The Association between a Novel Baby-Friendly Hospital Program and Equitable Support for Breastfeeding in Vietnam
Abstract
:1. Introduction
2. Materials and Methods
2.1. Intervention and Study Sample
2.2. Outcomes
2.3. Exposure and Covariates
2.4. Statistical Analysis
3. Results
3.1. Study Sample
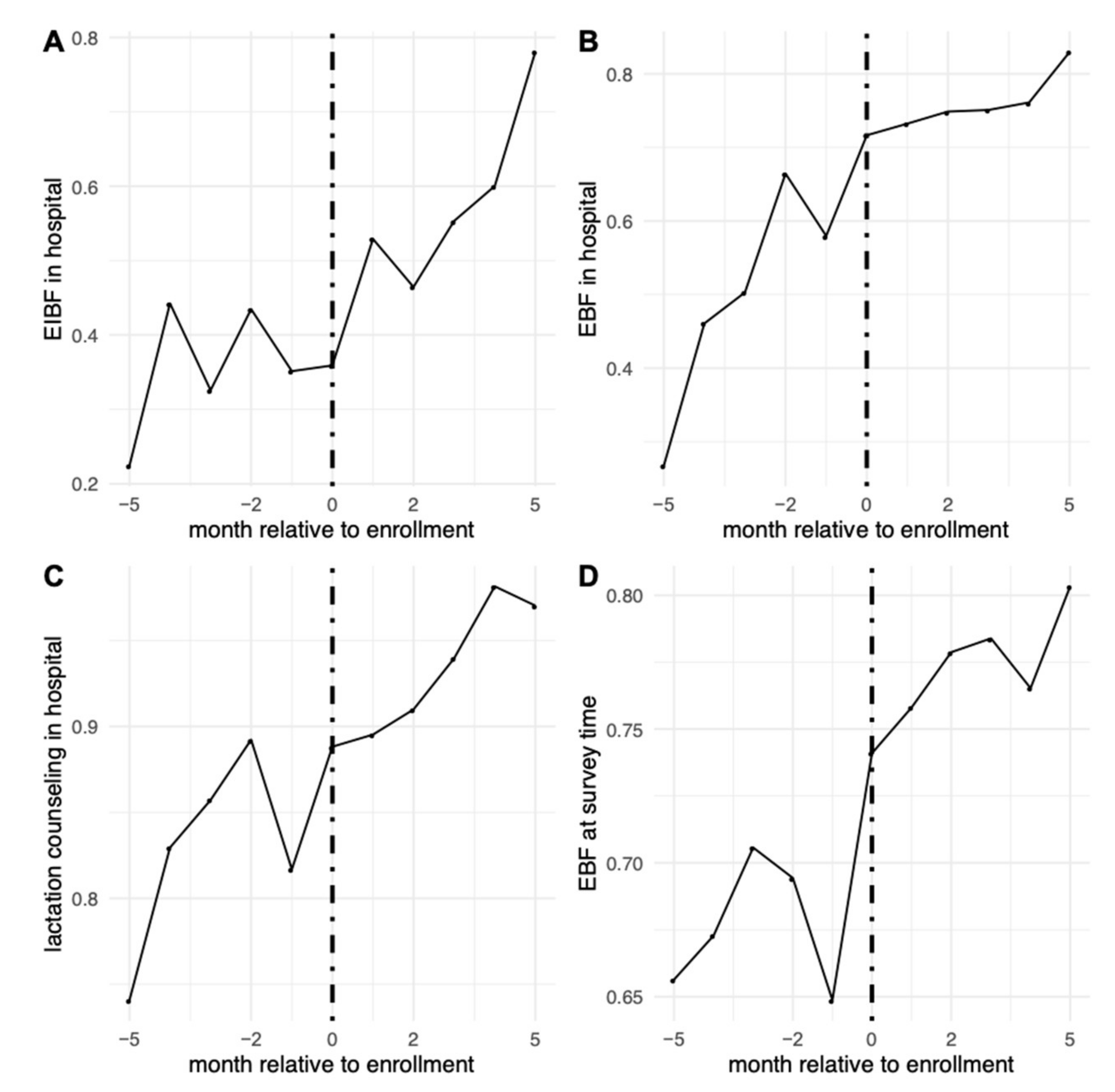
3.2. The Association between Enrollment and Breastfeeding Outcomes
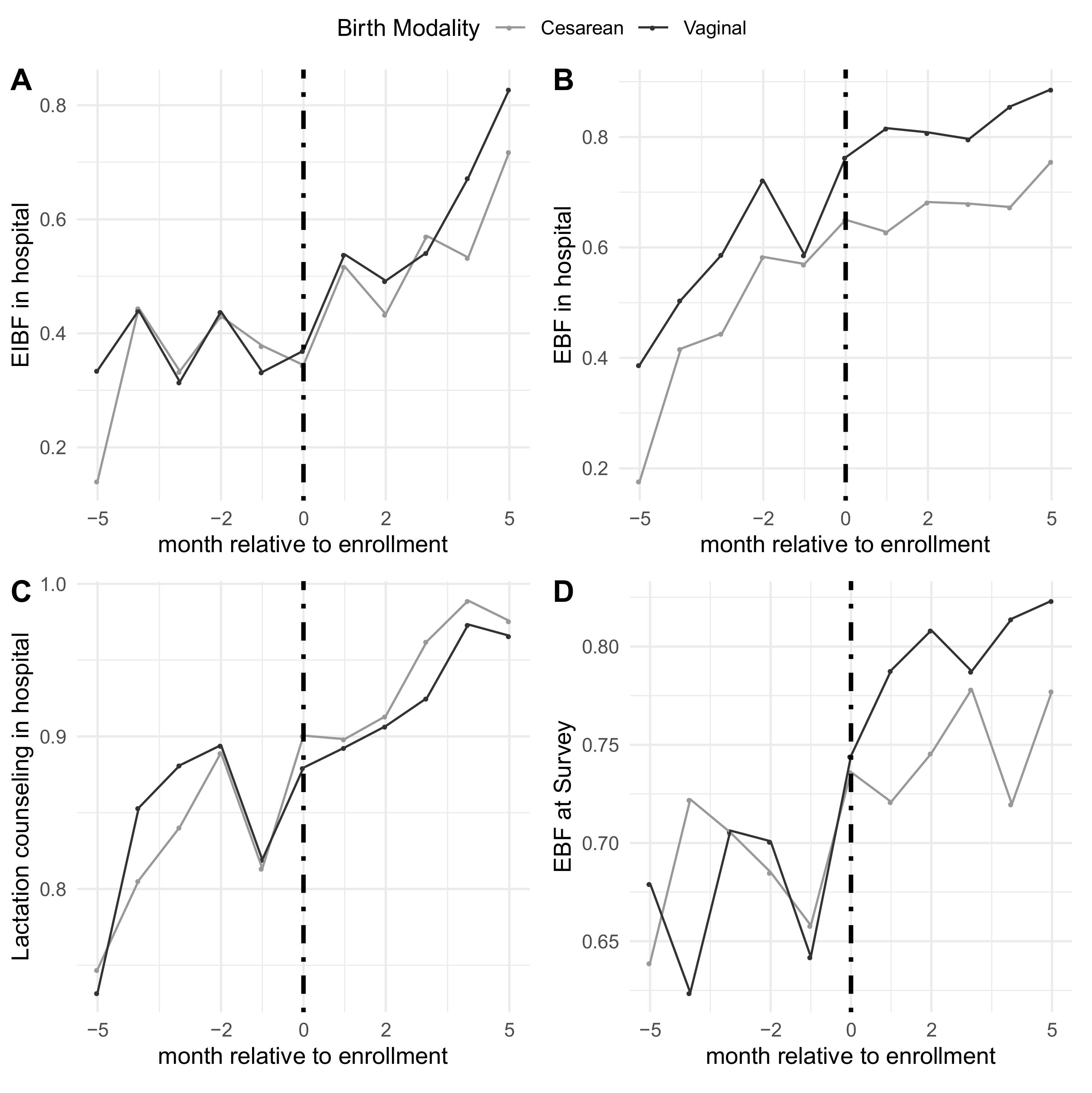
3.3. Variation by Modality of Birth
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Detailed Accreditation Process
Appendix B. Enrollment Date and Number of Births Sampled Per Hospital
| Hospital | n (Births) | % (Total Births in Sample) | Hospital Enrollment Date (Day/Month/Year) |
| Ca Mau Obstetric and Pediatric Hospital | 486 | 5.1% | 2 April 2019 |
| Tran Van Thoi General Hospital | 294 | 3.1% | 1 April 2019 |
| Dam Doi General Hospital | 222 | 2.3% | 3 April 2019 |
| U Minh District Hospital | 248 | 2.6% | 4 April 2019 |
| Cai Nuoc General Hospital | 252 | 2.6% | 5 April 2019 |
| Phu Vang District Hospital | 259 | 2.7% | 24 March 2019 |
| Nam Dong District Hospital | 249 | 2.6% | 25 March 2019 |
| Phong Dien District Hospital | 250 | 2.6% | 26 March 2019 |
| Quang Dien District Hospital | 233 | 2.4% | 27 March 2019 |
| Quang Nam Provincial General Hospital | 580 | 6.1% | 13 April 2019 |
| Dong Giang District Hospital | 235 | 2.5% | 16 March 2019 |
| Que Son District Hospital | 228 | 2.4% | 17 March 2019 |
| Vinh Duc General Hospital | 249 | 2.6% | 16 March 2019 |
| Quang Nam Central General Hospital | 505 | 5.3% | 15 March 2019 |
| Quang Nam Regional General Hospital | 495 | 5.2% | 14 March 2019 |
| Minh Thien General Hospital | 260 | 2.7% | 15 March 2019 |
| Da Nang Hospital for Women and Children | 508 | 5.3% | 7 June 2019 |
| Da Nang Family Hospital | 252 | 2.6% | 16 May 2019 |
| Cam Le District Hospital | 249 | 2.6% | 16 May 2019 |
| Son Tra District Hospital | 252 | 2.6% | 17 May 2019 |
| Hai Chau District Hospital | 243 | 2.5% | 17 May 2019 |
| Central Highland Region General Hospital | 521 | 5.4% | 11 February 2020 |
| Cu Mgar District Hospital | 255 | 2.7% | 10 February 2020 |
| Can Tho Obstetrics and Gynecology Hospital | 503 | 5.2% | 26 July 2019 |
| Phuong Chau International General Hospital | 278 | 2.9% | 25 July 2019 |
| Tu Du Hospital | 502 | 5.2% | 19 July 2019 |
| Hung Vuong Hospital | 507 | 5.3% | 18 July 2019 |
| Quang Ninh Obstetrics and Pediatrics Hospital | 470 | 4.9% | 24 May 2019 |
| TOTAL | 9585 | 100% |
Appendix C. Survey Questionnaire
| No. | Question | Answer |
| 0 | Call response | (1) Mother agreed to continue the call (moved to question 1) (2) Babysitter (father, grandparents) agreed to continue the call (moved to question 1) (3) Mother refuse to continue the call (stop the call) (4) Mother is busy (stop the call) (5) Phone number is wrong or not available (stop the call) (7) Baby died (stop the call) |
| 1 | How old is your youngest child? | (Note the child’s age in months) |
| 1a | Is your child a boy or a girl? | (1) Boy (2) Girl (9) Others (twins, etc.) |
| 2 | Is s/he breastfed? | (1) Yes (move to question 2a) (2) No (move to question 3) |
| 2a | Apart from breastfeeding your child, do you let your child eat or drink anything else? | (1) Exclusive breastmilk (from the biological mother or others) (2) Breastmilk and formula milk (3) Breastmilk and water (9) Breastmilk and other drinks/foods |
| 3 | Did you deliver him/her vaginally or via cesarean? | (1) Vaginally (2) Via cesarean |
| 3a | Is your baby pre-term? | (1) <37 weeks (<259 days) (2) ≥37 weeks (≥259 days) |
| 4 | Was s/he placed on your chest/abdomen for skin-to-skin contact immediately after birth? | (1) Yes (move to question 5a) (2) No (move to question 5b) (8) No answer (9) Don’t know/don’t remember |
| 5a | How long was s/he in skin-to-skin contact with you? | (1) Less than 90 min (2) More than 90 min (9) Don’t know/don’t remember |
| 5b | How long after birth was your child returned to stay with you? | (1) Immediately or less than one hour (2) From one to six hours (3) More than six hours (9) Don’t know/don’t remember |
| 6 | Was your child breastfed within 90 min after birth? | (1) Yes (0) No (8) No answer (9) Don’t know/don’t remember |
| 7 | Was your child given water or formula milk during the hospital stay? | (1) Yes (0) No (8) No answer (9) Don’t know/don’t remember |
| 8 | Did you receive breastfeeding counseling from doctors and nurses during your hospital stay? | (1) Yes (0) No (8) No answer (9) Don’t know/don’t remember |
| 9 | Did doctors and nurses in the hospital counsel you to use formula milk for babies aged under 24 months? | (1) Yes (move to question 9a) (0) No (8) No answer (9) Don’t know/don’t remember |
| 9a | Why were you counseled to use formula milk by doctors/nurses? | (1) Having little breastmilk/no breastmilk (2) Cesarean childbirth (3) The mother is sick, thus not able to breastfeed her baby (4) The baby is sick or born preterm, thus not able to breastfeed (5) The mother wants to feed her baby with formula milk (7) Other (please specify) (8) No answer (9) Don’t know/don’t remember |
| 10 | Did you see any forms of advertising/marketing of formula milk for babies aged under 24 months, feeding bottles and artificial pacifiers in the hospital? | (1) Posters or advertisements of infant formula for babies aged under 24 months (2) Formula company staff marketing formula milk for children under 24 months at the hospital (3) Formula milk products for children under 24 months being displayed for sales or introduced by health staff (4) Persons asking for your phone number and calling you to introduce breastmilk substitutes after birth, feeding bottles, or artificial pacifiers (5) Advertisements of formula milk for pregnant women and postpartum mothers (6) Feeding bottles and artificial pacifiers being advertised and displayed for sale (9) Other types of advertisements/marketing about formula milk for babies aged less than 24 months (describe) (0) No abovementioned forms seen |
| 11 | Did you have a birth companion of choice at the childbirth ward? | (1) Yes (0) No |
| 12 | What is your ethnicity? | (1) Kinh (2) Tay (3) Thai (4) Hoa (5) Khmer … (56) Other (specify in question 12a) |
| 12a | Please specify your ethnicity? | |
| 13 | Do you have any recommendations for the hospital to better support breastfeeding? | (1) Yes (note down the comments) (0) No |
References
- León-Cava, N.; Lutter, C.; Ross, J.; Martin, L. Quantifying the Benefits of Breastfeeding: A Summary of the Evidence; Pan American Health Organization: Washington, DC, USA, 2002. [Google Scholar]
- Wardlaw, T.M.; Johansson, E.W.; Hodge, M.J. Pneumonia: The Forgotten Killer of Children; UNICEF: New York, NY, USA, 2006. [Google Scholar]
- Lamberti, L.M.; Zakarija-Grković, I.; Walker, C.L.; Theodoratou, E.; Nair, H.; Campbell, H.; Black, R.E. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: A systematic literature review and meta-analysis. BMC Public Health 2013, 13, S18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowatte, G.; Tham, R.; Allen, K.J.; Tan, D.J.; Lau, M.X.; Dai, X.; Lodge, C.J. Breastfeeding and childhood acute otitis media: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 85–95. [Google Scholar] [CrossRef] [Green Version]
- Giugliani, E.R.; Horta, B.L.; de Mola, C.L.; Lisboa, B.O.; Victora, C.G. Effect of breastfeeding promotion interventions on child growth: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahl, R.; Barros, A.J.; França, G.V.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C.; et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef] [Green Version]
- Khan, J.; Vesel, L.; Bahl, R.; Martines, J.C. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: Effects on neonatal mortality and morbidity—A systematic review and meta-analysis. Matern. Child Health J. 2015, 19, 468–479. [Google Scholar] [CrossRef]
- Debes, A.K.; Kohli, A.; Walker, N.; Edmond, K.; Mullany, L.C. Time to initiation of breastfeeding and neonatal mortality and morbidity: A systematic review. BMC Public Health 2013, 13, S19. [Google Scholar] [CrossRef] [Green Version]
- NEOVITA Study Group. Timing of initiation, patterns of breastfeeding, and infant survival: Prospective analysis of pooled data from three randomised trials. Lancet. Glob. Health 2016, 4, e266–e275. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, P.H.; Kim, S.S.; Tran, L.M.; Menon, P.; Frongillo, E.A. Early breastfeeding practices contribute to exclusive breastfeeding in Bangladesh, Vietnam and Ethiopia. Matern. Child Nutr. 2020, e13012. [Google Scholar] [CrossRef] [Green Version]
- Smith, E.R.; Hurt, L.; Chowdhury, R.; Sinha, B.; Fawzi, W.; Edmond, K.M.; Group, N.S. Delayed breastfeeding initiation and infant survival: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0180722. [Google Scholar] [CrossRef] [Green Version]
- WHO. Global Strategy for Infant and Young Child Feeding; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- UNICEF. The State of the World’s Children’s 2014 in Numbers: Every Child Counts: Revealing Disparities, Advancing Children’s Rights; UNICEF: New York, NY, USA, 2014. [Google Scholar]
- Walters, D.D.; Phan, L.T.H.; Mathisen, R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan 2019, 34, 407–417. [Google Scholar] [CrossRef] [Green Version]
- Meyers, D. Breastfeeding and Health Outcomes. Breastfeed. Med. 2009, 4, S15. [Google Scholar] [CrossRef]
- Renfrew, M.J.; Dyson, L.; McCormick, F.; Misso, K.; Stenhouse, E.; King, S.; Williams, A. Breastfeeding promotion for infants in neonatal units: A systematic review. Child Care Health Dev. 2010, 36, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Imdad, A.; Yakoob, M.Y.; Bhutta, Z.A. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health 2011, 11, S24. [Google Scholar] [CrossRef] [Green Version]
- Moore, E.R.; Bergman, N.; Anderson, G.C.; Medley, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst. Rev. 2016, 11, Cd003519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Escamilla, R.; Martinez, J.L.; Segura-Pérez, S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: A systematic review. Matern. Child Nutr. 2016, 12, 402–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization; United Nations Children’s Fund (UNICEF). Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services: Implementing the Revised Baby-Friendly Hospital Initiative 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Silva, O.L.O.; Rea, M.F.; Sarti, F.M.; Buccini, G. Cost-effectiveness analysis of Baby-Friendly Hospital Initiative in promotion of breast-feeding and reduction of late neonatal infant mortality in Brazil. Public Health Nutr. 2020, 1–11. [Google Scholar] [CrossRef]
- Fallon, V.M.; Harrold, J.A.; Chisholm, A. The impact of the UK Baby Friendly Initiative on maternal and infant health outcomes: A mixed-methods systematic review. Matern. Child Nutr. 2019, 15, e12778. [Google Scholar] [CrossRef] [Green Version]
- Baerug, A.; Langsrud, Ø.; Løland, B.F.; Tufte, E.; Tylleskar, T.; Fretheim, A. Effectiveness of Baby-friendly community health services on exclusive breastfeeding and maternal satisfaction: A pragmatic trial. Matern. Child Nutr. 2016, 12, 428–439. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. National Implementation of the Baby-Friendly Hospital Initiative; World Health Organization: Geneva, Switzerland, 2017; p. 9241512385. [Google Scholar]
- Nguyen, P.-H.; Menon, P.; Ruel, M.; Hajeebhoy, N. A situational review of infant and young child feeding practices and interventions in Viet Nam. Asia Pac. J. Clin. Nutr. 2011, 20, 359–374. [Google Scholar] [PubMed]
- Pérez-Escamilla, R.; Hall Moran, V. Scaling up breastfeeding programmes in a complex adaptive world. Matern. Child Nutr. 2016, 12, 375–380. [Google Scholar] [CrossRef]
- Bui, Q.T.-T.; Lee, H.-Y.; Le, A.T.-K.; Van Dung, D.; Vu, L.T.-H. Trends and determinants for early initiation of and exclusive breastfeeding under six months in Vietnam: Results from the Multiple Indicator Cluster Surveys, 2000–2011. Glob. Health Action 2016, 9, 29433. [Google Scholar] [CrossRef] [PubMed]
- General Statistics Office and UNICEF. Viet Nam Muliple Indicator Cluster Survey 2014, Final Report; General Statistics Office and UNICEF: Hanoi, Vietnam, 2015. [Google Scholar]
- Abrahams, S.W. Milk and social media: Online communities and the International Code of Marketing of Breast-milk Substitutes. J. Hum. Lact. 2012, 28, 400–406. [Google Scholar] [CrossRef]
- Rollins, N.C.; Bhandari, N.; Hajeebhoy, N.; Horton, S.; Lutter, C.K.; Martines, J.C.; Piwoz, E.G.; Richter, L.M.; Victora, C.G.; Group, T.L.B.S. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016, 387, 491–504. [Google Scholar] [CrossRef]
- Boerma, T.; Ronsmans, C.; Melesse, D.Y.; Barros, A.J.; Barros, F.C.; Juan, L.; Moller, A.-B.; Say, L.; Hosseinpoor, A.R.; Yi, M. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018, 392, 1341–1348. [Google Scholar] [CrossRef]
- Giang, H.T.N.; Ulrich, S.; Tran, H.T.; Bechtold-Dalla Pozza, S. Monitoring and interventions are needed to reduce the very high Caesarean section rates in Vietnam. Acta Paediatr. 2018, 107, 2109–2114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, P.H.; Keithly, S.C.; Nguyen, N.T.; Nguyen, T.T.; Tran, L.M.; Hajeebhoy, N. Prelacteal feeding practices in Vietnam: Challenges and associated factors. BMC Public Health 2013, 13, 932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takahashi, K.; Ganchimeg, T.; Ota, E.; Vogel, J.P.; Souza, J.P.; Laopaiboon, M.; Castro, C.P.; Jayaratne, K.; Ortiz-Panozo, E.; Lumbiganon, P. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: Secondary analysis of the WHO global survey. Sci. Rep. 2017, 7, 44868. [Google Scholar] [CrossRef] [Green Version]
- Le, Q.-N.T.; Phung, K.-L.; Nguyen, V.-T.T.; Anders, K.L.; Nguyen, M.-N.; Hoang, D.-T.T.; Bui, T.-T.T.; Van Nguyen, V.-C.; Thwaites, G.E.; Simmons, C. Factors associated with a low prevalence of exclusive breastfeeding during hospital stay in urban and semi-rural areas of southern Vietnam. Int. Breastfeed. J. 2018, 13, 46. [Google Scholar] [CrossRef]
- Maternal and Child Health Department Vietnam Ministry of Health. Annual Report on Reproductive Healthcare in Viet Nam; Maternal and Child Health Department Vietnam Ministry of Health: Hanoi, Vietnam, 2020. [Google Scholar]
- WHO: Western Pacific Region. Introducing and Sustaining EENC in Hospitals: Routine Childbirth and Newborn Care; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Alive and Thrive. Centers of Excellence for Breastfeeding in Viet Nam: Evaluation Checklists; Alive and Thrive: Hanoi, Vietnam, 2019. [Google Scholar]
- Alive and Thrive. Centers of Excellence for Breastfeeding in Viet Nam: Mother Survey Questionnaire; Alive and Thrive: Hanoi, Vietnam, 2019. [Google Scholar]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- RStudio Team. RStudio: Integrated Development for R; RStudio: Boston, MA, USA, 2020. [Google Scholar]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [Green Version]
- Abdel-Hady, D.M.; El-Gilany, A.H. Calculating Exclusive Breastfeeding Rates: Comparing Dietary "24-Hour Recall" with Recall "Since Birth" Methods. Breastfeed. Med. 2016, 11, 514–518. [Google Scholar] [CrossRef]
- Platt, R.W.; Harper, S.B. Survey data with sampling weights: Is there a "best" approach? Environ. Res. 2013, 120, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Insurance code for health facilities nationwide. Decision 384/QD-BYT Web site. Available online: http://kcb.vn/vanban/quyet-dinh-384-qd-byt-ngay-30-01-2019-ban-hanh-nguyen-tac-cap-ma-co-so-kham-benh-chua-benh/danh-muc-co-so-kham-chua-benh-kem-ma-bhyt-01-02-2019 (accessed on 15 December 2020).
- Acharya, P.; Khanal, V. The effect of mother’s educational status on early initiation of breastfeeding: Further analysis of three consecutive Nepal Demographic and Health Surveys. BMC Public Health 2015, 15, 1069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitano, N.; Nomura, K.; Kido, M.; Murakami, K.; Ohkubo, T.; Ueno, M.; Sugimoto, M. Combined effects of maternal age and parity on successful initiation of exclusive breastfeeding. Prev. Med. Rep. 2015, 3, 121–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Approving the Vietnam’s National Hospital Quality Standards. Decision 6858/QD-BYT Web site. Available online: https://thuvienphapluat.vn/van-ban/the-thao-y-te/Quyet-dinh-6858-QD-BYT-Bo-tieu-chi-chat-luong-benh-vien-Viet-Nam-2016-331011.aspx (accessed on 15 December 2020).
- WHO. EENC Annual Implementation and Review and Planning Guide; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- On approving national technical guidelines on reproductive health services. Decision 4128/QD-BYT Web site. Available online: https://thuvienphapluat.vn/van-ban/the-thao-y-te/quyet-dinh-4128-qd-byt-2016-huong-dan-quoc-gia-ve-cac-dich-vu-cham-soc-suc-khoe-sinh-san-357665.aspx (accessed on 15 December 2020).
- Approving national technical guidelines on Early Essential Newborn Care in vaginal birth. Decision 4673/QD-BYT Web site. Available online: https://thuvienphapluat.vn/van-ban/the-thao-y-te/Quyet-dinh-4673-QD-BYT-2014-tai-lieu-huong-dan-chuyen-mon-Cham-soc-thiet-yeu-ba-me-tre-so-sinh-trong-va-ngay-sau-de-258447.aspx (accessed on 15 December 2020).
- Approving national technical guidelines on Early Essential Newborn Care in cesarean birth. Decision 6734/QD-BYT Web site. Available online: https://thuvienphapluat.vn/van-ban/the-thao-y-te/Quyet-dinh-6734-QD-BYT-tai-lieu-huong-dan-chuyen-mon-cham-soc-thiet-yeu-ba-me-tre-so-sinh-2016-330090.aspx (accessed on 15 December 2020).
- Centers of Excellence for Breastfeeding. Available online: https://www.aliveandthrive.org/how-we-work/centers-of-excellence-for-breastfeeding/ (accessed on 24 October 2020).
| Variables | n | % |
|---|---|---|
| Response * | ||
| Mothers agreed to continue the call | 8501 | 81.2% |
| Father, grandparents, or other caregiver agreed to continue the call | 1084 | 10.4% |
| Mother refused to continue the call (stopped the call) | 33 | 0.3% |
| Mother is busy (stopped the call) | 134 | 1.3% |
| Phone number is wrong or not available (stopped the call) | 703 | 6.7% |
| Infant died (stop the call) | 18 | 0.2% |
| Birth Year and Quarter | ||
| 2019 Q1 | 1599 | 16.7% |
| 2019 Q2 | 2125 | 22.2% |
| 2019 Q3 | 1920 | 20.0% |
| 2019 Q4 | 1951 | 20.4% |
| 2020 Q1 | 1989 | 20.8% |
| Sex | ||
| Male | 3909 | 51.6% |
| Female | 3637 | 48.0% |
| Twins | 31 | 0.4% |
| Childbirth | ||
| Vaginal Birth | 5184 | 54.1% |
| Caesarian Birth | 4401 | 45.9% |
| Term | ||
| Pre-term (<37 weeks) | 197 | 3.9% |
| Full term (≥37 weeks) | 4888 | 96.1% |
| Private vs. Public Hospital | ||
| Private | 1039 | 10.8% |
| Public | 8546 | 89.2% |
| EIBF | EBF During Hospital Stay | Lactation Counseling | EBF at Survey Time | |
|---|---|---|---|---|
| RD | RD | RD | RD | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| Constant | n = 9190 | n = 9584 | n = 9584 | n = 9244 |
| 0.31 | 0.67 | 0.87 | 0.715 | |
| (0.25, 0.38) | (0.60, 0.74) | (0.85, 0.90) | (0.68, 0.75) | |
| Month | 0.001 | 0.03 | 0.008 | 0.01 |
| (−0.01, 0.01) | (0.02, 0.04) | (0.002, 0.01) | (0.003, 0.02) | |
| Enrolled | 0.06 | 0.05 | 0.004 | 0.03 |
| (0.03, 0.09) | (0.02, 0.09) | (−0.02, 0.03) | (−0.004, 0.06) | |
| Month × Enrolled | 0.07 | −0.02 | 0.009 | −0.001 |
| (0.06, 0.08) | (−0.03, −0.005) | (0.002, 0.02) | (−0.01, 0.01) |
| EIBF | EBF During Hospital Stay | Lactation Counseling | EBF at Survey Time | |
|---|---|---|---|---|
| RD | RD | RD | RD | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| Vaginal Births | n = 5048 | n = 5183 | n = 5183 | n = 5001 |
| Constant | 0.33 | 0.71 | 0.88 | 0.71 |
| (0.26, 0.39) | (0.65, 0.77) | (0.85, 0.91) | (0.67, 0.75) | |
| Month | −0.002 | 0.04 | 0.01 | 0.01 |
| (−0.02, 0.01) | (0.02, 0.05) | (0.003, 0.02) | (−0.001, 0.03) | |
| Enrolled | 0.04 | 0.06 | −0.02 | 0.04 |
| (−0.002, 0.09) | (0.02, 0.01) | (−0.05, 0.01) | (−0.003, 0.08) | |
| Month*Enrolled | 0.09 | −0.02 | 0.01 | 0.001 |
| (0.07, 0.11) | (−0.03, −0.005) | (−0.002, 0.02) | (−0.01, 0.02) | |
| Cesarean Births | n = 4142 | n = 4401 | n = 4401 | n = 4243 |
| Constant | 0.29 | 0.59 | 0.86 | 0.71 |
| (0.19, 0.38) | (0.51. 0.68) | (0.83, 0.89) | (0.66, 0.75) | |
| Month | 0.01 | 0.02 | 0.01 | 0.01 |
| (−0.01, 0.02) | (0.01, 0.04) | (−0.003, 0.01) | (−0.0001, 0.03) | |
| Enrolled | 0.08 | 0.05 | 0.03 | 0.01 |
| (0.02, 0.13) | (−0.003, 0.10) | (−0.002, 0.06) | (−0.04. 0.06) | |
| Month*Enrolled | 0.04 | −0.01 | 0.01 | −0.003 |
| (0.03, 0.06) | (−0.03, 0.004) | (−0.0002, 0.02) | (−0.02, 0.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joyce, C.M.; Hou, S.S.-Y.; Ta, B.T.T.; Vu, D.H.; Mathisen, R.; Vincent, I.; Duc, V.N.; Nandi, A. The Association between a Novel Baby-Friendly Hospital Program and Equitable Support for Breastfeeding in Vietnam. Int. J. Environ. Res. Public Health 2021, 18, 6706. https://doi.org/10.3390/ijerph18136706
Joyce CM, Hou SS-Y, Ta BTT, Vu DH, Mathisen R, Vincent I, Duc VN, Nandi A. The Association between a Novel Baby-Friendly Hospital Program and Equitable Support for Breastfeeding in Vietnam. International Journal of Environmental Research and Public Health. 2021; 18(13):6706. https://doi.org/10.3390/ijerph18136706
Chicago/Turabian StyleJoyce, Caroline M., Sherry Shu-Yeu Hou, Binh T. T. Ta, Duong Hoang Vu, Roger Mathisen, Ilona Vincent, Vinh Nguyen Duc, and Arijit Nandi. 2021. "The Association between a Novel Baby-Friendly Hospital Program and Equitable Support for Breastfeeding in Vietnam" International Journal of Environmental Research and Public Health 18, no. 13: 6706. https://doi.org/10.3390/ijerph18136706
APA StyleJoyce, C. M., Hou, S. S.-Y., Ta, B. T. T., Vu, D. H., Mathisen, R., Vincent, I., Duc, V. N., & Nandi, A. (2021). The Association between a Novel Baby-Friendly Hospital Program and Equitable Support for Breastfeeding in Vietnam. International Journal of Environmental Research and Public Health, 18(13), 6706. https://doi.org/10.3390/ijerph18136706







