A Model for Risk Prediction of Cerebrovascular Disease Prevalence—Based on Community Residents Aged 40 and above in a City in China
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sampling Methods
2.3. Survey Content and Method
2.4. Criteria
2.5. Grouping
2.6. Quality Control
2.7. Statistical Analysis
2.8. Calculation of Individual Risk Level of Cerebrovascular Disease
- (1)
- The odds ratio (OR) of each risk factor screened by the Poisson regression model was converted into the risk scores of each impact factor according to the conversion standard shown in Table 1. For example, there are n risk factors that affect the cerebrovascular system, which are recorded as f1, f2, f3…fn. Poisson regression model can be used to calculate the relative risk OR of each risk factor, which are ORf1, ORf2, ORf3…ORfn. According to the range of OR value in Table 1, the corresponding risk score (RC) can be found. The risk scores of each risk factor were RCf1, RCf2, RCf3…RCfn.
- (2)
- Calculate the average risk score of the population. First of all, on the basis of the factors f1, f2, f3…fn that affect cerebrovascular diseases screened by the Poisson regression, consult relevant literature and find the exposure rate (ER) of each influencing factor in the population. The exposure rates of each risk factor were recorded as ERf1, ERf2, ERf3…ERfn. Then, the average risk score (average risk score of the population, AROP) was calculated with the risk score value and exposure rate of the influencing factors.In our study, the AROP was calculated through the following means:
- (1)
- According to the China health statistics yearbook 2019 [31], the exposure rate (ER) of CVD patients aged 60 or above in China in 2018 was 0.17.
- (2)
- According to Chinese guidelines for the prevention and treatment of hypertension (revised edition 2018) [32], the ER of CVD patients who had a medical history of hypertension in China in 2017 was 0.28.
- (3)
- According to Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2017 edition) [33], the ER of CVD patients who had a medical history of type 2 diabetes in China in 2016 was 0.11.
- (4)
- According to a Chinese report on stroke prevention and treatment 2017 [34], the ER of CVD patients with a medical history of stroke in China in 2016 was 0.28.
The specific method for calculation: - (3)
- Calculation of the risk score of individual (RCI): Refer to the scoring standard in Table 1, and according to the questionnaire answered by the individual, the risk score points were accumulated if there was a risk factor; otherwise, the risk score was recorded as 0. The individual risk factor scores were RCIf1, RCIf2, RCIf3…RCIfn. Sum the risk scores of each risk factor formed the total risk value of the individual.The specific calculation method is:
- (4)
- Calculation of the risk of individual cerebrovascular disease R is as follows:The specific calculation method is: .
3. Results
3.1. The Prevalence of Cerebrovascular Disease
3.2. The Risk Factors of Cerebrovascular Disease
3.3. Development of the Risk Prediction Model
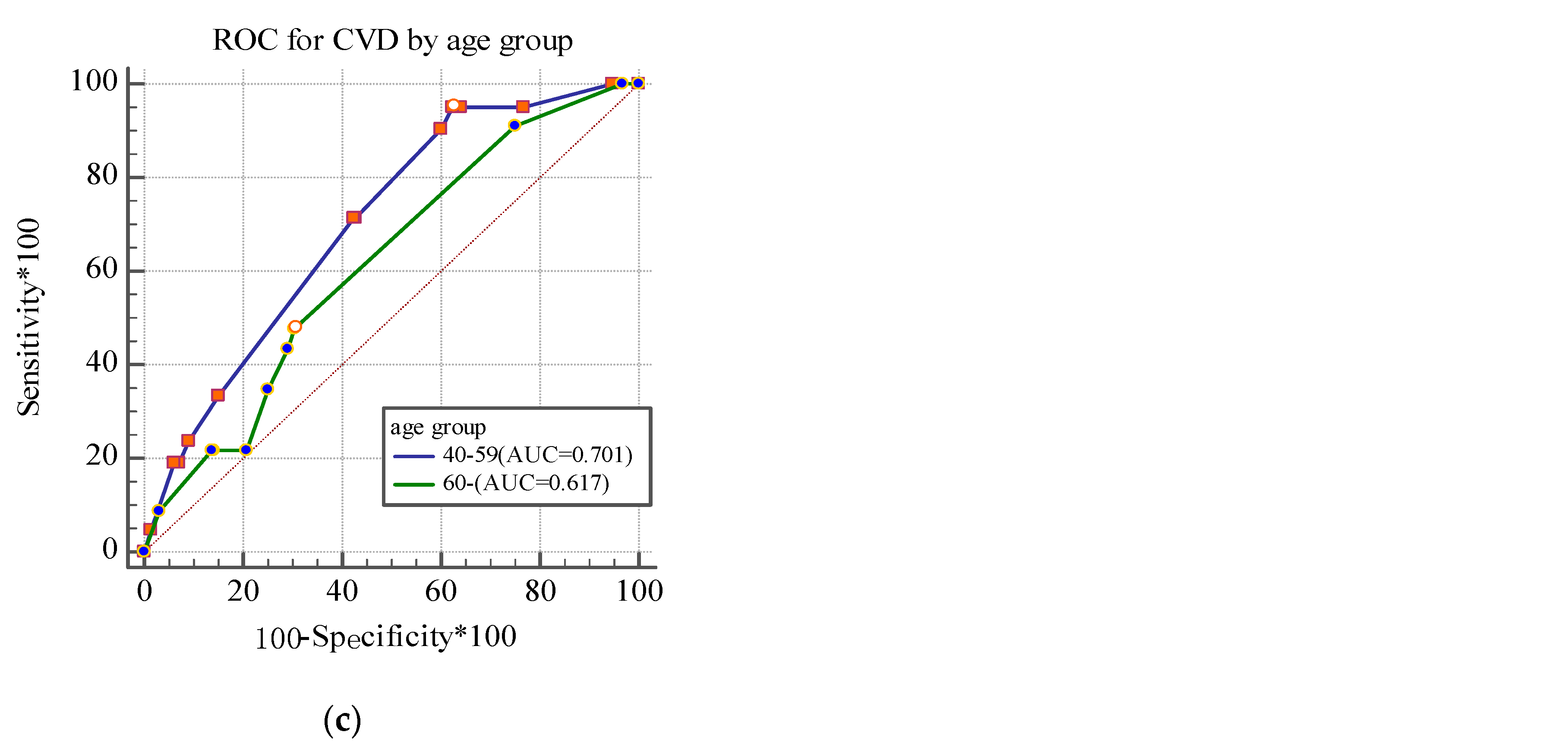
3.4. Validation of the Risk Prediction Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| CVD | Cerebrovascular disease |
| DBP | Diastolic blood pressure |
| OR | Odds ratio |
| ROC | Receiver operating characteristic |
| SBP | Systolic blood pressure |
References
- Roller, R.E. Zerebrovaskuläre Erkrankungen. Cerebrovascular disease. Ther. Umsch. 2008, 65, 441–444. [Google Scholar] [CrossRef]
- Wang, Y.J.; Li, Z.X.; Gu, H.Q.; Zhai, Y.; Jiang, Y.; Zhao, X.Q.; Wang, Y.L.; Yang, X.; Wang, C.J.; Meng, X.; et al. China Stroke Statistics 2019: A Report From the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc. Neurol. 2020, 5, 211–239. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Wang, H.; Zhu, J.; Chen, W.; Wang, L.; Liu, S.; Li, Y.; Wang, L.; Liu, Y.; Yin, P.; et al. Cause-specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 251–272. [Google Scholar] [CrossRef]
- Mora, S.; Cook, N.; Buring, J.E.; Ridker, P.M.; Lee, I.M. Physical activity and reduced risk of cardiovascular events: Potential mediating mechanisms. Circulation 2007, 116, 2110–2118. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.D.; Folsom, A.R.; Blair, S.N. Physical activity and stroke risk: A meta-analysis. Stroke 2003, 34, 2475–2481. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.H.; Liang, W. Life-long physical activity involvement and the risk of ischemic stroke in southern china. Stroke Res. Treat. 2011, 2010, 415241. [Google Scholar] [CrossRef]
- Manson, J.E.; Colditz, G.A.; Stampfer, M.J.; Willett, W.C.; Krolewski, A.S.; Rosner, B.; Arky, R.A.; Speizer, F.E.; Hennekens, C.H. A prospective study of maturity-onset diabetes mellitus and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 1991, 151, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Amarenco, P.; Labreuche, J.; Lavallée, P.; Touboul, P.J. Statins in stroke prevention and carotid atherosclerosis: Systematic review and up-to-date meta-analysis. Stroke 2004, 35, 2902–2909. [Google Scholar] [CrossRef]
- Kurth, T.; Kase, C.S.; Berger, K.; Gaziano, J.M.; Cook, N.R.; Buring, J.E. Smoking and risk of hemorrhagic stroke in women. Stroke 2003, 34, 2792–2795. [Google Scholar] [CrossRef]
- Oliveira, G.B.; Avezum, A.; Roever, L. Cardiovascular Disease Burden: Evolving Knowledge of Risk Factors in Myocardial Infarction and Stroke through Population-Based Research and Perspectives in Global Prevention. Front. Cardiovasc. Med. 2015, 13, 32. [Google Scholar] [CrossRef]
- Brouwer, E.D.; Watkins, D.; Olson, Z.; Goett, J.; Nugent, R.; Levin, C. Provider costs for prevention and treatment of cardiovascular and related conditions in low- and middle-income countries: A systematic review. BMC Public Health 2015, 26, 1183. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Yatsuya, H.; Iso, H.; Yamagishi, K.; Kokubo, Y.; Saito, I.; Suzuki, K.; Sawada, N.; Inoue, M. Development of a point-based prediction model for the incidence of total stroke: Japan public health center study. Stroke 2013, 44, 1295–1302. [Google Scholar] [CrossRef] [PubMed]
- Yin, P.; Qi, J.L.; Liu, Y.N. Burden of disease in the Chinese population from 2005 to 2017. Chin. Circ. J. 2019, 34, 1145–1154. [Google Scholar]
- Nishimura, K.; Okamura, T.; Watanabe, M.; Nakai, M.; Takegami, M.; Higashiyama, A.; Kokubo, Y.; Okayama, A.; Miyamoto, Y. Predicting coronary heart disease using risk factor categories for a Japanese urban population, and comparison with the framingham risk score: The suita study. J. Atheroscler. Thromb. 2014, 21, 784–798. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, S.; Matsumoto, M.; Kayaba, K.; Gotoh, T.; Nago, N.; Tsutsumi, A.; Kajii, E. Risk charts illustrating the 10-year risk of stroke among residents of Japanese rural communities: The JMS Cohort Study. J. Epidemiol. 2009, 19, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.H.; Chen, J.H.; Muo, C.H.; Chang, Y.J.; Sung, F.C.; Hsu, C.Y. Increased risk of ischaemic stroke amongst patients with chronic osteomyelitis: A population-based cohort study in Taiwan. Eur. J. Neurol. 2015, 22, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Root, M.M. Building prediction models for coronary heart disease by synthesizing multiple longitudinal research findings. Eur. J. Cardiovasc. Prev. Rehabil. 2005, 12, 459–464. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Riley, L.; Guthold, R.; Cowan, M.; Savin, S.; Bhatti, L.; Armstrong, T.; Bonita, R. The World Health Organization STEPwise Approach to Noncommunicable Disease Risk-Factor Surveillance: Methods, Challenges, and Opportunities. Am. J. Public Health 2016, 106, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Soler, E.P.; Ruiz, V.C. Epidemiology and risk factors of cerebral ischemia and ischemic heart diseases: Similarities and differences. Curr. Cardiol. Rev. 2010, 6, 138–149. [Google Scholar] [CrossRef]
- Truett, J.; Cornfield, J.; Kannel, W. A multivariate analysis of the risk of coronary heart disease in Framingham. J. Chronic Dis. 1967, 20, 511–524. [Google Scholar] [CrossRef]
- Slager, C.J.; Wentzel, J.J.; Gijsen, F.J.; Schuurbiers, J.C.; van der Wal, A.C.; van der Steen, A.F.; Serruys, P.W. The role of shear stress in the generation of rupture-prone vulnerable plaques. Nat. Clin. Pract. Cardiovasc. Med. 2005, 2, 401–407. [Google Scholar] [CrossRef]
- Colditz, G.A.; Samplin-Salgado, M.; Ryan, C.T.; Dart, H.; Fisher, L.; Tokuda, A.; Rockhill, B. Harvard Center for Cancer Prevention. Harvard report on cancer prevention, volume 5: Fulfilling the potential for cancer prevention: Policy approaches. Cancer Causes Control 2002, 13, 199–212. [Google Scholar] [CrossRef]
- Kim, D.J.; Rockhill, B.; Colditz, G.A. Validation of the Harvard Cancer Risk Index: A prediction tool for individual cancer risk. J. Clin. Epidemiol. 2004, 57, 332–340. [Google Scholar] [CrossRef]
- Padwal, R.S.; Hemmelgarn, B.R.; Khan, N.A.; Grover, S.; McAlister, F.A.; McKay, D.W.; Wilson, T.; Penner, B.; Burgess, E.; Bolli, P.; et al. The 2008 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1—Blood pressure measurement, diagnosis and assessment of risk. Can. J. Cardiol. 2008, 24, 455–463. [Google Scholar] [CrossRef][Green Version]
- Kopin, L.; Lowenstein, C. Dyslipidemia. Ann. Intern. Med. 2017, 167, ITC81–ITC96. [Google Scholar] [CrossRef]
- Chamberlain, J.J.; Rhinehart, A.S.; Shaefer, C.F., Jr.; Neuman, A. Diagnosis and Management of Diabetes: Synopsis of the 2016 American Diabetes Association Standards of Medical Care in Diabetes. Ann. Intern. Med. 2016, 164, 542–552. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Jiang, B.; Sun, H.; Ru, X.; Sun, D.; Wang, L.; Wang, L.; Jiang, Y.; Li, Y.; Wang, Y.; et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017, 135, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Atwood, K.A.; Emmons, K.; Monson, R.R.; Willett, W.C.; Trichopoulos, D.; Hunter, D.J. Harvard report on cancer prevention volume 4: Harvard Cancer Risk Index. Risk Index Working Group, Harvard Center for Cancer Prevention. Cancer Causes Control 2000, 11, 477–488. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of China. China Health Statistics Yearbook 2019 in Beijing; China Union Medical College Press: Beijing, China, 2019.
- Wang, Z.W.; Wang, W. Interpretation of Chinese guidelines for the prevention and treatment of hypertension (revised edition 2018). Chin. Cardiovasc. Dis. 2019, 17, 193–197. [Google Scholar]
- Society, C.D. Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2017 Edition). Chin. J. Pract. Intern. Med. 2018, 38, 292–344. [Google Scholar]
- Wang, L.D.; Liu, J.M.; Yang, Y. Summary of Chinese report on stroke prevention and treatment 2017. Chin. J. Cerebrovasc. Dis. 2018, 15, 56–62. [Google Scholar]
- Bastien, M.; Poirier, P.; Lemieux, I.; Després, J.P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog. Cardiovasc. Dis. 2014, 56, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Batsis, J.A.; Coutinho, T.; Somers, V.K.; Hodge, D.O.; Carter, R.E.; Sochor, O.; Kragelund, C.; Kanaya, A.M.; Zeller, M.; et al. Normal-Weight Central Obesity and Mortality Risk in Older Adults with Coronary Artery Disease. Mayo Clin. Proc. 2016, 91, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Roughead, E.E.; Kalisch, L.M.; Ramsay, E.N.; Ryan, P.; Gilbert, A.L. Use of health services and medicines amongst Australian war veterans: A comparison of young elderly, near centenarians and centenarians. BMC Geriatr. 2010, 10, 83. [Google Scholar] [CrossRef]
- Lackland, D.T.; Weber, M.A. Global burden of cardiovascular disease and stroke: Hypertension at the core. Can. J. Cardiol. 2015, 31, 569–571. [Google Scholar] [CrossRef]
- Karmali, K.N.; Lloyd-Jones, D.M. Global Risk Assessment to Guide Blood Pressure Management in Cardiovascular Disease Prevention. Hypertension 2017, 69, e2–e9. [Google Scholar] [CrossRef]
- Bloch, K.V.; Szklo, M.; Kuschnir, M.C.; Abreu Gde, A.; Barufaldi, L.A.; Klein, C.H.; de Vasconcelos, M.T.; da Veiga, G.V.; Figueiredo, V.C.; Dias, A.; et al. The Study of Cardiovascular Risk in Adolescents—ERICA: Rationale, design and sample characteristics of a national survey examining cardiovascular risk factor profile in Brazilian adolescents. BMC Public Health 2015, 15, 850. [Google Scholar] [CrossRef]
- Ádám, B.; Molnár, Á.; Gulis, G.; Ádány, R. Integrating a quantitative risk appraisal in a health impact assessment: Analysis of the novel smoke-free policy in Hungary. Eur. J. Public Health 2013, 23, 211–217. [Google Scholar] [CrossRef]
- Pirie, K.; Peto, R.; Reeves, G.K.; Green, J.; Beral, V.; Million Women Study Collaborators. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet 2013, 381, 133–141. [Google Scholar] [CrossRef]
- Smith, P.J.; Blumenthal, J.A.; Hoffman, B.M.; Cooper, H.; Strauman, T.A.; Welsh-Bohmer, K.; Browndyke, J.N.; Sherwood, A. Aerobic exercise and neurocognitive performance: A meta-analytic review of randomized controlled trials. Psychosom. Med. 2010, 72, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Cotman, C.W.; Berchtold, N.C.; Christie, L.A. Exercise builds brain health: Key roles of growth factor cascades and inflammation. Trends Neurosci. 2007, 30, 464–472. [Google Scholar] [CrossRef]
- Aycock, D.M.; Kirkendoll, K.D.; Coleman, K.C.; Clark, P.C.; Albright, K.C.; Alexandrov, A.W. Family history of stroke among African Americans and its association with risk factors, knowledge, perceptions, and exercise. J. Cardiovasc. Nurs. 2015, 30, E1–E6. [Google Scholar] [CrossRef]
- Debette, S.; Goeggel Simonetti, B.; Schilling, S.; Martin, J.J.; Kloss, M.; Sarikaya, H.; Hausser, I.; Engelter, S.; Metso, T.M.; Pezzini, A.; et al. Familial occurrence and heritable connective tissue disorders in cervical artery dissection. Neurology 2014, 83, 2023–2031. [Google Scholar] [CrossRef] [PubMed]
- O’eill, S.M.; Rubinstein, W.S.; Wang, C.; Yoon, P.W.; Acheson, L.S.; Rothrock, N.; Starzyk, E.J.; Beaumont, J.L.; Galliher, J.M.; Ruffin, M.T., IV; et al. Familial risk for common diseases in primary care: The Family Healthware Impact Trial. Am. J. Prev. Med. 2009, 36, 506–514. [Google Scholar] [CrossRef]
- Jousilahti, P.; Rastenyte, D.; Tuomilehto, J.; Sarti, C.; Vartiainen, E. Parental history of cardiovascular disease and risk of stroke. A prospective follow-up of 14371 middle-aged men and women in Finland. Stroke 1997, 28, 1361–1366. [Google Scholar] [CrossRef] [PubMed]

| Odds Ratio (OR) | Strength of Association | Mark | Risk Score |
|---|---|---|---|
| 0.9~1.1 | Not significant | 0 | |
| 0.7~0.9 or 1.1~1.4 | Weak | − or + | 5 |
| 0.4~0.6 or 1.5~2.9 | Moderate | −− or ++ | 10 |
| 0.2~0.3 or 3.0~6.9 | Strong | −−− or +++ | 25 |
| <0.2 or 7.0~ | Very strong | −−−− or ++++ | 50 |
| R | Risk Levels |
|---|---|
| R < 0 | Very low |
| 0 < R < 0.5 | Lower |
| 0.5 < R < 0.9 | Low |
| 0.9 < R < 1.1 | Moderate |
| 1.1 < R < 2.0 | High |
| 2.0 < R < 5.0 | Higher |
| R > 5.0 | Very high |
| Modelling Group | Validation Group | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | Prevalence of CVD | p | ||
| Gender | Male | 401 | 37.51 | 421 | 39.38 | 822 | 6.3 | 0.001 |
| Female | 668 | 62.49 | 648 | 60.62 | 1316 | 3.3 | ||
| Age | 40–59 | 299 | 27.97 | 284 | 26.57 | 583 | 3.1 | <0.001 |
| 60- | 770 | 72.03 | 785 | 73.43 | 1555 | 7.2 | ||
| Physical exercise | Lack of exercise | 188 | 17.59 | 201 | 18.80 | 389 | 8.0 | <0.001 |
| Exercise regularly | 881 | 82.41 | 868 | 81.20 | 1749 | 3.7 | ||
| Smoking | No | 911 | 85.22 | 907 | 84.85 | 1818 | 3.8 | <0.001 |
| Yes | 158 | 14.78 | 162 | 15.15 | 320 | 8.4 | ||
| Alcohol drinking | No | 927 | 86.72 | 907 | 84.85 | 1834 | 4.7 | 0.275 |
| Yes | 142 | 13.28 | 162 | 15.15 | 304 | 3.3 | ||
| Obesity | No | 839 | 78.48 | 830 | 77.64 | 1669 | 4.4 | 0.624 |
| Yes | 230 | 21.52 | 239 | 22.36 | 469 | 4.9 | ||
| Hypertension | No | 488 | 45.65 | 467 | 43.69 | 955 | 1.9 | <0.001 |
| Yes | 581 | 54.35 | 602 | 56.31 | 1183 | 6.6 | ||
| Dyslipidemia | No | 601 | 56.22 | 614 | 57.44 | 1215 | 4.0 | 0.167 |
| Yes | 468 | 43.78 | 455 | 42.56 | 923 | 5.2 | ||
| Diabetes | No | 920 | 86.06 | 913 | 85.41 | 1833 | 3.5 | <0.001 |
| Yes | 149 | 13.94 | 156 | 14.59 | 305 | 10.5 | ||
| Cardiopathy | No | 940 | 87.9 | 934 | 87.37 | 1874 | 4.3 | 0.318 |
| Yes | 129 | 12.07 | 135 | 12.63 | 264 | 5.7 | ||
| Family history of CVD | No | 925 | 86.53 | 911 | 85.22 | 1836 | 3.9 | 0.002 |
| Yes | 144 | 13.47 | 158 | 14.78 | 302 | 7.9 | ||
| Total | 1069 | 1069 | 2138 | 4.5 | ||||
| β | Wald χ2 | p | OR # | 95%CI | |
|---|---|---|---|---|---|
| Constant | –5.405 | 90.808 | <0.001 | ||
| Age group | |||||
| 40–59 | 1 | ||||
| 60- | 1.189 | 4.046 | 0.025 | 3.284 | 1.310~11.019 |
| Physical exercise | |||||
| Exercise regularly | 1 | ||||
| Lack of exercise | 0.836 | 7.897 | 0.005 | 2.306 | 1.258~4.068 |
| Smoking | |||||
| No | 1 | ||||
| Yes | 0.667 | 4.469 | 0.035 | 1.949 | 1.015~3.534 |
| Hypertension | |||||
| No | 1 | ||||
| Yes | 0.920 | 6.607 | 0.010 | 2.510 | 1.296~5.351 |
| Diabetes | |||||
| No | 1 | ||||
| Yes | 1.161 | 16.138 | <0.001 | 3.194 | 1.786~5.586 |
| Family history of CVD | |||||
| No | 1 | ||||
| Yes | 0.839 | 5.768 | 0.016 | 2.315 | 1.167~4.593 |
| Risk Factors | OR # | Risk Score | Exposure of the Reference Population | |
|---|---|---|---|---|
| Size | Resource | |||
| Age (≥60) | 3.171 | 25 | 0.17 | China health statistics yearbook 2019 |
| Physical exercise | 2.306 | 10 | 0.82 | Data from this study |
| Hypertension | 2.436 | 10 | 0.28 | Chinese guidelines for the prevention and treatment of hypertension (revised edition 2018) |
| Diabetes | 3.220 | 25 | 0.11 | Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2017 Edition) |
| Smoking | 1.877 | 10 | 0.28 | Chinese report on stroke prevention and treatment 2017 |
| Family history of CVD * | 2.315 | 10 | 0.14 | Data from this study |
| Risk Level | Modeling Group | Validation Group (Predicted Risk Level) | Validation Group (Actual Risk Level) | |||
|---|---|---|---|---|---|---|
| N Enrolled (%) | N Illness (%) | N Enrolled (%) | N Illness (%) | N Enrolled (%) | N Illness (%) | |
| Very low | 30 (2.8) | 0 (0.0) | 35 (3.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Relatively low | 123 (11.51) | 0 (0.0) | 126 (11.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Low | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| General | 75 (7.0) | 2 (2.6) | 88 (8.2) | 1 (0.8) | 307 (30.0) | 4 (1.3) |
| Relatively high | 283 (26.5) | 11 (3.7) | 241 (22.5) | 7 (2.9) | 234 (22.8.) | 5 (2.1) |
| High | 506 (47.3) | 39 (7.2) | 579 (54.2) | 36 (6.2) | 484 (47.2) | 35 (6.7) |
| Total | 1069 (100.0) | 52 (4.9) | 1069 (100.0) | 44 (4.1) | 1069 (100.0) | 44 (4.1) |
| Cut-Off Point | Male | Female | Total | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity% | Specificity% | Youden index | PPV% | NPV% | Sensitivity% | Specificity% | Youden index | PPV% | NPV% | Sensitivity% | Specificity% | Youden Index | PPV% | NPV% | |
| 0.45 | 100.0 | 7.6 | 0.076 | 6.6 | 100 | 94.4 | 20.6 | 0.151 | 3.3 | 99.1 | 97.7 | 15.6 | 0.133 | 4.7 | 99.4 |
| 0.90 | 100.0 | 14.4 | 0.144 | 7.1 | 100 | 94.4 | 30.3 | 0.248 | 3.7 | 99.4 | 97.7 | 24.2 | 0.219 | 5.2 | 99.6 |
| 1.13 | 100.0 | 16.0 | 0.160 | 7.3 | 100 | 94.4 | 33.2 | 0.276 | 3.9 | 99.4 | 97.7 | 26.5 | 0.243 | 5.4 | 99.6 |
| 1.35 | 100.0 | 17.7 | 0.177 | 7.4 | 100 | 88.9 | 34.6 | 0.235 | 3.7 | 98.9 | 95.5 | 28.1 | 0.236 | 5.4 | 99.3 |
| 1.58 | 88.5 | 31.4 | 0.199 | 7.8 | 97.6 | 72.2 | 56.5 | 0.287 | 4.5 | 98.6 | 81.8 | 46.8 | 0.287 | 6.2 | 98.4 |
| 1.80 | 88.5 | 31.9 | 0.204 | 7.9 | 97.7 | - | - | - | - | - | 81.8 | 47.0 | 0.288 | 6.2 | 98.4 |
| 2.03 | 53.9 | 69.6 | 0.235 | 10.4 | 95.8 | 22.2 | 86.2 | 0.084 | 4.4 | 97 | 40.9 | 79.8 | 0.207 | 7.7 | 96.9 |
| 2.25 | 50.0 | 70.1 | 0.201 | 9.9 | 95.1 | 22.2 | 86.5 | 0.087 | 4.5 | 97 | 38.6 | 80.2 | 0.188 | 7.4 | 96.8 |
| 2.48 | 42.3 | 73.7 | 0.160 | 9.6 | 94.5 | 16.7 | 89.4 | 0.060 | 4.3 | 96.9 | 34.1 | 81.6 | 0.157 | 7.0 | 96.6 |
| 2.70 | 26.9 | 83.3 | 0.102 | 11.9 | 94.8 | 11.1 | 93.0 | 0.041 | 4.3 | 96.8 | 20.5 | 90.6 | 0.111 | 8.6 | 96.3 |
| 3.15 | 11.5 | 97.7 | 0.093 | 25 | 93.8 | 0.0 | 97.9 | −0.021 | 0.0 | 96.6 | 6.8 | 97.9 | 0.047 | 12.0 | 95.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Q.; Luo, D.; Zhou, X.; Cai, X.; Li, Q.; Lu, Y.; Chen, J. A Model for Risk Prediction of Cerebrovascular Disease Prevalence—Based on Community Residents Aged 40 and above in a City in China. Int. J. Environ. Res. Public Health 2021, 18, 6584. https://doi.org/10.3390/ijerph18126584
Zhu Q, Luo D, Zhou X, Cai X, Li Q, Lu Y, Chen J. A Model for Risk Prediction of Cerebrovascular Disease Prevalence—Based on Community Residents Aged 40 and above in a City in China. International Journal of Environmental Research and Public Health. 2021; 18(12):6584. https://doi.org/10.3390/ijerph18126584
Chicago/Turabian StyleZhu, Qin, Die Luo, Xiaojun Zhou, Xianxu Cai, Qi Li, Yuanan Lu, and Jiayan Chen. 2021. "A Model for Risk Prediction of Cerebrovascular Disease Prevalence—Based on Community Residents Aged 40 and above in a City in China" International Journal of Environmental Research and Public Health 18, no. 12: 6584. https://doi.org/10.3390/ijerph18126584
APA StyleZhu, Q., Luo, D., Zhou, X., Cai, X., Li, Q., Lu, Y., & Chen, J. (2021). A Model for Risk Prediction of Cerebrovascular Disease Prevalence—Based on Community Residents Aged 40 and above in a City in China. International Journal of Environmental Research and Public Health, 18(12), 6584. https://doi.org/10.3390/ijerph18126584







