Prevalence and Associated Factors of Falls among Older Adults between Urban and Rural Areas of Shantou City, China
Abstract
:1. Introduction
2. Methods
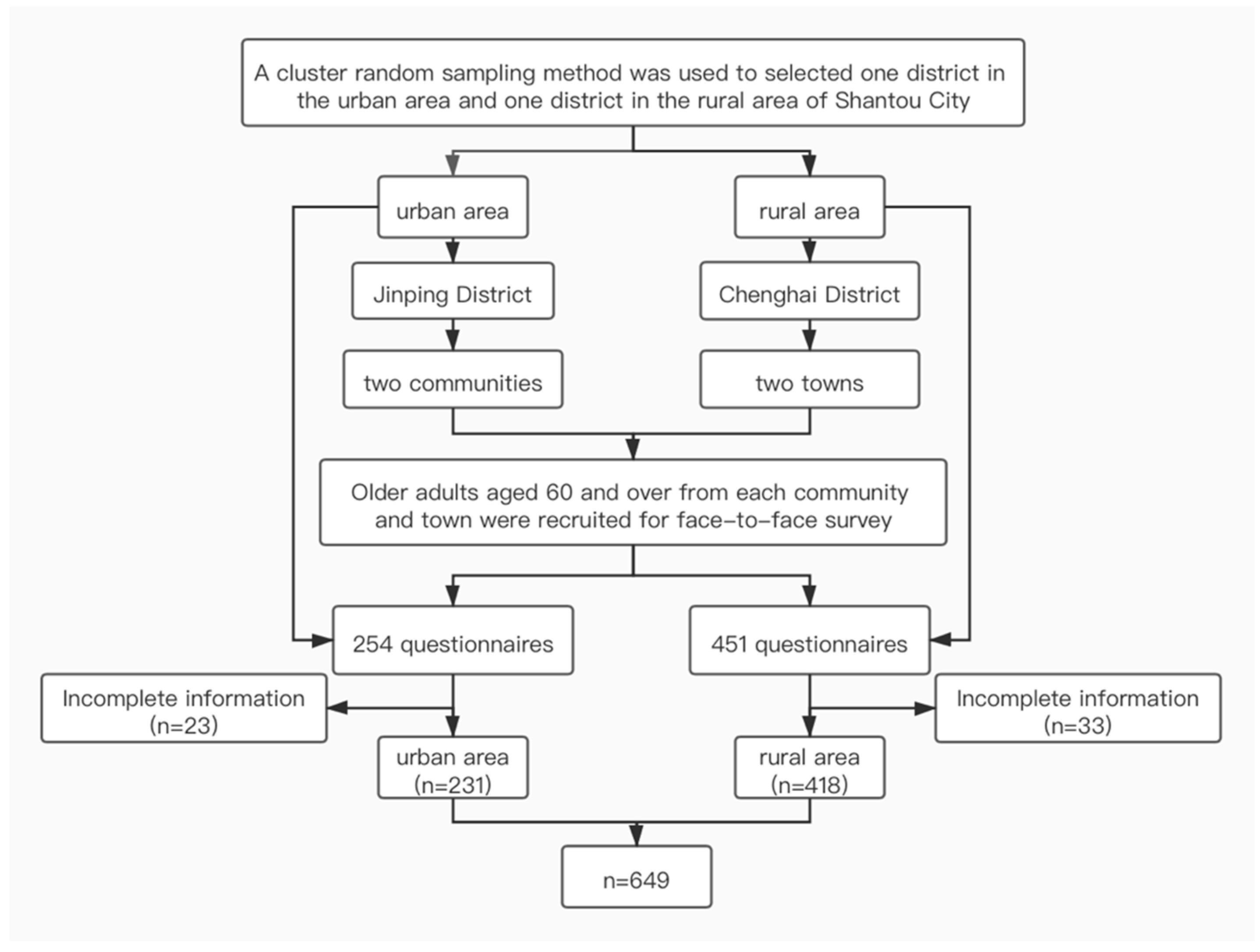
2.1. Subjects
2.2. Study Design
2.3. Data Collection
2.4. Ethics
2.5. Data Analysis
3. Results
3.1. The Incidence of Falls and Injury Rates among Older Adults in Shantou City
3.2. Analysis of Associated Factors of Falls among Older Adults in the Past Year
3.2.1. Univariate Analysis of Associated Factors of Falls among Older Adults in Shantou City
3.2.2. Multivariate Analysis of Associated Factors of Falls among Older Adults in the Past Year
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Falls. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 10 January 2021).
- White, U.E.; Black, A.A.; Wood, J.M.; Delbaere, K. Fear of falling invision impairment. Optom. Vis. Sci. 2015, 92, 730–735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Center for Chronic and Non-Communicable Disease Control and Prevention, Chinese Centre for Disease Control and Prevention. National Injury Surveillance Dataset (2015) [M]; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- National Bureau of Statistics of China. Annual Data. 2019. Available online: http://data.stats.gov.cn/index (accessed on 10 January 2021).
- Li, L.T.; Wang, S.Y. Disease burden and risk factors of falls in the elderly. Chin. J. Epidemiol. 2001, 22, 262–264. [Google Scholar]
- China Disease Prevention and Control Center. Technical Guidelines for Falls Intervention in the Elderly. 2011. Available online: http://www.nhc.gov.cn/wjw/gfxwj/201304/729e74b51ab5434c965ec03164eca46d.shtml (accessed on 10 January 2021).
- Hong, J.; Kong, H.J.; Yoon, H.J. Web-Based Telepresence Exercise Program for Community-Dwelling Elderly Women with a High Risk of Falling: Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mirelman, A.; Rochester, L.; Maidan, I.; Del Din, S.; Alcock, L.; Nieuwhof, F.; Rikkert, M.O.; Bloem, B.R.; Pelosin, E.; Avanzino, L.; et al. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): A randomised controlled trial. Lancet 2016, 388, 1170–1182. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Thomas, S.M.; Veroniki, A.A.; Hamid, J.S.; Cogo, E.; Strifler, L.; Khan, P.A.; Robson, R.S.; Kathryn, M.; MacDonald, H.; et al. Comparisons of Interventions for preventing falls in older adults: A systematic review and meta-analysis. JAMA 2017, 318, 1687–1699. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics. Tabulation on the 2010 Population Census of the People’s Republic of China; China Statistics Press: Beijing, China, 2012. [Google Scholar]
- Zhou, B.Y.; Shi, J.; Yu, P.L. Consequence and risk factors of falls-related injuries in community-dwelling elderly in Beijing. Chin. J. Epidemiol. 2013, 34, 778–781. [Google Scholar]
- Dai, Y.; Wang, Z.Y.; Zhang, Y.Y.; Zhu, W. Investigation on Falls of Elderly and KAP in Yangpu District of Shanghai. Health Educ. Health Promot. 2018, 13, 461–464. [Google Scholar]
- Zhou, H.; Peng, K.; Tiedemann, A.; Peng, J.; Sherrington, C. Risk factors for falls among older community dwellers in Shenzhen, China. Inj. Prev. 2019, 25, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Li, F.F.; Zhou, D.D.; Ye, Z.F.; Ren, J.; Wang, S.M. Epidemiologic characteristics of fall in the elderly in urban and rural areas in Shanghai. Chin. J. Epidemiol. 2019, 40, 779–785. [Google Scholar]
- He, J. Incidence and Risk Factor Analysis of Fall Among the Elderly in Urban and Rural Communities. Master’s Thesis, Ningxia Medical University, Yinchuan, China, 2015. [Google Scholar]
- Gao, M.L.; Song, Y.T. Meta-analysis of the prevalence of fall in elderly in China. Beijing Med. J. 2014, 36, 796–798. [Google Scholar]
- Kalula, S.Z.; Ferreira, M.; Swingler, G.H.; Badri, M. Risk factors for falls in older adults in a South African Urban Community. BMC Geriatr. 2016, 16, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, E.J.; Kim, S.A.; Kim, N.R.; Rhee, J.A.; Yun, Y.W.; Shin, M.H. Risk Factors for Falls in Older Korean Adults: The 2011 Community Health Survey. J. Korean Med. Sci. 2014, 29, 1482–1487. [Google Scholar] [CrossRef] [PubMed]
- Masumoto, T.; Yamada, Y.; Yamada, M.; Nakaya, T.; Kimura, M. Fall risk factors and sex differences among community-dwelling elderly individuals in Japan. A Kameoka study. Jpn. J. Public Health 2015, 62, 390–401. [Google Scholar]
- Hwang, H.F.; Chen, S.J.; Lee-Hsieh, J.; Chien, D.K.; Chen, C.Y.; Lin, M.R. Effects of Home-Based Tai Chi and Lower Extremity Training and Self-Practice on Falls and Functional Outcomes in Older Fallers from the Emergency Department-A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2016, 64, 518–525. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.S.; Ji, W.N.; Bo, Y.C.; Hong, S.M. The association of lower urinary tract symptoms with incidental falls and fear of falling in later life: The Community Health Survey. Neurourol. Urodyn. 2018, 37, 775–784. [Google Scholar] [CrossRef]
- Zhao, Y.L.; Alderden, J.; Lind, B.K.; Kim, H. A Comprehensive Assessment of Risk Factors for Falls in Community-Dwelling Older Adults. J. Gerontol. Nurs. 2018, 4, 40–48. [Google Scholar] [CrossRef]
- Hou, W.H.; Kang, C.M.; Ho, M.H.; Kuo, M.C.; Chen, H.L.; Chang, W.Y. Evaluation of an inpatient fall risk screening tool to identify the most critical fall risk factors in inpatients. J. Clin. Nurs. 2016, 26, 698. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Akers, L.; Chou, L.S.; Pidgeon, D.; Voit, J.; Winters-Stone, K. Effectiveness of a therapeutic Tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling: A randomized clinical trial. JAMA Intern. Med. 2018, 178, 1301–1310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kendrick, D.; Kumar, A.; Carpenter, H.; Zijlstra, G.A.; Skelton, D.A.; Cook, J.R.; Stevens, Z.; Belcher, C.M.; Haworth, D.; Gawler, S.J.; et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst. Rev. 2014, 28, CD009848. [Google Scholar] [CrossRef]
- Huang, L.; Jiang, Y.; Zhu, M.; Li, Z.; Zhao, Q. Assessment of Fall-related Knowledge, Attitude, Behaviorr and Perception of Elderly People in Songjian District, Shanhai. Health Educ. Health Promot. 2019, 14, 398–401. [Google Scholar]
- Lai, E.T.; Yu, R.; Woo, J. The Associations of Income, Education and Income Inequality and Subjective Well-Being among Elderly in Hong Kong-A Multilevel Analysis. Int. J. Environ. Res. Public Health 2020, 17, 1271. [Google Scholar] [CrossRef] [Green Version]
- Berlie, H.D.; Garwood, C.L. Diabetes medications related to an increased risk of falls and fall-related morbidity in the elderly. Ann. Pharm. 2020, 44, 712–717. [Google Scholar] [CrossRef]
- Sumesh, K.; Hugh, K.; Susan, C.; Shi, L.; Zhao, Y.; Jayanti, M.; Uchenna, M.; Vivian, F. Association Between Hypoglycemia and Fall-Related Events in Type 2 Diabetes Mellitus: Analysis of a U.S. Commercial Database. J. Manag. Care Spec. Pharm. 2015, 21, 243–253. [Google Scholar]
- Dhalwani, N.N.; Fahami, R.; Sathanapally, H.; Seidu, S.; Davies, M.J.; Khunti, K. Association between polypharmacy and falls in older adults: A longitudinal study from England. BMJ Open 2017, 7, e016358. [Google Scholar] [CrossRef] [Green Version]
- Sophonratanapokin, B.; Sawangdee, Y.; Soonthorndhada, K. Effect of the living environment on falls among the elderly in Thailand. Southeast Asian J. Trop. Med. Public Health 2012, 43, 1537–1547. [Google Scholar] [PubMed]
| Area | Fall (n) | Fall Rate (%) | Injuries (n) | Injury Rate (%) |
|---|---|---|---|---|
| All | 134 | 20.65 | 94 | 14.48 |
| Urban areas | 63 | 27.27 | 43 | 18.61 |
| Rural areas | 71 | 16.99 | 51 | 12.20 |
| Variable | All (n = 649) | χ2 | p-Value | Urban Areas (n = 231) | χ2 | p-Value | Rural Areas (n = 418) | χ2 | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Fall | Fall | Fall | |||||||
| Areas | 9.610 | 0.002 * | |||||||
| Urban | 63 (27.27) | ||||||||
| Rural | 71 (16.99) | ||||||||
| Sex | 3.035 | 0.082 | 0.547 | 0.459 | 2.445 | 0.118 | |||
| Male | 33 (16.50) | 16(23.88) | 17(12.78) | ||||||
| Female | 101(22.49) | 47(28.66) | 54(18.95) | ||||||
| Age | 0.816 | 0.665 | 0.364 | 0.834 | 3.282 | 0.194 | |||
| 60–69 | 90(19.91) | 48(28.24) | 42(14.89) | ||||||
| 70–79 | 37(23.13) | 13(24.07) | 24(22.64) | ||||||
| ≥80 | 7(18.92) | 2(28.57) | 5(16.67) | ||||||
| Education level | 5.203 | 0.023 * | 7.513 | 0.006 * | 0.967 | 0.325 | |||
| High school and below | 118(22.39) | 55(31.98) | 63(17.75) | ||||||
| College and above | 16(13.11) | 8(13.56) | 8(12.70) | ||||||
| Previous occupation | 10.857 | 0.001 * | 0.687 # | 6.021 | 0.014 * | ||||
| Farmer | 102(24.58) | 3(37.50) | 29(12.83) | ||||||
| Non farmer | 32(13.68) | 60(26.91) | 42(21.88) | ||||||
| Living alone | 0.000 | 0.989 | 0.393 | 0.531 | 1.311 | 0.252 | |||
| No | 104(20.63) | 57(27.94) | 47(15.67) | ||||||
| Yes | 30(20.69) | 6(22.22) | 24(20.34) | ||||||
| Calcium or Vitamin D | 4..205 | 0.040 * | 1.401 | 0.236 | 1.000# | ||||
| No | 112(19.48) | 44(25.29) | 68(16.96) | ||||||
| Yes | 22(29.73) | 19(33.33) | 3(17.65) | ||||||
| Vision | 0.142 | 0.707 | 0.003 | 0.956 | 1.161 | 0.281 | |||
| Normal | 56(21.37) | 40(27.40) | 16(13.79) | ||||||
| Weaken | 78(20.16) | 23(27.06) | 55(18.21) | ||||||
| Dizziness | 0.158 # | 0.349 # | 1.000 # | ||||||
| No | 131(20.40) | 60(26.67) | 71(17.03) | ||||||
| Yes | 3(42.86) | 3(50.00) | 0(0.00) | ||||||
| Diabetes | 0.260 | 0.610 | 0.869 | 0.351 | 0.383 | 0.536 | |||
| No | 120(20.94) | 58(26.61) | 62(17.46) | ||||||
| Yes | 14(18.42) | 5(38.46) | 9(14.29) | ||||||
| Hypertension | 1.976 | 0.160 | 3.388 | 0.066 | 1.050 | 0.306 | |||
| No | 83(19.08) | 43(24.29) | 40(15.50) | ||||||
| Yes | 51(23.83) | 20(37.04) | 31(19.38) | ||||||
| Heart disease | 2.493 | 0.114 | 0.102 | 0.749 | 1.000 # | ||||
| No | 123(22.45) | 45(32.85) | 78(18.98) | ||||||
| Yes | 30(29.70) | 29(30.85) | 1(14.29) | ||||||
| Hypotension | 1.428 | 0.232 | 1.322 | 0.250 | 1.000 # | ||||
| No | 128(20.32) | 58(26.48) | 70(17.03) | ||||||
| Yes | 6(31.58) | 5(41.67) | 1(14.29) | ||||||
| Diabetes medicine | 1.018 | 0.313 | 6.704 | 0.023 * | 0.000 | 1.000 | |||
| No | 117(20.10) | 55(25.35) | 62(16.99) | ||||||
| Yes | 17(25.37) | 8(57.14) | 9(16.98) | ||||||
| Hypertension medicine | 2.333 | 0.127 | 0.230 | 0.632 | 1.008 | 0.315 | |||
| No | 85(19.02) | 43(24.16) | 42(15.61) | ||||||
| Yes | 49(24.26) | 20(27.03) | 29(19.46) | ||||||
| Incontinence | 14.238 | >0.001 * | 5.702 | 0.017 * | 8.126 | 0.004 * | |||
| No | 113(22.24) | 53(25.12) | 60(15.50) | ||||||
| Yes | 21(41.18) | 10(50.00) | 11(35.48) | ||||||
| Cane | 4.601 | 0.032 * | 1.000 # | 8.533 | 0.014 * | ||||
| No | 117(19.63) | 62(27.31) | 55(14.9) | ||||||
| Needed | 17(32.08) | 1(25.00) | 16(30.3) | ||||||
| Home environment issues | 2.087 | 0.352 | 5.080 | 0.079 | 7.685 | 0.021 | |||
| ≤1 | 60(21.66) | 37(33.94) | 23(13.69) a | ||||||
| 2–3 | 56(18.54) | 22(22.68) | 34(16.59) a,b | ||||||
| >3 | 18(25.71) | 4(16.00) | 14(31.11) b | ||||||
| Balance ability | 42.891 | <0.001 * | 14.65 | <0.001 * | 26.152 | <0.001 * | |||
| Normal | 35(10.51) | 16(15.09) | 19(8.37) | ||||||
| Reduced | 99(31.33) | 47(37.60) | 52(27.23) | ||||||
| Fear of falling | 5.753 | 0.016 * | 5.697 | 0.017 * | 4.432 | 0.035 * | |||
| Not afraid | 49(16.50) | 30(21.58) | 19(12.03) | ||||||
| Afraid | 85(24.15) | 33(35.87) | 52(20.00) | ||||||
| Can fall be prevented | 6.806 | 0.033 * | 2.959 | 0.228 | 0.256 | 0.880 | |||
| No | 80(18.91) a | 26(27.08) | 54(16.51) | ||||||
| Yes | 35(20.59) a,b | 19(22.35) | 16(18.82) | ||||||
| Do not know | 19(33.93) b | 18(36.00) | 1(16.67) | ||||||
| Fall prevention education | 4.693 | 0.030 * | 4.456 | 0.035 * | 0.682 | 0.409 | |||
| No | 117(22.32) | 59(29.80) | 58(17.79) | ||||||
| Yes | 17(13.60) | 4(12.12) | 13(14.13) |
| Variable | Assignment |
|---|---|
| Areas | Rural = 1, Urban = 2 |
| Sex | Male = 1, Female = 2 |
| Age | 1 = 60–69, 2 = 70–79, 3 = ≥80 |
| Education level Previous occupation | College and above = 1, High school and below = 2 Non-farmer = 1, Farmer = 2 |
| Calcium or Vitamin D | Yes = 1, No = 2 |
| Diabetes medicine | No =1, Yes =2 |
| Incontinence | No =1, Yes =2 |
| Cane | No =1, Yes =2 |
| Home environment issues | 1 = ≤1, 2 = 2–3, 3 = >3 |
| Balance ability | Normal = 1, Reduced = 2 |
| Fear of falling | Afraid = 1, Not afraid = 2 |
| Can fall be prevented | Yes =1, Do not know = 2, No =3 |
| Fall prevention education | No = 1, Yes = 2 |
| Factor | β | SE | Wald | p-Value * | OR | 95% CI |
|---|---|---|---|---|---|---|
| All | ||||||
| Education level (reference: College and above) | 0.870 | 0.308 | 7.980 | 0.005 * | 2.387 | 1.305–4.366 |
| Previous occupation (reference: Farmer) | 0.946 | 0.239 | 15.715 | <0.001 * | 2.574 | 1.613–4.109 |
| Incontinence | 1.058 | 0.327 | 10.715 | 0.001 * | 2.881 | 1.517–5.470 |
| Fall prevention education | 0.619 | 0.295 | 4.389 | 0.036 * | 1.856 | 1.041–3.311 |
| Balance ability (reference: Normal) | 1.365 | 0.223 | 37.644 | <0.001 * | 3.917 | 2.532–6.058 |
| Urban areas | ||||||
| Education level (reference: College and above) | 1.314 | 0.458 | 8.253 | 0.004 * | 3.722 | 1.518–9.126 |
| Diabetes medicine use | 1.346 | 0.608 | 4.905 | 0.027 * | 3.842 | 1.167–12.643 |
| Incontinence | 1.551 | 0.554 | 7.831 | 0.005 * | 4.717 | 1.592–13.979 |
| Fall prevention education | 1.203 | 0.596 | 4.079 | 0.043 * | 3.331 | 1.036–10.710 |
| Balance ability (reference: Normal) | 1.273 | 0.348 | 13.386 | <0.001 * | 3.573 | 1.806–7.069 |
| Rural areas | ||||||
| Previous occupation (reference: farmer) | 0.885 | 0.286 | 9.579 | 0.002 * | 2.422 | 1.383–4.242 |
| Incontinence (reference: No) | 0.901 | 0.437 | 4.249 | 0.039 * | 2.462 | 1.045–5.800 |
| Home environment issues (reference: ≤1) | 8.344 | 0.015 * | ||||
| 2–3 | 0.324 | 0.308 | 1.103 | 0.294 | 1.382 | 0.756–2.528 |
| >3 | 1.241 | 0.430 | 8.311 | 0.004 * | 3.459 | 1.488–8.042 |
| Balance ability (reference: Normal) | 1.447 | 0.301 | 23.091 | <0.001 * | 4.250 | 2.355–7.668 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, X.; Lin, Z.; Gao, R.; Yang, Y.; Li, L. Prevalence and Associated Factors of Falls among Older Adults between Urban and Rural Areas of Shantou City, China. Int. J. Environ. Res. Public Health 2021, 18, 7050. https://doi.org/10.3390/ijerph18137050
Chen X, Lin Z, Gao R, Yang Y, Li L. Prevalence and Associated Factors of Falls among Older Adults between Urban and Rural Areas of Shantou City, China. International Journal of Environmental Research and Public Health. 2021; 18(13):7050. https://doi.org/10.3390/ijerph18137050
Chicago/Turabian StyleChen, Xiaodong, Zeting Lin, Ran Gao, Yijian Yang, and Liping Li. 2021. "Prevalence and Associated Factors of Falls among Older Adults between Urban and Rural Areas of Shantou City, China" International Journal of Environmental Research and Public Health 18, no. 13: 7050. https://doi.org/10.3390/ijerph18137050
APA StyleChen, X., Lin, Z., Gao, R., Yang, Y., & Li, L. (2021). Prevalence and Associated Factors of Falls among Older Adults between Urban and Rural Areas of Shantou City, China. International Journal of Environmental Research and Public Health, 18(13), 7050. https://doi.org/10.3390/ijerph18137050







