near-Misses | Direct Effect | Indirect effect | Total Effect (Direct + Indirect) | |||
|---|---|---|---|---|---|---|
| Working Hour → Near-Miss | Working Hour → Job-Related Stress → Fatigue → Near-Miss | Working Hour → Sleep Problem → Fatigue → Near-Miss | Working Hour → Depressive Symptom → Fatigue → Near-Miss | |||
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | ||
| Work experience ≤ 3 years (N = 203) | ||||||
| Working hours/week | ||||||
| 35–40 h/w | 60/28 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 41–50 h/w | 92/53 | 1.37 (0.66, 2.85) | 1.16 (1.00, 1.47) | 1.04 (0.89, 1.24) | 1.01 (0.94, 1.14) | 1.67 (0.77, 3.66) |
| 51–60 h/w | 34/21 | 1.22 (0.45, 3.57) | 1.26 (1.00, 1.90) | 1.35 (1.01, 2.07) | 1.03 (0.90, 1.21) | 2.14 (0.76, 6.48) |
| ≥61 h/w | 17/12 | 1.39 (0.39, 8.26) | 1.52 (1.00, 2.90) | 1.40 (1.02, 2.42) | 1.06 (0.81, 1.45) | 3.14 (1.04, 26.66) |
| Work experience > 3 years (N = 326) | ||||||
| Working hours/week | ||||||
| 35–40 h/w | 109/45 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 41–50 h/w | 129/69 | 1.49 (0.88, 2.68) | 1.10 (1.01, 1.27) | 1.01 (0.96, 1.09) | 1.02 (0.96, 1.12) | 1.68 (0.97, 3.18) |
| 51–60 h/w | 41/23 | 1.48 (0.68, 3.36) | 1.17 (1.02, 1.47) | 1.02 (0.94, 1.15) | 1.05 (0.96, 1.20) | 1.85 (0.85, 4.31) |
| ≥61 h/w | 47/27 | 1.50 (0.72, 3.18) | 1.22 (1.04, 1.54) | 1.02 (0.93, 1.16) | 1.08 (0.98, 1.29) | 2.00 (0.95, 4.37) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anzai, T.; Yamauchi, T.; Ozawa, M.; Takahashi, K. A Generalized Structural Equation Model Approach to Long Working Hours and Near-Misses among Healthcare Professionals in Japan. Int. J. Environ. Res. Public Health 2021, 18, 7154. https://doi.org/10.3390/ijerph18137154
Anzai T, Yamauchi T, Ozawa M, Takahashi K. A Generalized Structural Equation Model Approach to Long Working Hours and Near-Misses among Healthcare Professionals in Japan. International Journal of Environmental Research and Public Health. 2021; 18(13):7154. https://doi.org/10.3390/ijerph18137154
Chicago/Turabian StyleAnzai, Tatsuhiko, Takashi Yamauchi, Masaki Ozawa, and Kunihiko Takahashi. 2021. "A Generalized Structural Equation Model Approach to Long Working Hours and Near-Misses among Healthcare Professionals in Japan" International Journal of Environmental Research and Public Health 18, no. 13: 7154. https://doi.org/10.3390/ijerph18137154
APA StyleAnzai, T., Yamauchi, T., Ozawa, M., & Takahashi, K. (2021). A Generalized Structural Equation Model Approach to Long Working Hours and Near-Misses among Healthcare Professionals in Japan. International Journal of Environmental Research and Public Health, 18(13), 7154. https://doi.org/10.3390/ijerph18137154






