Microbial Air Quality in Healthcare Facilities
Abstract
1. Preface
2. Methodology
3. Waterborne and Bioaerosol-Associated Infections
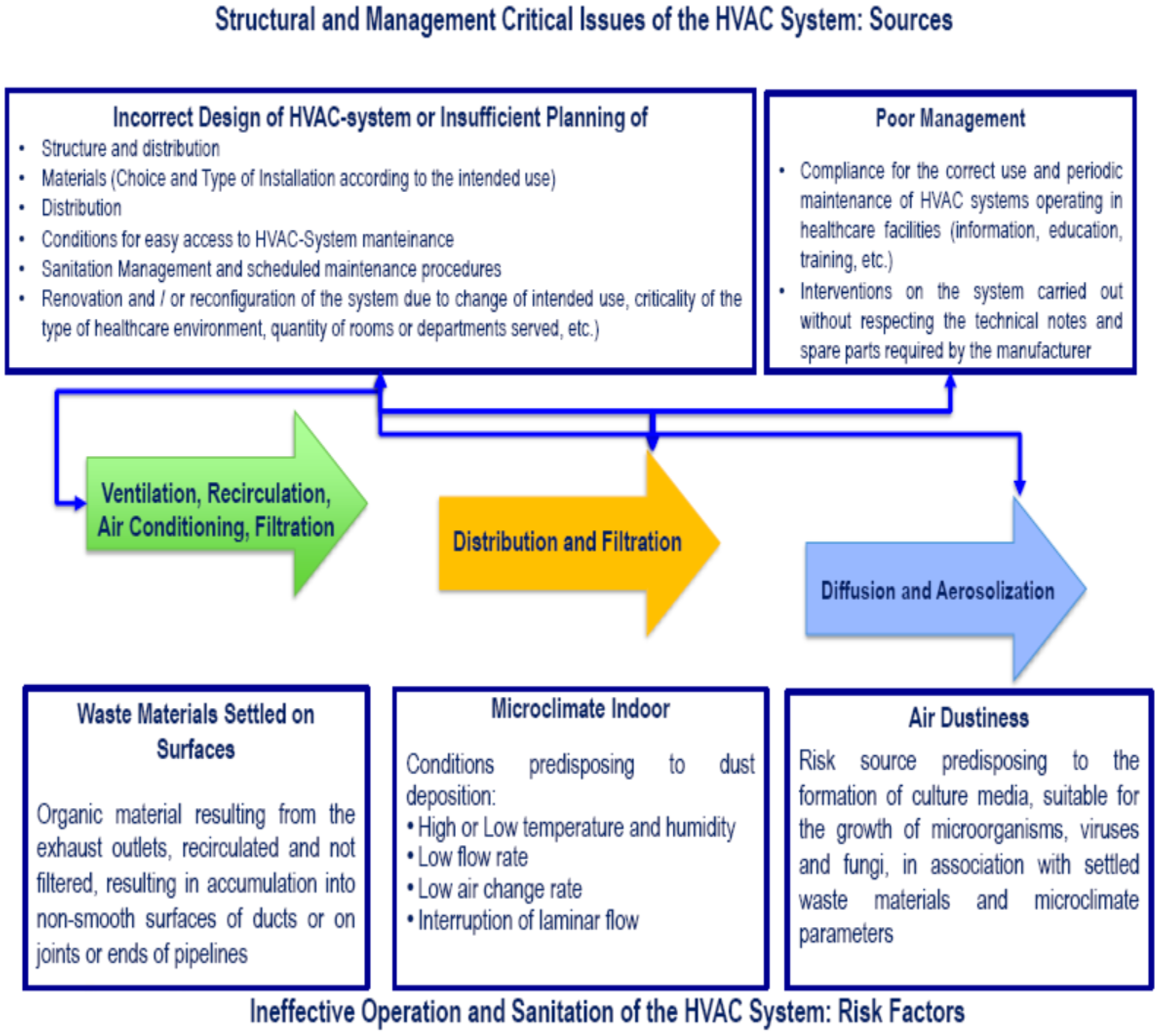
4. Air Treatment Systems and Airborne Diffusion of Microorganisms
5. Mold Infections in Hospital Environments
6. Surfaces as a Potential Source of Infection
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bereket, W.; Hemalatha, K.; Getenet, B.; Wondwossen, T.; Solomon, A.; Zeynudin, A.; Kannan, S. Update on bacterial nosocomial infections. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1039–1044. [Google Scholar] [PubMed]
- Cohen, B.; Spirito, C.M.; Liu, J.; Cato, K.D.; Larson, E. Concurrent detection of bacterial pathogens in hospital roommates. Nurs. Res. 2019, 68, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Scarafile, G. Antibiotic resistance: Current issues and future strategies. Rev. Health Care 2016, 7, 16. [Google Scholar] [CrossRef]
- Saran, S.; Gurjar, M.; Baronia, A.; Sivapurapu, V.; Ghosh, P.S.; Raju, G.M.; Maurya, I. Heating, ventilation and air conditioning (HVAC) in intensive care unit. Crit. Care 2020, 24, 194. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W. The effect of environmental parameters on the survival of airborne infectious agents. J. R. Soc. Interface 2009, 6 (Suppl. 6), S737–S746. [Google Scholar] [CrossRef] [PubMed]
- Klevens, M.; Edwards, J.R.; Richards, C.L.; Horan, T.C.; Gaynes, R.P.; Pollock, D.A.; Cardo, D.M. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007, 122, 160–166. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Report on the Burden of Endemic Health Care-Associated Infection Worldwide; World Health Organization Press: Geneva, Switzerland, 2011. [Google Scholar]
- Chisholm, R.H.; Campbell, P.T.; Wu, Y.; Tong, S.Y.C.; McVernon, J.; Geard, N. Implications of asymptomatic carriers for infectious disease transmission and control. R. Soc. Open Sci. 2018, 5, 172341. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Schwebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef]
- Weber, D.J.; Anderson, D.; Rutala, W.A. The role of the surface environment in healthcare-associated infections. Curr. Opin. Infect. Dis. 2013, 26, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Decker, B.K.; Palmore, T.N. Hospital water and opportunities for infection prevention. Curr. Infect. Dis. Rep. 2014, 16, 432. [Google Scholar] [CrossRef]
- Pande, S.; Dwive, A.K. Nosocomial infections through hospital waste. Int. J. Waste Resour. 2016, 6. [Google Scholar] [CrossRef]
- Nazaroff, W.W. Indoor bioaerosol dynamics. Indoor Air 2016, 26, 61–78. [Google Scholar] [CrossRef] [PubMed]
- Messina, G.; Ceriale, E.; Lenzi, D.; Burgassi, S.; Azzolini, E.; Manzi, P. Environmental contaminants in hospital settings and progress in disinfecting techniques, BioMed. Res. Inter. 2013, 2013, 1–8. [Google Scholar] [CrossRef]
- English, K.M.; Langley, J.M.; McGeer, A.; Hupert, N.; Tellier, R.; Henry, B.; Halperin, S.A.; Johnston, L.; Pourbohloul, B. Contact among healthcare workers in the hospital setting: Developing the evidence base for innovative approaches to infection control. BMC Infect. Dis. 2018, 18, 184. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Guidelines on Hand Hygiene in Health Care; World Health Organization Press: Geneva, Switzerland, 2009. [Google Scholar]
- Haverstick, S.; Goodrich, C.; Freeman, R.; James, S.; Kullar, R.; Ahrens, M. Patients’ Hand Washing and Reducing Hospital-Acquired Infection. Crit. Care Nurse 2017, 37, e1–e8. [Google Scholar] [CrossRef]
- McBryde, E.S.; Bradley, L.C.; Whitby, M.; McElwain, D.L. An investigation of contact transmission of methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 2004, 58, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Raza, T.; Ullah, S.R.; Mehmood, K.; Andleeb, S. Vancomycin resistant Enterococci: A brief review. J. Pak. Med. Assoc. 2018, 68, 768–772. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Surveillance of Antimicrobial Resistance in Europe Surveillance Report; ECDC: Stockholm, Sweden, 2018; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/surveillance-antimicrobial-resistance-Europe-2018.pdf (accessed on 6 June 2021).
- Grundmann, H.; Glasner, C.; Albiger, B.; Aanensen, D.M.; Tomlinson, C.T.; Andrasević, A.T.; Cantón, R.; Carmeli, Y.; Friedrich, A.W.; Giske, C.G. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): A prospective, multinational study. Lancet Infect. Dis. 2017, 17, 153–163. [Google Scholar] [CrossRef]
- Segagni Lusignani, L.; Starzengruber, P.; Dosch, V.; Assadian, O.; Presterl, E.; Diab-Elschahawi, M. Molecular epidemiology of multidrug-resistant clinical isolates of Acinetobacter baumannii. Wien. Klin. Wochenschr. 2017, 129, 816–822. [Google Scholar] [CrossRef] [PubMed]
- Ayobami, O.; Willrich, N.; Harder, T.; Okeke, N.; Eckmanns, T.; Markwart, R. The incidence and prevalence of hospital-acquired (carbapenem-resistant) Acinetobacter baumannii in Europe, Eastern Mediterranean and Africa: A systematic review and meta-analysis. Emerg. Microbes Infect. 2019, 8, 1747–1759. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Regional Outbreak of New Delhi Metallo-Betalactamase-Producing Carbapenem-Resistant Enterobacteriaceae, Italy, 2018–2019; ECDC: Stockholm, Sweden, 2019; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/04-Jun-2019-RRA-Carbapenems%2C%20Enterobacteriaceae-Italy.pdf (accessed on 6 June 2021).
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.A.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.M.; Armbruster, C.R.; Arduino, M.J. Plumbing of hospital premises is a reservoir for opportunistically pathogenic microorganisms: A review. Biofouling 2013, 29, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Decker, B.K.; Palmore, T.N. The role of water in healthcare-associated infections. Curr. Opin. Infect. Dis. 2013, 26, 345–351. [Google Scholar] [CrossRef]
- Capelletti, R.V.; Moraes, Â.M. Waterborne microorganisms and biofilms related to hospital infections: Strategies for prevention and control in healthcare facilities. J. Water Health 2016, 14, 52–67. [Google Scholar] [CrossRef]
- Bonadonna, L.; Memoli, G.; Chiaretti, G. Formazione di biofilm su materiali a contatto con acqua: Aspetti sanitari e tecnologici. In Rapporti ISTISAN 08/19; Istituto Superiore di Sanità: Roma, Italy, 2008. [Google Scholar]
- Exner, M.; Kramer, A.; Lajoie, L.; Gebel, J.; Engelhart, S.; Hartemann, P. Prevention and control of health care-associated waterborne infections in health care facilities. Am. J. Infect. Control. 2005, 33, S26–S40. [Google Scholar] [CrossRef] [PubMed]
- Loveday, H.P.; Wilson, J.A.; Kerr, K.; Pitchers, R.; Walker, J.T.; Browne, J. Association between healthcare water systems and Pseudomonas aeruginosa infections: A rapid systematic review. J. Hosp. Infect. 2014, 86, 7–15. [Google Scholar] [CrossRef]
- Emmerson, A.M. Emerging waterborne infections in health-care settings. Emerg. Infect. Dis. 2001, 7, 272–276. [Google Scholar] [CrossRef]
- Trautmann, M.; Lepper, P.M.; Haller, M. Ecology of Pseudomonas aeruginosa in the intensive care unit and the evolving role of water outlets as a reservoir of the organism. Am. J. Infect. Control. 2005, 33 (Suppl. 1), S41–S49. [Google Scholar] [CrossRef]
- Jones, S. Hand hygiene and transmission of Pseudomonas aeruginosa on hands in a hospital environment. Infect. Prev. 2011, 12, 146–148. [Google Scholar] [CrossRef]
- de Abreu, P.M.; Farias, P.G.; Paiva, G.S.; Almeida, A.M.; Morais, P.V. Persistence of microbial communities including Pseudomonas aeruginosa in a hospital environment: A potential health hazard. BMC Microbiol. 2014, 14, 118. [Google Scholar] [CrossRef]
- Haley, C.E.; Cohen, M.L.; Halter, J.; Meyer, R.D. Nosocomial legionnaires’ disease: A continuing common-source epidemic at Wadsworth Medical Center. Ann. Intern. Med. 1979, 90, 583–586. [Google Scholar] [CrossRef]
- Kirby, B.D.; Snyder, K.M.; Meyer, R.D.; Finegold, S.M. Legionnaires’ disease: Report of sixty-five nosocomially acquired cases and review of the literature. Medicine 1980, 59, 188–205. [Google Scholar] [CrossRef]
- Parry, M.F.; Stampleman, L.; Hutchinson, J.H.; Folta, D.; Steinberg, M.G.; Krasnogor, L.J. Waterborne Legionella bozemanii and nosocomial pneumonia in immunosuppressed patients. Ann. Intern. Med. 1985, 103, 205–210. [Google Scholar] [CrossRef]
- Joly, J.R.; Alary, M. Occurrence of nosocomial Legionnaires’ disease in hospitals with contaminated potable water supply. In Legionella: Current Status and Emerging Perspectives; Barbaree, J.M., Breiman, R.F., Dufour, A.P., Eds.; ASM Press: Washington, DC, USA, 1994; pp. 39–43. [Google Scholar]
- World Health Organization (WHO). Legionella and the Prevention of Legionellosis; Bartram, J., Chartier, Y., Lee, J.V., Pond, K., Surman-Lee, S., Eds.; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Pereira, A.C.; Ramos, B.; Reis, A.C.; Cunha, M.V. Non-Tuberculous Mycobacteria: Molecular and Physiological Bases of Virulence and Adaptation to Ecological Niches. Microorganisms 2020, 8, 1380. [Google Scholar] [CrossRef]
- Briancesco, R.; Semproni, M.; Della Libera, S.; Sdanganelli, M.; Bonadonna, L. Non-tuberculous mycobacteria and microbial populations in drinking water distribution systems. Ann. Ist. Super. Sanita 2010, 46, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Falkinham, J.O., 3rd. Nontuberculous mycobacteria from household plumbing of patients with nontuberculous mycobacteria disease. Emerg. Infect. Dis. 2011, 17, 419–424. [Google Scholar] [CrossRef]
- Briancesco, R.; Semproni, M.; Paradiso, R.; Bonadonna, L. Nontuberculous mycobacteria: An emerging risk in engineered environmental habitats. Ann. Microbiol. 2014, 64, 735–740. [Google Scholar] [CrossRef]
- Anaissie, E.J.; Stratton, S.L.; Dignani, M.C.; Lee, C.; Summerbell, R.C.; Rex, J.R.; Monson, T.P.; Walsh, T.J. Pathogenic molds (including Aspergillus species) in hospital water distribution systems-a 3-year prospective study and clinical implication for patients with hematologic malignancies. Blood 2003, 101, 2542–2546. [Google Scholar] [CrossRef]
- Green, B.J.; Tovey, E.R.; Sercombe, J.K.; Blachere, F.M.; Beezhold, D.H.; Schmechel, D. Airborne fungal fragments and allergenicity. Med. Mycol. 2006, 44, S245–S255. [Google Scholar] [CrossRef] [PubMed]
- Moscato, U.; Borghini, A.; Teleman, A.A. HVAC Management in Health Facilities. In Indoor Air Quality in Healthcare Facilities; Capolongo, S., Settimo, G., Gola, M., Eds.; Springer Briefs in Public Health: Cham, Switzerland, 2017. [Google Scholar]
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) ANSI/ASHRAE Standard 62.1. Ventilation for Acceptable Indoor Air Quality; American Society of Heating, Refrigeration, and Air-Conditioning Engineers: Atlanta, GA, USA, 2016. [Google Scholar]
- Medical Advisory Secretariat. Air cleaning technologies: An evidence-based analysis. Ont. Health Technol. Assess. Ser. 2015, 5, 1–52. [Google Scholar]
- Pasquarella, C.; Barchitta, M.; D’Alessandro, D.; Cristina, M.L.; Mura, I.; Nobile, M.; Auxilia, F.; Agodi, A.; Gruppo Italiano di Studio sull’Igiene Ospedaliera- SItI (GISIO). Heating, ventilation and air conditioning (HVAC) system, microbial air contamination and surgical site infection in hip and knee arthroplasties: The GISIO-SItI Ischia study. Ann. Ig. 2018, 30, 22–35. [Google Scholar] [CrossRef]
- Saran, S.; Gurjar, M.; Azim, A.; Maurya, I. Structural risk factors for hospital-acquired infections in intensive care unit. HERD 2020, 1–9. [Google Scholar] [CrossRef]
- Hanssen, S.O. HVAC: The importance of clean intake section and dry filter in cold climate. Indoor Air 2004, 14 (Suppl. l7), 195–201. [Google Scholar] [CrossRef] [PubMed]
- Moscato, U.; Capolongo, S.; D’alessandro, D. Approfondimenti di Igiene ed Edilizia Ospedaliera. In Igiene, Medicina Preventiva e Sanità Pubblica; Ricciardi, G., Ed.; Idelson-Gnocchi: Naples, Italy, 2013. [Google Scholar]
- Caggiano, G.; Napoli, C.; Coretti, C.; Lovero, G.; Scarafile, G.; De Giglio, O.; Montagna, M.T. Mold contamination in a controlled hospital environment: A 3-year surveillance in southern Italy. BMC Infect. Dis. 2014, 14, 595. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Cruz, C.P.; Najera Aguilar, M.J.; Arroyo-Helguera, O.E. Fungal and Bacterial Contamination on Indoor Surfaces of a Hospital in Mexico. Jundishapur J. Microbiol. 2012, 5, 460–464. [Google Scholar] [CrossRef]
- Ricciardi, W.; Angelillo, I.F.; Brusaferro, S.; De Giusti, M.; De Vito, E.; Moscato, U.; Pavia, M.; Siliquini, R.; Villari, P. Igiene per le Professioni Sanitarie, II Edizione; Idelson-Gnocchi: Naples, Italy, 2019. [Google Scholar]
- Obbard, J.; Fang, L. Airborne concentrations of bacteria in a hospital environment in Singapore. Water Air Soil Pollut. 2003, 144, 333–341. [Google Scholar] [CrossRef]
- Taccone, F.S.; Van den Abeele, A.M.; Bulpa, P.; Misset, B.; Meersseman, W.; Cardoso, T.; Paiva, J.; Blasco-Navalpotro, M.; De Laere, E.; Dimopoulos, G.; et al. Epidemiology of invasive aspergillosis in critically ill patients: Clinical presentation, underlying conditions and outcomes. Crit. Care 2015, 19, 7. [Google Scholar] [CrossRef]
- Fishman, J.A. Overview: Fungal infections in the transplant patient. Transpl. Infect. Dis. 2002, 4 (Suppl. 3) (Suppl. 3), 3–11. [Google Scholar] [CrossRef]
- Kauffman, C.A.; Freifeld, A.G.; Andes, D.R.; Baddley, J.W.; Herwaldt, L.; Walker, R.C.; Alexander, B.D.; Anaissie, E.J.; Benedict, K.; Ito, J.I.; et al. Endemic fungal infections in solid organ and hematopoietic cell transplant recipients enrolled in the Transplant-Associated Infection Surveillance Network (TRANSNET). Transpl. Infect. Dis. 2014, 16, 213–224. [Google Scholar] [CrossRef]
- Bonadonna, L.; Briancesco, R.; Coccia, A.M.; Di Napoli, I.; Ferrante, I.; Forgia, C.; Giacomelli, M.; Giorgi, D.A.; Meloni, P.; Palmieri, S.; et al. Indagini sulla presenza di microrganismi in ambiente ospedaliero e rischi correlati. In La Qualità Dell’aria Indoor: Attuale Situazione Nazionale e Comunitaria. L’esperienza del Gruppo di Studio Nazionale sull’Inquinamento Indoor, Proceedings of the Workshop: La Qualità Dell’aria Indoor, Istituto Superiore di Sanità, Roma, 28 Maggio 2014; Santarsiero, A., Musmeci, L., Fuselli, S., e Gruppo di Studio Nazionale sull’Inquinamento Indoor, Eds.; Rapporti ISTISAN 15/4; Istituto Superiore di Sanità: Roma, Italy, 2015; pp. 102–108. [Google Scholar]
- Stephens, B.; Azimi, P.; Thoemmes, M.S.; Heidarinejad, M.; Allen, J.G.; Gilbert, J.A. Microbial exchange via fomites and implications for human health. Curr. Pollut. Rep. 2019, 5, 198–213. [Google Scholar] [CrossRef]
- Godič Torkar, K.; Ivić, S. Surveillance of bacterial colonisation on contact surfaces in different medical wards. Arh. Hig. Toksikol. 2017, 68, 116–126. [Google Scholar] [CrossRef] [PubMed][Green Version]
- D’Souza, A.W.; Potter, R.F.; Wallace, M.; Shupe, A.; Patel, S.; Sun, X.; Gul, D.; Kwon, J.H.; Andleeb, S.; Burnham, C.A.D.; et al. Spatiotemporal dynamics of multidrug resistant bacteria on intensive care unit surfaces. Nat. Commun. 2019, 10, 4569. [Google Scholar] [CrossRef] [PubMed]
- Chaoui, L.; Mhand, R.; Mellouki, F.; Rhallabi, N. Contamination of the Surfaces of a Health Care Environment by Multidrug-Resistant (MDR) Bacteria. Int. J. Microbiol. 2019, 29, 3236526. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, A.C.; Damasceno, Q.S. Surfaces of the hospital environment as possible deposits of resistant bacteria: A review. Rev. Esc. Enferm. USP 2010, 44, 1118–1123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sears, D.; Schwartz, B.S. Candida auris: An emerging multidrug-resistant pathogen. Int. J. Infect. Dis. 2017, 63, 95–98. [Google Scholar] [CrossRef]
- Hlophe, S.T.; McKerrow, N. Hospital-acquired Klebsiella pneumoniae infections in a paediatric intensive care unit. S. Afr. J. Child Health 2014, 8, 125–128. [Google Scholar] [CrossRef]
- Jin., C.; Shi, R.; Jiang, X.; Zhou, F.; Qiang, J.; An, C. Epidemic Characteristics of Carbapenem-Resistant Klebsiella pneumoniae in the Pediatric Intensive Care Unit of Yanbian University Hospital, China. Infect. Drug. Resist. 2020, 13, 1439–1446. [Google Scholar] [CrossRef]
- Lemmen, S.W.; Häfner, H.; Zolldann, D.; Stanzel, S.; Lütticken, R. Distribution of multiresistant Gram negative versus Grampositive bacteria in the hospital inanimate environment. J. Hosp. Infect. 2004, 56, 191–197. [Google Scholar] [CrossRef]
- Walker, J.; Moore, G.; Collins, S.; Parks, S.; Garvey, M.I.; Lamagni, T.; Smith, G.; Dawkin, L.; Goldenberg, S.; Chand, M. Microbiological problems and biofilms associated with Mycobacterium chimaera in heater-cooler units used for cardiopulmonary bypass. J. Hosp. Infect. 2017, 96, 209–220. [Google Scholar] [CrossRef]
- Schreiber, P.W.; Sax, H. Nosocomial and healthcare related infections Mycobacterium chimaera infections associated with heater–cooler units in cardiac surgery. Curr. Opin. Infect. Dis. 2017, 30, 388–394. [Google Scholar] [CrossRef]
- van Ingen, J.; Kohl, T.A.; Kranzer, K.; Hasse, B.; Keller, P.M.; Katarzyna Szafrańska, A.; Hillemann, D.; Chand, M.; Schreiber, P.W.; Sommerstein, R.; et al. Global outbreak of severe Mycobacterium chimaera disease after cardiac surgery: A molecular epidemiological study. Lancet Infect. Dis. 2017, 17, 1033–1041. [Google Scholar] [CrossRef]
- Cappabianca, G.; Paparella, D.; D’Onofrio, A.; Caprili, L.; Minniti, G.; Lanzafame, M.; Parolari, A.; Musumeci, F.; Beghi, C. Mycobacterium chimaera infections following cardiac surgery in Italy: Results from a National Survey Endorsed by the Italian Society of Cardiac Surgery. J. Cardiovasc. Med. 2018, 19, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Hanczvikkel, A.; Tóth, Á. Quantitative study about the role of environmental conditions in the survival capability of multidrug-resistant bacteria. J. Infect. Public Health 2018, 11, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Katzenberger, R.H.; Rösel, A.; Vonberg, R.P. Bacterial survival on inanimate surfaces: A field study. BMC Res. Notes 2021, 4, 97. [Google Scholar] [CrossRef]
- Bravo, Z.; Orruño, M.; Navascues, T.; Ogayara, E.; Ramos-Vivasb, J.; Kaberdin, V.R.; Arana, I. Analysis of Acinetobacter baumannii survival in liquid media and on solid matrices as well as effect of disinfectants. J. Hosp. Infect. 2019, 103, e42–e52. [Google Scholar] [CrossRef] [PubMed]
- Walther, B.A.; Ewald, P.W. Pathogen survival in the external environment and the evolution of virulence. Biol. Rev. Camb. Philos. Soc. 2004, 79, 849–869. [Google Scholar] [CrossRef] [PubMed]
- Drabick, J.A.; Gracely, E.J.; Heidecker, G.J.; LiPuma, J.J. Survival of Burkholderia cepacia on dry environmental surfaces. J. Hosp. Infect. 1996, 32, 267–277. [Google Scholar] [CrossRef]
- Kusumaningrum, H.D.; Riboldi, G.; Hazeleger, W.C.; Beumer, R.R. Survival of foodborne pathogens on stainless steel surfaces and cross-contamination to foods. Int. J. Food Microbiol. 2003, 85, 227–236. [Google Scholar] [CrossRef]
- Falsey, A.R.; Walsh, E.E. Transmission of Chlamydia pneumoniae. J. Infect. Dis. 1993, 168, 493–496. [Google Scholar] [CrossRef]
- Novak, K.D.; Kowalski, R.P.; Karenchak, L.M.; Gordon, Y.J. Chlamydia trachomatis can be transmitted by a nonporous plastic surface in vitro. Cornea 1995, 14, 523–526. [Google Scholar] [CrossRef]
- Wendel, K.A. Diseases due to other category B bacterial pathogens II: Psittacosis, Q fever and typhus. In Biodefense: Principles and Pathogens; Bronze, M.S., Greenfield, R.A., Eds.; Horizon Bioscience: Norfolk, VA, USA, 2005; pp. 493–498. [Google Scholar]
- Weber, D.J.; Rutala, W.A.; Miller, M.B.; Huslage, K.; Sickebert-Bennet, E. Role of hospital surfaces in the transmission of health care-associated pathogens: Norovirus, Clostridium difficile and Acinetobacter species. Am. Infect. Control. 2010, 38, S25–S33. [Google Scholar] [CrossRef]
- Augustine, J.L.; Renshaw, H.W. Survival of Corynebacterium pseudotuberculosis in axenic purulent exudate on common barnyard fomites. Am. J. Vet. Res. 1986, 47, 713–715. [Google Scholar]
- Noskin, G.A.; Stosor, V.; Cooper, I.; Peterson, L.R. Recovery of vancomycin- resistant enterococci on fingertips and environmental surfaces. Infect. Control Hosp. Epidemiol. 1995, 16, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Wendt, C.; Wiesenthal, B.; Dietz, E.; Rüden, H. Survival of vancomycin-resistant and vancomycin-susceptible enterococci on dry surfaces. J. Clin. Microbiol. 1998, 36, 3734–3736. [Google Scholar] [CrossRef] [PubMed]
- Neely, A.N.; Maley, M.P. Survival of enterococci and staphylococci on hospital fabric and plastic. J. Clin. Microbiol. 2000, 38, 724–726. [Google Scholar] [CrossRef] [PubMed]
- Wagenvoort, H.T.; De Brauwer, E.I.G.B.; Penders, R.J.R.; Willems, R.J.; Top, J.; Bonten, M.J. Environmental survival of vancomycin-resistant Enterococcus faecium. J. Hosp. Infect. 2011, 77, 274–283. [Google Scholar] [CrossRef]
- Wilks, S.A.; Michels, H.; Keevil, C.W. The survival of Escherichia coli O157 on a range of metal surfaces. Int. J. Food Microbiol. 2005, 105, 445–454. [Google Scholar] [CrossRef]
- Siroli, L.; Patrignani, F.; Serrazanetti, D.I.; Chiavari, C.; Benevelli, M.; Grazia, L.; Lanciotti, R. Survival of Spoilage and Pathogenic Microorganisms on Cardboard and Plastic Packaging Materials. Front. Microbiol. 2017, 8, 2606. [Google Scholar] [CrossRef]
- West, A.P.; Millar, M.R.; Tomkins, D.S. Effect of physical environment on survival of Helicobacter Pylori. J. Clin. Pathol. 1992, 45, 228–231. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hirai, Y. Survival of bacteria under dry conditions; from a viewpoint of nosocomial infection. J. Infect. Dis. 1991, 19, 191–200. [Google Scholar] [CrossRef]
- Neely, A.N. A Survey of Gram-Negative Bacteria Survival on Hospital Fabrics and Plastics. J. Burn. Care Rehabil. 2000, 21, 523–527. [Google Scholar] [CrossRef]
- Otter, J.A.; French, G.L. Survival of nosocomial bacteria and spores on surfaces and inactivation by hydrogen peroxide vapor. J. Clin. Microbiol. 2009, 47, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Esteves, D.C.; Pereira, V.C.; Souza, J.M.; Keller, R.; Simões, R.D.; Winkelstroter Eller, L.K.; Rodrigues, M.V.P. Influence of bioloical fluids in bacterial viability on different hospital surfaces and fomites. Am. J. Infect. Control. 2016, 44, 311–314. [Google Scholar] [CrossRef]
- Wilks, S.A.; Michels, H.T.; Keevil, C.W. Survival of Listeria monocytogenes Scott A on metal surfaces: Implications for cross-contamination. Int. J. Food Microbiol. 2006, 111, 82–93. [Google Scholar] [CrossRef] [PubMed]
- Mitscherlich, E.; Marth, E.H. Microbial Survival in the Environment; Springer: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Pérez, J.L.; Gómez, E.; Sauca, G. Survival of gonococci from urethral discharge on fomites. Eur. J. Clin. Microbiol. Infect. Dis. 1990, 9, 54–55. [Google Scholar] [CrossRef]
- Tzeng, Y.L.; Martin, L.E.; Stephens, D.S. Environmental survival of Neisseria meningitidis. Epidemiol. Infect. 2014, 1042, 187–190. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koca, O.; Altoparlak, U.; Ayyildiz, A.; Kaynar, H. Persistence of nosocomial pathogens on various fabrics. Eurasian J. Med. 2012, 44, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Scott, E.; Bloomfield, S.F. The survival and transfer of microbial contamination via cloths, hands and utensils. J. Appl. Bacteriol. 1990, 68, 271–278. [Google Scholar] [CrossRef]
- Finn, S.; Händler, K.; Condell, O.; Colgan, A.; Cooney, S.; McClure, P.; Amézquita, A.; Hinton, J.C.D.; Fanning, S. ProP is required for the survival of desiccated Salmonella enterica serovar typhimurium cells on a stainless steel surface. Appl. Environ. Microbiol. 2013, 79, 4376–4384. [Google Scholar] [CrossRef]
- Ramachandran, G.; Aheto, K.; Shirtliff, M.E.; Tennant, S.M. Poor biofilm-forming ability and long-term survival of invasive Salmonella typhimurium ST313. Pathog Dis. 2016, 74, ftw049. [Google Scholar] [CrossRef]
- Margas, E.; Meneses, N.; Conde-Petit, B.; Dodd, C.E.R.; Holah, J. Survival and death kinetics of Salmonella strains at low relative humidity, attached to stainless steel surfaces. Int. J. Food Microbiol. 2014, 187, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Hossain, M.A.; Khan, S.I.; Khan, M.N.H.; Sack, R.B.; Albert, M.J.; Huq, A.; Colwell, R.R. Survival of Shigella dysenteriae Type 1 on Fomites. J. Health Popul. Nutr. 2001, 19, 177–182. [Google Scholar] [PubMed]
- Huang, R.; Mehta, S.; Weed, D.; Price, C.S. Methicillin-resistant Staphylococcus aureus survival on hospital fomites. Infect. Control Hosp. Epidemiol. 2006, 27, 1267–1269. [Google Scholar] [CrossRef]
- Petti, S.; De Giusti, M.; Moroni, C.; Polimeni, A. Long-term survival curve of methicillin resistant Staphylococcus aureus on clinical contact surfaces in natural-like conditions. Am. J. Infect. Control 2012, 40, 1010–1012. [Google Scholar] [CrossRef] [PubMed]
- Walsh, R.L.; Camilli, A. Streptococcus pneumoniae is desiccation tolerant and infectious upon rehydration. MBio 2011, 2, e00092-11. [Google Scholar] [CrossRef]
- Marks, L.R.; Reddinger, R.M.; Hakansson, A.P. Biofilm formation enhances fomite survival of Streptococcus pneumonia and Streptococcus pyogenes. Infect. Immun. 2014, 82, 1141–1146. [Google Scholar] [CrossRef]
- Wagenvoort, J.H.; Penders, R.J.; Davies, B.I.; Lutticken, R. Similar environmental survival patterns of Streptococcus pyogenes strains of different epidemiologic backgrounds and clinical severity. Eur. J. Clin. Microbiol. Infect. Dis. 2005, 24, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Rose, L.J.; Donlan, R.; Banerjee, S.N.; Arduino, S.M. Survival of Yersinia pestis on environmental surfaces. Appl. Environ. Microbiol. 2003, 69, 2166–2171. [Google Scholar] [CrossRef]
- Rangel-Frausto, M.S.; Houston, A.K.; Bale, M.J.; Fu, C.; Wenzel, R.P. An experimental model for study of Candida survival and transmission in human volunteers. Eur. J. Clin. Microbioland Infect. Dis. 1994, 13, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Traoré, O.; Springthorpe, V.S.; Sattar, S.A. A quantitative study of the survival of two species of Candida on porous and non-porous environmental surfaces and hands. J. Appl. Microbiol. 2002, 92, 549–555. [Google Scholar] [CrossRef]
- Piedrahita, C.T.; Cadnum, J.L.; Jencson, A.L.; Shaikh, A.A.; Ghannoum, M.A.; Donskey, C.J. Environmental Surfaces in Healthcare Facilities are a Potential Source for Transmission of Candida auris and Other Candida Species. Infect. Control Hosp. Epidemiol. 2017, 38, 1107–1109. [Google Scholar] [CrossRef]
- Welsh, R.M.; Bentz, M.L.; Shams, A.; Houston, H.; Lyons, A.; Rose, L.J.; Litvintseva, A.P. Survival, Persistence, and Isolation of the Emerging Multidrug-Resistant Pathogenic Yeast Candida auris on a Plastic Health Care Surface. J. Clin. Microbiol. 2017, 55, 2996–3005. [Google Scholar] [CrossRef]
- Short, B.; Brown, J.; Delaney, C.; Sherry, L.; Williams, C.; Ramage, G.; Kean, R. Candida auris exhibits resilient biofilm characteristics in vitro: Implications for environmental persistence. J. Hosp. Infect. 2019, 103, 92–96. [Google Scholar] [CrossRef]
- Lamarre, C.; Sokol, S.; Debeaupuis, J.P.; Henry, C.; Lacroix, C.; Glaser, P.; Coppée, J.Y.; François, J.M.; Latgé, J.P. Transcriptomic analysis of the exit from dormancy of Aspergillus fumigatus conidia. BMC Genom. 2008, 9, 417. [Google Scholar] [CrossRef]
- Novodvorska, M.; Stratford, M.; Blythe, M.J.; Wilson, R.; Beniston, R.G.; Archer, D.B. Metabolic activity in dormant conidia of Aspergillus niger and developmental changes during conidial outgrowth. Fungal. Genet. Biol. 2016, 94, 23–31. [Google Scholar] [CrossRef]
- Neely, A.N.; Orloff, M.M. Survival of Some Medically Important Fungi on Hospital Fabrics and Plastics. J. Clin. Microbiol. 2001, 39, 3360–3361. [Google Scholar] [CrossRef]
- Weaver, L.; Michels, H.T.; Keevil, C.W. Potential for preventing spread of fungi in air-conditioning systems constructed using copper instead of aluminum. Lett. Appl. Microbiol. 2010, 50, 18–23. [Google Scholar] [CrossRef]
- Gupta, M.; Bisesi, M.; Lee, J. Comparison of survivability of Staphylococcus aureus and spores of Aspergillus niger on commonly used floor materials. Am. J. Infect. Control 2017, 45, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Nelson, P.E.; Dignani, M.C.; Anaissie, E.J. Taxonomy, Biology, and Clinical Aspects of Fusarium Species. J. Clin. Microbiol. 1994, 7, 479–504. [Google Scholar] [CrossRef] [PubMed]
- Hara, J.; Okomator, S.; Minekawa, Y.; Yamazaki, K.; Kase, T. Survival and disinfection of adenovirus type 19 and enterovirus 70 in ophthalmic practice. Jpn. J. Ophthalmol. 1990, 34, 421–427. [Google Scholar] [PubMed]
- Mahl, M.C.; Sadler, C. Virus survival on inanimate surfaces. Can. J. Microbiol. 1975, 21, 819–823. [Google Scholar] [CrossRef]
- Abad, F.X.; Villena, C.; Guix, S.; Caballero, S.; Pintó, R.M.; Bosch, A. Potential role of fomites in the vesicular transmission of human astroviruses. Appl. Environ. Microbiol. 2001, 67, 3904–3907. [Google Scholar] [CrossRef] [PubMed]
- Wladowetz, V.W.; Dmitrijewa, R.A.; Safjulin, A.A. Die Persistenz von Viren auf Oberflächen und die Anwendung der UV-Bestrahl- ung zur Virusdesinfektion. Z. Gesamte Hyg. 1974, 7, 173–176. [Google Scholar]
- Gordon, Y.J.; Gordon, R.Y.; Romanowski, E.; Araullo-Cruz, T.P. Prolonged recovery of desiccated adenoviral serotypes 5, 8, and 19 from plastic and metal surfaces in vitro. Ophthalmology 1993, 100, 1835–1839. [Google Scholar] [CrossRef]
- Abad, F.X.; Pinto, R.M.; Bosch, A. Survival of enteric viruses on environmental fomites. Appl. Environ. Microbiol. 1994, 60, 3704–3710. [Google Scholar] [CrossRef]
- Gerth, H.J. Viren und virale Erkrankungen. In Hygiene und Infektionen im Krankenhaus; Thofern, E., Botzenhart, K., Eds.; Fischer: Stuttgart, Germany, 1983; pp. 55–106. [Google Scholar]
- Rabenau, H.F.; Cinatl, J.; Morgenstern, B.; Bauer, G.; Preiser, W.; Doerr, H.W. Stability and inactivation of SARS coronavirus. Med. Microbiol. Immunol. 2005, 194, 1–6. [Google Scholar] [CrossRef]
- Kim, S.J.; Si, J.; Lee, J.E.; Ko, G. Temperature and humidity influences on inactivation kinetics of enteric viruses on surfaces. Environ. Sci. Technol. 2012, 46, 13303–13310. [Google Scholar] [CrossRef]
- D’Souza, D.H.; Sair, A.; Williams, K.; Papafragkou, E.; Jean, J.; Moore, C.; Jaykus, L. Persistence of caliciviruses on environmental surfaces and their transfer to food. Int. J. Food Microbiol. 2006, 108, 84–91. [Google Scholar] [CrossRef]
- Clay, S.; Maherchandani, S.; Malik, Y.S.; Goyal, S.M. Survival on uncommon fomites of feline calicivirus, a surrogate of noroviruses. Am. J. Infect. Control 2006, 34, 41–43. [Google Scholar] [CrossRef]
- Arthur, S.E.; Gibson, K.E. Environmental persistence of Tulane virus—A surrogate for human norovirus. Can. J. Microbiol. 2016, 62, 449–454. [Google Scholar] [CrossRef]
- Warnes, S.L.; Keevil, C.W. Inactivation of norovirus on dry copper alloy surfaces. PloS ONE 2013, 8, e75017. [Google Scholar] [CrossRef]
- Buckley, D.; Fraser, A.; Huang, G.; Jiang, X. Recovery Optimization and Survival of the Human Norovirus Surrogates Feline Calicivirus and Murine Norovirus on Carpet. Appl. Environ. Microbiol. 2017, 83, e01336-17. [Google Scholar] [CrossRef]
- Sizun, J.; Yu, M.W.; Talbot, P.J. Survival of human coronaviruses 229E and OC43 in suspension and after drying on surfaces: A possible source of hospital-acquired infections. J. Hosp. Infect. 2000, 46, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Gagneur, A.; Legrand, M.C.; Picard, B.; Baron, R.; Talbot, P.J.; de Parscau, L.; Sizun, J. Nosocomial infections due to human coronaviruses in the newborn. Arch. Pediatr. 2002, 9, 61–69. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.W.H.; Chu, J.T.S.; Perera, M.R.A.; Hui, K.P.Y.; Yen, H.; Chan, M.C.W.; Peiris, M.; Poon, L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 2020, 1, e10. [Google Scholar] [CrossRef]
- Kratzel, A.; Steiner, S.; Todt, D.; V’kovski, P.; Brueggemann, Y.; Steinmann, J.; Steinmann, E.; Thiel, V.; Pfaender, S. Temperature-dependent surface stability of SARS-CoV-2. J. Infect. 2020, 81, 452–482. [Google Scholar] [CrossRef]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Marzoli, F.; Bortolami, A.; Pezzuto, A.; Mazzetto, E.; Piro, R.; Terregino, C.; Bonfante, F.; Belluco, S. A systematic review of human coronaviruses survival on environmental surfaces. Sci. Total Environ. 2021, 778, 146191. [Google Scholar] [CrossRef] [PubMed]
- Duan, S.M.; Zhao, X.S.; Wen, R.F.; Huang, J.J.; Pi, G.H.; Zhang, S.X.; Han, J.; Bi, S.L.; Ruan, L.; Dong, X.P. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed. Environ. Sci. 2003, 16, 246–255. [Google Scholar]
- Van Doremalen, N.; Bushmaker, T.; Munster, V.J. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Eurosurveillance 2013, 18. [Google Scholar] [CrossRef] [PubMed]
- Otter, J.A.; Donskey, C.; Yezli, S.; Douthwaite, S.; Goldenberg, S.D.; Weber, D.J. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: The possible role of dry surface contamination. J. Hosp. Infect. 2016, 92, 235–250. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.Y.Y.; Cheng, P.K.C.; Lim, W.W.L. Survival of Severe Acute Respiratory Syndrome Coronavirus. Clin. Infect. Dis. 2005, 41, e67–e71. [Google Scholar] [CrossRef]
- Müller, A.; Tillmann, R.L.; Simon, A.; Schildgen, O. Stability of human metapneumovirus and human coronavirus NL63 on medical instruments and in the patient environment. J. Hosp. Infect. 2008, 69, 406–408. [Google Scholar] [CrossRef][Green Version]
- Warnes, S.L.; Little, Z.R.; Keevil, C.W. Human coronavirus 229E remains infectious on common touch surface materials. Mbio 2015, 6, e01697-15. [Google Scholar] [CrossRef]
- Firquet, S.; Beaujard, S.; Lobert, P.-E.; Sané, F.; Caloone, D.; Izard, D.; Hober, D. Survival of Enveloped and Non-Enveloped Viruses on Inanimate Surfaces. Microbes Environ. 2015, 30, 140–144. [Google Scholar] [CrossRef]
- Faix, R.G. Survival of cytomegalovirus on environmental surfaces. J. Pediatr. 1984, 106, 649–652. [Google Scholar] [CrossRef]
- Faix, R.G. Comparative Efficacy of Handwashing Agents against Cytomegalovirus. Infect. Control 1987, 158–162. [Google Scholar] [CrossRef]
- Mocé-Llivina, L.; Papageorgiou, G.T.; Jofre, J. A membrane-based quantitative carrier test to assess the virucidal activity of disinfectants and persistence of viruses on porous fomites. J. Virol. Methods 2006, 135, 49–55. [Google Scholar] [CrossRef]
- Westhoff Smith, D.; Hill-Batorski, L.; N’jai, A.; Eisfeld, A.J.; Neumann, G.; Halfmann, P.; Kawaoka, Y. Ebola Virus Stability under Hospital and Environmental Conditions. J. Infect. Dis. 2016, 214, S142–S144. [Google Scholar] [CrossRef] [PubMed]
- Piercy, T.J.; Smither, S.J.; Steward, J.A.; Eastaugh, L.; Lever, M.S. The survival of filoviruses in liquids, on solid substrates and in a dynamic aerosol. J. Appl. Microbiol. 2010, 109, 1531–1539. [Google Scholar] [CrossRef]
- Mbithi, J.N.; Springthorpe, V.S.; Sattar, S.A. Effect of relative humidity and air temperature on survival of hepatitis A virus on environmental surfaces. Appl. Environ. Microbiol. 1991, 57, 1394–1399. [Google Scholar] [CrossRef]
- Bond, W.W.; Favero, M.S.; Petersen, N.J.; Gravelle, C.R.; Ebert, J.W.; Maynard, J.E. Survival of hepatitis B virus after drying and storage for one week. Lancet 1981, I, 550–551. [Google Scholar] [CrossRef]
- Favero, M.S.; Bond, W.W.; Petersen, N.J.; Berquist, K.R.; Maynard, J.E. Detection Methods for Study of the Stabillity of Hepatitis B Antigen on Surfaces. J. Infect. Dis. 1974, 129, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Paintsil, E.; Binka, M.; Patel, A.; Lindenbach, B.D.; Heimer, R. Hepatitis C virus maintains infectivity for weeks after drying on inanimate surfaces at room temperature: Implications for risks of transmission. J. Infect. Dis. 2014, 209, 1205–1211. [Google Scholar] [CrossRef]
- Doerrbecker, J.; Friesland, M.; Ciesek, S.; Erichsen, T.J.; Mateu-Gelabert, P.; Steinmann, J.; Steinmann, J.; Pietschmann, T.; Steinmann, E. Inactivation and survival of hepatitis C virus on inanimate surfaces. J. Infect. Dis. 2011, 204, 1830–1838. [Google Scholar] [CrossRef]
- Carducci, A.; Verani, M.; Casini, B.; Giuntini, A.; Mazzoni, F.; Rovini, E.; Passaglia, A.; Giusti, L.; Valenza, A.; Lombardi, R. Detection and potential indicators of the presence of hepatitis C virus on surfaces in hospital settings. Lett. Appl. Microbiol. 2002, 34, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Rheinbaben, F.V.; Wolff, M.H. Virusdesinfektion. In Handbuch der Viruswirksamen Desinfektion; Springer: Berlin/Heidelberg, Germany, 2002; pp. 266–282. [Google Scholar]
- Tjotta, E.; Hungnes, O.; Grinde, B. Survival of HIV-1: Activity after disinfection, temperature and pH changes, or drying. J. Med. Virol. 1991, 35, 223–227. [Google Scholar] [CrossRef]
- Barré-Sinoussi, F.; Nugeyre, M.T.; Chermann, J.C. Resistance of AIDS virus at room temperature. Lancet 1985, II, 721–722. [Google Scholar] [CrossRef]
- Nerurkar, L.S.; West, F.; May, M.; Madden, D.L.; Sever, J.L. Survival of herpes simplex virus in water specimens collected from hot spa facilities and on plastic surfaces. JAMA 1983, 250, 3081–3083. [Google Scholar] [CrossRef] [PubMed]
- Tollefson, S.J.; Cox, R.G.; Williams, J.V. Studies of culture conditions and environmental stability of human metapneumovirus. Virus Res. 2010, 151, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Bean, B.; Moore, B.M.; Sterner, B.; Peterson, L.R.; Gerding, D.N.; Balfour, H.H. Survival of influenza viruses an environmental surfaces. J. Infect. Dis. 1982, 146, 47–51. [Google Scholar] [CrossRef]
- Brady, M.T.; Evans, J.; Cuartes, J. Survival and disinfection of parainfluenza viruses on environmental surfaces. Am. J. Infect. Control. 1990, 18, 18–23. [Google Scholar] [CrossRef]
- Pirtle, E.C.; Beran, G.W. Virus survival in the environment. Rev. Sci. Tech. 1991, 10, 733–748. [Google Scholar] [CrossRef]
- Thompson, K.-A.; Bennett, A.M. Persistence of influenza on surfaces. J. Hosp. Infect. 2017, 95, 194–199. [Google Scholar] [CrossRef]
- Greatorex, J.S.; Digard, P.; Curran, M.D.; Moynihan, R.; Wensley, H.; Wreghitt, T.; Varsani, H.; Garcia, F.; Enstone, J.; Nguyen-Van-Ta, J.S. Survival of influenza A(H1N1) on materials found in households: Implications for infection control. PloS ONE 2011, 6, e27932. [Google Scholar] [CrossRef]
- Roden, R.B.S.; Lowy, D.R.; Schiller, J.T. Papillomavirus is resistant to desiccation. J. Infect. Dis. 1997, 176, 1076–1079. [Google Scholar] [CrossRef] [PubMed]
- Tamrakar, S.B.; Henley, J.; Gurian, P.L.; Gerba, C.P.; Mitchell, J.; Enger, K.; Rose, G.B. Persistence analysis of poliovirus on three different types of fomites. J. Appl. Microbiol. 2017, 122, 522–530. [Google Scholar] [CrossRef]
- Wood, J.P.; Choi, Y.W.; Wendling, M.Q.; Rogers, J.V.; Chappie, D.J. Environmental persistence of vaccinia virus on materials. Lett. Appl. Microbiol. 2013, 57, 399–404. [Google Scholar] [CrossRef]
- Schoenbaum, M.A.; Freund, J.D.; Beran, G.W. Survival of pseudorabies virus in the presence of selected diluents and fomites. J. Am. Vet. Med. Assoc. 1991, 198, 1393–1397. [Google Scholar] [PubMed]
- Hall, C.B.; Douglas, R.G.; Geiman, J.M. Possible transmission by fomites of respiratory syncytial virus. J. Infect. Dis. 1980, 141, 98–102. [Google Scholar] [CrossRef]
- Sattar, S.A.; Karim, Y.G.; Springthorpe, V.S.; Johnson-Lussenburg, C.M. Survival of human rhinovirus type 14 dried onto nonporous inanimate surfaces: Effect of relative humidity and suspending medium. Can. J. Microbiol. 1987, 33, 802–806. [Google Scholar] [CrossRef] [PubMed]
- Reed, S.E. An investigation of the possible transmission of rhinovirus colds through direct contact. Epidemiol. Infect. 1975, 75, 249–258. [Google Scholar]
- Ansari, S.A.; Springthorpe, V.S.; Sattar, S.A. Survival and vehicular spread of human rotaviruses: Possible relation to seasonality of outbreaks. Rev. Infect. Dis. 1991, 13, 448–461. [Google Scholar] [CrossRef] [PubMed]
- Sattar, S.; Lloyd-Evans, N.; Springthorpe, V.S. Institutional outbreaks of rotavirus diarrhoea: Potential role of fomites and environmental surfaces as vehicles for virus transmission. Epidemiol. Infect. 1986, 96, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Keswick, B.H.; Pickering, L.; DuPont, H.L.; Woodward, W.E. Survival and Detection of Rotaviruses on Environmental Surfaces in Day Care Centers. Appl. Environ. Microbiol. 1983, 46, 813–816. [Google Scholar] [CrossRef]
- Moe, K.; Shirley, J.A. The Effects of Relative Humidity and Temperature on the Survival of Human Rotavirus in Faeces. Arch. Virol. 1982, 72, 179–186. [Google Scholar] [CrossRef]
- Mahnel, H. Experimentelle Ergebnisse über die Stabilität von Pockenviren unter Labor- und Umweltbedingungen. Zent. Vet. 1987, 34, 449–464. [Google Scholar]
- World Health Organization (WHO). Guidelines on Core Components of Infection Prevention and Control Programs at the National and Acute Health Care Facility Level; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Cassini, A.; Plachouras, D.; Eckmanns, T.; Abu Sin, M.; Blank, H.P.; Ducomble, T.; Haller, S.; Harder, T.; Klingeberg, A.; Sixtensson, M.; et al. Burden of Six Healthcare-Associated Infections on European Population Health: Estimating Incidence-Based Disability Adjusted Life Years through a Population Prevalence-Based Modelling Study. PLoS Med. 2016, 13, e1002150. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. Infezioni Correlate All’assistenza, Aspetti Epidemiologici. Available online: http://www.epicentro.iss.it/problemi/infezioni_correlate/epid.asp (accessed on 10 April 2021).
- Bonadonna, L.; Cannarozzi de Grazia, M.; Capolongo, S.; Casini, B.; Cristina, M.L.; Daniele, G.; D’Alessandro, D.; De Giglio, O.; Di Benedetto, A.; Di Vittorio, G.; et al. Water safety in healthcare facilities. The Vieste Charter. Ann. Ig. 2017, 29, 92–100. [Google Scholar] [CrossRef]
- Caselli, E.; D’Accolti, M.; Vandini, A.; Lanzoni, L.; Camerada, M.T.; Coccagna, M.; Branchini, A.; Antonioli, P.; Balboni, P.G.; Di Luca, D.; et al. Impact of a probiotic-based cleaning intervention on the microbiota ecosystem of the hospital surfaces: Focus on the resistome remodulation. PLoS ONE 2016, 11, e0148857. [Google Scholar] [CrossRef] [PubMed]
- Center of Disease Control (CDC). Guidelines for environmental infection control in health-care facilities. In Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee; CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Legionnaires’ disease. In Annual Epidemiological Report for 2015; ECDC, Ed.; ECDC: Stockholm, Sweden, 2017. [Google Scholar]
- Centers for Disease Control (CDC). Guidelines for environmental infection control in health-care facilities. In Morbidity and Mortality Weekly Report (MMWR); No. RR-10; CDC: Atlanta, GA, USA, 2003; Volume 52. [Google Scholar]

| Bacteria | Duration of Survival on Inanimate Surfaces (Range) | References |
|---|---|---|
| Acinetobacter baumannii (including MRD) | 2 days–>4 months | [75,76,77] |
| Bordetella pertussis | 3–5 days | [78] |
| Burkolderia cepacia | >1 week | [79] |
| Campylobacter jejuni | 15 min–7 h | [80] |
| Chlamydia pneumonae/tracomatis | 30 min–≤30 h | [81,82] |
| Chlamydia psittaci | 15 days to months | [83] |
| Clostridium difficile (spores) | 5 months | [84] |
| Corynebacterium diphtheriae | 7 days–6 months | [78] |
| Corynebacterium pseudotuberculosis | 1–8 days | [85] |
| Enterococcus faecalis/faecium (including VRE) | 5 day–3 months | [86,87,88,89] |
| Escherichia coli (including pathogenic) | <1 h–28 days | [77,90,91] |
| Haemophilus influenzae | 12 days | [9] |
| Helicobacter pylori | ≤90 min | [92] |
| Klebsiella pneumoniae | 1 h–6 weeks | [93,94,95,96] |
| Listeria monocitogenes | at least 24 h | [97] |
| Mycobacterium tuberculosis | 10–120 day | [98] |
| Neisseria gonorrhoeae | >24 h | [99] |
| Neisseria meningitides | 72 h | [100] |
| Proteus mirabilis | 4 h–26 days | [94] |
| Proteus vulgaris | 1–2 days | [98] |
| Pseudomonas aeruginosa | 5 h–33 days | [93,101] |
| Salmonella enterica serovar Abony | 1–>24 h | [102] |
| Salmonella enterica serovar Enteritidis | 1–48 h | [93,102] |
| Salmonella enterica serovar Typhimurium | 5 h–12 weeks | [93,103,104] |
| Salmonella typhi | 6 h–4 weeks | [98] |
| Salmonella spp. | at least 30 days | [105] |
| Serratia marcescens | <1 h–11 days | [93,94] |
| Shigella spp. | 1.5–4 h | [106] |
| Staphylococcus aureus (including MRSA) | 6 h–12 days | [77,107,108] |
| Stenotrophomonas maltophylia | 2–7 days | [101] |
| Streptococcus pneumoniae | 1 day up 30 months | [109,110] |
| Streptococcus pyogenes | 3 days–6.5 months | [110,111] |
| Yersinia pestis | up to 5 days | [112] |
| Yeasts and Molds | ||
| Candida albicans | 1–120 days | [113,114] |
| Candida auris (MRD) | 3–14 days | [114,115,116,117] |
| Cryptococcus neoformans | 30 days | [101] |
| Aspergillus spp. (conidia) | 1 year | [118,119] |
| Aspergillus flavus | 2–30 days | [120,121] |
| Aspergillus fumigatus | 1–30 days | [101,120,121] |
| Aspergillus niger | 1–30 days | [120,121,122] |
| Fusarium spp. | 48 h–>30 days | [120,121,123] |
| Mucor spp. | 16–>30 days | [121] |
| Paecilomyces spp. | <1–11 days | [120] |
| Penicillum crysogenum | 6–120 h | [121] |
| Viruses | Duration of Survival on Inanimate Surfaces (Range) | References |
|---|---|---|
| Adenovirus | 1 h–>12 weeks | [124,125,126,127,128,129,130,131] |
| Astrovirus | 7–90 days | [126] |
| Caliciviridae | <5 min–>168 days | [132,133,134,135,136,137] |
| Coronavirus (SARS-CoV-2, SARS-CoV, MERS-CoV, HCoV -229E, HCoV -OC43, HCoV -NL63) | 30 min–>8 days | [131,138,139,140,141,142,143,144,145,146,147,148,149,150] |
| Coxsackie virus | 2–5 weeks | [125,130,151] |
| Cytomegalovirus | 1 h–4 h | [152,153] |
| Echovirus | 48 h–7 days | [127,154] |
| Filoviruses | 2 days–>32 days | [155,156] |
| Hepatitis A Virus | 2 h–>60 days | [126,129,132,157] |
| Hepatitis B Virus | >14 days | [158,159] |
| Hepatitis C Virus | 5 days–6 weeks | [160,161,162] |
| Human Immunodeficiency Virus | >5 days | [163,164,165] |
| Herpes Simplex Virus, Type 1 and 2 | 4.5 h–>8 weeks | [125,130,131,151,163] [166] |
| Human Metapneumovirus (HMPV) | 2–8 h | [167] |
| Influenza Virus | 1–2 days | [127,147,168,169,170,171,172] |
| Parainfluenza Virus | <0.5 h–>8 h | [169] |
| Feline Norovirus and Calicivirus | 8 h–7 days | [133,134] |
| Papillomaviridae | >7 days | [173] |
| Papovavirus | 8 days | [163] |
| Parvovirus | >1 year | [163] |
| Poliovirus Type 1 | 4 h– >60 days | [129,154,157,163,174] |
| Poliovirus Type 2 | 1 day–8 weeks | [125,126,130] |
| Poxviridae | <1 day–56 days | [125,175] |
| Pseudorabies Virus | >/= 7 days | [176] |
| Respiratory Syncytial Virus | 0.5 h–6 months | [177] |
| Rhinovirus | 2 h–7 days | [178,179] |
| Rotavirus | 1 h–>60 days | [126,129,180,181,182,183] |
| Vaccinia Virus | 3–>20 weeks | [125,184] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonadonna, L.; Briancesco, R.; Coccia, A.M.; Meloni, P.; Rosa, G.L.; Moscato, U. Microbial Air Quality in Healthcare Facilities. Int. J. Environ. Res. Public Health 2021, 18, 6226. https://doi.org/10.3390/ijerph18126226
Bonadonna L, Briancesco R, Coccia AM, Meloni P, Rosa GL, Moscato U. Microbial Air Quality in Healthcare Facilities. International Journal of Environmental Research and Public Health. 2021; 18(12):6226. https://doi.org/10.3390/ijerph18126226
Chicago/Turabian StyleBonadonna, Lucia, Rossella Briancesco, Anna Maria Coccia, Pierluigi Meloni, Giuseppina La Rosa, and Umberto Moscato. 2021. "Microbial Air Quality in Healthcare Facilities" International Journal of Environmental Research and Public Health 18, no. 12: 6226. https://doi.org/10.3390/ijerph18126226
APA StyleBonadonna, L., Briancesco, R., Coccia, A. M., Meloni, P., Rosa, G. L., & Moscato, U. (2021). Microbial Air Quality in Healthcare Facilities. International Journal of Environmental Research and Public Health, 18(12), 6226. https://doi.org/10.3390/ijerph18126226






