Subjective Feelings of Polish Doctors after Receiving the COVID-19 Vaccine
Abstract
1. Introduction
2. Materials and Methods
- How many doses of the vaccine have you taken?
- Did you take the vaccine voluntarily?
- Did you feel fear when you were vaccinated?
- Are you concerned about the negative effects of the vaccine?
- Did you need a doctor’s help after receiving the vaccine?
- Have you been hospitalized after receiving the vaccine?
- Have there been any post-vaccination reactions? (injection site pain, swelling, redness, fatigue, headache, muscle pain, joint pain, chills, fever, nausea).
- How do you rate the effectiveness of the vaccine you have received?
- Will taking the vaccine help to contain the pandemic?
- Are you afraid of getting infected with COVID-19?
- Are you afraid of infection and illness of someone close to you?
- Did any of your family have COVID-19?
- Did any of your family die from COVID-19?
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Bartsch, S.M.; O’Shea, K.J.; Wedlock, P.T.; Strych, U.; Ferguson, M.C.; Bottazzi, M.E.; Randall, S.L.; Siegmund, S.S.; Cox, S.N.; Hotez, P.J.; et al. The Benefits of Vaccinating With the First Available COVID-19 Coronavirus Vaccine. Am. J. Prev. Med. 2021, 60, 605–613. [Google Scholar] [CrossRef]
- Mortensen, C.R.; Becker, D.V.; Ackerman, J.M.; Neuberg, S.L.; Kenrick, D.T. Infection Breeds Reticence. Psychol. Sci. 2010, 21, 440–447. [Google Scholar] [CrossRef]
- Schaller, M. Parasites, behavioral defenses, and the social psychological mechanisms through which cultures are evoked. Psychol. Inq. 2006, 17, 96–101. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Sahebi, A.; Nejati-Zarnaqi, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110247. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Wen, X.; Dong, Y.; Liu, B.; Cui, M. Psychological Influence of Coronovirus Disease 2019 (COVID-19) Pandemic on the General Public, Medical Workers, and Patients With Mental Disorders and its Countermeasures. Psychosomatics 2020, 61, 616–624. [Google Scholar] [CrossRef]
- Tan, B.Y.; Kanneganti, A.; Lim, L.J.; Tan, M.; Chua, Y.X.; Tan, L.; Sia, C.H.; Denning, M.; Goh, E.T.; Purkayastha, S.; et al. Burnout and Associated Factors Among Health Care Workers in Singapore During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 1751–1758. [Google Scholar] [CrossRef]
- Jurczyński, Z. Narzędzia pomiaru w psychologii. Kardiochirurgia Torakochirurgia Polska Pol. J. Cardio-Thorac. 1999, 42, 43–56. [Google Scholar]
- Fauzi, M.F.M.; Yusoff, H.M.; Robat, R.M.; Saruan, N.A.M.; Ismail, K.I.; Haris, A.F.M. Doctors’ Mental Health in the Midst of COVID-19 Pandemic: The Roles of Work Demands and Recovery Experiences. Int. J. Environ. Res. Public Health 2020, 17, 7340. [Google Scholar] [CrossRef] [PubMed]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef]
- Bartsch, S.M.; O’Shea, K.J.; Ferguson, M.C.; Bottazzi, M.E.; Wedlock, P.T.; Strych, U.; McKinnell, J.A.; Siegmund, S.S.; Cox, S.N.; Hotez, P.J.; et al. Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention. Am. J. Prev. Med. 2020, 59, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Creese, J.; Byrne, J.P.; Conway, E.; Barrett, E.; Prihodova, L.; Humphries, N. We All Really Need to just Take a Breath: Composite Narratives of Hospital Doctors’ Well-Being during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2051. [Google Scholar] [CrossRef]
- Paffenholz, P.; Peine, A.; Hellmich, M.; Paffenholz, S.V.; Martin, L.; Luedde, M.; Haverkamp, M.; Roderburg, C.; Marx, G.; Heidenreich, A.; et al. Perception of the 2020 SARS-CoV-2 pandemic among medical professionals in Germany: Results from a nationwide online survey. Emerg. Microbes Infect. 2020, 9, 1590–1599. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. Covid-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 120. [Google Scholar] [CrossRef]
- Yu, Y.; Lau, J.T.; She, R.; Chen, X.i.; Li, L.; Chen, X. Prevalence and associated factors of intention of COVID-19 vaccination among healthcare workers in China: Application of the Health Belief Model. Hum. Vaccines Immunother. 2021, 19, 1–9. [Google Scholar] [CrossRef]
- Iyengar, K.P.; Ish, P.; Upadhyaya, G.K.; Malhotra, N.; Vaishya, R.; Jain, V.K. COVID-19 and mortality in doctors. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1743–1746. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Sikavi, D.R.; Lo, C.H.; Kwon, S.; Song, M.; et al. Risk, of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, 475–483. [Google Scholar] [CrossRef]
- Walsh, E.E.; Frenck, R.W.; Falsey, A.R.; Kitchin, A.J.; Gurtman, A.; Lockhart, S.T.; Neuzil, K.; Mulligan, M.J.; Bailey, R.; Swanson, K.E.; et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N. Engl. J. Med. 2020, 383, 2439–2450. [Google Scholar] [CrossRef]
- Naguy, A.; Moodliar-Rensburg, S.; Alamiri, B. Coronaphobia and chronophobia—A psychiatric perspective. Asian J. Psychiatry 2020, 51, 102050. [Google Scholar] [CrossRef]
- Jahan, I.; Ullah, I.; Griffiths, M.D.; Mamun, M.A. COVID-19 suicide and its causative factors among the healthcare professionals: Case study evidence from press reports. Perspect. Psychiatr. Care 2021. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, D. The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian J. Psychiatry 2020, 50, 1021032. [Google Scholar] [CrossRef]
- Dangal, G. An Overview and Changing Scenario of Post-graduate Medical Education in Nepal: What Is the Way Forward? J. Nepal Health Res. Counc. 2020, 18. [Google Scholar] [CrossRef]
- SteelFisher, G.K.; Blendon, R.J.; Caporello, H. An Uncertain Public—Encouraging Acceptance of COVID-19 Vaccines. N. Engl. J. Med. 2021, 384, 1483–1487. [Google Scholar] [CrossRef]
- Paek, H.-J.; Hove, T. Risk Perceptions and Risk Characteristics. Oxf. Res. Encycl. Commun. 2017, 10. [Google Scholar] [CrossRef]
- Lange, K.W. Coronavirus disease 2019 (COVID-19) and global mental health. Glob. Health J. 2021, 5, 31–36. [Google Scholar] [CrossRef]
- Rimmer, A. Do doctors have to have the Covid-19. BMJ 2021. [Google Scholar] [CrossRef]
Short Biography of Authors

| KERRYPNX | Age (Years) | Work Experience (Years) | |
|---|---|---|---|
| Group of Respondents | n | Mean ± SD | Mean ± SD |
| All respondents | 149 | 32.1 ± 6.99 | 6.2 ± 6.8 |
| Gender: | |||
| women | 85 | 31.18 ± 6.35 | 5.25 ± 6 |
| men | 64 | 33.38 ± 7.61 | 7.48 ± 7.62 |
| Age: | |||
| 26–30 years old | 93 | 28.03 ± 1.34 | 2.55 ± 1.26 |
| 31–45 years old | 48 | 36.67 ± 4.18 | 9.94 ± 4.69 |
| 46–69 years old | 8 | 52.38 ± 7.63 | 26.38 ± 8.63 |
| Question | Answer | Age | Chi-Square Test for Independence | ||||
|---|---|---|---|---|---|---|---|
| 26–30 yo | 31–45 yo | 46–69 yo | Chi-Square | df | p | ||
| n | n | n | |||||
| How do you rate the effectiveness of the vaccine you have received? | Effective | 44 (47.3%) | 37 (77.1%) | 6 (75%) | 12.886 | 4 | 0.012 |
| Ineffective | 2 (2.2%) | 1 (2.1%) | 0 | ||||
| I have no opinion | 47 (50.5%) | 10 (20.8%) | 2 (25%) | ||||
| Are you worried about the negative effects of taking the vaccine? | Yes | 21 (22.6%) | 6 (12.5%) | 1 (12.5%) | 14.205 | 6 | 0.027 |
| No | 55 (59.1%) | 25 (52.1%) | 5 (62.5%) | ||||
| I do not think about that | 12 (12.9%) | 17 (35.4%) | 1 (12.5%) | ||||
| I do not care | 5 (5.4%) | 0 | 1 (12.5%) | ||||
| Do you agree that taking the vaccine will help to contain the pandemic? | I definitely agree | 42 (45.1%) | 32 (66.7%) | 5 (62.5%) | 9.837 | 8 | 0.277 |
| I agree | 38 (40.9%) | 11 (22.9%) | 3 (37.5%) | ||||
| I rather agree | 9 (9.7%) | 3 (6.2%) | 0 | ||||
| I rather disagree | 0 | 1 (2.1%) | 0 | ||||
| Hard to say | 4 (4.3%) | 1 (2.1%) | 0 | ||||
| Did you feel fear when you were vaccinated? | Yes | 8 (8.6%) | 5 (10.4%) | 1 (12.5%) | 2.25 | 4 | 0.69 |
| Little | 27 (29%) | 19 (39.6%) | 3 (37.5%) | ||||
| No | 58 (62.4%) | 24 (50%) | 4 (50%) | ||||
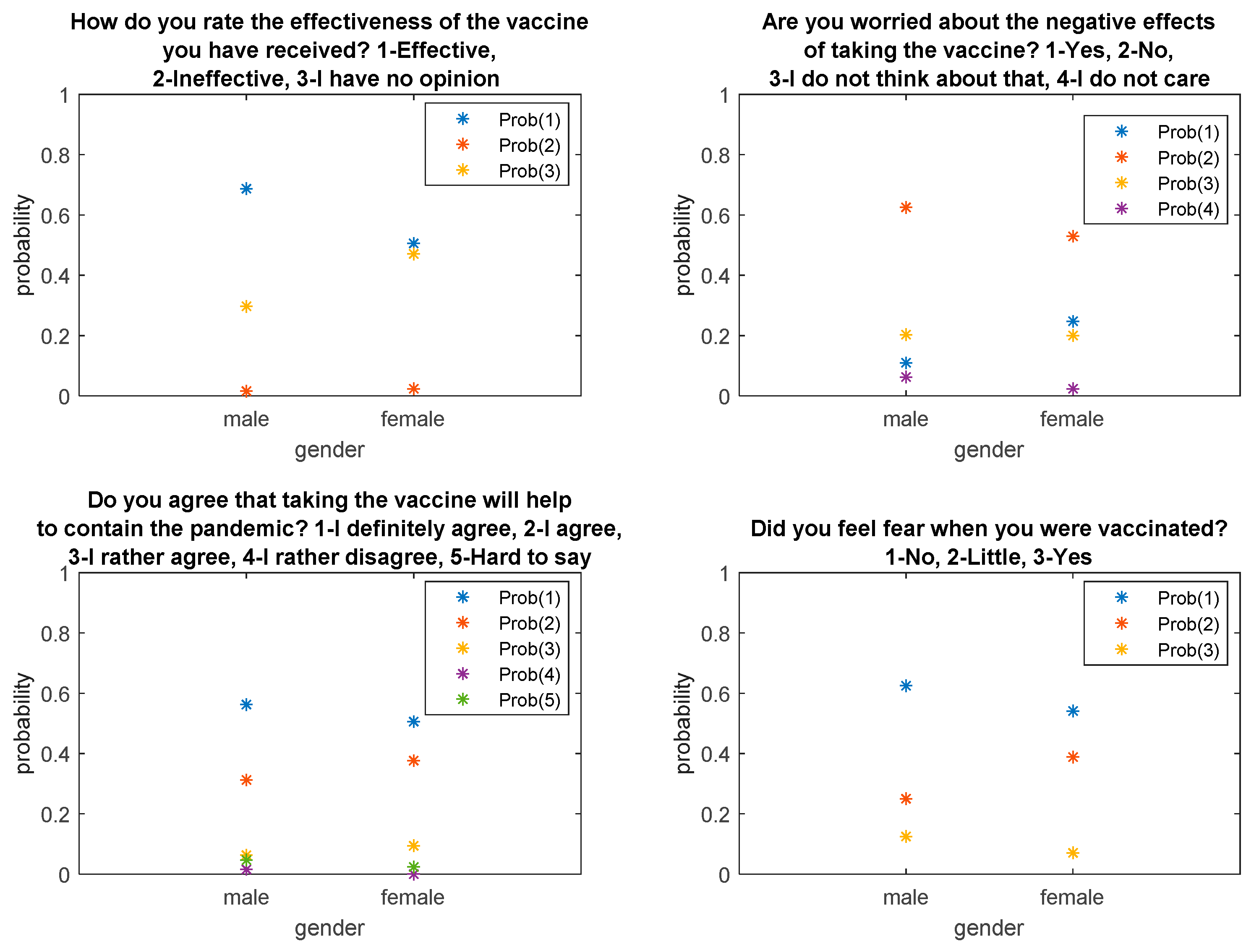
| Question | Answer | Gender | Chi-Square Test for Independence | |||
|---|---|---|---|---|---|---|
| Women | Men | Chi-Square | df | p | ||
| n | n | |||||
| How do you rate the effectiveness of the vaccine you have received? | Effective | 43 (50.6%) | 44 (68.7%) | 4.958 | 2 | 0.084 |
| Ineffective | 2 (2.4%) | 1 (1.6%) | ||||
| I have no opinion | 40 (47%) | 19 (29.7%) | ||||
| Are you worried about the negative effects of taking the vaccine? | Yes | 21 (24.7%) | 7 (10.9%) | 5.647 | 3 | 0.13 |
| No | 45 (52.9%) | 40 (62.5%) | ||||
| I do not think about that | 17 (20%) | 13 (20.3%) | ||||
| I do not care | 2 (2.4%) | 4 (6.3%) | ||||
| Do you agree that taking the vaccine will help to contain the pandemic? | I definitely agree | 43 (50.6%) | 36 (56,3%) | 3.023 | 4 | 0.554 |
| I agree | 32 (37.6%) | 20 (31.2%) | ||||
| I rather agree | 8 (9.4%) | 4 (6.2%) | ||||
| I rather disagree | 0 | 1 (1.6%) | ||||
| Hard to say | 2 (2.4%) | 3 (4.7%) | ||||
| Did you feel fear when you were vaccinated? | Yes | 6 (7.1%) | 8 (12.5%) | 3.716 | 2 | 0.156 |
| Little | 33 (38.8%) | 16 (25%) | ||||
| No | 46 (54.1%) | 40 (62.5%) | ||||
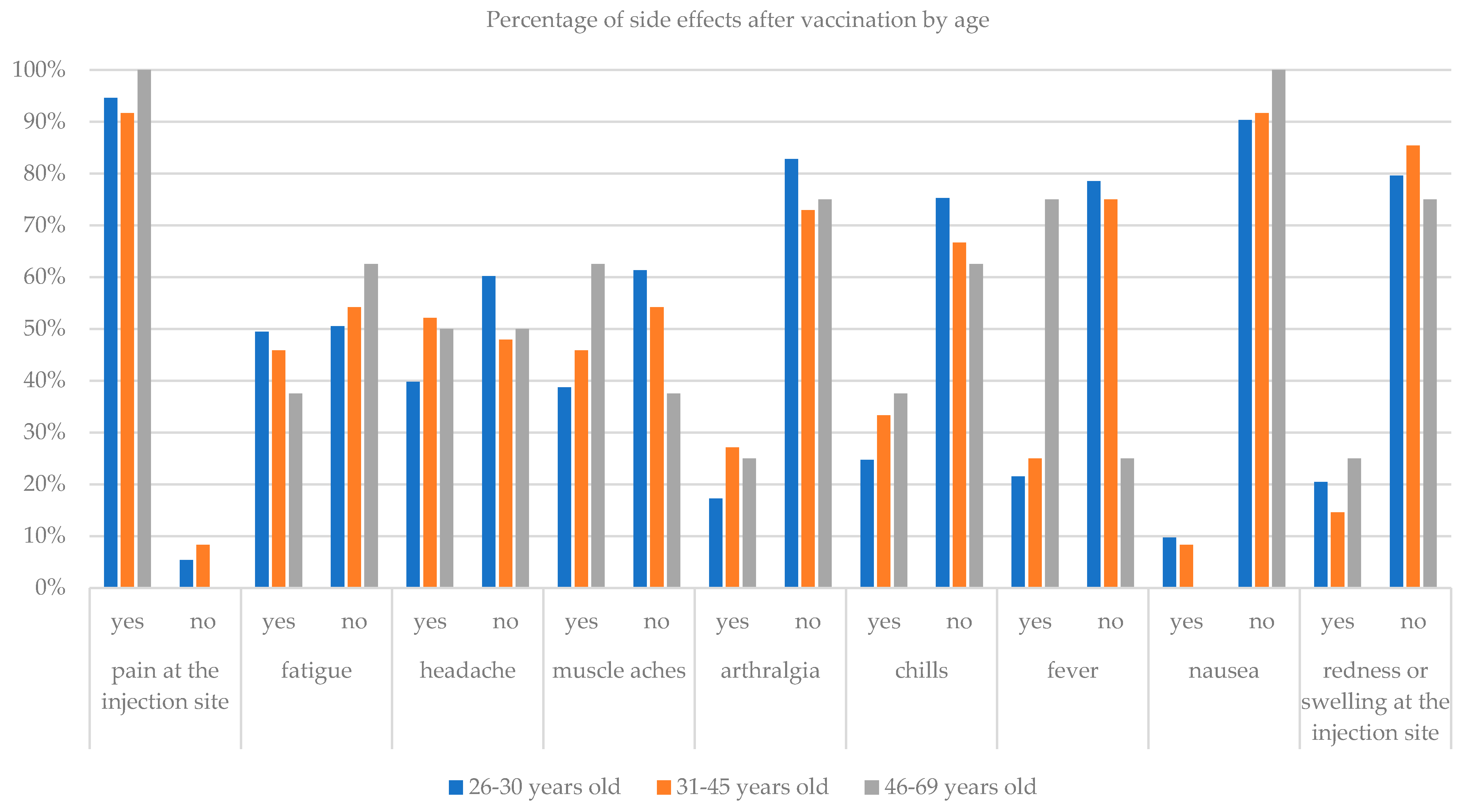
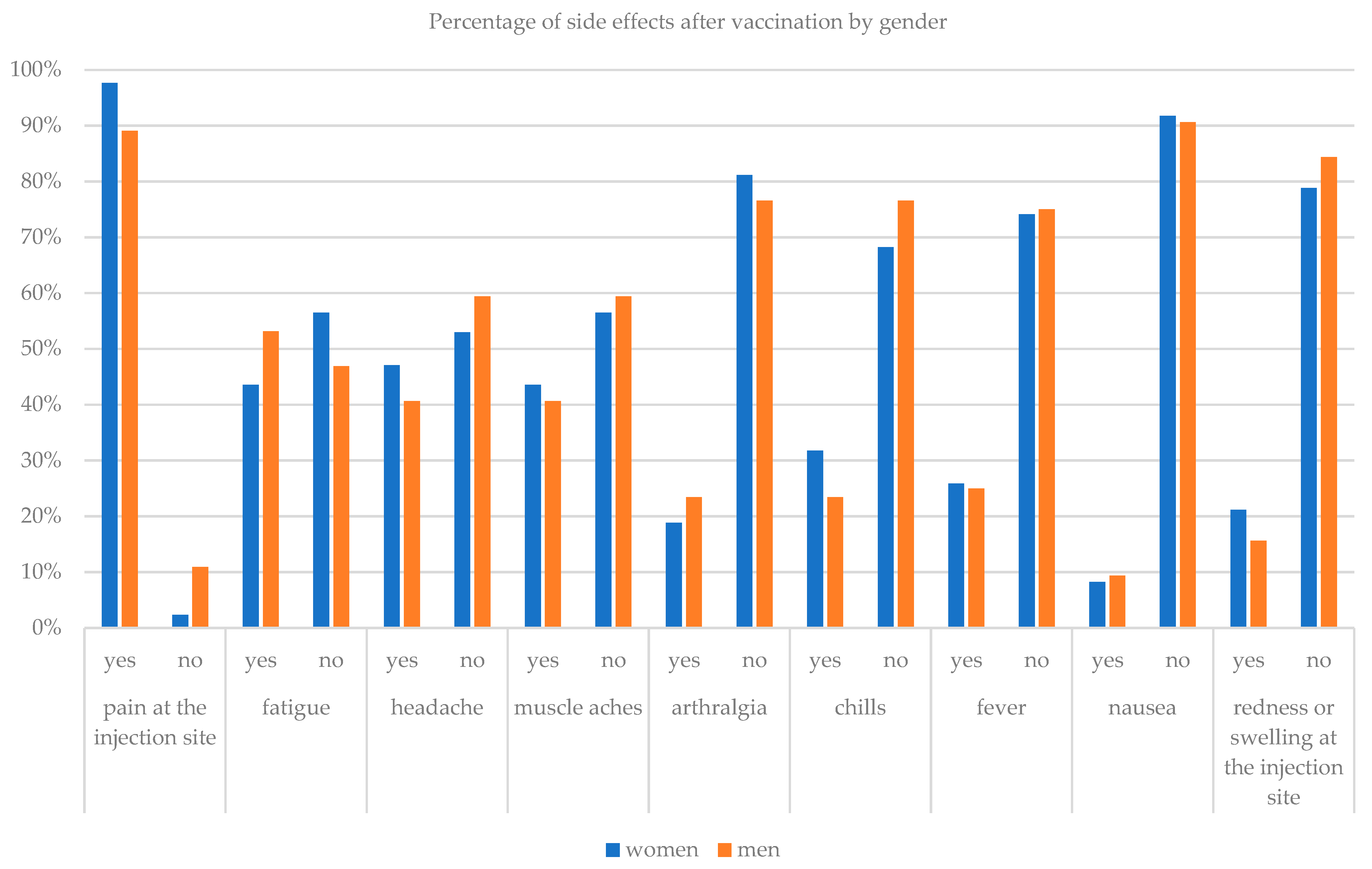
| Side Effect after Taking the Vaccine | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Pain at the Injection Site | Fatigue | Headache | Muscle Aches | Arthralgia | Chills | Fever | Nausea | Redness or Swelling at the Injection Site | ||
| Age | 26–30 yo | yes | 88 | 46 | 37 | 36 | 16 | 23 | 20 | 9 | 19 |
| n | no | 5 | 47 | 56 | 57 | 77 | 70 | 73 | 84 | 74 | |
| 31–45 yo | yes | 44 | 22 | 25 | 22 | 13 | 16 | 12 | 4 | 7 | |
| n | no | 4 | 26 | 23 | 26 | 35 | 32 | 36 | 44 | 41 | |
| 46–69 yo | yes | 8 | 3 | 4 | 5 | 2 | 3 | 6 | 0 | 2 | |
| n | no | 0 | 5 | 4 | 3 | 6 | 5 | 2 | 8 | 6 | |
| chi-square test | chi-sq | 1.031 | 0.516 | 2.052 | 2.074 | 1.966 | 1.519 | 11.104 | 0.88 | 0.923 | |
| df | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | ||
| p | 0.597 | 0.772 | 0.358 | 0.354 | 0.374 | 0.468 | 0.004 | 0.644 | 0.63 | ||
| Gender | Women n | yes | 83 | 37 | 40 | 37 | 16 | 27 | 22 | 7 | 18 |
| no | 2 | 48 | 45 | 48 | 69 | 58 | 63 | 78 | 67 | ||
| men n | yes | 57 | 34 | 26 | 26 | 15 | 15 | 16 | 6 | 10 | |
| no | 7 | 30 | 38 | 38 | 49 | 49 | 48 | 58 | 54 | ||
| chi-square test | chi-sq | 4.741 | 1.348 | 0.612 | 0.126 | 0.471 | 1.251 | 0.015 | 0.060 | 0.737 | |
| df | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| p | 0.029 | 0.246 | 0.434 | 0.722 | 0.492 | 0.263 | 0.903 | 0.807 | 0.391 | ||
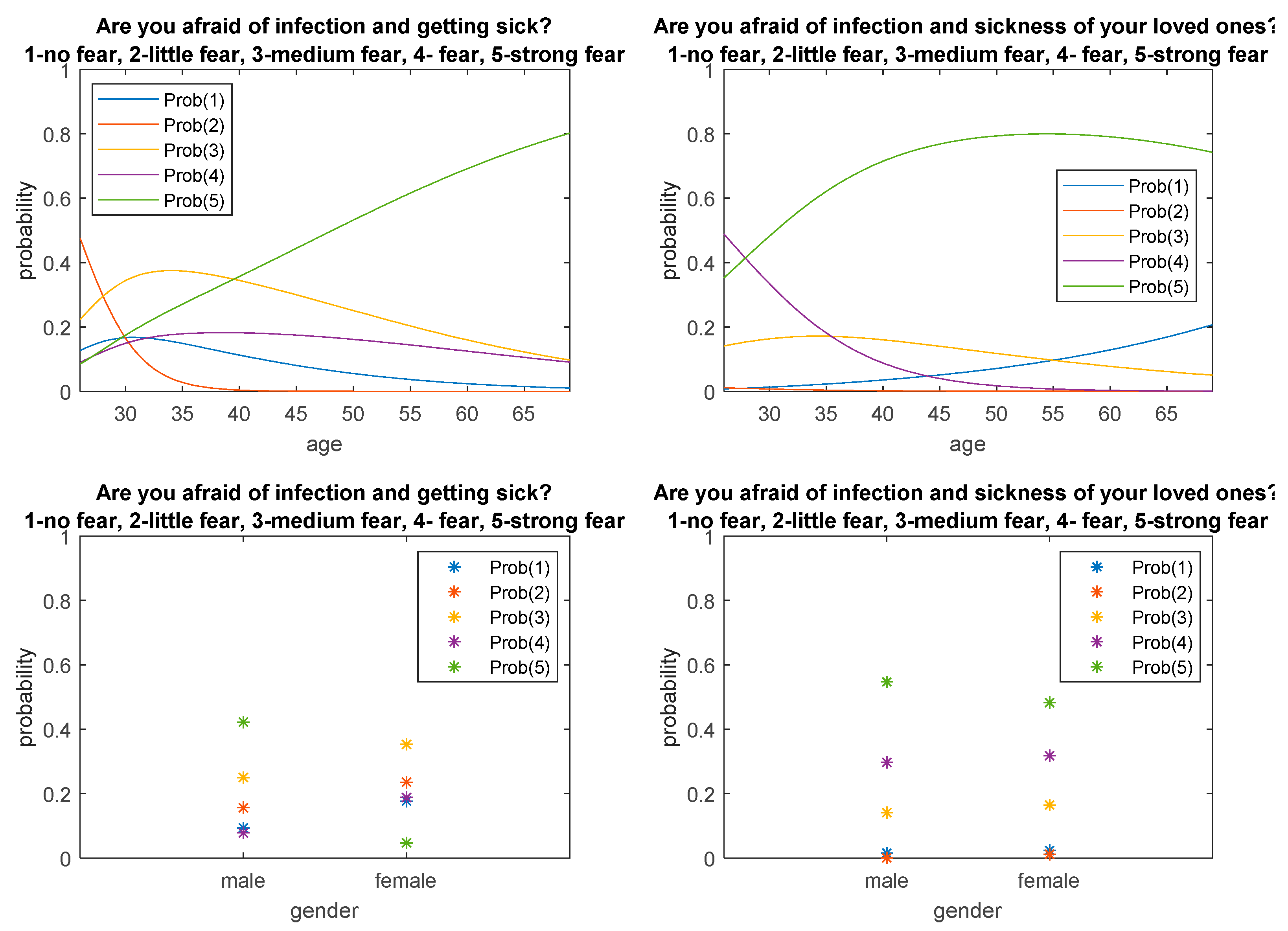
| Mann–Whitney Test | ||||
|---|---|---|---|---|
| Variable | Mean ± SD | n | z-Value | p |
| Are you afraid of infection and getting sick? | ||||
| women | 2.69 ± 1.11 | 85 | −3.8621 | <0.001 |
| men | 3.58 ± 1.41 | 64 | ||
| Are you afraid of infection and sickness of your loved ones? | ||||
| women | 4.22 ± 0.93 | 85 | −0.8712 | 0.384 |
| men | 4.36 ± 0.84 | 64 | ||
| Kruskal–Wallis Test | Mann–Whitney Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AvsB | AvsC | BvsC | |||||||||
| Variable | Mean ± SD | n | chi-sq | df | p | z-val | p | z-val | p | z-val | p |
| Are you afraid of infection and getting sick? | |||||||||||
| 26–30 years old | 2.62 ± 1.16 | 93 | 30.066 | 2 | <0.001 | −5.20 | <0.001 | −2.62 | 0.009 | −0.02 | 0.982 |
| 31–45 years old | 3.83 ± 1.21 | 48 | |||||||||
| 46–69 years old | 3.75 ± 1.49 | 8 | |||||||||
| Are you afraid of infection and sickness of your loved ones? | |||||||||||
| 26–30 years old | 4.15 ± 0.85 | 93 | 11.232 | 2 | 0.0036 | −3.22 | 0.0013 | −0.94 | 0.349 | 0.37 | 0.712 |
| 31–45 years old | 4.58 ± 0.79 | 48 | |||||||||
| 46–69 years old | 4.00 ± 1.51 | 8 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zdziarski, K.; Landowski, M.; Zabielska, P.; Karakiewicz, B. Subjective Feelings of Polish Doctors after Receiving the COVID-19 Vaccine. Int. J. Environ. Res. Public Health 2021, 18, 6291. https://doi.org/10.3390/ijerph18126291
Zdziarski K, Landowski M, Zabielska P, Karakiewicz B. Subjective Feelings of Polish Doctors after Receiving the COVID-19 Vaccine. International Journal of Environmental Research and Public Health. 2021; 18(12):6291. https://doi.org/10.3390/ijerph18126291
Chicago/Turabian StyleZdziarski, Krzysztof, Marek Landowski, Paulina Zabielska, and Beata Karakiewicz. 2021. "Subjective Feelings of Polish Doctors after Receiving the COVID-19 Vaccine" International Journal of Environmental Research and Public Health 18, no. 12: 6291. https://doi.org/10.3390/ijerph18126291
APA StyleZdziarski, K., Landowski, M., Zabielska, P., & Karakiewicz, B. (2021). Subjective Feelings of Polish Doctors after Receiving the COVID-19 Vaccine. International Journal of Environmental Research and Public Health, 18(12), 6291. https://doi.org/10.3390/ijerph18126291






