Urban and Rural Disparities in a WeChat-Based Smoking Cessation Intervention among Chinese Smokers
Abstract
:1. Introduction
2. Methods
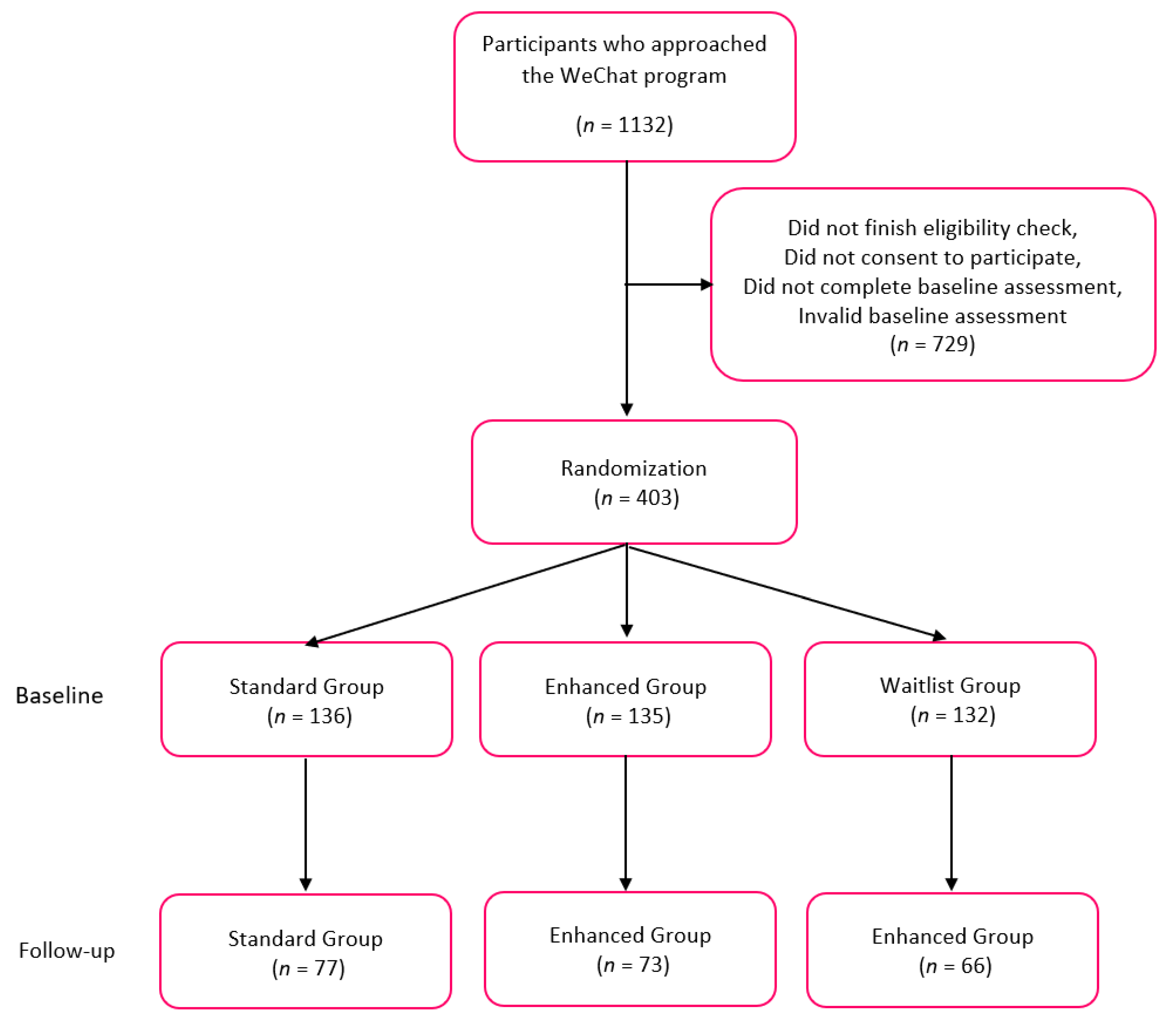
2.1. Program and Participants Description
2.2. Measures
2.2.1. Baseline and Follow-Up Questionnaires
2.2.2. Living Areas and Demographic Measures
2.2.3. Smoking Cessation Measures
2.3. Analysis
3. Results
3.1. Demographic Information and Smoking Behavior at Baseline by Living Area
3.2. The Comparison of Change in Smoking Behaviors between Baseline and Follow-Up for Urban, Suburban, and Rural Participants
3.3. Associations between Smoking Cessation Outcomes and Living Areas
3.4. Stage of Change
3.5. 24-h PPA
3.6. Moderating Analysis
3.7. Stage of Change
3.8. 24-h PPA
4. Discussion
4.1. Urban and Rural Disparities
4.2. Using WeChat to Mitigate the Difference between Urban and Rural
4.3. Using WeChat to Aid Smoking Cessation
4.4. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Launches New Report on Global Tobacco Use Trends. Available online: https://www.who.int/news/item/19-12-2019-who-launches-new-report-on-global-tobacco-use-trends (accessed on 25 May 2021).
- WHO. Tobacco. 2018. Available online: http://www.who.int/news-room/fact-sheets/detail/tobacco (accessed on 19 March 2019).
- American Cancer Society. Consumption, the Tobacco Atlas. 2017. Available online: http://tobaccoatlas.org/topic/consumption/ (accessed on 20 June 2020).
- WHO. Global Adult Tobacco Survey; Fact Sheet: China, 2018; Available online: https://www.who.int/docs/default-source/wpro---documents/countries/china/2018-gats-china-factsheet-cn-en.pdf?sfvrsn=3f4e2da9_2 (accessed on 20 June 2020).
- Zhao, J.; Li, X.; Stewart, S.L.; Gao, W.; Qi, F.; Zhang, L.; Pang, Z.; Qiao, Q.; Ning, F.; Tong, E. Cigarette smoking and secondhand smoke exposure before and after a tobacco-free Olympic policy period: Qingdao, China. Nicotine Tob. Res. 2019, 21, 1531–1538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.-H.; Ang, T.F.A.; Lin, H.-C.; Chang, Y.-C. Rural-urban disparities in smoking patterns among Chinese adults: A social-ecological approach. J. Ethn. Subst. Abus. 2019, 20, 241–256. [Google Scholar] [CrossRef] [PubMed]
- Mao, A.; Yang, T.; Bottorff, J.L.; Sarbit, G. Personal and social determinants sustaining smoking practices in rural China: A qualitative study. Int. J. Equity Health 2014, 13, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, G.; Jason, H.; Yang, Y. Global Adult Tobacco Survey (GATS) China 2010 Country Report in English; China Three Gorges Publisher House: Beijing, China, 2011. [Google Scholar]
- Chen, Z.M.; Liu, B.Q.; Boreham, J.; Wu, Y.P.; Chen, J.S.; Peto, R. Smoking and liver cancer in China: Case-control comparison of 36,000 liver cancer deaths vs. 17,000 cirrhosis deaths. Int. J. Cancer 2003, 107, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Peto, R.; Zhou, M.; Iona, A.; Smith, M.; Yang, L.; Guo, Y.; Chen, Y.; Bian, Z.; Lancaster, G. Contrasting male and female trends in tobacco-attributed mortality in China: Evidence from successive nationwide prospective cohort studies. Lancet 2015, 386, 1447–1456. [Google Scholar] [CrossRef] [Green Version]
- Buisness of Apps. We Chat Revenue and Usage Statistics. 2020. Available online: https://www.businessofapps.com/data/wechat-statistics/ (accessed on 22 October 2020).
- Techjury. 21+ Exciting We Chat Statistics. 2021. Available online: https://techjury.net/blog/wechat-statistics/#gref (accessed on 24 May 2021).
- Firms, We Chat Statistics. 2020. Available online: https://99firms.com/blog/wechat-statistics/#gref (accessed on 18 May 2020).
- CNNIC. Statistics: China Internet Users. China Internet Watch. 2020. Available online: https://www.cnnic.com.cn/IDR/ReportDownloads/201911/P020191112539794960687.pdf (accessed on 19 November 2020).
- Wu, Q.; Huang, Y.; van Velthoven, M.H.; Wang, W.; Chang, S.; Zhang, Y. Feasibility of using WeChat to improve infant and young child feeding in rural areas in China: A mixed quantitative and qualitative study. PLoS ONE 2021, 16, e0246942. [Google Scholar]
- Hu, D.Y.; Hong, X.; Li, X. Oral health in China–trends and challenges. Int. J. Oral Sci. 2011, 3, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dawson, G.M.; Noller, J.M.; Skinner, J.C. Models of smoking cessation brief interventions in oral health. Public Health Bull 2013, 24, 131–134. [Google Scholar] [CrossRef]
- CDC. National Health Intervview Suevey-Smoking Status Recodes. Available online: https://www.cdc.gov/nchs/nhis/tobacco/tobacco_recodes.htm (accessed on 24 May 2021).
- Glanz, K. Health Behavior: Theory, Research, and Practice; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Kuo, W. China Market Research Tool. 2018. Available online: https://medium.com/@williamkuo1988/china-market-research-tool-e612d559b649 (accessed on 29 January 2019).
- Prochaska, J.O.; Velicer, W.F.; Di Clemente, C.C.; Fava, J. Measuring processes of change: Applications to the cessation of smoking. J. Consult. Clin. Psychol. 1988, 56, 520. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.A.; Velicer, W.F.; Fava, J.L. Latent transition analysis to the stages of change for smoking cessation. Addict. Behav. 1996, 21, 67–80. [Google Scholar] [CrossRef]
- Carlson, L.E.; Lounsberry, J.J.; Maciejewski, O.; Wright, K.; Collacutt, V.; Taenzer, P. Telehealth-delivered group smoking cessation for rural and urban participants: Feasibility and cessation rates. Addict. Behav. 2012, 37, 108–114. [Google Scholar] [CrossRef] [PubMed]
- CDC. Tobacco Use by Geographic Region. 2018. Available online: https://www.cdc.gov/tobacco/disparities/geographic/index.htm (accessed on 20 June 2020).
- Northridge, M.E.; Vallone, D.; Xiao, H.; Green, M.; Blackwood, J.W.; Kemper, S.E.; Duke, J.; Watson, K.A.; Burrus, B.; Treadwell, H.M. The importance of location for tobacco cessation: Rural–urban disparities in quit success in underserved West Virginia counties. J. Rural Health 2008, 24, 106–115. [Google Scholar] [CrossRef] [PubMed]
- WHO. Report of China City Adult Tobacco Survey 2013–2014: A 14-City Experience. 2015. Available online: http://www.wpro.who.int/china/tobacco_report_20150819_en.pdf (accessed on 20 June 2020).
- Stancheva, T. 21 Mind-Blowing WeChat Statistics in 2021. Available online: https://review42.com/resources/wechat-statistics/ (accessed on 20 June 2020).
- Chen, X.; Zhao, D.; Wen, T.; Xiao, X.; Pan, Z.; He, J.; Zheng, P.; Hao, W.; Lin, H.; Abdullah, A.S. To text or not to text? Acceptability of WeChat and text messaging intervention to promote tobacco control assistance among parents who smoke in rural China. Tob. Induc. Dis. 2019, 17, 88. [Google Scholar] [CrossRef] [PubMed]
- Walk the Chat. We Chat Official Account: A Simple Guide. Available online: https://walkthechat.com/wechat-official-account-simple-guide/ (accessed on 10 June 2021).
- Lancaster, T.; Stead, L.F. Individual behavioural counselling for smoking cessation. Cochrane Database Syst. Rev. 2017, 3, 1333. [Google Scholar] [CrossRef] [PubMed]
- Stead, L.F.; Hartmann-Boyce, J.; Perera, R.; Lancaster, T. Telephone counselling for smoking cessation. Cochrane Database Syst. Rev. 2013, 8, 35. [Google Scholar] [CrossRef] [PubMed]
| Variables | Urban (n = 124) | Suburban (n = 58) | Rural (n = 34) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Group | 0.36 | |||||||
| Standard group | 46 | 37.1 | 23 | 39.7 | 8 | 23.5 | ||
| Enhanced group | 42 | 33.9 | 20 | 34.5 | 11 | 32.4 | ||
| Waitlist group | 36 | 29.0 | 15 | 25.9 | 15 | 44.1 | ||
| Demographic Information | ||||||||
| Age (Mean, SD) | 30.3 | 9.3 | 27.8 | 6.5 | 28.1 | 8.5 | 0.14 | |
| Age Category | 0.13 | |||||||
| 18–24 | 37 | 30.1 | 21 | 36.8 | 15 | 45.5 | ||
| 25–29 | 37 | 30.1 | 14 | 24.6 | 7 | 21.2 | ||
| 30–39 | 27 | 22.0 | 19 | 33.3 | 8 | 24.2 | ||
| ≥40 | 22 | 17.9 | 3 | 5.3 | 3 | 9.1 | ||
| Sex | 0.16 | |||||||
| Male | 112 | 90.3 | 54 | 93.1 | 34 | 100.0 | ||
| Female | 12 | 9.7 | 4 | 6.9 | 0 | 0.0 | ||
| Household Income 1 in RMB | 0.21 | |||||||
| ≤49,999 | 37 | 29.8 | 21 | 36.1 | 13 | 38.2 | ||
| 50,000–99,999 | 33 | 26.6 | 20 | 34.5 | 14 | 41.2 | ||
| 100,000–199,999 | 38 | 30.7 | 10 | 17.2 | 5 | 14.7 | ||
| ≥200,000 | 16 | 12.9 | 7 | 12.2 | 2 | 5.9 | ||
| Hukou Type 2 (Household Registration) | <0.01 | |||||||
| Non-agricultural register 3 | 99 | 79.8 | 23 | 40.0 | 4 | 11.8 | ||
| Agricultural register3 | 25 | 20.2 | 35 | 60.3 | 30 | 88.2 | ||
| Education Level | <0.01 | |||||||
| High school or less | 33 | 26.1 | 23 | 39.7 | 21 | 61.8 | ||
| Associate college | 46 | 37.1 | 22 | 37.9 | 9 | 26.5 | ||
| College and above | 45 | 36.3 | 13 | 22.4 | 4 | 11.8 | ||
| Marital Status | 0.92 | |||||||
| Married | 73 | 58.9 | 35 | 60.3 | 19 | 55.9 | ||
| Single 4 | 51 | 41.1 | 23 | 39.7 | 15 | 44.1 | ||
| Occupation | 0.02 | |||||||
| Business 5 | 68 | 54.8 | 21 | 36.2 | 11 | 32.4 | ||
| Government/agency officers/professional staff 6 | 25 | 20.2 | 11 | 19.0 | 4 | 11.8 | ||
| Labor Workers 7 | 11 | 8.9 | 10 | 17.2 | 7 | 20.6 | ||
| Self-employed and other 8 | 20 | 16.1 | 16 | 27.6 | 12 | 35.3 | ||
| BMI 9 | <0.01 | |||||||
| Underweight and normal weight | 70 | 56.9 | 46 | 79.3 | 14 | 41.2 | ||
| Overweight and obese | 53 | 43.1 | 12 | 20.7 | 20 | 58.8 | ||
| Smoking Behavior | ||||||||
| Age at Smoking Initiation (mean, SD) | 17.8 | 3.8 | 18.7 | 4.3 | 18.1 | 3.9 | 0.35 | |
| Duration of Smoking Habit (mean, SD) | 12.6 | 9.0 | 9.1 | 6.0 | 10.1 | 7.2 | 0.02 | |
| Stage of Change | 0.03 | |||||||
| Pre-contemplation | 8 | 6.5 | 2 | 3.5 | 5 | 14.7 | ||
| Contemplation | 67 | 54.0 | 22 | 37.9 | 12 | 35.3 | ||
| Preparation | 49 | 39.5 | 34 | 58.6 | 17 | 50.0 | ||
| Smoked in the Past 24 Hours | 0.38 | |||||||
| Yes | 116 | 94.0 | 54 | 93.1 | 34 | 100 | ||
| No | 8 | 6.5 | 4 | 6.9 | 0 | 0 | ||
| Smoked in the Past 7 Days | ||||||||
| Yes | 124 | 100 | 58 | 100 | 34 | 100 | ||
| No | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Attempts to Quit | 1.00 | |||||||
| Yes | 116 | 93.6 | 55 | 94.8 | 32 | 94.1 | ||
| No | 8 | 6.5 | 3 | 5.2 | 2 | 5.9 | ||
| Daily Cigarettes Use | 0.44 | |||||||
| 10 or fewer | 57 | 46.0 | 25 | 43.1 | 13 | 38.2 | ||
| 11–20 | 56 | 45.2 | 25 | 43.1 | 15 | 44.1 | ||
| 21–30 | 7 | 5.7 | 6 | 10.3 | 6 | 17.7 | ||
| 31 or more | 4 | 3.2 | 2 | 3.4 | 0 | 0.0 | ||
| Nicotine Dependence (Mean, SD) | 4.9 | 2.4 | 5.4 | 2.5 | 5.5 | 2.3 | 0.36 | |
| Variables | Urban (n = 124) | Suburban (n = 58) | Rural (n = 34) | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Stage of Change (Overall p = 0.02, χ2 = 12.17) | |||||||
| Progressed | 37 | 29.8 | 13 | 22.4 | 15 | 44.1 | |
| Regressed | 17 | 13.7 | 16 | 27.6 | 9 | 26.5 | |
| No change | 70 | 56.5 | 29 | 50.0 | 10 | 29.4 | |
| Change in 24-h PPA Rates (Overall p = 0.12, χ2 = 10.45, Table (p) using Fisher’s Exact Test < 0.0001) | |||||||
| Progressed | 33 | 26.6 | 16 | 27.6 | 18 | 52.9 | |
| Regressed | 3 | 2.4 | 2 | 3.5 | 0 | 0 | |
| No change (smoking) | 83 | 66.9 | 38 | 65.5 | 16 | 47.1 | |
| No change (non-smoking) | 5 | 4.0 | 2 | 3.45 | 0 | 0 | |
| Variables | Crude Model | Adjusted Model | |||||
|---|---|---|---|---|---|---|---|
| Beta | 95% CI | p-Value | Beta | 95% CI | p-Value | ||
| Group | |||||||
| Group 1 (standard group) | 0.24 | (−0.02, 0.50) | 0.07 | 0.23 | (−0.03, 0.50) | 0.09 | |
| Group 2 (enhanced group) | 0.39 | (0.13, 0.65) | <0.01 | 0.40 | (0.13, 0.67) | 0.004 | |
| Group 3 (waitlist group) | Ref | Ref | Ref | Ref | |||
| Age | |||||||
| 18–29 | Ref | Ref | Ref | Ref | |||
| ≥30 | −0.21 | (−0.43, −0.02) | 0.06 | −0.21 | (−0.43, 0.01) | 0.07 | |
| Gender | |||||||
| Male | 0.33 | (−0.07, 0.73) | 0.11 | 0.33 | (−0.07, 0.73) | 0.10 | |
| Female | Ref | Ref | Ref | Ref | |||
| Household Income | |||||||
| ≤99,999 | Ref | Ref | Ref | Ref | |||
| ≥100,000 | 0.14 | (−0.08, 0.37) | 0.20 | 0.18 | (−0.07, 0.42) | 0.15 | |
| Education Level | |||||||
| High school or less | Ref | Ref | Ref | Ref | |||
| Associate college and above | 0.11 | (−0.27, 0.18) | 0.68 | −0.04 | (−0.29, 0.20) | 0.72 | |
| Self-Reported Living Area | |||||||
| Urban | Ref | Ref | Ref | Ref | |||
| Suburban | 0.02 | (−0.23, 0.27) | 0.89 | 0.02 | (−0.23, 0.27) | 0.88 | |
| Rural | 0.32 | (0.02, 0.62) | 0.04 | 0.35 | (0.04, 0.67) | 0.02 | |
| Hukou Type (Household Registration) | |||||||
| Non-agricultural register | Ref | Ref | - | - | - | ||
| Agricultural register | 0.17 | (−0.04, 0.39) | 0.11 | - | - | - | |
| Marital Status | |||||||
| Married | Ref | Ref | - | - | - | ||
| Single and other | 0.10 | (−0.12, 0.31) | 0.39 | - | - | - | |
| Occupation | 0.93 | ||||||
| Business | Ref | Ref | - | - | - | ||
| Government/agency officers/professional staff | −0.10 | (−0.39, 0.20) | 0.51 | - | - | - | |
| Labor workers | −0.04 | (−0.38, 0.29) | 0.80 | - | - | - | |
| Self-employed and other | 0.03 | (−0.31, 0.25) | 0.82 | - | - | - | |
| BMI | |||||||
| Underweight or normal weight | Ref | Ref | - | - | - | ||
| Overweight and obese | −0.07 | (−0.29, 0.15) | 0.51 | - | - | - | |
| Age of Smoking Initiation | −0.02 | (−0.05, 0.00) | 0.06 | - | - | - | |
| Nicotine Dependence Score | −0.02 | (−0.07, 0.02) | 0.33 | - | - | - | |
| Baseline Stage | 0.25 | (0.08, 0.42) | 0.004 | ||||
| Variables | Crude Model | Adjusted Model | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||
| Group | |||||||
| Group 1 (standard group) | 1.45 | (0.68, 3.08) | 0.34 | 1.64 | (0.73, 3.67) | 0.95 | |
| Group 2 (enhanced group) | 2.24 | (1.07, 4.71) | 0.03 | 2.57 | (1.15, 5.76) | 0.03 | |
| Group 3 (waitlist group) | Ref | Ref | Ref | Ref | |||
| Age | |||||||
| 18–29 | Ref | Ref | Ref | Ref | |||
| ≥30 | 0.63 | (0.35, 1.17) | 0.22 | 0.67 | (0.35, 1.28) | 0.22 | |
| Gender | |||||||
| Male | 2.04 | (0.56, 7.41) | 0.28 | 2.00 | (0.53, 7.57) | 0.31 | |
| Female | Ref | Ref | Ref | Ref | |||
| Household Income | |||||||
| ≤99,999 | Ref | Ref | Ref | Ref | |||
| ≥100,000 | 0.98 | (0.54, 1.79) | 0.95 | 1.18 | (0.58, 2.41) | 0.64 | |
| Education Level | |||||||
| High school or less | Ref | Ref | Ref | Ref | |||
| Associate college or above | 0.69 | (0.38, 1.26) | 0.23 | 0.81 | (0.40, 1.63) | 0.55 | |
| Self-reported Living Area | |||||||
| Urban | Ref | Ref | Ref | Ref | |||
| Suburban | 1.05 | (0.52, 2.11) | 0.89 | 1.03 | (0.49, 2.13) | 0.13 | |
| Rural | 3.10 | (1.42, 6.78) | <0.01 | 3.23 | (1.36, 7.68) | 0.006 | |
| Hukou Type (Household Registration) | |||||||
| Non-agricultural register | Ref | Ref | - | - | - | ||
| Agricultural register | 2.04 | (1.14, 3.67) | 0.02 | - | - | - | |
| Marital Status | |||||||
| Married | Ref | Ref | - | - | - | ||
| Single and other | 1.92 | (1.07, 3.45) | 0.03 | - | - | - | |
| Occupation | |||||||
| Business | Ref | Ref | - | - | - | ||
| Government/agency officers/professional staff | 0.95 | (0.43, 2.12) | 0.91 | - | - | - | |
| Labor workers | 0.89 | (0.35, 2.24) | 0.81 | - | - | - | |
| Self-employed and other | 1.11 | (0.53, 2.32) | 0.78 | - | - | - | |
| BMI | |||||||
| Underweight and normal weight | Ref | Ref | - | - | - | ||
| Overweight and obese | 0.87 | (0.48, 1.58) | 0.65 | - | - | - | |
| Age of Smoking Initiation | 1.04 | (0.96, 1.12) | 0.33 | - | - | - | |
| Nicotine Dependence Score | 0.95 | (0.85, 1.07) | 0.43 | ||||
| Baseline Stage | 1.10 | (0.69, 1.76) | 0.70 | ||||
| Variables | Adjusted Model 1 | |||
|---|---|---|---|---|
| Beta | 95% CI | p-Value | ||
| Stage of Change at Follow-up Crude Model: Living Area * Group (p = 0.48) 2 Adjusted Model: Living Area * Group (p = 0.47) | ||||
| Stage of Change at Follow-up for Urban Participants | ||||
| Standard group | 0.33 | (0.00, 0.66) | 0.05 | |
| Enhanced group | 0.66 | (0.32, 1.00) | <0.001 | |
| Waitlist group | Ref | Ref | ||
| Stage of Change at Follow-up for Suburban Participants | ||||
| Standard group | −0.04 | (−0.58, 0.50) | 0.88 | |
| Enhanced group | 0.20 | (−0.54, 0.58) | 0.94 | |
| Waitlist group | Ref | Ref | ||
| Stage of Change at Follow-up for Rural Participants | ||||
| Standard group | 0.24 | (−0.62, 1.10) | 0.57 | |
| Enhanced group | 0.11 | (−0.73, 0.96) | 0.79 | |
| Waitlist group | Ref | Ref | ||
| Change in 24-h PPA Rate Crude Model: Living Area * Group (p = 0.39) 2 Adjusted Model: Living Area * Group (p = 0.31) | ||||
| OR | 95% CI | p-value | ||
| Change in 24-h PPA Rate for Urban Participants | ||||
| Standard group | 1.56 | (0.46, 5.23) | 0.56 | |
| Enhanced group | 4.19 | (1.27, 13.78) | 0.009 | |
| Waitlist group | Ref | Ref | ||
| Change in 24-h PPA Rate for Suburban Participants ¤ | ||||
| Standard group | 1.42 | (0.28, 7.23) | 0.89 | |
| Enhanced group | 1.70 | (0.33, 8.67) | 0.59 | |
| Waitlist group | Ref | Ref | ||
| Change in 24-h PPA Rate for Rural Participants ¤ | ||||
| Standard group | 3.37 | (0.46, 24.43) | 0.15 | |
| Enhanced group | 0.68 | (0.12, 3.97) | 0.27 | |
| Waitlist group | Ref | Ref | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, T.; Li, M.; Williams, D.; Fritz, J.; Phillippi, S.; Yu, Q.; Kantrow, S.; Chen, L.; Chen, Y.; Beiter, K.; et al. Urban and Rural Disparities in a WeChat-Based Smoking Cessation Intervention among Chinese Smokers. Int. J. Environ. Res. Public Health 2021, 18, 6731. https://doi.org/10.3390/ijerph18136731
Luo T, Li M, Williams D, Fritz J, Phillippi S, Yu Q, Kantrow S, Chen L, Chen Y, Beiter K, et al. Urban and Rural Disparities in a WeChat-Based Smoking Cessation Intervention among Chinese Smokers. International Journal of Environmental Research and Public Health. 2021; 18(13):6731. https://doi.org/10.3390/ijerph18136731
Chicago/Turabian StyleLuo, Ting, Mirandy Li, Donna Williams, Jackson Fritz, Stephen Phillippi, Qingzhao Yu, Stephen Kantrow, Liwei Chen, Yongchun Chen, Kaylin Beiter, and et al. 2021. "Urban and Rural Disparities in a WeChat-Based Smoking Cessation Intervention among Chinese Smokers" International Journal of Environmental Research and Public Health 18, no. 13: 6731. https://doi.org/10.3390/ijerph18136731
APA StyleLuo, T., Li, M., Williams, D., Fritz, J., Phillippi, S., Yu, Q., Kantrow, S., Chen, L., Chen, Y., Beiter, K., & Tseng, T.-S. (2021). Urban and Rural Disparities in a WeChat-Based Smoking Cessation Intervention among Chinese Smokers. International Journal of Environmental Research and Public Health, 18(13), 6731. https://doi.org/10.3390/ijerph18136731






