Effects of a Modified Tap Dance Program on Ankle Function and Postural Control in Older Adults: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Aim
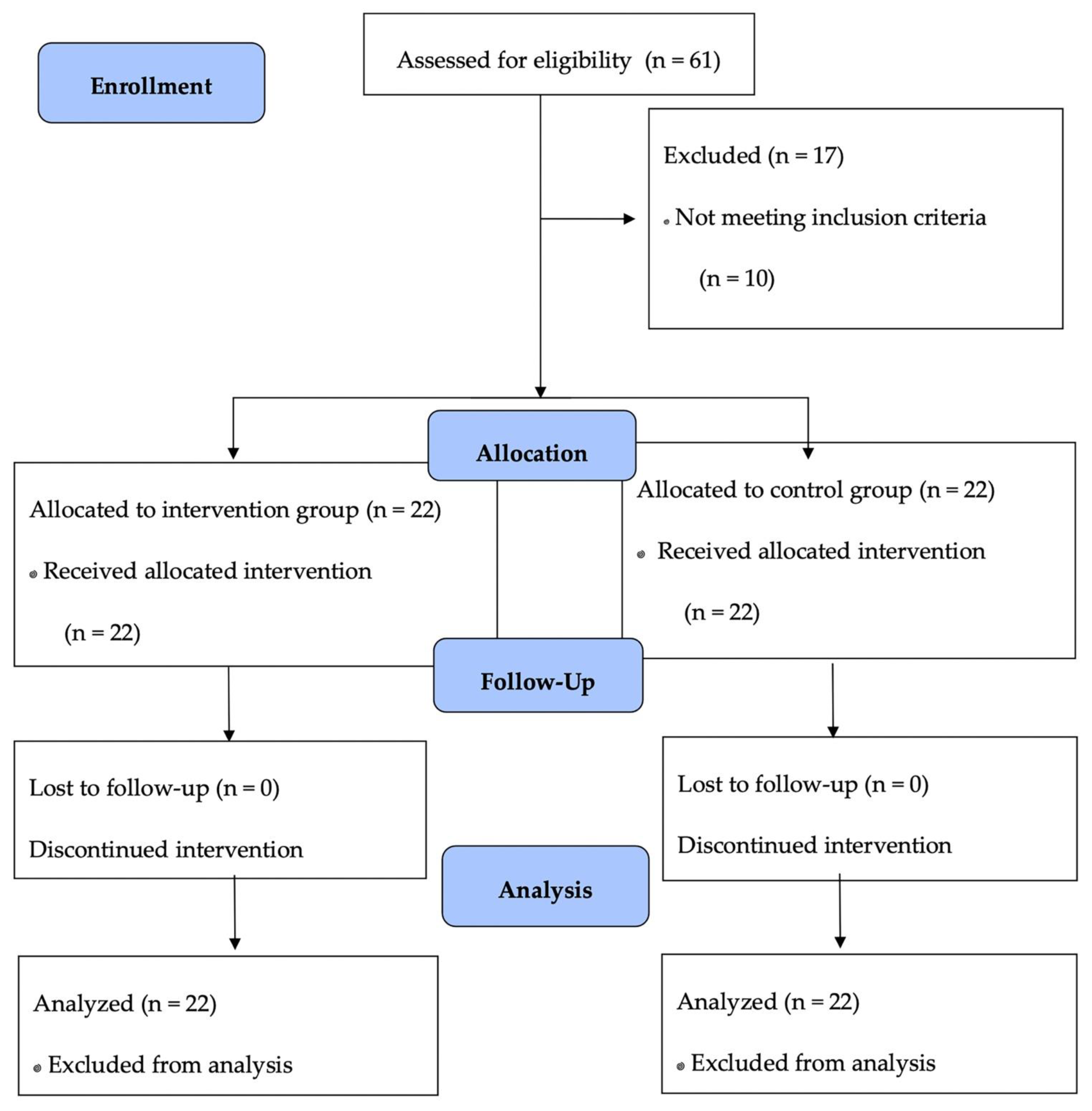
2.2. Trial Design
2.3. Participants
2.4. Intervention
2.5. Outcomes
2.5.1. Ankle Function
- Muscle strength: Ankle strength was evaluated using the five times sit-to-stand (FTSST) test. Participants were asked to perform five rises from a 43 cm-high chair as fast as possible with arms crossed over the chest. The total duration was recorded in seconds. To gain familiarity with the test procedure, each participant practiced twice before the formal test. The test–retest reliability of the FTSST is well accepted (ICC = 0.89, 95%CI = 0.79–0.95), and it has been used as a valid test for ankle muscle strength in dorsiflexion [24] and plantar flexion (R2 = 0.72) [25].
- Range of motion (ROM): A standard universal goniometer (XuBin Medical Equipment Company, Handan, China) was used to measure ankle ROM during active plantar flexion and dorsiflexion on both sides; i.e., left ankle dorsiflexion (LD-ROM), left ankle plantar flexion (LP-ROM), right ankle dorsiflexion (RD-ROM), and right ankle plantar flexion (RP-ROM). Participants were asked to sit on a treatment table with their knees fully extended (at 0°) and their feet hanging off the table. During the test, participants had to be completely relaxed, actively moving the ankle into dorsiflexion or plantar flexion from a neutral starting position until a firm end-feel was elicited. The goniometer axis was centered on the lateral malleolus, and the arms were aligned with the fibular shaft and the head of the fifth metatarsal. Each test was repeated twice, and the best score was recorded.
2.5.2. Postural Control
- The Footscan® (RSscan, Footscan Balance, Version 7, Olen, Belgium) was applied to measure the sway of the COP in a stance. Participants were instructed to stand barefoot on the platform with hands touching their hips and eyes looking straight ahead or closed. Each participant was tested twice with 30 s rest intervals during the following three tests [26]: Test 1: standing with hands touching hips, feet together, and looking straight ahead; Test 2: standing with hands touching hips and eyes closed; Test 3: tandem stance (toes of the left foot touching the right heel) with hands touching hips, looking straight ahead. Each test lasted 33 s. The test was stopped if a participant’s foot left the floor.
2.6. Randomization
2.7. Sample Size
2.8. Data Analysis
2.9. Ethical Approval
2.10. Trial Registration
3. Results
3.1. Ankle Function
3.2. Postural Control
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Milanović, Z.; Pantelić, S.; Trajković, N.; Sporiš, G.; Kostić, R.; James, N. Age-related Decrease in Physical Activity and Functional Fitness Among Elderly Men and Women. Clin. Interv. Aging 2013, 8, 549–556. [Google Scholar] [CrossRef]
- World Health Organization. Available online: http://www.who.int/mediacentre/factsheets/fs344/en/ (accessed on 21 April 2021).
- Tromp, A.M.; Smit, J.H.; Deeg, D.J.H.; Bouter, L.M.; Lips, P. Predictors for Falls and Fractures in the Longitudinal Aging Study Amsterdam. J. Bone Miner. Res. 1998, 13, 1932–1939. [Google Scholar] [CrossRef]
- Ito, T.; Sakai, Y.; Nishio, R.; Ito, Y.; Morita, Y. Relationship between Postural Stability and Fall Risk in Elderly People with Lumbar Spondylosis during Local Vibratory Stimulation for Proprioception: A Retrospective Study. Somatosens. Mot. Res. 2020, 1–5. [Google Scholar] [CrossRef]
- Jehu, D.; Paquet, N.; Lajoie, Y. Balance and Mobility Training with or without Concurrent Cognitive Training does not Improve Posture.; but Improves Reaction Time in Healthy Older Adults. Gait Posture 2017, 52, 227–232. [Google Scholar] [CrossRef]
- Ni, M.; Mooney, K.; Richards, L.; Balachandran, A.; Sun, M.W. Comparative Impacts of Tai Chi, Balance Training and a Specially Designed Yoga Program on Balance in Older Fallers. Arch. Phys. Med. Rehabil. 2014, 95, 1620–1628. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Barbosa, F.; Pozo-Cruz, J.D.; Pozo-Cruz, B.; Alfonso-Rosa, R.M.; Rogers, M.E.; Zhang, Y. Effects of Supervised Whole Body Vibration Exercise on Fall Risk Factors, Functional Dependence and Health-Related Quality of Life in Nursing Home Residents Aged 80+. Maturitas 2014, 79, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Donath, L.; Faude, O.; And, R.R.; Zahner, L. Effects of Stair-Climbing on Balance, Gait, Strength, Resting Heart Rate, and Submaximal Endurance in Healthy Seniors. Scand. J. Med. Sci. Sports 2014, 24, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Hrysomallis, C. Balance Ability and Athletic Performance. Sports Med. 2011, 41, 221–232. [Google Scholar] [CrossRef]
- Hortobágyi, T.; Lesinski, M.; Gäbler, M.; Vanswearingen, J.M.; Malatesta, D.; Granacher, U. Effects of Three Types of Exercise Interventions on Healthy Old Adults’ Gait Speed: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 1627–1643. [Google Scholar] [CrossRef] [PubMed]
- Low, D.C.; Walsh, G.S.; Arkesteijn, M. Effectiveness of Exercise Interventions to Improve Postural Control in Older Adults: A Systematic Review and Meta-Analyses of Center of Pressure Measurements. Sports Med. 2017, 47, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Oddsson, L.I.E.; Boissy, P.; Melzer, I. How to Improve Gait and Balance Function in Elderly Individuals: Compliance with Principles of Training. Eur. Rev. Aging Phys. A 2007, 4, 15–23. [Google Scholar] [CrossRef]
- Horak, F.B.; Shupert, C.L.; Mirka, A. Components of Postural Dyscontrol in the Elderly: Review. Neurobiol. Aging 1989, 10, 727–738. [Google Scholar] [CrossRef]
- Góes, S.M.; Leite, N.; Stefanello, J.M.; Homann, D.; Rodacki, A.L.F. Ankle Dorsiflexion May Play an Important Role in Falls in Women with Fibromyalgia. Clin. Biomech. 2015, 30, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Pijnappels, M.; van der Burg Petra, J.C.E.; Reeves, N.D.; Dien, J.H. Identification of Elderly Fallers by Muscle Strength Measures. Eur. J. Appl. Physiol. 2008, 102, 585–592. [Google Scholar] [CrossRef]
- Mecagni, C.; Smith, J.P.; Roberts, K.E.; O’Sullivan, S.B. Balance and Ankle Range of Motion in Community-Dwelling Women Aged 64 to 87 Years: A Correlational Study. Phys. Ther. 2000, 80, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Schwenk, M.; Jordan, D.H.; Honarvararaghi, B.; Mohler, J.; Armstrong, D.G.; Najafi, B. Effectiveness of Foot and Ankle Exercise Programs on Reducing the Risk of Falling in Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Podiatr. Med. Assoc. 2013, 103, 534–547. [Google Scholar] [CrossRef]
- Hwang, W.N.; Braun, K.L. The Effectiveness of Dance Interventions to Improve Older Adults’ Health: A Systematic Literature Review. Altern. Ther. Health Med. 2015, 21, 64–70. [Google Scholar] [PubMed]
- Fernández-Argüelles, E.L.; Rodríguez-Mansilla, J.; Antunez, L.E.; Garrido-Ardila, E.M.; Muñoz, R.P. Effects of Dancing on the Risk of Falling Related Factors of Healthy Older Adults: A Systematic Review. Arch. Gerontol. Geriat. 2015, 60, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Patti, A.; Bellafiore, M.; Battaglia, G.; Sahin, F.N.; Paoli, A. Group Fitness Activities For The Elderly: An Innovative Approach To Reduce Falls And Injuries. Aging Clin. Exp. Res. 2014, 26, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.W.; Zhao, Y.N. A Pilot Design for a Modified Tap Dance Program for Ankle Function Improvement and Fall Prevention. J. Phys. Act. Res. 2019, 4, 67–72. [Google Scholar] [CrossRef]
- Zhao, Y.; Cai, K.; Wang, Q.; Hu, Y.; Gao, H. Effect of Tap Dance on Plantar Pressure, Postural Stability and Lower Body Function in Older Patients at Risk of Diabetic Foot: A Randomized Controlled Trial. BMJ Open Diabetes Res. Care 2021, 9, 1909. [Google Scholar] [CrossRef] [PubMed]
- Fitts, P.M.; Posner, M.I. Human Performance; Brooks/Cole Publishing Company: Belmont, CA, USA, 1967. [Google Scholar]
- Lord, S.R.; Murray, S.M.; Kirsten, C.; Bridget, M.; Anne, T. Sit-to-stand Performance Depends on Sensation, Speed, Balance, and Psychological Status in Addition to Strength in Older People. J. Gerontol. A Biol. 2002, 57, M539–M543. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, E.K.; Horvat, M.A.; Holtsberg, P.A.; Wisenbaker, J.M. Repeated Chair Stands as A Measure of Lower Limb Strength in Sexagenarian Women. J. Gerontol. A Biol. 2004, 59, 1207–1212. [Google Scholar] [CrossRef] [PubMed]
- Czerwiński, E.; Borowy, P.; Jasiak, B. Current Guidelines for Using Physiotherapy to Prevent Falls. Ortop. Traumatol. Rehabil. 2006, 8, 380–387. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Gatev, P.; Thomas, S.; Kepple, T.; Hallett, M. Feedforward Ankle Strategy of Balance during Quiet Stance in Adults. J. Physiol. 1999, 514, 915–928. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B. The Loss of Skeletal Muscle Strength, Mass, and Quality in Older Adults: The Health, Aging and Body Composition Study. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 6, 1059–1064. [Google Scholar] [CrossRef]
- Kutsuna, T.; Hiyama, Y.; Kusaka, S.; Kusumoto, Y.; Tsuchiya, J.; Umeda, M.; Takahashi, T. The Effect of Short-Term Health Promotion Intervention on Motor Function in Community-Dwelling Older Adults. Aging Clin. Exp. Res. 2019, 31, 475–481. [Google Scholar] [CrossRef]
- Benedetti, F. How the Doctor’s Words Affect the Patient’s Brain. Eval. Health Prof. 2002, 25, 369–388. [Google Scholar] [CrossRef]
- Becker, H.; Roberts, G.; Voelmeck, W. Explanations for Improvement in Both Experimental and Control Groups. West. J. Nurs. Res. 2003, 25, 746–755. [Google Scholar] [CrossRef]
- Justine, M.; Ruzali, D.; Hazidin, E.; Said, A.; Bukry, S.A.; Manaf, H. Range of Motion, Muscle Length, and Balance Performance in Older Adults with Normal, Pronated, and Supinated Feet. J. Phys Ther. Sci. 2016, 28, 916–922. [Google Scholar] [CrossRef]
- Lyu, B.J.; Lee, C.L.; Chang, W.D.; Chang, N.J. Effects of Vibration Rolling with and without Dynamic Muscle Contraction on Ankle Range of Motion, Proprioception, Muscle Strength and Agility in Young Adults: A Crossover Study. Int. J. Environ. Res. Public Health 2020, 17, 354. [Google Scholar] [CrossRef]
- Valverde-Guijarro, E.; Alguacil-Diego, I.M.; Vela-Desojo, L.; Cano-de-la-Cuerda, R. Effects of Contemporary Dance and Physiotherapy Intervention on Balance and Postural Control in Parkinson’s Disease. Disabil. Rehabil. 2020, 11, 1–8. [Google Scholar] [CrossRef]
- Bastug, G. Examination of Body Composition, Flexibility, Balance, and Concentration Related to Dance Exercise. Asia Pac. J. Educ. 2018, 4, 210–215. [Google Scholar] [CrossRef]
- Hackney, M.E.; Earhart, G.M. Effects of Dance on Movement Control in Parkinson’s Disease: A Comparison of Argentine Tango and American Ballroom. J. Rehabil. Med. 2009, 41, 475–481. [Google Scholar] [CrossRef]
- McNeely, M.E.; Duncan, R.P.; Earhart, G.M. A Comparison of Dance Interventions in People with Parkinson Disease and Older Adults. Maturitas 2015, 81, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Areeudomwong, P.; Saysalum, S.; Phuttanurattana, N.; Sripoom, P.; Buttagat, V.; Keawduangdee, P. Balance and Functional Fitness Benefits of a Thai Boxing Dance Program among Community-Dwelling Older Adults at Risk of Falling: A Randomized Controlled Study. Arch. Gerontol. Geriatr. 2019, 83, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Blain, H.; Dabas, F.; Mekhinini, S.; Picot, M.C.; Miot, S.; Bousquet, J.; Bernard, P.L. Effectiveness of A Programme Delivered in A Falls Clinic in Preventing Serious injuries in High-Risk Older Adults: A Pre-and Post-Intervention Study. Maturitas 2019, 122, 80–86. [Google Scholar] [CrossRef]
| Parameters | MTD (n = 22) | CON (n = 22) | All (n = 44) |
|---|---|---|---|
| Age (years) | 63.9 ± 4.21 | 64.6 ± 3.75 | 64.1 ± 4.02 |
| Female (%) | 18 (81.8%) | 17 (77.3%) | 35 (79.5%) |
| Height (cm) | 158 ± 5.47 | 160 ± 13.6 | 160 ± 8.16 |
| Body mass index (kg/m2) | 24.0 ± 2.80 | 26.5 ± 6.5 | 25.2 ± 3.09 |
| SBP (mmHg) | 124 ± 13.6 | 126 ± 21.5 | 127.9 ± 14.5 |
| DBP (mmHg) | 75.9 ± 8.71 | 74.9 ± 8.99 | 74.5 ± 9.16 |
| Tests | MTD (n = 22) | CON (n = 22) | Adjusted Difference (95% CI) * |
|---|---|---|---|
| Five times sit-to-stand test (s) | |||
| Pretest | 7.45 ± 1.51 | 8.49 ± 1.94 | |
| Midtest | 6.88 ± 1.06 | 8.39 ± 1.95 | −1.51 (−1.81, −0.14) ^ |
| Posttest | 6.44 ± 1.28 # | 7.05 ± 1.19 # | −0.61 (−0.98, 0.44) |
| Range of motion in left dorsiflexion (°) | |||
| Pretest | 14.2 ± 5.94 | 11.8 ± 5.62 | |
| Midtest | 13.2 ± 6.33 | 12.1 ± 7.74 | 1.10 (−3.72, 5.12) |
| Posttest | 10.4 ± 7.05 | 10.9 ± 5.51 | −0.50 (−4.45, 3.52) |
| Range of motion in left plantar flexion (°) | |||
| Pretest | 30.4 ± 5.96 | 30.2 ± 8.15 | |
| Midtest | 44.0 ± 4.83 # | 37.9 ± 8.27 # | 6.10 (2.04, 10.1) ^ |
| Posttest | 39.5 ± 7.22 # | 37.8 ± 5.88 # | 1.70 (−2.39, 5.67) |
| Range of motion in right dorsiflexion (°) | |||
| Pretest | 14.2 ± 6.91 | 14.5 ± 8.45 | |
| Midtest | 11.6 ± 5.81 | 12.5 ± 7.57 | −0.90 (−4.98, 3.25) |
| Posttest | 9.78 ± 6.02 # | 11.7 ± 5.75 | −1.92 (−5.53, 1.73) |
| Range of motion in right plantar flexion (°) | |||
| Pretest | 29.8 ± 6.37 | 30.4 ± 10.9 | |
| Midtest | 42.3 ± 5.86 # | 37.8 ± 6.01 # | 4.50 (1.14, 8.00) ^ |
| Posttest | 39.8 ± 7.15 # | 38.2 ± 5.36 # | 1.60 (−2.19, 5.55) |
| Tests | MTD | CON | Adjusted Difference 95% (CI) * |
|---|---|---|---|
| Test 1: Standing with both feet, eyes opened | |||
| Total travelled distance of center of pressure (mm) | |||
| Pretest | 105 ± 26.8 | 154 ± 62.6 | |
| Midtest | 127 ± 43.5 # | 185 ± 68.0 | −58.0 (−58.9, 7.08) |
| Posttest | 125 ± 47.2 | 185 ± 120 | −60.0 (−103, 20.9) |
| Ellipse area (mm2) | |||
| Pretest | 6.58 ± 5.13 | 8.23 ± 5.59 | |
| Midtest | 6.54 ± 4.05 | 11.1 ± 6.69 | −4.56 (−7.38, −0.77) ^ |
| Posttest | 7.40 ± 5.49 | 8.24 ± 4.77 | −0.84 (−2.83, 2.73) |
| Test 2: Standing with both feet, eyes closed | |||
| Total travelled distance of center of pressure (mm) | |||
| Pretest | 124 ± 32.6 | 175 ± 85.3 | |
| Midtest | 138 ± 56.9 | 171 ± 59.1 | −33.0 (−46.9, 22.6) |
| Posttest | 137 ± 62.8 | 184 ± 65.9 | −47.0 (−50.6, 18.2) |
| Ellipse area (mm2) | |||
| Pretest | 5.91 ± 4.26 | 7.48 ± 4.34 | |
| Midtest | 7.02 ± 5.09 | 9.85 ± 7.21 | −2.83 (−5.62, 1.65) |
| Posttest | 7.40 ± 6.21 | 9.56 ± 5.43 | −2.16 (−3.92, 2.06) |
| Test 3: Tandem stance with right foot forward, eyes opened | |||
| Total travelled distance of center of pressure (mm) | |||
| Pretest | 452 ± 223 | 526 ± 263 | |
| Midtest | 438 ± 153 | 487 ± 124 | −49.0 (−121, 45.8) |
| Posttest | 488 ± 149 | 490 ± 187 | −2.00 (−91.1, 113) |
| Ellipse area (mm2) | |||
| Pretest | 31.5 ± 73.7 | 16.0 ± 13.8 | |
| Midtest | 21.3 ± 10.6 | 21.5 ± 14.5 | 1.70 (−6.79, 8.50) |
| Posttest | 13.0 ± 11.9 | 15.7 ± 9.27 | −2.70 (−8.52, 4.54) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Zhao, Y. Effects of a Modified Tap Dance Program on Ankle Function and Postural Control in Older Adults: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 6379. https://doi.org/10.3390/ijerph18126379
Wang Q, Zhao Y. Effects of a Modified Tap Dance Program on Ankle Function and Postural Control in Older Adults: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(12):6379. https://doi.org/10.3390/ijerph18126379
Chicago/Turabian StyleWang, Qianwen, and Yanan Zhao. 2021. "Effects of a Modified Tap Dance Program on Ankle Function and Postural Control in Older Adults: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 12: 6379. https://doi.org/10.3390/ijerph18126379
APA StyleWang, Q., & Zhao, Y. (2021). Effects of a Modified Tap Dance Program on Ankle Function and Postural Control in Older Adults: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(12), 6379. https://doi.org/10.3390/ijerph18126379






