The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
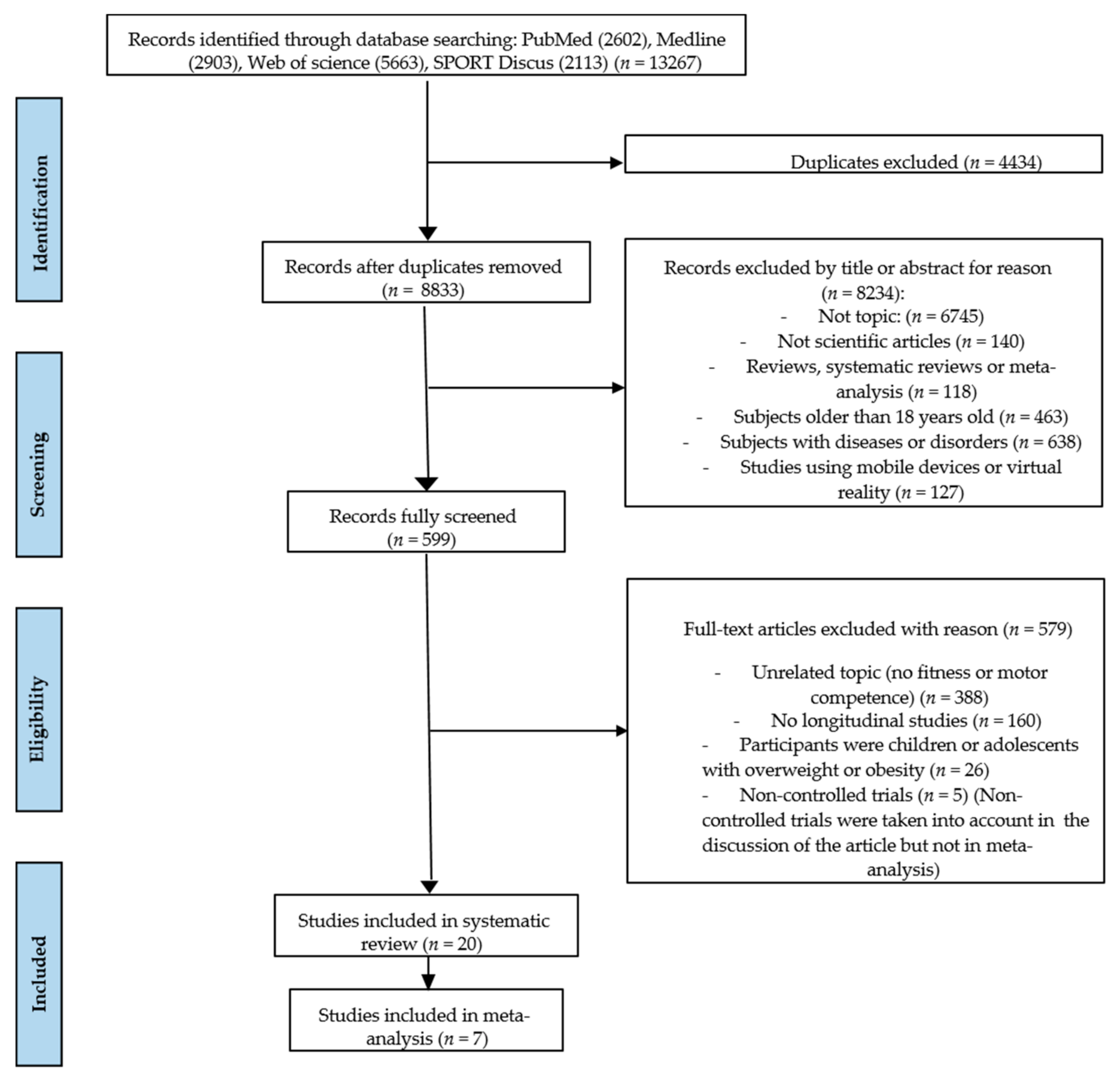
2.4. Search Summary
2.5. Risk of Bias
2.6. Data Extraction
2.7. Meta-Analyses
3. Results and Discussion
3.1. AVG Interventions
3.2. AVG Effects
3.2.1. Body Mass Index and Percentage of Body Fat
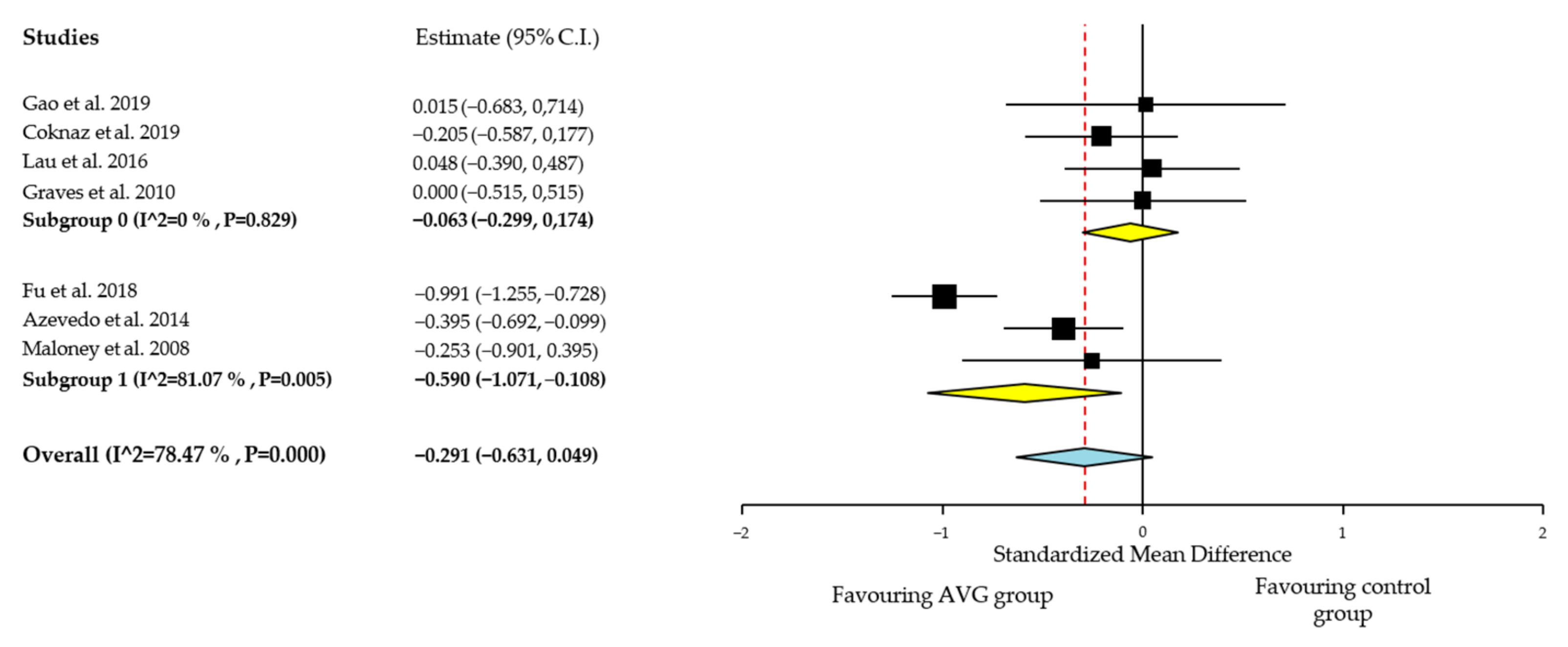
Quantitative Analysis of BMI
3.2.2. Cardiorespiratory Fitness
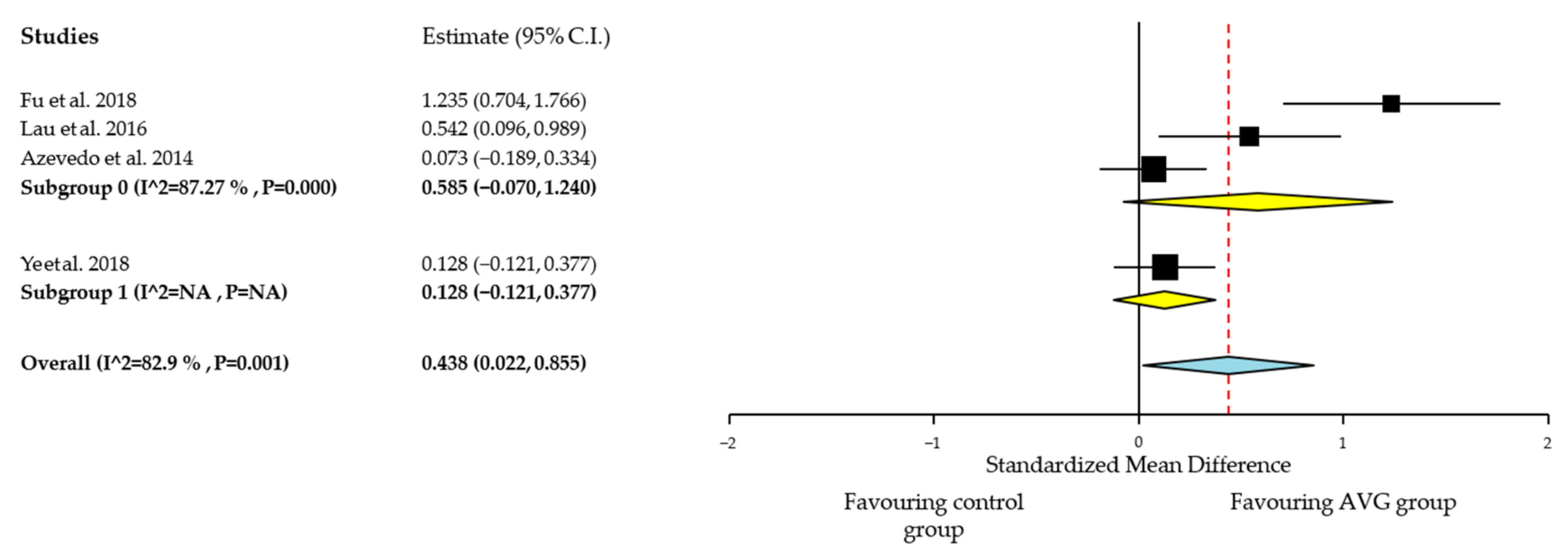
Quantitative Analysis of Cardiorespiratory Fitness
3.2.3. Muscular Fitness
3.2.4. Motor Competence
4. Limitations
5. Perspectives
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef]
- Chen, W.; Hammond-Bennett, A.; Hypnar, A.; Mason, S. Health-related physical fitness and physical activity in elementary school students. BMC Public Health 2018, 18, 195. [Google Scholar] [CrossRef] [PubMed]
- Pahkala, K.; Hernelahti, M.; Heinonen, O.J.; Raittinen, P.; Hakanen, M.; Lagström, H.; Viikari, J.S.A.; Rönnemaa, T.; Raitakari, O.T.; Simell, O. Body mass index, fitness and physical activity from childhood through adolescence. Br. J. Sports Med. 2013, 47, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Blair, S.N.; Cheng, Y.; Holder, J.S. Is physical activity or physical fitness more important in defining health benefits? Sci. Sport. Exerc. 2001, 33, 379–399. [Google Scholar] [CrossRef] [PubMed]
- Tomkinson, G.R.; Carver, K.D.; Atkinson, F.; Daniell, N.D.; Lewis, L.K.; Fitzgerald, J.S.; Lang, J.; Ortega, F.B. European normative values for physical fitness in children and adolescents aged 9–17 years: Results from 2 779 165 Eurofit performances representing 30 countries. Br. J. Sports Med. 2017, 52, 1445–1456. [Google Scholar] [CrossRef] [PubMed]
- Micheli, L.; Mountjoy, M.; Engebretsen, L.; Hardman, K.; Kahlmeier, S.; Lambert, E.; Ljungqvist, A.; Matsudo, V.; McKay, H.; Sundberg, C.J. Fitness and health of children through sport: The context for action. Br. J. Sports Med. 2011, 45, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Ahluwalia, N.; Dalmasso, P.; Rasmussen, M.; Lipsky, L.; Currie, C.; Haug, E.; Kelly, C.; Damsgaard, M.T.; Due, P.; Tabak, I.; et al. Trends in overweight prevalence among 11-, 13- and 15-year-olds in 25 countries in Europe, Canada and USA from 2002 to 2010. Eur. J. Public Health 2015, 25, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Nittari, G.; Scuri, S.; Petrelli, F.; Pirillo, I.; Di Luca, N.M.; Grappasonni, I. Fighting obesity in children from European World Health Organization member states. Epidemiological data, medical-social aspects, and prevention programs. La Clin. Ter. 2019, 170, e223–e230. [Google Scholar] [CrossRef]
- Westerterp, K.R. Changes in physical activity over the lifespan: Impact on body composition and sarcopenic obesity. Obes. Rev. 2018, 19, 8–13. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Alonso-Martinez, A.M.; Ramírez-Vélez, R.; Izquierdo, M. Effects of Exercise Intervention on Health-Related Physical Fitness and Blood Pressure in Preschool Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sports Med. 2019, 50, 187–203. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.; Pate, R.R.; Gorber, S.C.; Kho, M.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, 197–239. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; Rial Rebullido, T.; MacDonald, J.P. Pediatric Inactivity Triad: A Risky PIT. Curr. Sports Med. Rep. 2018, 17, 45–47. [Google Scholar] [CrossRef]
- Moliner-Urdiales, D.; Ruiz, J.R.; Ortega, F.B.; Jiménez-Pavón, D.; Vicente-Rodriguez, G.; Rey-López, J.P.; Martínez-Gómez, D.; Casajús, J.A.; Mesana, M.I.; Marcos, A.; et al. Secular trends in health-related physical fitness in Spanish adolescents: The AVENA and HELENA Studies. J. Sci. Med. Sport 2010, 13, 584–588. [Google Scholar] [CrossRef]
- Cohen, D.; Voss, C.; Taylor, M.; Delextrat, A.; Ogunleye, A.; Sandercock, G. Ten-year secular changes in muscular fitness in English children. Acta Paediatr. Int. J. Paediatr. 2011, 100, e175–e177. [Google Scholar] [CrossRef]
- Albon, H.M.; Hamlin, M.J.; Ross, J.J. Secular trends and distributional changes in health and fitness performance variables of 10-14-year-old children in New Zealand between 1991 and 2003. Br. J. Sports Med. 2010, 44, 263–269. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; Bruno, L.E. A fundamental approach for treating pediatric dynapenia in kids. ACSM Health Fit. J. 2017, 21, 18–24. [Google Scholar] [CrossRef]
- Smith, J.J.; Eather, N.; Weaver, R.G.; Riley, N.; Beets, M.W.; Lubans, D.R. Behavioral Correlates of Muscular Fitness in Children and Adolescents: A Systematic Review. Sports Med. 2019, 49, 887–904. [Google Scholar] [CrossRef]
- Fühner, T.; Kliegl, R.; Arntz, F.; Kriemler, S.; Granacher, U. An Update on Secular Trends in Physical Fitness of Children and Adolescents from 1972 to 2015: A Systematic Review. Sports Med. 2021, 51, 303–320. [Google Scholar] [CrossRef]
- Lai, S.K.; Costigan, S.A.; Morgan, P.J.; Lubans, D.R.; Stodden, D.F.; Salmon, J.; Barnett, L.M. Do School-Based Interventions Focusing on Physical Activity, Fitness, or Fundamental Movement Skill Competency Produce a Sustained Impact in These Outcomes in Children and Adolescents? A Systematic Review of Follow-Up Studies. Sports Med. 2014, 44, 67–79. [Google Scholar] [CrossRef]
- Jaakkola, T.; Yli-Piipari, S.; Huotari, P.; Watt, A.; Liukkonen, J. Fundamental movement skills and physical fitness as predictors of physical activity: A 6-year follow-up study. Scand. J. Med. Sci. Sports 2016, 26, 74–81. [Google Scholar] [CrossRef]
- Cattuzzo, M.T.; Henrique, R.D.S.; Ré, A.H.N.; de Oliveira, I.S.; Melo, B.M.; Moura, M.D.S.; de Araújo, R.C.; Stodden, D. Motor competence and health related physical fitness in youth: A systematic review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef]
- Milne, N.; Leong, G.M.; Hing, W. The relationship between children’s motor proficiency and health-related fitness. J. Paediatr. Child Health 2016, 52, 825–831. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental Movement Skills in Children and Adolescents Review of Associated Health Benefits. Sport. Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef]
- American College of Sport Medicine Exercise is Medicine: The Power of Physical Activity. Available online: https://www.exerciseismedicine.org/support_page.php/physical-activity-health-impact/ (accessed on 10 April 2020).
- Beedie, C.; Mann, S.; Jimenez, A.; Kennedy, L.; Lane, A.M.; Domone, S.; Wilson, S.; Whyte, G. Death by effectiveness: Exercise as medicine caught in the efficacy trap! Br. J. Sports Med. 2016, 50, 323–324. [Google Scholar] [CrossRef]
- Peng, W.; Lin, J.-H.; Crouse, J. Is Playing Exergames Really Exercising? A Meta-Analysis of Energy Expenditure in Active Video Games. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 681–688. [Google Scholar] [CrossRef]
- Sween, J.; Wallington, S.F.; Sheppard, V.; Taylor, T.; Llanos, A.; Adams-Campbell, L.L. The Role of Exergaming in Improving Physical Activity: A Review. J. Phys. Act. Health 2014, 11, 864–870. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, S.; Pasco, D.; Pope, Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes. Rev. 2015, 16, 783–794. [Google Scholar] [CrossRef]
- Leblanc, A.G.; Chaput, J.-P.; McFarlane, A.; Colley, R.C.; Thivel, D.; Biddle, S.J.H.; Maddison, R.; Leatherdale, S.T.; Tremblay, M.S. Active Video Games and Health Indicators in Children and Youth: A Systematic Review. PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
- Biddiss, E.; Irwin, J. Active Video Games to Promote Physical Activity in Children and Youth A Systematic Review. Arch. Pediatr. Adolesc. Med. 2010, 164, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.; Cerin, E.; Baranowski, T. Active Video Games for Youth: A Systematic Review. J. Phys. Act. Health 2011, 8, 724–737. [Google Scholar] [CrossRef] [PubMed]
- Comeras-Chueca, C.; Villalba-Heredia, L.; Pérez-Llera, M.; Lozano-Berges, G.; Marín-Puyalto, J.; Vicente-Rodríguez, G.; Matute-Llorente, Á.; Casajús, J.A.; González-Agüero, A. Assessment of Active Video Games’ Energy Expenditure in Children with Overweight and Obesity and Differences by Gender. Int. J. Environ. Res. Public Health 2020, 17, 6714. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, L.B.; Watson, D.B.; Haighton, C.; Adams, J. The effect of dance mat exergaming systems on physical activity and health—related outcomes in secondary schools: Results from a natural experiment. BMC Public Health 2014, 14. [Google Scholar] [CrossRef]
- Fu, Y.; Burns, R.D. Effect of an Active Video Gaming Classroom Curriculum on Health-Related Fitness, School Day Step Counts, and Motivation in Sixth Graders. J. Phys. Act. Health 2018, 15, 644–650. [Google Scholar] [CrossRef]
- Fu, Y.; Burns, R.D.; Constantino, N.; Zhang, P. Differences in Step Counts, Motor Competence, and Enjoyment Between an Exergaming Group and a Non-Exergaming Group. Games Health J. 2018, 7, 335–340. [Google Scholar] [CrossRef]
- Ye, S.; Lee, J.E.; Stodden, D.F.; Gao, Z. Impact of Exergaming on Children’s Motor Skill Competence and Health-Related Fitness: A Quasi-Experimental Study. J. Clin. Med. 2018, 7, 261. [Google Scholar] [CrossRef]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated March 2011]; Cochrane: London, UK, 2011. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Estarli, M.; Barrera, E.S.A.; et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev. Esp. Nutr. Hum. Diet. 2016, 20, 148–160. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, P.; Felden, É.P.G.; Zequinão, M.A.; Cordeiro, P.C.; de Freitas, K.T.D.; dos Santos, J.O.L.; Cardoso, F.L. Positive effect of a motor intervation program with exergames: A blind randomized trial. Int. J. Game Based Learn. 2020, 10, 55–64. [Google Scholar] [CrossRef]
- McGann, J.; Issartel, J.; Hederman, L.; Conlan, O. Hop.Skip.Jump.Games: The effect of “principled” exergameplay on children’s locomotor skill acquisition. Br. J. Educ. Technol. 2019, 51, 798–816. [Google Scholar] [CrossRef]
- Gao, Z.; Lee, J.E.; Zeng, N.; Pope, Z.C.; Zhang, Y.; Li, X. Home-Based Exergaming on Preschoolers’ Energy Expenditure, Cardiovascular Fitness, Body Mass Index and Cognitive Flexibility: A Randomized Controlled Trial. J. Clin. Med. 2019, 8, 1745. [Google Scholar] [CrossRef] [PubMed]
- Coknaz, D.; Mirzeoglu, A.D.; Atasoy, H.I.; Alkoy, S.; Coknaz, H.; Goral, K. A digital movement in the world of inactive children: Favourable outcomes of playing active video games in a pilot randomized trial. Eur. J. Nucl. Med. Mol. Imaging 2019, 178, 1567–1576. [Google Scholar] [CrossRef]
- Ye, S.; Pope, Z.C.; Lee, J.E.; Gao, Z. Effects of school-based exergaming on urban children’s physical activity and cardiorespiratory fitness: A quasi-experimental study. Int. J. Environ. Res. Public Health 2019, 16, 4080. [Google Scholar] [CrossRef]
- Lau, P.W.C.; Wang, J.J.; Maddison, R. A Randomized-Controlled Trial of School-Based Active Videogame Intervention on Chinese Children’s Aerobic Fitness, Physical Activity Level, and Psychological Correlates. Games Health J. 2016, 5, 405–412. [Google Scholar] [CrossRef]
- Vernadakis, N.; Papastergiou, M.; Zetou, E.; Antoniou, P. The impact of an exergame-based intervention on children’s fundamental motor skills. Comput. Educ. 2015, 83, 90–102. [Google Scholar] [CrossRef]
- Johnson, T.M.; Ridgers, N.D.; Hulteen, R.M.; Mellecker, R.R.; Barnett, L.M. Does playing a sports active video game improve young children’s ball skill competence? J. Sci. Med. Sport 2016, 19, 432–436. [Google Scholar] [CrossRef]
- Mombarg, R.; Jelsma, D.; Hartman, E. Effect of Wii-intervention on balance of children with poor motor performance. Res. Dev. Disabil. 2013, 34, 2996–3003. [Google Scholar] [CrossRef]
- Sheehan, D.P.; Katz, L. The effects of a daily, 6-week exergaming curriculum on balance in fourth grade children. J. Sport Health Sci. 2013, 2, 131–137. [Google Scholar] [CrossRef]
- Sheehan, D.P.; Katz, L. The impact of a six week exergaming curriculum on balance with grade three school children using the wii FIT+TM. Int. J. Comput. Sci. Sport 2012, 11, 5–22. [Google Scholar] [CrossRef]
- Maloney, A.E.; Stempel, A.; Wood, M.E.; Patraitis, C.; Beaudoin, C. Can Dance Exergames Boost Physical Activity as a School-Based Intervention? Games Health J. 2012, 1, 416–421. [Google Scholar] [CrossRef]
- Graves, L.E.F.; Ridgers, N.D.; Atkinson, G.; Stratton, G. The Effect of Active Video Gaming on Children’s Physical Activity, Behavior Preferences and Body Composition. Pediatr. Exerc. Sci. 2010, 22, 535–546. [Google Scholar] [CrossRef]
- Maloney, A.E.; Bethea, T.C.; Kelsey, K.S.; Marks, J.T.; Paez, S.; Rosenberg, A.M.; Catellier, D.J.; Hamer, R.M.; Sikich, L. A Pilot of a Video Game (DDR) to Promote Physical Activity and Decrease Sedentary Screen Time. Obesity 2008, 16, 2074–2080. [Google Scholar] [CrossRef]
- Cifci, C.; Baspinar, S.G. The Effects of Active Video Games on Strength, Vertical Jumping and Flexibility in Children Aged 12 to 15 Years Old. Int. J. Appl. Exerc. Physiol. 2020, 9, 70–77. [Google Scholar] [CrossRef]
- Gao, Z.; Zeng, N.; Pope, Z.C.; Wang, R.; Yu, F. Effects of exergaming on motor skill competence, perceived competence, and physical activity in preschool children. J. Sport Health Sci. 2019, 8, 106–113. [Google Scholar] [CrossRef]
- De Brito-Gomes, J.L.; Perrier-Melo, R.J.; De Oliveira, S.F.M.; Guimarães, F.J.D.S.P.; Costa, M.D.C. Physical Effort, Energy Expenditure, and Motivation in Structured and Unstructured Active Video Games: A Randomized Controlled Trial. Hum. Mov. 2016, 17, 190–198. [Google Scholar] [CrossRef]
- Owens, S.G.; Garner, J.C.; Loftin, J.M.; van Blerk, N.; Ermin, K. Changes in Physical Activity and Fitness after 3 Months of Home Wii Fit Use. J. Strength Cond. Res. 2011, 25, 3191–3197. [Google Scholar] [CrossRef]
- Bethea, T.C.; Berry, D.; Maloney, A.E.; Sikich, L. Pilot Study of an Active Screen Time Game Correlates with Improved Physical Fitness in Minority Elementary School Youth. Games Health J. 2012, 1, 29–36. [Google Scholar] [CrossRef]
- Gao, Z.; Zeng, N.; McDonough, D.J.; Su, X. A Systematic Review of Active Video Games on Youth’s Body Composition and Physical Activity. Int. J. Sports Med. 2020, 41, 561–573. [Google Scholar] [CrossRef]
- Hernández-Jiménez, C.; Sarabia, R.; Paz-Zulueta, M.; Paras-Bravo, P.; Pellico, A.; Azcona, L.R.; Blanco, C.; Madrazo, M.; Agudo, M.J.; Sarabia, C.; et al. Impact of Active Video Games on Body Mass Index in Children and Adolescents: Systematic Review and Meta-Analysis Evaluating the Quality of Primary Studies. Int. J. Environ. Res. Public Health 2019, 16, 2424. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Pinto, R.Z.; Saraiva, B.T.C.; Tebar, W.R.; Delfino, L.D.; Franco, M.R.; Silva, C.C.M.; Christofaro, D.G.D. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 4–12. [Google Scholar] [CrossRef]
- Zeng, N.; Gao, Z. Exergaming and obesity in youth: Current perspectives. Int. J. Gen. Med. 2016, 9, 275–284. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, S. Are field-based exergames useful in preventing childhood obesity? A systematic review. Int. Assoc. Study Obes. 2014, 15, 1–16. [Google Scholar] [CrossRef]
- Norris, E.; Hamer, M.; Stamatakis, E. Active Video Games in Schools and Effects on Physical Activity and Health: A Systematic Review. J. Pediatr. 2016, 172, 40–46.e5. [Google Scholar] [CrossRef]
- Lamboglia, C.M.G.F.; Da Silva, V.T.B.L.; Filho, J.E.D.V.; Pinheiro, M.H.N.P.; Munguba, M.; Júnior, F.V.I.S.; De Paula, F.A.R.; Da Silva, C.A.B. Exergaming as a Strategic Tool in the Fight against Childhood Obesity: A Systematic Review. J. Obes. 2013, 2013, 438364. [Google Scholar] [CrossRef] [PubMed][Green Version]
- George, A.M.; Rohr, L.E.; Byrne, J. Impact of Nintendo Wii Games on Physical Literacy in Children: Motor Skills, Physical Fitness, Activity Behaviors, and Knowledge. Sports 2016, 4, 3. [Google Scholar] [CrossRef]
- Gao, Z.; Lee, J.E.; Pope, Z.; Zhang, D. Effect of Active Videogames on Underserved Children’s Classroom Behaviors, Effort, and Fitness. Games Health J. 2016, 5, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Kari, T. Can Exergaming Promote Physical Fitness and Physical Activity? Int. J. Gaming Comput. Simul. 2014, 6, 59–77. [Google Scholar] [CrossRef]
- Kari, T. Promoting Physical Activity and Fitness with Exergames. In Transforming Gaming and Computer Simulation Technologies across Industries; IGI Global: Hershey, PA, USA, 2016; pp. 225–245. [Google Scholar] [CrossRef]
- Van Brussel, M.; Bongers, B.C.; Hulzebos, E.H.; Burghard, M.; Takken, T. A Systematic Approach to Interpreting the Cardiopulmonary Exercise Test in Pediatrics. Pediatr. Exerc. Sci. 2019, 31, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, N.; Welsman, J.; Winsley, R. Is Peak VO2a Maximal Index of Children’s Aerobic Fitness? Int. J. Sport. Med. 1996, 17, 356–359. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.C.; Jelsma, L.D.; Ferguson, G.D. The effect of exergames on functional strength, anaerobic fitness, balance and agility in children with and without motor coordination difficulties living in low-income communities. Hum. Mov. Sci. 2017, 55, 327–337. [Google Scholar] [CrossRef]
- De Medeirosa, P.; Capistranoa, R.; Almeida, M.; Aparecida, S.; Silva, T.; Cardoso, F. Exergames as a tool for the acquisition and development of motor skills and abilities: A systematic review. Rev. Paul. Pediatr. 2017, 35, 464–471. [Google Scholar] [CrossRef][Green Version]
- Page, Z.E.; Barrington, S.; Edwards, J.; Barnett, L.M. Do active video games benefit the motor skill development of non-typically developing children and adolescents: A systematic review. J. Sci. Med. Sport 2017, 20, 1087–1100. [Google Scholar] [CrossRef]
- De Meester, A.; Maes, J.; Stodden, D.; Cardon, G.; Goodway, J.; Lenoir, M.; Haerens, L. Identifying profiles of actual and perceived motor competence among adolescents: Associations with motivation, physical activity, and sports participation. J. Sports Sci. 2016, 34, 2027–2037. [Google Scholar] [CrossRef]
- Bardid, F.; De Meester, A.; Tallir, I.; Cardon, G.; Lenoir, M.; Haerens, L. Configurations of actual and perceived motor competence among children: Associations with motivation for sports and global self-worth. Hum. Mov. Sci. 2016, 50, 1–9. [Google Scholar] [CrossRef]
| Study, Year | R | D | Mi | Me | S | O |
|---|---|---|---|---|---|---|
| Medeiros et al., 2020 [46] |  |  |  |  |  |  |
| McGann et al., 2019 [47] |  |  |  |  |  |  |
| Gao et al., 2019 [48] |  |  |  |  |  |  |
| Coknaz et al., 2019 [49] |  |  |  |  |  |  |
| Ye et al., 2019 [50] |  |  |  |  |  |  |
| Fu et al., 2018 [37] |  |  |  |  |  |  |
| Lau et al., 2017 [51] |  |  |  |  |  |  |
| Vernadakis et al., 2015 [52] |  |  |  |  |  |  |
| Johnson et al., 2015 [53] |  |  |  |  |  |  |
| Mombarg et al., 2013 [54] |  |  |  |  |  |  |
| Sheehan et al., 2013 [55] |  |  |  |  |  |  |
| Sheehan et al., 2012 [56] |  |  |  |  |  |  |
| Maloney et al., 2012 [57] |  |  |  |  |  |  |
| Graves et al., 2010 [58] |  |  |  |  |  |  |
| Maloney et al., 2008 [59] |  |  |  |  |  |  |
| Author, Year | Pre-Intervention | At Intervention | Post-Intervention | Overall Risk of Bias | ||||
|---|---|---|---|---|---|---|---|---|
| Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Result | ||
| Çifci et al., 2020 [60] | LOW | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW |
| Gao et al., 2019 [61] | LOW | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW |
| Fu et al., 2018 [36] | LOW | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW |
| Ye et al., 2018 [38] | LOW | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW |
| Azevedo et al., 2014 [35] | LOW | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW |
| Study [Ref.] | Participants | Study Design | Intervention | Control | Training | Variables and Test Used | Outcomes | |
|---|---|---|---|---|---|---|---|---|
| n | Age | |||||||
| Medeiros et al., 2020 [46] | n = 64 male (30) female (34) | 9.09 ± 0.75 years | RCT | Xbox Kinect (n = 32) | CG: PE curriculum class (n = 32) | Period: 9 weeks Frequency: 2 days per week Duration: 45 min per session | MC (TGMD-2) | AVG and CG showed improvements in MC, but AVG showed improvements in more skills of TGMD-2 |
| Çifci et al., 2020 [60] | n = 100 male (50) female (50) | 12–15 years | Non-RCT | Xbox Kinect (n = 50) | No intervention (n = 50) | Period: 8 weeks Frequency: 40 min per week | MF (handgrip, leg dynamometry and vertical jump) | AVG improved MF. No differences on MF between AVG and CG were observed. |
| McGann et al., 2019 [47] | n = 40 male (21) female (19) | 5–7 years | RCT | AVG focus on MC playing at Scratch with Kinect (n = 20) | Traditional AVG (n = 20) | Period: 8 weeks Frequency: Daily | MC (TGMD-2) | Improvements on MC for both AVG and CG, and group by time effect with significantly higher scores by AVG. |
| Gao et al., 2019 [48] | n = 32 male (16) female (16) | 4.72 ± 0.73 years | RCT | Home-based AVG (LeapTV gaming console) (n = 18) | No intervention (n = 14) | Period: 12 weeks Frequency: 5 days per week Duration: 30 min per session | BMI CRF (3-Minute Step Test) | No effects for BMI and CRF |
| Coknaz et al., 2019 [49] | n = 106 male (46) female (60) | AVG group: 9.62 ± 1.02 years Control group: 10.31 ± 1.15 years | RCT | Nintendo Wii (n = 53) | No intervention | Period: 12 weeks Frequency: 3 days per week Duration: 50–60 min per session | BMI | AVG decreased BMI while CG increased |
| Gao et al., 2019 [61] | n = 56 male (23) female (33) | 4.5 ± 0.46 years | Non-RCT | Nintendo Wii and Xbox Kinect (n = 20) | No intervention (n = 36) | Period: 8 weeks Frequency: 5 days per week Duration: 20 min per session | MC (TGMD-2) | No group effect, but time effect for MC |
| Ye et al., 2019 [50] | n = 81 male (42) female (39) | 9.23 ± 0.62 years | RCT | AVG during recess (Nintendo Wii and Xbox Kinect) (n = 36) | No intervention (n = 45) | Period: School year Frequency: 5 days per week during recess Duration: 50 min per session | CRF (Half-mile run test) | No effects for CRF |
| Fu et al., 2018 [36] | n = 65 male and female | 11.6 ± 0.5 years | Non-RCT | AVG (GoNoodle, Adventure to Fitness, and Cosmic Kids Yoga) in regular school class time (n = 33) | Five 30-min of free-play sessions (n = 32) | Period: 18 weeks Frequency: 3 days per week Duration: 30 min per session | CRF (20-m PACER) | AVG showed a higher CRF than CG |
| Fu et al., 2018 [37] | n = 65 male (34) female (31) | 4.9 ± 0.7 years | RCT | AVG (GoNoodles, Adventure to Fitness, and Cosmic Kids Yoga) in regular school class time (n = 36) | Five 30-min of free-play sessions (n = 29) | Period: 12 weeks Frequency: 5 days per week Duration: 30 min per session | MC (TGMD-3) | AVG showed higher increase in TGMD-3 score than CG |
| Ye et al., 2018 [38] | n = 250 male and female | 8.27 ± 0.70 years | Non-RCT | 125 min of AVG (Nintendo Wii and Xbox Kinect) + PE (n = 135) | 125 min of PE only (5 classes per week) (n = 115) | Period: 9 month Frequency: 3 PE classes and 2 exergaming sessions per week Duration: 125 min | BMI HRF (FITNESSGRAM protocols for PACER) MF (hand-grip dynamometry, push-ups and curl-ups) MC (speed for kicking and throwing, maximum standing long jump distance and hopping) | AVG improved BMI, CRF, MF and OCS, while CG improved CRF and object control skills but worsened MF and BMI. |
| Lau et al., 2016 [51] | n = 80 male (25) female (55) | 9.23 ± 0.52 years | RCT | Xbox Kinect (n = 40) | No intervention (n = 40) | Period: 12 weeks Frequency: twice a week after school Duration: 60 min per day | BMI CRF (20-m shuttle run test) | BMI increased in AVG and CRF increased in AVG and CG, with higher improvements in AVG |
| Vernadakis et al., 2015 [52] | n = 66 males and females | 6.35 ± 0.73 years | RCT | Xbox Kinect (n = 22) | EXE: traditional motor competence training program (n = 22) and no intervention (n = 22) | Period: 8 weeks Frequency and duration: Non-reported | MSC (OCS with TGMD-2) | AVG and EXE showed improvements in OCS. CG2 showed no improvements |
| Johnson et al., 2015 [59] | n = 36 male (53%) female (47%) | 6–10 years | RCT | Xbox Kinect (n = 19; 7.9 ± 1.5 years) | No intervention (n = 17; 8.0 ± 1.2 years) | Period: 6 weeks Frequency: 5 days per week Duration: 50 min in lunchtime | MSC (OCS with TGMD-3) | No effects on OCS or differences between groups for AVG |
| Azevedo et al., 2014 [35] | n = 497 male and female | 11–13 years old | Non-RCT | Dance Mat Exergaming (n = 280; 11.2 ± 0.4 year; 63.9% female) | No intervention (n = 217, 11.3 ± 0.4 years; 64.5% female) | Period: 12 months Frequency: 2 h per week | BMI %BF (DXA) CRF (20-m shuttle run test) | AVG showed a positive effect on weight, BMI and %BF compared to CG, but not on CRF |
| Mombarg et al., 2013 [54] | n = 29 male (23) female (6) | 7–12 years | RCT | Nintendo Wii (Wii-balance board with the Wii-fit-plus) (n = 15) | No intervention (n = 14) | Period: 6 weeks Frequency: 3 days per week Duration: 30 min per session | MC (movement assessment battery for children and Bruininks–Oseretsky Test) | Both AVG and CG showed improvements in MC. Balance scores of the AVG improved significantly, whereas those of the control group showed no significant progress. There were significant interaction effects on balance scores, favoring the AVG. |
| Sheehan et al., 2013 [55] | n = 61 male (33) female (28) | 9–10 years | RCT | iDanceTM, XR BoardTM /LightspaceTM, and Wii FitTM Plus. (n = 21) | CG1: PE curriculum class (n = 21) CG2: PE geared toward agility, balance, and coordination (ABC) improvement (n = 19) | Period: 6 weeks Frequency: 4–5 days per week Duration: 34 min per session | MC (balance test with the HUR BT4TM platform) | AVG and the ABC PE (CG2) improved their postural stability significantly compared to those in the curricular PE class. |
| Sheehan et al., 2012 [56] | n = 65 male (29) female (36) | 9–10 years | RCT | Wii Fit+™ (n = 22) | CG1: PE curriculum class (n = 21) CG2: PE geared toward agility, balance, and coordination (ABC) improvement (n = 22) | Period: 6 weeks Frequency: 3 days per week Duration: 34 min per session | MC (balance test with the HUR BT4TM platform) | AVG and the ABC PE (CG2) improved the balance compared to those in the curricular PE class. Improvement were not significantly different from CG2. |
| Maloney et al., 2012 [57] | n = 58 male (71%) female (29%) | 13.7 ± 0.6 years | RCT | Playstation 2 (In the Groove) (n = 29) | No intervention (n = 29) | Period: 10 and 20 weeks Frequency: 4–5 school days per week Duration: 10 min per session | BMI | AVG decreased BMI more than CG |
| Graves et al., 2010 [58] | n = 58 male (39) female (19) | 9.2 ± 0.5 years | RCT | Nintendo Wii jOG (n = 29) | No intervention (n = 29) | Period: 6 and 12 weeks Frequency and duration: Non-reported home-based | BMI FM (DXA) | No effects for BF or BMI |
| Maloney et al., 2008 [59] | n = 60 male (30) female (30) | 7.5 ± 0.5 years | RCT | DDR (n = 40) | No intervention (n = 20) | Period: 28 weeks Home-based | BMI | No changes in BMI |
| Variable | N | Hedges’g Effect Size | 95 % CI | p Value | I² |
|---|---|---|---|---|---|
| BMI | 7 | −0.291 | −0.631; 0.049 | 0.000 | 78.47% |
| CRF | 4 | 0.438 | 0.022; 0.855 | 0.001 | 82.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comeras-Chueca, C.; Marin-Puyalto, J.; Matute-Llorente, A.; Vicente-Rodriguez, G.; Casajus, J.A.; Gonzalez-Aguero, A. The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6965. https://doi.org/10.3390/ijerph18136965
Comeras-Chueca C, Marin-Puyalto J, Matute-Llorente A, Vicente-Rodriguez G, Casajus JA, Gonzalez-Aguero A. The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(13):6965. https://doi.org/10.3390/ijerph18136965
Chicago/Turabian StyleComeras-Chueca, Cristina, Jorge Marin-Puyalto, Angel Matute-Llorente, German Vicente-Rodriguez, Jose A. Casajus, and Alex Gonzalez-Aguero. 2021. "The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 13: 6965. https://doi.org/10.3390/ijerph18136965
APA StyleComeras-Chueca, C., Marin-Puyalto, J., Matute-Llorente, A., Vicente-Rodriguez, G., Casajus, J. A., & Gonzalez-Aguero, A. (2021). The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(13), 6965. https://doi.org/10.3390/ijerph18136965







