Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review
Abstract
1. Introduction
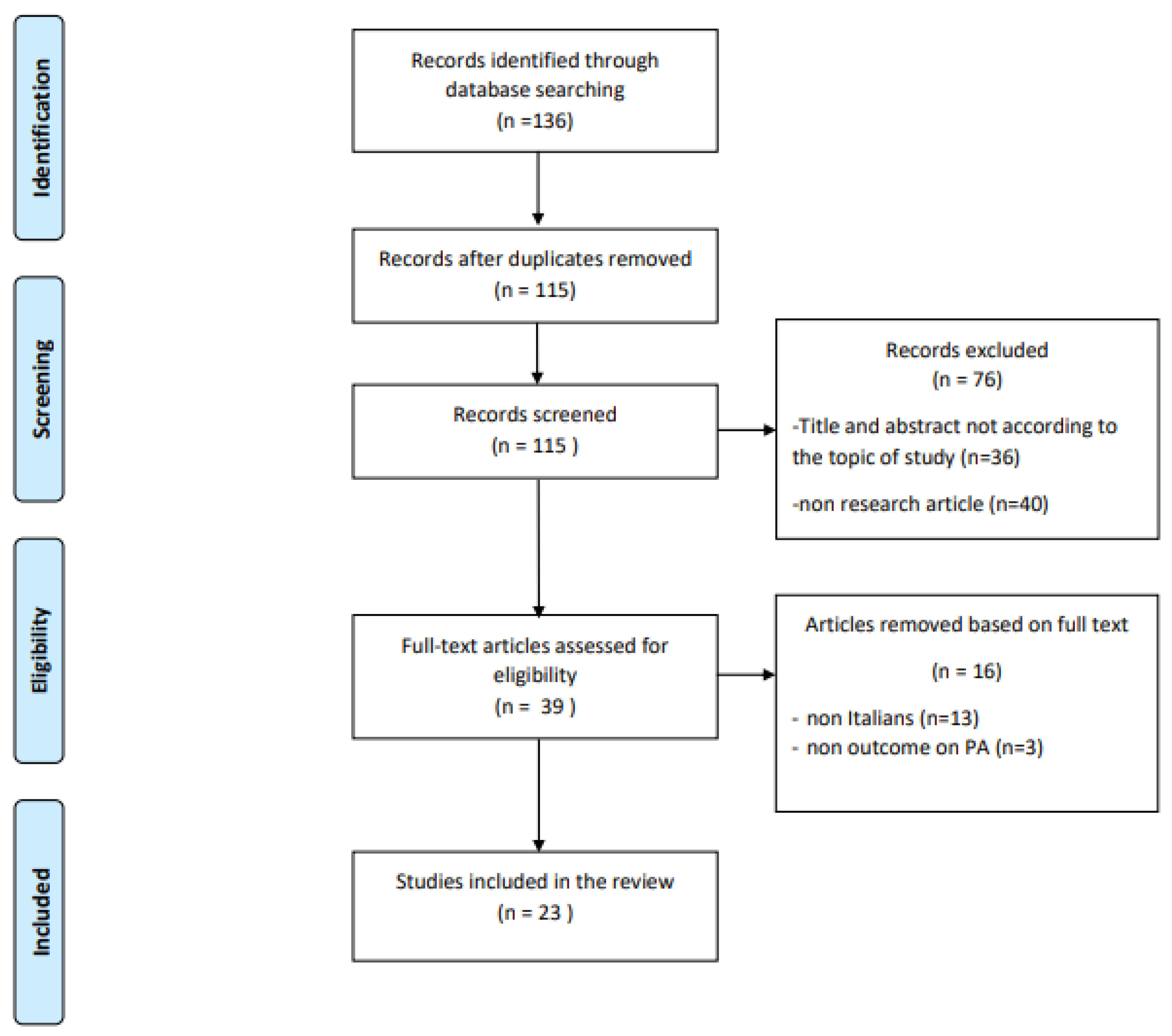
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bohn, B.; Herbst, A.; Pfeifer, M.; Krakow, D.; Zimny, S.; Kopp, F.; Melmer, A.; Steinacker, J.M.; Holl, R.W. DPV Initiative. Impact of Physical Activity on Glycemic Control and Prevalence of Cardiovascular Risk Factors in Adults With Type 1 Diabetes: A Cross-sectional Multicenter Study of 18,028 Patients. Diabetes Care. 2015, 38, 1536–1543. [Google Scholar] [CrossRef] [PubMed]
- Riddell, M.C.; Gallen, I.W.; Smart, C.E.; Taplin, C.E.; Adolfsson, P.; Lumb, A.N.; Kowalski, A.; Rabasa-Lhoret, R.; McCrimmon, R.J.; Hume, C.; et al. Exercise management in type 1 diabetes: A consensus statement. Lancet Diabetes Endocrinol. 2017, 5, 377–390. [Google Scholar] [CrossRef]
- Gielen, S.; Laughlin, M.H.; O’Conner, C.; Duncker, D.J. Exercise training in patients with heart disease: Review of beneficial effects and clinical recommendations. Prog. Cardiovasc. Dis. 2015, 57, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Ai, D.; Zhang, N. Exercise Benefits Coronary Heart Disease. Adv. Exp. Med. Biol. 2017, 1000, 3–7. [Google Scholar] [PubMed]
- Anziska, Y.; Inan, S. Exercise in neuromuscular disease. Semin. Neurol. 2014, 34, 542–556. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.L.; Lee, M.; Huang, T.T. Effectiveness of physical activity on patients with depression and Parkinson’s disease: A systematic review. PLoS ONE 2017, 27, e0181515. [Google Scholar] [CrossRef]
- Lauzé, M.; Daneault, J.F.; Duval, C. The Effects of Physical Activity in Parkinson’s Disease: A Review. J. Parkinsons Dis. 2016, 19, 685–698. [Google Scholar] [CrossRef]
- Duggal, N.A.; Niemiro, G.; Harridge, S.; Simpson, R.J.; Lord, J.M. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat. Rev. Immunol. 2019, 19, 563–572. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non Randomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2009. [Google Scholar]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G.; ESH Working Group on CV Risk in Low Resource Settings. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef]
- Assaloni, R.; Pellino, V.C.; Puci, M.V.; Ferraro, O.E.; Lovecchio, N.; Girelli, A.; Vandoni, M. Coronavirus disease (Covid-19): How does the exercise practice in active people with type 1 diabetes change? A preliminary survey. Diabetes Res. Clin. Pract. 2020, 166, 108297. [Google Scholar] [CrossRef] [PubMed]
- Barchetta, I.; Cimini, F.A.; Bertoccini, L.; Ceccarelli, V.; Spaccarotella, M.; Baroni, M.G.; Cavallo, M.G. Effects of work status changes and perceived stress on glycaemic control in individuals with type 1 diabetes during COVID-19 lockdown in Italy. Diabetes Res. Clin. Pract. 2020, 170, 108513. [Google Scholar] [CrossRef] [PubMed]
- Capaldo, B.; Annuzzi, G.; Creanza, A.; Giglio, C.; De Angelis, R.; Lupoli, R.; Masulli, M.; Riccardi, G.; Rivellese, A.A.; Bozzetto, L. Blood Glucose Control During Lockdown for COVID-19: CGM Metrics in Italian Adults With Type 1 Diabetes. Diabetes Care 2020, 43, e88–e89. [Google Scholar] [CrossRef]
- Caruso, I.; Di Molfetta, S.; Guarini, F.; Giordano, F.; Cignarelli, A.; Natalicchio, A.; Perrini, S.; Leonardini, A.; Giorgino, F.; Laviola, L. Reduction of hypoglycaemia, lifestyle modifications and psychological distress during lockdown following SARS-CoV-2 outbreak in type 1 diabetes. Diabetes Metab. Res. Rev. 2020, e3404. [Google Scholar] [CrossRef] [PubMed]
- Predieri, B.; Leo, F.; Candia, F.; Lucaccioni, L.; Madeo, S.F.; Pugliese, M.; Vivaccia, V.; Bruzzi, P.; Iughetti, L. Glycemic Control Improvement in Italian Children and Adolescents With Type 1 Diabetes Followed Through Telemedicine During Lockdown Due to the COVID-19 Pandemic. Front. Endocrinol. 2020, 11, 595735. [Google Scholar] [CrossRef] [PubMed]
- Tornese, G.; Ceconi, V.; Monasta, L.; Carletti, C.; Faleschini, E.; Barbi, E. Glycemic Control in Type 1 Diabetes Mellitus During COVID-19 Quarantine and the Role of In-Home Physical Activity. Diabetes Technol Ther. 2020, 22, 462–467. [Google Scholar] [CrossRef]
- Di Stefano, V.; Battaglia, G.; Giustino, V.; Gagliardo, A.; D’Aleo, M.; Giannini, O.; Palma, A.; Brighina, F. Significant reduction of physical activity in patients with neuromuscular disease during COVID-19 pandemic: The long-term consequences of quarantine. J. Neurol. 2021, 268, 20–26. [Google Scholar] [CrossRef]
- Pellegrini, M.; Ponzo, V.; Rosato, R.; Scumaci, E.; Goitre, I.; Benso, A.; Belcastro, S.; Crespi, C.; De Michieli, F.; Ghigo, E.; et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients 2020, 12, 2016. [Google Scholar] [CrossRef]
- Sassone, B.; Mandini, S.; Grazzi, G.; Mazzoni, G.; Myers, J.; Pasanisi, G. Impact of COVID-19 Pandemic on Physical Activity in Patients With Implantable Cardioverter-Defibrillators. J. Cardiopulm. Rehabil. Prev. 2020, 40, 285–286. [Google Scholar] [CrossRef]
- Schirinzi, T.; Di Lazzaro, G.; Salimei, C.; Cerroni, R.; Liguori, C.; Scalise, S.; Alwardat, M.; Mercuri, N.B.; Pierantozzi, M.; Stefani, A.; et al. Physical activity changes and correlate effects in patients with Parkinson’s disease during COVID-19 lockdown. Mov. Disord. Clin. Pract. 2020, 7, 797–802. [Google Scholar] [CrossRef]
- Barrea, L.; Pugliese, G.; Framondi, L.; Di Matteo, R.; Laudisio, D.; Savastano, S.; Colao, A.; Muscogiuri, G. Does Sars-Cov-2 threaten our dreams? Effect of quarantine on sleep quality and body mass index. J. Transl. Med. 2020, 18, 318. [Google Scholar] [CrossRef]
- Buoite Stella, A.; AjČeviĆ, M.; Furlanis, G.; Cillotto, T.; Menichelli, A.; Accardo, A.; Manganotti, P. Smart technology for physical activity and health assessment during COVID-19 lockdown. J. Sports Med. Phys. Fitness. 2021, 61, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Cancello, R.; Soranna, D.; Zambra, G.; Zambon, A.; Invitti, C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int J. Environ. Res. Public Health 2020, 17, 6287. [Google Scholar] [CrossRef] [PubMed]
- Di Corrado, D.; Magnano, P.; Muzii, B.; Coco, M.; Guarnera, M.; De Lucia, S.; Maldonato, N.M. Effects of social distancing on psychological state and physical activity routines during the COVID-19 pandemic. Sport Sci. Health 2020, 1–6. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, G.; Camussi, E.; Piccinelli, C.; Senore, C.; Armaroli, P.; Ortale, A.; Garena, F.; Giordano, L. Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens?. L’isolamento sociale durante l’epidemia da SARS-CoV-2 ha avuto un impatto sugli stili di vita dei cittadini? Epidemiol. Prev. 2020, 44 (Suppl. S2), 353–362. [Google Scholar] [PubMed]
- Gallè, F.; Sabella, E.A.; Da Molin, G.; De Giglio, O.; Caggiano, G.; Di Onofrio, V.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; Orsi, G.B.; et al. Understanding Knowledge and Behaviors Related to CoViD-19 Epidemic in Italian Undergraduate Students: The EPICO Study. Int J. Environ. Res. Public Health 2020, 17, 3481. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Ferracuti, S.; De Giglio, O.; Caggiano, G.; Protano, C.; Valeriani, F.; Parisi, E.A.; Valerio, G.; Liguori, G.; et al. Sedentary Behaviors and Physical Activity of Italian Undergraduate Students during Lockdown at the Time of CoViD-19 Pandemic. Int J. Environ. Res. Public Health 2020, 17, 6171. [Google Scholar] [CrossRef]
- Giustino, V.; Parroco, A.M.; Gennaro, A.; Musumeci, G.; Palma, A.; Battaglia, G. Physical activity levels and related energy expenditure during COVID-19 quarantine among the sicilian active population: A cross-sectional online survey study. Sustainability 2020, 12, 4356. [Google Scholar] [CrossRef]
- Luciano, F.; Cenacchi, V.; Vegro, V.; Pavei, G. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. Eur. J. Sport Sci. 2020, 1–10. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Raiola, G.; Aliberti, S.; Esposito, G.; Altavilla, G.; D’Isanto, T.; D’Elia, F. How has the practice of physical activity changed during the covid-19 quarantine? a preliminary survey. Teor. Metod. Fiz. Vihov. 2020, 20, 242–247. [Google Scholar] [CrossRef]
- Tornaghi, M.; Lovecchio, N.; Vandoni, M.; Chirico, A.; Codella, R. Physical activity levels across COVID-19 outbreak in youngsters of Northwestern Lombardy. J. Sports Med. Phys. Fitness 2020. [Google Scholar] [CrossRef]
- Chirico, A.; Lucidi, F.; Galli, F.; Giancamilli, F.; Vitale, J.; Borghi, S.; La Torre, A.; Codella, R. COVID-19 Outbreak and Physical Activity in the Italian Population: A Cross-Sectional Analysis of the Underlying Psychosocial Mechanisms. Front. Psychol. 2020, 11, 2100. [Google Scholar] [CrossRef]
- Hart, P.H.; Gorman, S.; Finlay-Jones, J.J. Modulation of the immune system by UV radiation: More than just the effects of vitamin D? Nat. Rev. Immunol. 2011, 19, 584–596. [Google Scholar] [CrossRef] [PubMed]
- Dewan, S.K.; Zheng, S.B.; Xia, S.J.; Bill, K. Senescent remodeling of the immune system and its contribution to the predisposition of the elderly to infections. Chin. Med. J. 2012, 125, 3325–3331. [Google Scholar] [PubMed]
- Simpson, R.J.; Lowder, T.W.; Spielmann, G.; Bigley, A.B.; LaVoy, E.C.; Kunz, H. Exercise and the aging immune system. Ageing Res. Rev. 2012, 11, 404–420. [Google Scholar] [CrossRef]
- Sharif, K.; Watad, A.; Bragazzi, N.L.; Lichtbroun, M.; Amital, H.; Shoenfeld, Y. Physical activity and autoimmune diseases: Get moving and manage the disease. Autoimmun. Rev. 2018, 17, 53–72. [Google Scholar] [CrossRef]
| Samples with Pathologies | Focus | Study Design | Sample, Pathology, Size, Age, % Males | PA Assessment Tool Survey Type | Amount of PA (Mean ± SD) | Main Findings |
|---|---|---|---|---|---|---|
| Assaloni et al. [12] | PA level in diabetes | Observational, cross-sectional | N = 154 T1D 44.8 ± 12.5 y, 54.5% males | Godin Leisure Time Exercise Q. online survey | Before L: 66 ± 42 min During L: 38 ± 31 min | PA decreased with worst glycaemia |
| Barchetta et al. [13] | Glycemic control in diabetes | Observational, cross-sectional | N = 50 T1D, 40.7 ± 13.5 y, 62% males | Q not validated Online survey | NR | Reduction of blood glucose control and weekly PA |
| Capaldo et al. [14] | Glucose control in diabetes | Observational, cross-sectional | N = 207 T1D 38.4 ± 12.7 y, 53.6% males | Q not validated Online survey | NR | Increased glycemic control, more regular meals, reduced PA |
| Caruso et al. [15] | Glucose control in diabetes | Observational, cross-sectional | N = 48 T1D 42.4 ± 15.9 y, 52.1% males | Q not validated Phone interview | NR | Increased glycemic control, reduced PA |
| Predieri et al. [16] | Glycemic control in diabetes | Observational, longitudinal | N = 62 T1D 11.1 ± 4.4 y, 50% males | Q not validated telemedicine | Before L: 3.27 ± 2.82 h/w During L: 0.24 ± 0.59 h/w | Decreased PA, improved glycemic control |
| Tornese et al. [17] | Glycemic control in diabetes | Observational, cross-sectional | N = 13 T1D median age = 14.2 y, 61.5% males | Q not validated telemedicine | During L: 3.3 h/w | Regular PA at home improved glycemic control |
| Di Stefano et al. [18] | Levels of PA in neuromuscular diseases (NMD) | Observational, cross-sectional | N = 268, 149 NMD patients (57.3 ± 13.7 y, 62.4% males), 119 controls (56 ± 6.8 y, 62.2% males) | IPAQ-SF Phone interview | NMD Before L: 901.3 ± 1299.6 During L: 400.6 ± 1088.5 Controls Before L: 4506.5 ± 7600.1 During L: 2362.3 ± 4498.9 | Significantly decrease of PA in both groups |
| Pellegrini et al. [19] | Changes in weight and diet in obesity | Observational, cross-sectional | N = 150 obese, aged 47.9 ± 16.0, 22% males | Q not validated | Significant weight increase, reduction in PA | |
| Sassone et al. [20] | Changes in PA in patients with implantable Cardioverter-defibrillators | Observational, cross-sectional | N = 24 cardiac patients, 72 ± 10 y, 70.8% males | Accelerometric sensors- collected data | Before L: 1.6 ± 0.5 h/day During L: 1.2 ± 0.3 h/day | Significant reduction in PA |
| Schirinzi et al. [21] | Changes in PA in Parkinson disease | Observational, cross-sectional | N = 74 Parkinson disease 61.3 ± 9.3 y, 50% males | IPAQ-SF Online survey | During L: 1994.7 ± 1971 MET-min/w | 60% of patients worsened, performing less PA |
| Sample without pathologies | Focus | Study design | Sample size, age, % males | PA assessment tool Survey type | Amount of PA (mean ± SD) | Main findings |
| Barrea et al. [22] | Sleep quality, Body mass index | Observational, cross-sectional | N = 121 44.9 ± 13.3 y, 35.5% males | Q not validated phone interview | NR | Significant increase in mean body weight and BMI, significant decrease in PA |
| Buoite Stella et al. [23] | Smart technologies for PA | Observational, cross-sectional | N = 400 35 ± 15 y, 31% males | Online survey IPAQ-SF; daily step count measured by smart devices | Before L: 3101 ± 3815 METs During L: 1839 ± 2254 METs | Significant reduction of performed steps and PA |
| Cancello et al. [24] | Lifestyle changes during lockdown | Observational, cross-sectional | N = 490 adults 16% males | Q not validated online survey | NR | Reduction of PA in active individuals, inception of PA in sedentary individuals |
| Di Corrado et al. [25] | Psychological status, PA | Observational, cross-sectional | N = 679 33.4 ± 12.8 y, 51% males | Q not validated Online survey | NR | Maintained or increased PA significantly |
| Di Renzo et al. [26] | Eating habits and lifestyle changes | Observational, cross-sectional | N = 3533 aged 12–86 23.9% males | Q not validated Online survey | NR | No significant difference in PA among inactive subjects, increase in PA in subjects who used to train more than 5 times a week |
| Ferrante et al. [27] | Impact of social isolation on lifestyle | Observational, cross-sectional | N = 7847 48.6 ± 13.9 y, 28.7% males | Q not validated Online survey | NR | Significant decrease in PA |
| Gallè et al. [28] | Sedentary behaviors and PA | Observational, cross-sectional | N = 1430 undergraduate students, 22.9 ± 4.5 y, 34.5% males | IPAQ-SF Online survey | Before L: 520 ± 820 min/w During L: 270 ± 340 min/w | Significantly increased sedentary lifestyle, decreased PA |
| Gallè et al. [29] | Health-related behaviors PA | Observational, cross-sectional | N = 2125 undergraduate students, 22.5 ± 0.08 y, 37.2% males | Questionnaire online survey | NR | Significant reduction in PA |
| Giustino et al. [30] | Level of PA | Observational, cross-sectional | N = 802, 32.27 ± 12.81 y, 49% males | IPAQ-SF online survey | Before L: 3006 MET-min/w During L: 1483.8 MET-min/w | Significant reduction of PA, especially in males and in overweight |
| Luciano et al. [31] | Behaviors during lockdown (PA, sedentariness, sleep) | Observational, cross-sectional | N = 1471 medicine students 23 ± 2 y, 30% males | IPAQ-SF online survey | Before L: 1588 MET-min/w During L: 960 MET-min/w | Decreased PA, and increased sitting and sleep time |
| Maugeri et al. [32] | PA on psychological | Observational, cross-sectional | N = 2524 43.6% males | IPAQ Online survey | Before L: 2429 MET-min/w During L: 1577 MET-min/w | PA level decreased with negative impact on psychological health |
| Raiola et al. [33] | Changes in PA | Observational, cross-sectional | N = 268 Mean age = 26 y | Q not validated Online survey | NR | No change in PA |
| Tornaghi et al. [34] | PA levels | Observational, cross-sectional | N = 1568 students Aged 15–18 | IPAQ Online survey | Before L: 1676.37 ± 20.6 MET-min/w After L: 1774.50 ± 33.93 MET-min/w | Inactive or moderately active students unchanged their PA level; highly active ones increased PA level |
| REFERENCE | Representativeness of Sample | Sample Size | Non-Respondents | Ascertainment of the Exposure | Comparability | Assessment of the Outcome | Statistics | NOS Score |
|---|---|---|---|---|---|---|---|---|
| Assaloni et al. [12] | 1 | 0 | 0 | 2 | 0 | 1 | 1 | 6 |
| Barchetta et al. [13] | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Barrea et al. [22] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 5 |
| Buoite Stella et al. [23] | 1 | 0 | 0 | 2 | 0 | 1 | 1 | 5 |
| Cancello et al. [24] | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Capaldo et al. [14] | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| Caruso et al. [15] | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Di Corrado et al. [25] | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Di Renzo et al. [26] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Di Stefano et al. [18] | 1 | 0 | 0 | 2 | 1 | 1 | 1 | 6 |
| Ferrante et al. [27] | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 8 |
| Gallè et al. [28] | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 6 |
| Gallè et al. [29] | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 6 |
| Giustino et al. [30] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 5 |
| Luciano et al. [31] | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 6 |
| Maugeri et al. [32] | 1 | 0 | 0 | 2 | 0 | 1 | 1 | 5 |
| Pellegrini et al. [19] | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Predieri et al. [16] | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 4 |
| Raiola et al. [33] | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 5 |
| Sassone et al. [20] | 1 | 0 | 0 | 2 | 0 | 2 | 1 | 6 |
| Schirinzi et al. [21] | 1 | 0 | 0 | 2 | 0 | 1 | 1 | 5 |
| Tornaghi et al. [34] | 1 | 0 | 0 | 2 | 1 | 1 | 1 | 6 |
| Tornese et al. [17] | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaccagni, L.; Toselli, S.; Barbieri, D. Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6416. https://doi.org/10.3390/ijerph18126416
Zaccagni L, Toselli S, Barbieri D. Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(12):6416. https://doi.org/10.3390/ijerph18126416
Chicago/Turabian StyleZaccagni, Luciana, Stefania Toselli, and Davide Barbieri. 2021. "Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 12: 6416. https://doi.org/10.3390/ijerph18126416
APA StyleZaccagni, L., Toselli, S., & Barbieri, D. (2021). Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. International Journal of Environmental Research and Public Health, 18(12), 6416. https://doi.org/10.3390/ijerph18126416








