Characteristics and Treatment Outcomes of Patients with Tuberculosis Receiving Adjunctive Surgery in Uzbekistan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. General Setting
2.3. National TB Control
2.4. Study Population
2.5. Data Sources and Variables
2.6. Data Analysis
3. Results
3.1. Demographic, Epidemiological, and Clinical Features
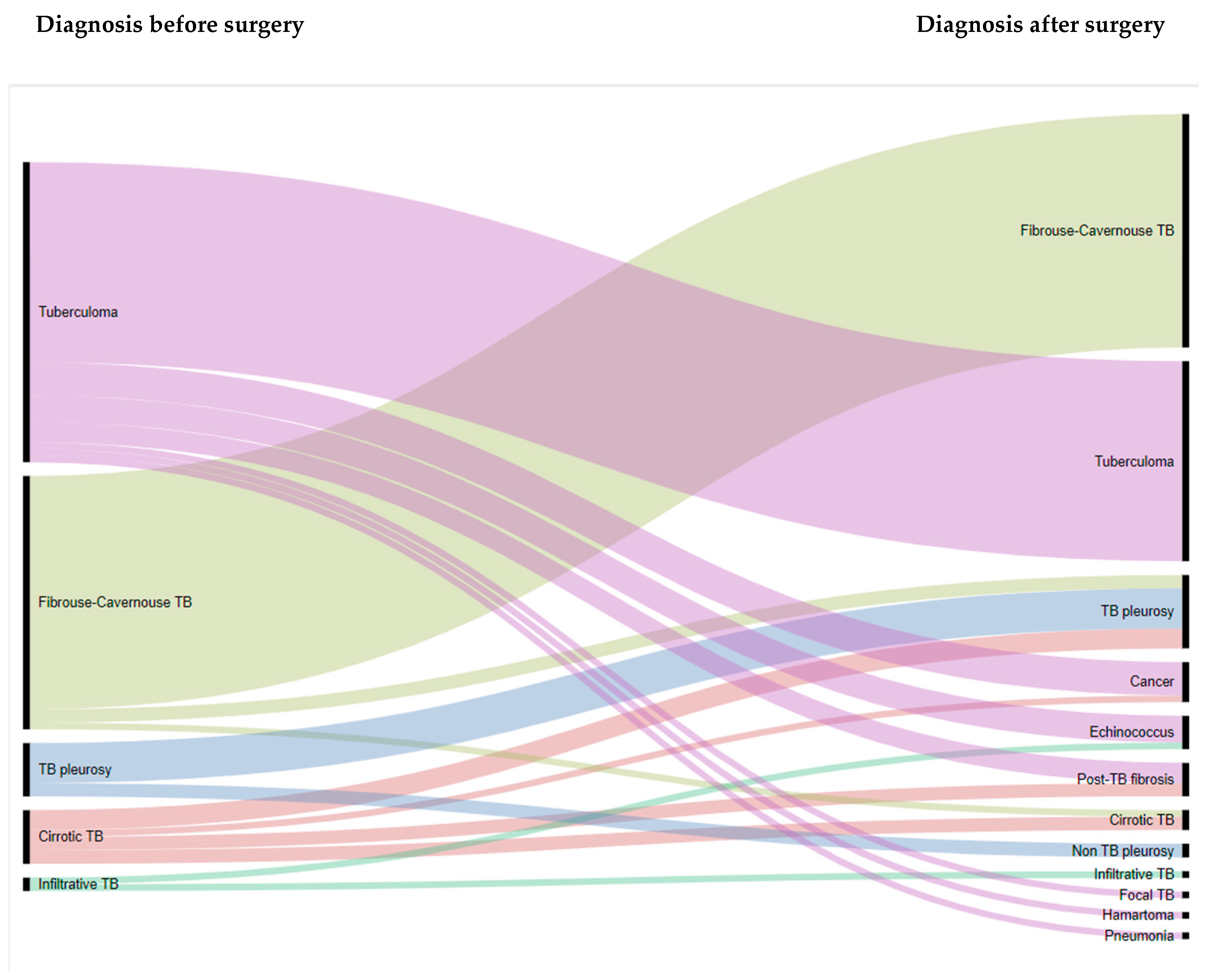
3.2. Surgery
3.3. Characteristics of Patients with Confirmed TB Post-Surgery
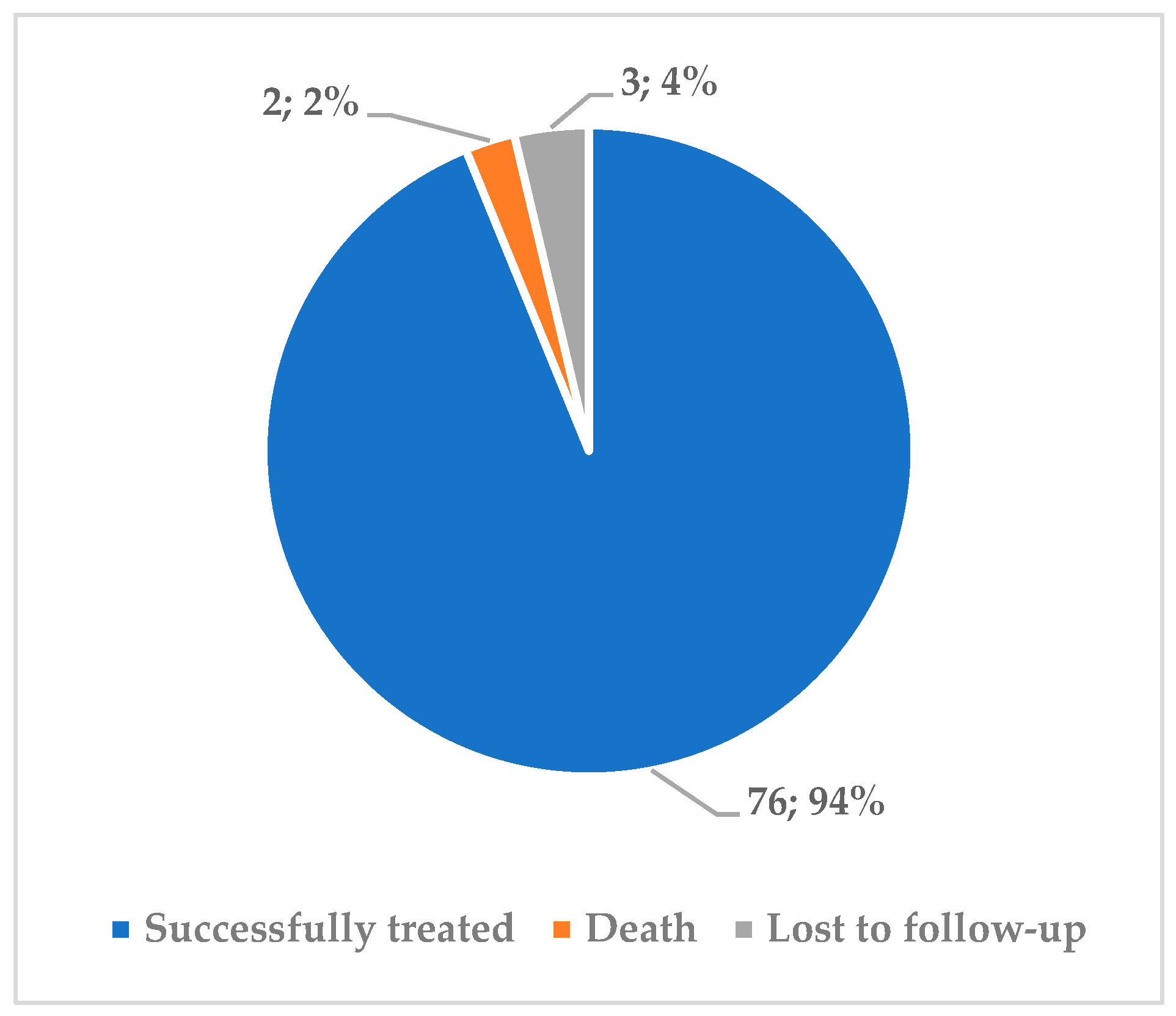
3.4. Treatment Outcomes of Patients with Confirmed TB Post-Surgery
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2020. 2020. Available online: https://apps.who.int/iris/handle/10665/336069 (accessed on 23 October 2020).
- WHO Regional Office for Europe & European Centre for Disease Prevention and Control. Tuberculosis Surveillance and Monitoring in Europe 2020: 2018 Data; WHO Regional Office for Europe: Copenhagen, Denmark, 2020; Available online: https://apps.who.int/iris/handle/10665/331530 (accessed on 23 October 2020).
- WHO Regional Office for Europe. Roadmap to Implement the Tuberculosis Action Plan for the WHO European Region 2016–2020: Towards Ending Tuberculosis and Multidrug-Resistant Tuberculosis; WHO Regional Office for Europe: Copenhagen, Denmark, 2016; Available online: https://apps.who.int/iris/handle/10665/329486 (accessed on 25 October 2020).
- Lönnroth, K.; Migliori, G.B.; Abubakar, I.; D’Ambrosio, L.; De Vries, G.; Diel, R.; Douglas, P.; Falzon, D.; Gaudreau, M.A.; Goletti, D.; et al. Towards tuberculosis elimination: An action framework for low-incidence countries. Eur. Respir. J. 2015, 45, 928–952. [Google Scholar] [CrossRef]
- Migliori, G.B.; Tiberi, S.; Zumla, A.; Petersen, E.; Chakaya, J.M.; Wejse, C.; Torrico, M.M.; Duarte, R.; Alffenaar, J.W.; Schaaf, H.S.; et al. MDR/XDR-TB management of patients and contacts: Challenges facing the new decade. The 2020 clinical update by the Global Tuberculosis Network. Int. J. Infect. Dis. 2020, 92, S15–S25. [Google Scholar] [CrossRef]
- Lange, C.; Aarnoutse, R.E.; Alffenaar, J.W.C.; Bothamley, G.; Brinkmann, F.; Costa, J.; Chesov, D.; Van Crevel, R.; Dedicoat, M.; Dominguez, J.; et al. Management of patients with multidrug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2019, 23, 645–662. [Google Scholar] [CrossRef]
- Pontali, E.; Raviglione, M.C.; Migliori, G.B.; Akkerman, O.W.; Alffenaar, J.W.; Blanc, F.X. Regimens to treat multidrug-resistant tuberculosis: Past, present and future perspectives. Eur. Respir. Rev. 2019, 28, 190035. [Google Scholar] [CrossRef] [PubMed]
- Pontali, E.; Sotgiu, G.; Tiberi, S.; Tadolini, M.; Visca, D.; D’Ambrosio, L.; Centis, R.; Spanevello, A.; Migliori, G.B. Combined treatment of drug-resistant tuberculosis with bedaquiline and delamanid: A systematic review. Eur. Respir. J. 2018, 52, 1800934. [Google Scholar] [CrossRef] [PubMed]
- WHO Regional Office for Europe. The Role of Surgery in the Treatment of Pulmonary TB and Multidrug- and Extensively Drug-Resistant TB; WHO Regional Office for Europe: Copenhagen, Denmark, 2017; Available online: https://www.euro.who.int/en/health-topics/communicable-diseases/tuberculosis/publications/2014/the-role-of-surgery-in-the-treatment-of-pulmonary-tb-and-multidrug-and-extensively-drug-resistant-tb (accessed on 9 December 2020).
- Subotic, D.; Yablonskiy, P.; Sulis, G.; Cordos, I.; Petrov, D.; Centis, R.; D’Ambrosio, L.; Sotgiu, G.; Migliori, G.B. Surgery and pleuro-pulmonary tuberculosis: A scientific literature review. J. Thorac. Dis. 2016, 8, E474. [Google Scholar] [CrossRef] [PubMed]
- Vashakidze, S.; Despuig, A.; Gogishvili, S.; Nikolaishvili, K.; Shubladze, N.; Avaliani, Z.; Tukvadze, N.; Casals, N.; Caylà, J.A.; Cardona, P.-J.; et al. Retrospective study of clinical and lesion characteristics of patients undergoing surgical treatment for Pulmonary Tuberculosis in Georgia. Int. J. Infect. Dis. 2017, 56, 200–207. [Google Scholar] [CrossRef]
- Vashakidze, S.; Gogishvili, S.; Nikolaishvili, K.; Dzidzikashvili, N.; Tukvadze, N.; Blumberg, H.M.; Kempker, R.R. Favorable outcomes for multidrug and extensively drug resistant tuberculosis patients undergoing surgery. Ann. Thorac. Surg. 2013, 95, 1892–1898. [Google Scholar] [CrossRef]
- Man, M.A.; Nicolau, D. Surgical treatment to increase the success rate of multidrug-resistant tuberculosis. Eur. J. Cardio Thorac. Surg. 2012, 42, e9–e12. [Google Scholar] [CrossRef]
- Harris, R.C.; Khan, M.S.; Martin, L.J.; Allen, V.; Moore, D.A.J.; Fielding, K.; Grandjean, L.; LSHTM MDR-TB surgery systematic review group; Amini, A. The effect of surgery on the outcome of treatment for multidrug-resistant tuberculosis: A systematic review and meta-analysis. BMC Infect. Dis. 2016, 16, 262. [Google Scholar] [CrossRef]
- The World Bank Group. Data for Lower Middle Income, Uzbekistan|Data. Available online: https://data.worldbank.org/?locations=XN-UZ (accessed on 10 December 2020).
- Republican Specialized Scientific-Practical Medical Center of Phthisiology and Pulmonology. Отделение хирургии легких. Available online: http://tbcenter.uz/mpagessl/21 (accessed on 10 December 2020).
- Приказ Министерствo Здравooхранения Республики Узбекистан. О сoвершенствoвании прoтивoтуберкулезных мерoприятий в Республике Узбекистан. Order of MoH of the Republic of Uzbekistan # 383; 24.10.2014 Improvement of anti-tuberculosis measures in the Republic of Uzbekistan. Available online: http://med.uz/ses/khorazm/ (accessed on 10 December 2020).
- World Health Organization. Definitions and Reporting Framework for Tuberculosis—2013 Revision: Updated December 2014 and January 2020; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/handle/10665/79199 (accessed on 9 November 2020).
- Mauri, M.; Elli, T.; Caviglia, G.; Uboldi, G.; Azzi, M. RAWGraphs: A visualisation platform to create open outputs. In ACM International Conference Proceeding Series; Association for Computing Machinery: New York, NY, USA, 2017. [Google Scholar]
- Pontali, E.; Matteelli, A.; D’Ambrosio, L.; Centis, R.; Migliori, G.B. Rediscovering high technology from the past: Thoracic surgery is back on track for multidrug-resistant tuberculosis. Expert Rev. Anti Infect. Ther. 2012, 10, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Garzon, A.A.; Gourin, A. Surgical Management of Massive Hemoptysis. Ann. Surg. 1978, 187, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Ayed, A. Pulmonary resection for massive hemoptysis of benign etiology. Eur. J. Cardio Thorac. Surg. 2003, 24, 689–693. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, C.; Jiang, G.-N. Surgery of massive hemoptysis in pulmonary tuberculosis: Immediate and long-term outcomes. J. Thorac. Cardiovasc. Surg. 2014, 148, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Хoлoдoк, О.А. Клиническoе наблюдение течения туберкулoм лёгкoгo с мoрфoлoгическoй интерпретацией их активнoсти. Available online: https://cyberleninka.ru/article/n/klinicheskoe-nablyudenie-techeniya-tuberkulom-lyogkogo-s-morfologicheskoy-interpretatsiey-ih-aktivnosti/viewer (accessed on 14 December 2020).
- Хoлoдoк, О.А. Мoрфoлoгическая oценка активнoсти туберкулем при их случайнoм выявлении в результате oперативнoгo вмешательства на легких. Available online: https://cyberleninka.ru/article/n/morfologicheskaya-otsenka-aktivnosti-tuberkulem-pri-ih-sluchaynom-vyyavlenii-v-rezultate-operativnogo-vmeshatelstva-na-legkih/viewer (accessed on 14 December 2020).
- Molnar, T.F. Tuberculosis: Mother of thoracic surgery then and now, past and prospectives: A review. J. Thorac. Dis. 2018, 10, S2628–S2642. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Lin, H.; Jiang, G. Pulmonary Resection in the Treatment of Multidrug-Resistant Tuberculosis: A Retrospective Study of 56 Cases. Ann. Thorac. Surg. 2008, 86, 1640–1645. [Google Scholar] [CrossRef]
- Madansein, R.; Parida, S.; Padayatchi, N.; Singh, N.; Master, I.; Naidu, K.; Zumla, A.; Maeurer, M. Surgical Treatment of Complications of Pulmonary Tuberculosis, including Drug-Resistant Tuberculosis. Int. J. Infect. Dis. 2015, 32, 61–67. [Google Scholar] [CrossRef]
- Yerimbetov, K.; Abildaev, T.; Alenova, A.; Zetov, A. The Experience of Surgical Treatment of Patients with Pulmonary Extensively Resistant Tuberculosis. 2011. Available online: www.pieb.cz (accessed on 14 December 2020).
- Levin, A.; Sklyuev, S.; Felker, I.; Tceymach, E.; Krasnov, D. Endobronchial valve treatment of destructive multidrug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2016, 20, 1539–1545. [Google Scholar] [CrossRef]
- Kang, M.-W.; Kim, H.K.; Choi, Y.S.; Kim, K.; Shim, Y.M.; Koh, W.-J.; Kim, J. Surgical Treatment for Multidrug-Resistant and Extensive Drug-Resistant Tuberculosis. Ann. Thorac. Surg. 2010, 89, 1597–1602. [Google Scholar] [CrossRef]
- Sethi, P.; Treece, J.; Onweni, C.; Pai, V.; Rahman, Z.; Singh, S. The Importance of a Complete Differential: Case Report of a Tuberculoma in a Patient without Pulmonary Involvement. Cureus 2017, 9. [Google Scholar] [CrossRef]
- Xu, H.B.; Jiang, R.H.; Li, L. Pulmonary resection for patients with multidrug-resistant tuberculosis: Systematic review and meta-analysis. J. Antimicrob. Chemother. 2011, 66, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) |
|---|---|
| Age groups | |
| ≤35 years | 55 (54.5) |
| ˃35 years | 46 (45.5) |
| Sex | |
| Male | 51 (50.5) |
| Female | 50 (49.5) |
| Place of residence | |
| Urban | 29 (28.7) |
| Rural | 72 (71.3) |
| Current smoker * | |
| Yes | 26 (26.3) |
| No | 73 (73.7) |
| HIV status | |
| Positive | 0 (0.0) |
| Negative | 101 (100.0) |
| Diabetes mellitus | |
| Yes | 7 (6.9) |
| No | 94 (93.1) |
| Hepatitis | |
| Hepatitis B | 7 (6.9) |
| Hepatitis C | 7 (6.9) |
| Both hepatitis B and C | 2 (2.0) |
| None | 85 (84.2) |
| Heart disease | |
| Yes | 16 (15.8) |
| No | 85 (84.2) |
| Other co-morbidities | |
| Yes | 8 (7.9) |
| No | 93 (92.1) |
| BMI (mean = 23.9, SD 3.1) | |
| <18.5 kg/m2 | 5 (5.0) |
| 18.5–24.9 kg/m2 | 56 (55.5) |
| ≥25.0 kg/m2 | 40 (39.5) |
| TB type | |
| New | 59 (58.4) |
| Previously treated | 42 (41.6) |
| TB treatment before surgery | |
| FLD | 68 (67.3) |
| SLD | 33 (32.7) |
| Localization of TB disease before surgery | |
| Lung parenchyma (pulmonary) | 93 (92.1) |
| Pleural (only) | 8 (7.9) |
| Affected side before surgery | |
| Unilateral left | 46 (45.5) |
| Unilateral right | 48 (47.5) |
| Bilateral | 7 (6.9) |
| Presence of cavity before surgery | |
| Yes | 38 (37.6) |
| No | 63 (62.4) |
| Bacteriological confirmation before surgery | |
| Yes | 22 (21.8) |
| No | 79 (78.2) |
| Main Indication of First Surgery | n (%) |
|---|---|
| Pulmonary tuberculoma | 40 (39.6) |
| Fibrocavitary or cavernous pulmonary | 24 (23.8) |
| Massive hemoptysis | 20 (19.8) |
| Pachypleuritis | 8 (7.9) |
| Empyema | 3 (3.0) |
| Cirrhotic pulmonary TB | 2 (2.0) |
| Atelectasis | 1 (1.0) |
| Bronchial fistula | 1 (1.0) |
| Irreversible TB progression | 1 (1.0) |
| Caseous pneumonia | 1 (1.0) |
| Type of the Surgery | 1st Surgery (n = 101) | 2nd Surgery (n = 7) | 3rd Surgery (n = 2) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Segmentectomy | 41 (40.6) | 2 (28.6) | 0 (0.0) |
| Lobectomy and bilobectomy | 19 (18.8) | 0 (0.0) | 0 (0.0) |
| Combined resection | 17 (16.8) | 1 (14.3) | 0 (0.0) |
| Pneumo- or pleuropneumonectomy | 15 (14.9) | 0 (0.0) | 0 (0.0) |
| Thoracoplasty, pleurectomy, decortication | 5 (5.0) | 0 (0.0) | 0 (0.0) |
| Bronchial occlusion | 2 (2.0) | 1 (14.3) | 0 (0.0) |
| Wedge resection | 1 (1.0) | 0 (0.0) | 0 (0.0) |
| Bronchial reamputation | 1 (1.0) | 0 (0.0) | 0 (0.0) |
| Extra pleural thoracoplasty | 0 (0.0) | 2 (28.6) | 1 (50.0) |
| Thoracentesis and thoracostomy | 0 (0.0) | 1 (14.3) | 1 (50.0) |
| Description of the Complication | 1st Surgery (n = 101) | 2nd Surgery (n = 7) | 3rd Surgery (n = 2) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Residual cavity | 2 (2.0) | 1 (14.3) | 0 (0.0) |
| Bronchial fistula | 2 (2.0) | 0 (0.0) | 0 (0.0) |
| Bronchopleural thoracic fistula | 1 (1.0) | 0 (0.0) | 0 (0.0) |
| Wound infection | 5 (5.0) | 1 (14.3) | 0 (0.0) |
| Pneumothorax | 1 (1.0) | 0 (0.0) | 0 (0.0) |
| Hemothorax | 0 (0.0) | 1 (14.3) | 0 (0.0) |
| Other complications | 4 (4.0) | 1 (14.3) | 0 (0.0) |
| Total number of complications | 15 | 4 | 0 |
| Characteristics | n (%) |
|---|---|
| TB type at the case registration | |
| New | 43 (53.1) |
| Retreatment | 38 (46.9) |
| Localization of TB disease | |
| Lung parenchyma (pulmonary) | 70 (86.4) |
| Pleural (only) | 11 (13.6) |
| Affected side | |
| Unilateral left | 40 (49.4) |
| Unilateral right | 35 (43.2) |
| Bilateral | 6 (7.4) |
| Presence of cavity before surgery | |
| Yes | 35 (43.2) |
| No | 46 (56.8) |
| Bacteriological confirmation after surgery | |
| Yes | 70 (86.4) |
| No | 11 (13.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riskiyev, A.; Ciobanu, A.; Hovhannesyan, A.; Akopyan, K.; Gadoev, J.; Parpieva, N. Characteristics and Treatment Outcomes of Patients with Tuberculosis Receiving Adjunctive Surgery in Uzbekistan. Int. J. Environ. Res. Public Health 2021, 18, 6541. https://doi.org/10.3390/ijerph18126541
Riskiyev A, Ciobanu A, Hovhannesyan A, Akopyan K, Gadoev J, Parpieva N. Characteristics and Treatment Outcomes of Patients with Tuberculosis Receiving Adjunctive Surgery in Uzbekistan. International Journal of Environmental Research and Public Health. 2021; 18(12):6541. https://doi.org/10.3390/ijerph18126541
Chicago/Turabian StyleRiskiyev, Anvar, Ana Ciobanu, Arax Hovhannesyan, Kristina Akopyan, Jamshid Gadoev, and Nargiza Parpieva. 2021. "Characteristics and Treatment Outcomes of Patients with Tuberculosis Receiving Adjunctive Surgery in Uzbekistan" International Journal of Environmental Research and Public Health 18, no. 12: 6541. https://doi.org/10.3390/ijerph18126541
APA StyleRiskiyev, A., Ciobanu, A., Hovhannesyan, A., Akopyan, K., Gadoev, J., & Parpieva, N. (2021). Characteristics and Treatment Outcomes of Patients with Tuberculosis Receiving Adjunctive Surgery in Uzbekistan. International Journal of Environmental Research and Public Health, 18(12), 6541. https://doi.org/10.3390/ijerph18126541









