Floorball Injuries Presenting to a Swiss Adult Emergency Department: A Retrospective Study (2013–2019)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection and Retrospective Analysis
2.3. Triage System
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Patient Analysis
3.1.1. Annual Distribution
3.1.2. Age and Sex Distribution
3.2. Injury and Clinical Analysis
3.2.1. Location and Type of Injury
3.2.2. Mechanisms of Injury
3.2.3. Treatment
3.2.4. Admission and Discharge
3.2.5. Cost Analysis
4. Discussion
4.1. Patient Analysis
4.2. Age and Sex Distribution
4.3. Injury and Clinical Analysis
4.3.1. Eyes
4.3.2. Lower Limbs
4.3.3. Face and Head
4.4. Type of Injury
4.5. Mechanisms of Injury
4.6. Admission, Discharge and Triage
4.7. Cost Analysis
4.8. Suggestions for Prevention
- Protective eyewear in floorball should be mandatory for young adults until at least the age of 16 years. Extending the age limit further and encouraging eyewear in non-organized practise should be seriously considered (Figure 5).
- As there are numerous injuries to the lower extremities, prevention should be focused on acute ankle and knee injuries. Avramakis et al. suggest that high-shanked shoes with low soles reduce supination in the ankle joint [38].
- The impact of dental injuries and therefore the knowledge of first aid and the benefit of wearing mouth guards in floorball should be further investigated.
- More effort is needed in analyzing the biomechanics behind specific movements in floorball, as this leads to a better understanding of the different injury mechanisms.
- Once this has been achieved, different equipment should be examined to find the optimum compromise between good performance and good protection.
- The main focus for injury prevention has been laid on competitive sport. As the popularity of floorball grows, further efforts should go into comparing competitive and unorganized play in order to establish whether there are different profiles of injuries and risks and whether preventive measurements in competitive floorball also work in mass sports.
4.9. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Federation, I.F. Floorball in a Nutshell. Available online: https://floorball.sport/this-is-floorball/floorball-in-a-nutshell/ (accessed on 1 May 2020).
- Federation, I.F. History in Short. Available online: https://floorball.sport/this-is-floorball/history-in-short/ (accessed on 1 May 2020).
- Tervo, T.; Nordstrom, A. Science of floorball: A systematic review. Open Access J. Sports Med. 2014, 5, 249–255. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Drolsum, L. Eye injuries in sports. Scand. J. Med. Sci. Sports 1999, 9, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Maxen, M.; Kühl, S.; Krastl, G.; Filippi, A. Eye injuries and orofacial traumas in floorball—A survey in Switzerland and Sweden. Dent. Traumatol. 2011, 27, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Engel, J.; Kälin, M.; Rogan, S. Injuries in Floorball: A Questionnaire Survey in Swiss National League A Floorball Players. Sportverletz Sportschaden 2019, 33, 36–42. [Google Scholar] [PubMed]
- Pasanen, K.; Hietamo, J.; Vasankari, T.; Kannus, P.; Heinonen, A.; Kujala, U.M.; Mattila, V.M.; Parkkari, J. Acute injuries in Finnish junior floorball league players. J. Sci. Med. Sport 2018, 21, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Tranaeus, U.; Heintz, E.; Johnson, U.; Forssblad, M.; Werner, S. Injuries in Swedish floorball: A cost analysis. Scand. J. Med. Sci. Sports 2017, 27, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Tranaeus, U.; Gotesson, E.; Werner, S. Injury Profile in Swedish Elite Floorball: A Prospective Cohort Study of 12 Teams. Sports Health 2016, 8, 224–229. [Google Scholar] [CrossRef]
- Pasanen, K.; Bruun, M.; Vasankari, T.; Nurminen, M.; Frey, W.O. Injuries during the international floorball tournaments from 2012 to 2015. BMJ Open Sport Exerc. Med. 2016, 2, e000217. [Google Scholar] [CrossRef][Green Version]
- Pasanen, K.; Parkkari, J.; Pasanen, M.; Hiilloskorpi, H.; Makinen, T.; Jarvinen, M.; Kannus, P. Neuromuscular training and the risk of leg injuries in female floorball players: Cluster randomised controlled study. BMJ 2008, 337, a295. [Google Scholar] [CrossRef]
- Bro, T.; Ghosh, F. Floorball-related eye injuries: The impact of protective eyewear. Scand. J. Med. Sci. Sports 2017, 27, 430–434. [Google Scholar] [CrossRef]
- Aman, M.; Forssblad, M.; Larsen, K. Incidence and body location of reported acute sport injuries in seven sports using a national insurance database. Scand. J. Med. Sci. Sports 2017, 28, 1147–1158. [Google Scholar] [CrossRef]
- Snellman, K.; Parkkari, J.; Kannus, P.; Leppälä, J.; Vuori, I.; Järvinen, M. Sports injuries in floorball: A prospective one-year follow-up study. Int. J. Sports Med. 2001, 22, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Leivo, T.; Haavisto, A.K.; Sahraravand, A. Sports-related eye injuries: The current picture. Acta Ophthalmol. 2015, 93, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Leivo, T.; Puusaari, I.; Makitie, T. Sports-related eye injuries: Floorball endangers the eyes of young players. Scand. J. Med. Sci. Sports 2007, 17, 556–563. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Babarro, A.; Calleja-González, J.; Viribay, A.; Fernández-Lázaro, D.; León-Guereño, P.; Mielgo-Ayuso, J. Relationship between Training Factors and Injuries in Stand.-Up Paddleboarding Athletes. Int. J. Environ. Res. Public Health 2021, 18, 880. [Google Scholar] [CrossRef] [PubMed]
- BFU. Status 2020 Statistik der Nichtberufsunfälle und des Sicherheitsniveaus in der Schweiz. Available online: https://www.bfu.ch/api/publications/bfu_2.384.01_status%202020%20%E2%80%93%20statistik%20der%20nichtberufsunf%C3%A4lle%20und%20des%20sicherheitsniveaus%20in%20der%20schweiz%20.pdf (accessed on 1 May 2020).
- Müller, M.; Schechter, C.B.; Hautz, W.E.; Sauter, T.C.; Exadaktylos, A.K.; Stock, S.; Birrenbach, T. The development and validation of a resource consumption score of an emergency department consultation. PLoS ONE 2021, 16, e0247244. [Google Scholar] [CrossRef] [PubMed]
- Dale, J.; Lang, H.; Roberts, J.A.; Green, J.; Glucksman, E. Cost effectiveness of treating primary care patients in accident and emergency: A comparison between general practitioners, senior house officers, and registrars. BMJ 1996, 312, 1340–1344. [Google Scholar] [CrossRef]
- Lamprecht, M.; Stamm, H. Observatorium Sport und Bewegung Schweiz Laufend aktualisierte Indikatoren Stand. November 2015 (Jahresbericht 2015); L&S Sozialforschung und Beratung AG: Zürich, Switzerland, 2015. [Google Scholar]
- Mackway-Jones, K. Emergency Triage: Manchester Triage Group; BMJ Publishing Group: London, UK, 1997. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Swissuihockey. Verband. Available online: https://www.swissunihockey.ch/de/administration/verband/ (accessed on 1 May 2020).
- Clarsen, B.; Bahr, R.; Heymans, M.W.; Engedahl, M.; Midtsundstad, G.; Rosenlund, L.; Thorsen, G.; Myklebust, G. The prevalence and impact of overuse injuries in five Norwegian sports: Application of a new surveillance method. Scand. J. Med. Sci. Sports 2015, 25, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Clarsen, B.; Myklebust, G.; Bahr, R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: The Oslo Sports Trauma Research Centre (OSTRC) Overuse Injury Questionnaire. Br. J. Sports Med. 2013, 47, 495–502. [Google Scholar] [CrossRef]
- Kaufman, J.H.; Tolpin, D.W. Glaucoma after traumatic angle recession. A ten-year prospective study. Am. J. Ophthalmol. 1974, 78, 648–654. [Google Scholar] [CrossRef]
- Ng, D.S.-C.; Ching, R.H.-Y.; Chan, C.W.-N. Angle-recession glaucoma: Long-term clinical outcomes over a 10-year period in traumatic microhyphema. Int. Ophthalmol. 2014, 35, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, F.; Bauer, B. Sports-related eye injuries. Acta Ophthalmol. Scand. 1995, 73, 353–354. [Google Scholar] [CrossRef] [PubMed]
- Swissuihockey.ch. Ich Spüre die Brille Schon gar Nicht Mehr. Available online: https://www.swissunihockey.ch/de/news/ich-spuere-die-brille-schon-gar-nicht-mehr/ (accessed on 1 May 2020).
- Leppänen, M.; Pasanen, K.; Krosshaug, T.; Kannus, P.; Vasankari, T.; Kujala, U.M.; Bahr, R.; Perttunen, J.; Parkkari, J. Sagittal Plane Hip, Knee, and Ankle Biomechanics and the Risk of Anterior Cruciate Ligament Injury: A Prospective Study. Orthop. J. Sports Med. 2017, 5, 2325967117745487. [Google Scholar] [CrossRef]
- Leppanen, M.; Pasanen, K.; Kujala, U.M.; Vasankari, T.; Kannus, P.; Ayramo, S.; Krosshaug, T.; Bahr, R.; Avela, J.; Perttunen, J.; et al. Stiff Landings Are Associated With Increased ACL Injury Risk in Young Female Basketball and Floorball Players. Am. J. Sports Med. 2017, 45, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Leppanen, M.; Pasanen, K.; Kulmala, J.-P.; Kujala, U.M.; Krosshaug, T.; Kannus, P.; Perttunen, J.; Vasankari, T.; Parkkari, J. Knee Control and Jump-Landing Technique in Young Basketball and Floorball Players. Int. J. Sports Med. 2016, 37, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Pasanen, K.; Parkkari, J.; Kannus, P.; Rossi, L.; Palvanen, M.; Natri, A.; Järvinen, M. Injury risk in female floorball: A prospective one-season follow-up. Scand. J. Med. Sci. Sports 2008, 18, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Wikstrom, J.; Andersson, C. A prospective study of injuries in licensed floorball players. Scand. J. Med. Sci. Sports 1997, 7, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Aman, M.; Forssblad, M.; Henriksson-Larsen, K. Incidence and severity of reported acute sports injuries in 35 sports using insurance registry data. Scand. J. Med. Sci. Sports 2016, 26, 451–462. [Google Scholar] [CrossRef]
- Löfgren, O.; Andersson, N.; Björnstig, U.; Lorantzon, R. Incidence, nature and causes of floorball injuries. Scand. J. Med. Sci. Sports 1994, 4, 211–214. [Google Scholar] [CrossRef]
- Avramakis, E.; Stakoff, A.; Stussi, E. Effect of shoe shaft and shoe sole height on the upper ankle joint in lateral movements in floorball (uni-hockey). Sportverletz Sportschaden 2000, 14, 98–106. [Google Scholar] [CrossRef] [PubMed]




| Total, n (%) | Male, n (%) | Female, n (%) | p | ||||
|---|---|---|---|---|---|---|---|
| Age group | 0.546 | ||||||
| 16–25 years | 119 | −45.2 | 16 | −55.2 | 103 | −44 | |
| 26–35 years | 79 | −30 | 8 | −27.6 | 71 | −30.3 | |
| 36–45 years | 32 | −12.2 | 3 | −10.3 | 29 | −12.4 | |
| 46–55 years | 19 | −7.2 | 0 | 0 | 19 | −8.1 | |
| 56–65 years | 10 | −3.8 | 1 | −3.4 | 9 | −3.8 | |
| >65 years | 4 | −1.5 | 1 | −3.4 | 3 | −1.3 | |
| Year of consultation | 0.722 | ||||||
| 2013 | 28 | −10.6 | 3 | −10.3 | 25 | −10.7 | |
| 2014 | 32 | −12.2 | 3 | −10.3 | 29 | −12.4 | |
| 2015 | 36 | −13.7 | 1 | −3.4 | 35 | −15 | |
| 2016 | 51 | −19.4 | 6 | −20.7 | 45 | −19.2 | |
| 2017 | 33 | −12.5 | 5 | −17.2 | 28 | −12 | |
| 2018 | 58 | −22.1 | 8 | −27.6 | 50 | −21.4 | |
| 2019 | 25 | −9.5 | 3 | −10.3 | 22 | −9.4 | |
| Triage | 0.783 | ||||||
| 1 (acute life-threatening) | 4 (1.5) | 0 (0.0) | 4 (1.7) | ||||
| 2 (highly urgent) | 50 (19.0) | 5 (17.2) | 45 (19.2) | ||||
| 3 (urgent) | 193 (73.4) | 23 (79.3) | 170 (72.6) | ||||
| 4 (less urgent) | 16 (6.1) | 1 (3.4) | 15 (6.4) | ||||
| Treatment area | 0.964 | ||||||
| Fast track | 45 (17.1) | 5 (17.2) | 40 | −17.1 | |||
| surgery/resuscitation room | 83 | −31.6 | 7 | −24.1 | 76 | −32.5 | |
| orthopaedic | 5 | −1.9 | 1 | −3.4 | 4 | −1.7 | |
| cranio-maxillo-facial surgery | 3 | −1.1 | 0 | 0 | 3 | −1.3 | |
| ophthalmology | 108 | −41.1 | 14 | −48.3 | 94 | −40.2 | |
| neurology | 3 | −1.1 | 0 | 0 | 3 | −1.3 | |
| ears–nose–throat | 9 | −3.4 | 1 | −3.4 | 8 | −3.4 | |
| internal medicine | 6 | −2.3 | 1 | −3.4 | 5 | −2.1 | |
| urology | 1 | −0.4 | 0 | 0 | 1 | −0.4 | |
| Route of admission | 0.424 | ||||||
| self-admission | 211 | −80.2 | 25 (86.2) | 186 (79.5) | |||
| ambulance | 13 | −4.9 | 2 (6.9) | 11 (4.7) | |||
| family doctor/city emergency practice | 13 | −4.9 | 2 (6.9) | 11 (4.7) | |||
| other hospital | 25 | −9.5 | 0 | 0 | 25 (10.7) | ||
| callmed | 1 | −0.4 | 0 | 0 | 1 (0.4) | ||
| Route of discharge | 0.532 | ||||||
| home | 245 | −93.2 | 26 | −89.7 | 219 | −93.6 | |
| hospitalized | 16 | −6.1 | 3 | −10.3 | 13 | −5.6 | |
| transfer to a different hospital | 2 | −0.8 | 0 | 0 | 2 | −0.9 | |
| Costs | 0.407 | ||||||
| <CHF 500 | 151 | −57.4 | 17 | −58.6 | 134 | −57.3 | |
| CHF 501- to 1000 | 55 | −20.9 | 8 | −27.6 | 47 | −20.1 | |
| CHF 1001- to 2000 | 35 | −13.3 | 1 | −3.4 | 34 | −14.5 | |
| CHF 2001- to CHF 5000 | 12 | −4.6 | 1 | −3.4 | 11 | −4.7 | |
| more than CHF 5001 | 10 | −3.8 | 2 | −6.9 | 8 | −3.4 | |
| Total, n (%) | Male, n (%) | Female, n (%) | p | p | ||||
|---|---|---|---|---|---|---|---|---|
| Type of trauma | 0.826 | |||||||
| Monotrauma | 235 | −89.4 | 25 | −86.2 | 210 | −89.7 | 0.56 | |
| Combined without life-threatening injuries | 22 | −8.4 | 3 | −10.3 | 19 | −8.1 | 0.683 | |
| Polytrauma with life-threatening injuries | 6 | −2.3 | 1 | −3.4 | 5 | −2.1 | 0.655 | |
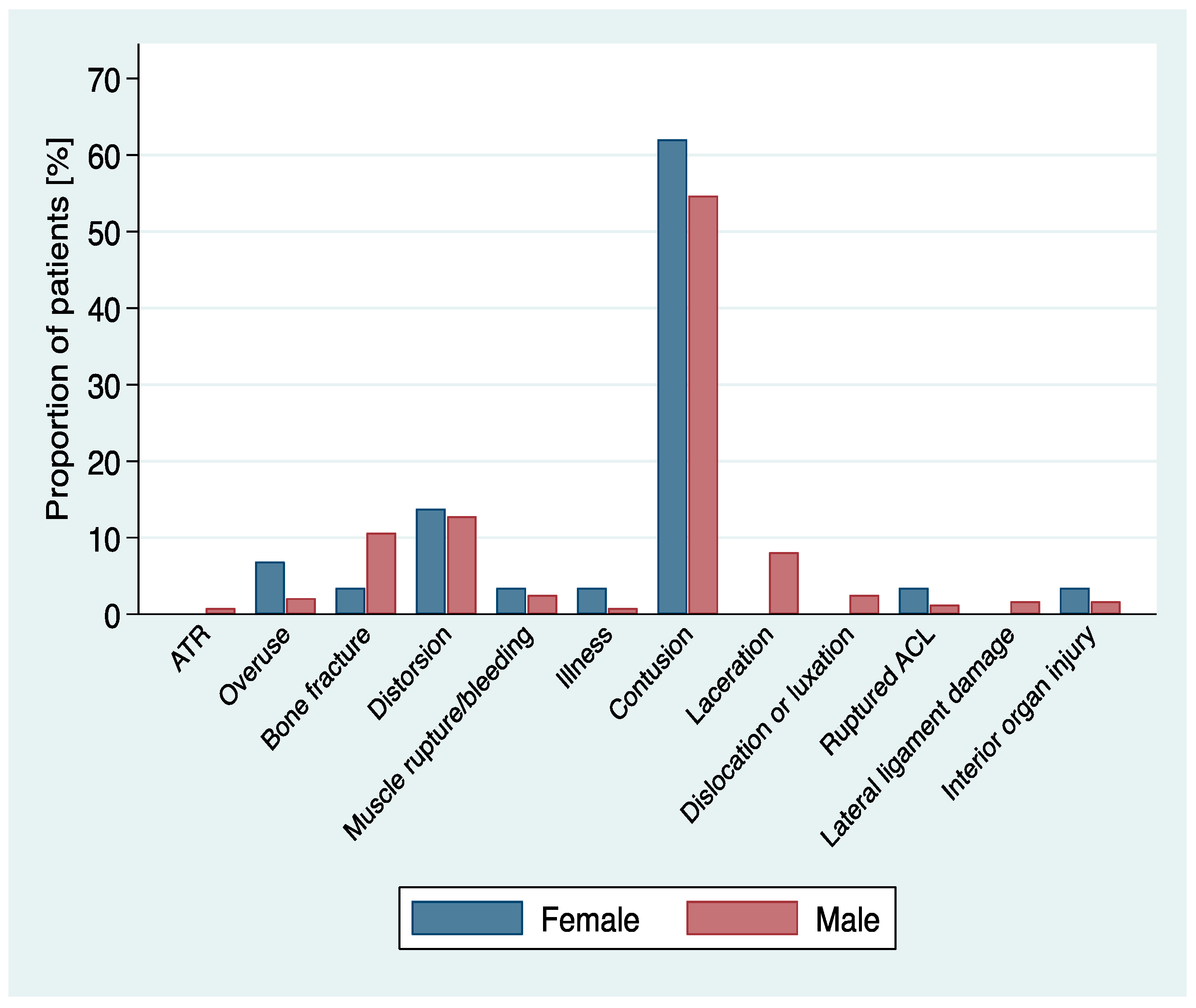
| Type of injury | 0.488 | |||||||
| Achilles tendon rupture (ATR) | 2 | −0.8 | 0 | 0 | 2 | −0.9 | 0.671 | |
| Overuse | 7 | −2.7 | 2 | −6.9 | 5 | −2.1 | 0.133 | |
| Bone fracture | 26 | −9.9 | 1 | −3.4 | 25 | −10.7 | 0.218 | |
| Distortion | 34 | −12.9 | 4 | −13.8 | 30 | −12.8 | 0.883 | |
| Muscle rupture/bleeding | 7 | −2.7 | 1 | −3.4 | 6 | −2.6 | 0.78 | |
| Illness | 3 | −1.1 | 1 | −3.4 | 2 | −0.9 | 0.215 | |
| Contusion | 146 | −55.5 | 18 | −62.1 | 128 | −54.7 | 0.451 | |
| Laceration | 19 | −7.2 | 0 | 0 | 19 | −8.1 | 0.111 | |
| Dislocation/luxation | 6 | −2.3 | 0 | 0 | 6 | −2.6 | 0.383 | |
| Ruptured anterior cruciate ligament (ACL) | 4 | −1.5 | 1 | −3.4 | 3 | −1.3 | 0.369 | |
| Lateral ligament damage | 4 | −1.5 | 0 | 0 | 4 | −1.7 | 0.478 | |
| Interior organ injury | 5 | −1.9 | 1 | −3.4 | 4 | −1.7 | 0.518 | |
| Body part | 0.978 | |||||||
| Lower extremities | ||||||||
| Heel | 1 | −0.4 | 0 | 0 | 1 | −0.4 | 0.518 | |
| Ankle | 22 | −8.4 | 3 | −10.3 | 19 | −8.1 | 0.724 | |
| Knee | 22 | −8.4 | 4 | −13.8 | 18 | −7.7 | 0.683 | |
| Foot, Toe | 10 | −3.8 | 1 | −3.4 | 9 | −3.8 | 0.263 | |
| Calf | 7 | −2.7 | 0 | 0 | 7 | −3 | 0.916 | |
| Thigh | 5 | −1.9 | 1 | −3.4 | 4 | −1.7 | 0.345 | |
| Upper extremities | ||||||||
| Hand and Finger | 10 | −3.8 | 1 | −3.4 | 9 | −3.8 | 0.528 | |
| Wrist | 4 | −1.5 | 0 | 0 | 4 | −1.7 | 0.916 | |
| Elbow | 2 | −0.8 | 0 | 0 | 2 | −0.9 | 0.478 | |
| Humerus, Arm | 1 | −0.4 | 0 | 0 | 1 | −0.4 | 0.724 | |
| Torso | ||||||||
| Torso, Rib | 11 | −4.2 | 1 (3.4) | 10 | −4.3 | 0.834 | ||
| Back, Neck | 9 | −3.4 | 0 | 0 | 9 | −3.8 | 0.283 | |
| Shoulder, Clavicle | 8 | −3 | 0 | 0 | 8 | −3.4 | 0.312 | |
| Genitals | 2 (0.8) | 0 (0.0) | 2 (0.9) | 0.617 | ||||
| Face, Head | 33 | −12.5 | 3 | −10.3 | 30 | −12.8 | 0.704 | |
| Tooth | 1 | −0.4 | 0 | 0 | 1 | −0.4 | 0.724 | |
| Eye | 115 | −43.7 | 15 | −51.7 | 100 | −42.7 | 0.357 | |
| Location of injury | 0.419 | |||||||
| Eye | 115 | −43.7 | 15 | −51.7 | 100 | −42.7 | 0.357 | |
| Lower extremities | 68 | −25.9 | 9 | −31 | 59 | −25.2 | 0.499 | |
| Upper extremities | 24 | −9.1 | 1 | −3.4 | 23 | −9.8 | 0.26 | |
| Trunk and Face | 56 | −21.3 | 4 | −13.8 | 52 | −22.2 | 0.296 | |
| Mechanism of injury | 0.474 | |||||||
| Blow with stick | 21 | −8 | 2 | −6.9 | 19 | −8.1 | 0.819 | |
| Blow with ball | 103 | −39.2 | 16 | −55.2 | 87 | −37.2 | 0.061 | |
| Direct player contact | 34 | −12.9 | 2 | −6.9 | 32 | −13.7 | 0.305 | |
| Tripping over own feet/over stick | 48 | −18.3 | 3 | −10.3 | 45 | −19.2 | 0.243 | |
| Fall after tackle | 18 | −6.8 | 2 | −6.9 | 16 | −6.8 | 0.991 | |
| Collision with boards/goal | 9 | −3.4 | 0 | 0 | 9 | −3.8 | 0.283 | |
| No contact | 25 | −9.5 | 4 | −13.8 | 21 | −9 | 0.404 | |
| No information | 5 | −1.9 | 0 | 0 | 5 | −2.1 | 0.427 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radtke, S.; Trepp, G.-L.; Müller, M.; Exadaktylos, A.K.; Klukowska-Rötzler, J. Floorball Injuries Presenting to a Swiss Adult Emergency Department: A Retrospective Study (2013–2019). Int. J. Environ. Res. Public Health 2021, 18, 6208. https://doi.org/10.3390/ijerph18126208
Radtke S, Trepp G-L, Müller M, Exadaktylos AK, Klukowska-Rötzler J. Floorball Injuries Presenting to a Swiss Adult Emergency Department: A Retrospective Study (2013–2019). International Journal of Environmental Research and Public Health. 2021; 18(12):6208. https://doi.org/10.3390/ijerph18126208
Chicago/Turabian StyleRadtke, Stephanie, Gian-Luca Trepp, Martin Müller, Aristomenis K. Exadaktylos, and Jolanta Klukowska-Rötzler. 2021. "Floorball Injuries Presenting to a Swiss Adult Emergency Department: A Retrospective Study (2013–2019)" International Journal of Environmental Research and Public Health 18, no. 12: 6208. https://doi.org/10.3390/ijerph18126208
APA StyleRadtke, S., Trepp, G.-L., Müller, M., Exadaktylos, A. K., & Klukowska-Rötzler, J. (2021). Floorball Injuries Presenting to a Swiss Adult Emergency Department: A Retrospective Study (2013–2019). International Journal of Environmental Research and Public Health, 18(12), 6208. https://doi.org/10.3390/ijerph18126208







